Predictors of Rehospitalization and Mortality in Diabetes-Related Hospital Admissions
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Endpoints and Variables
2.3. Inclusion and Exclusion Criteria
2.4. Statistical Analysis
3. Results
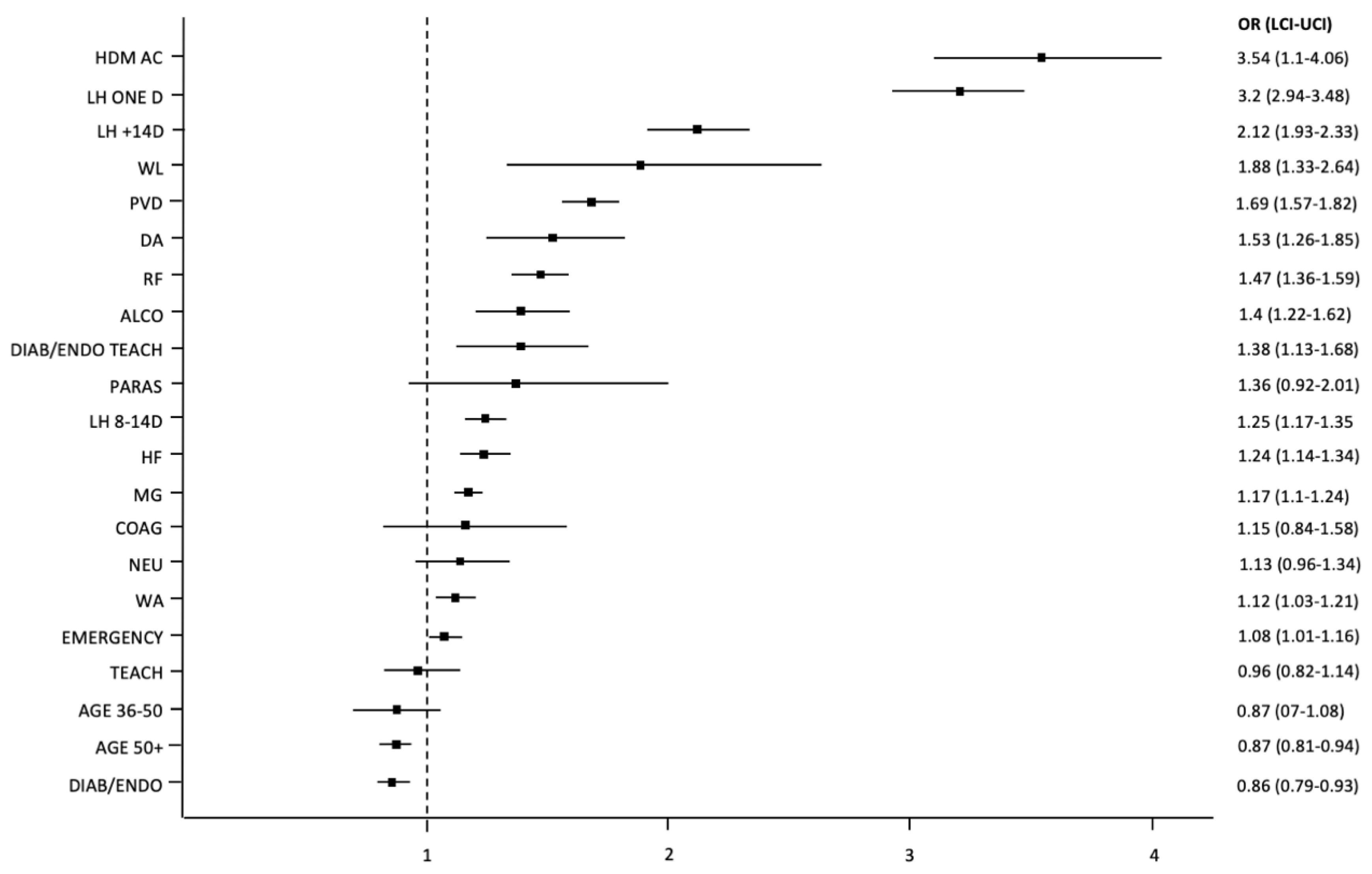
3.1. Readmissions to the Hospital in the Period of 90 Days after Discharge
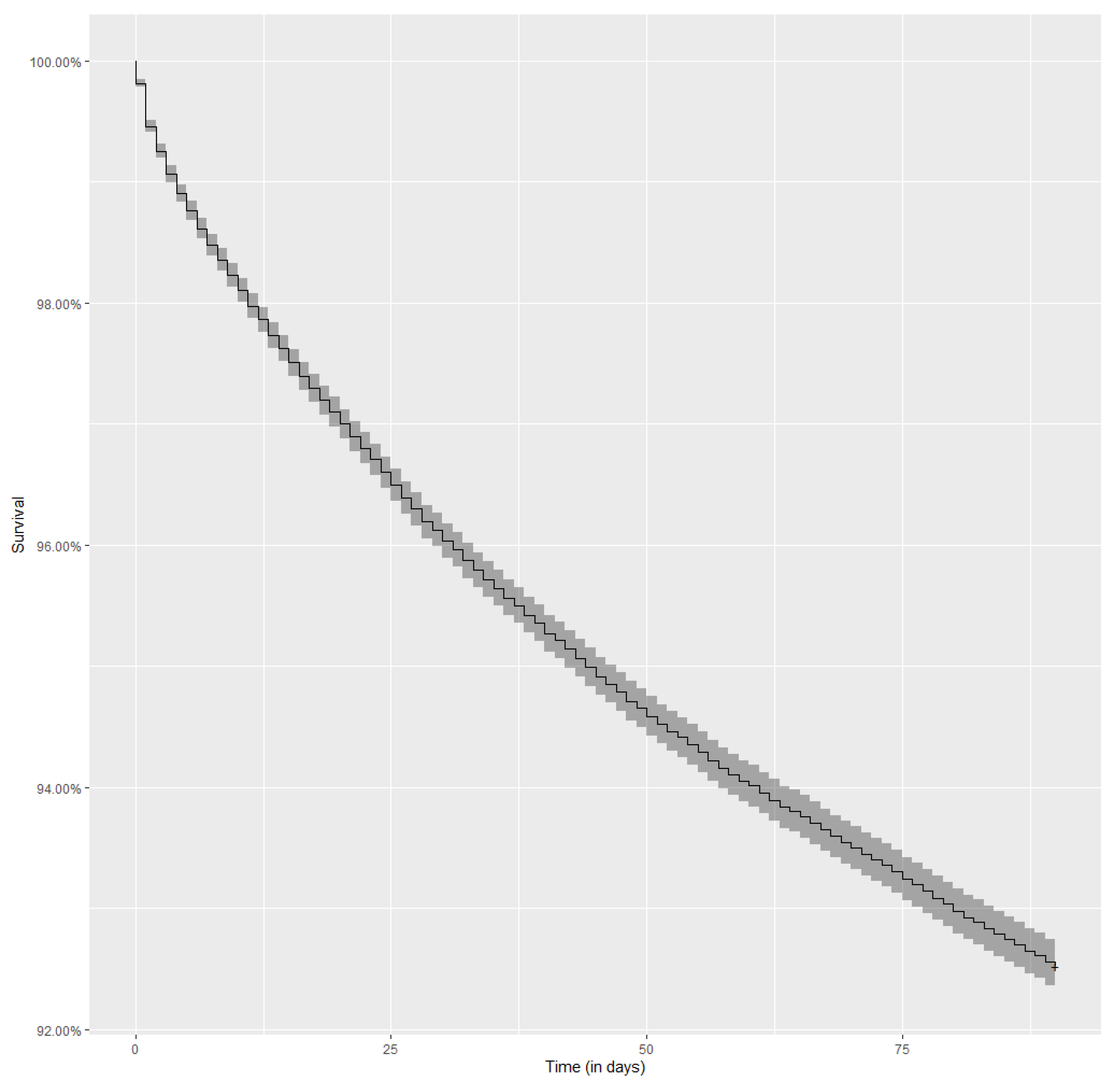
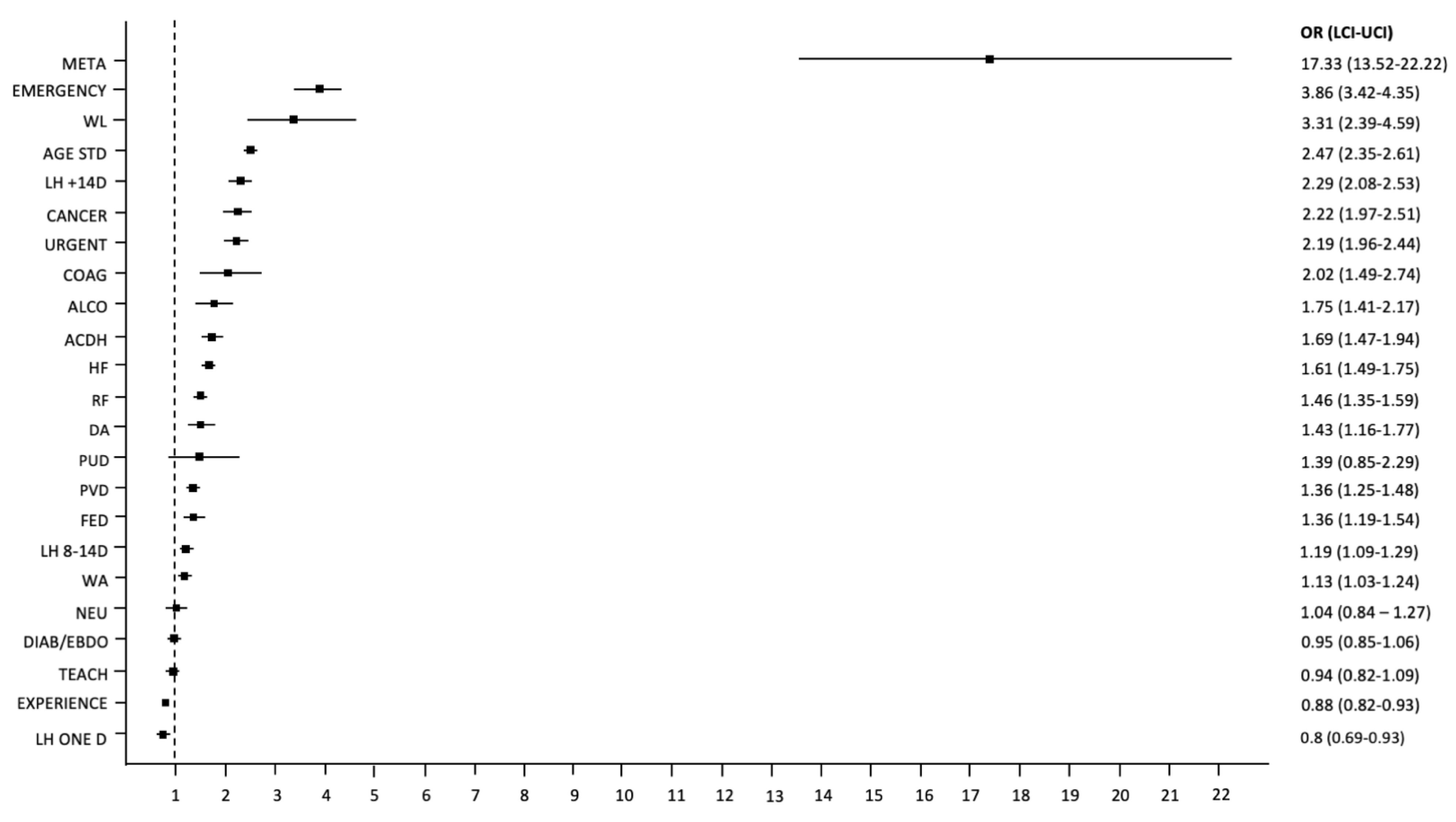
3.2. Death during 90 Days following Discharge
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- IDF Diabetes Atlas 10th Edition 2021. Available online: http://www.idf.org/diabetesatlas (accessed on 7 December 2021).
- Ostling, S.; Wyckoff, J.; Ciarkowski, S.L.; Pai, C.W.; Choe, H.M.; Bahl, V.; Gianchandani, R. The relationship between diabetes mellitus and 30-day readmission rates. Clin. Diabetes Endocrinol. 2017, 3, 3. [Google Scholar] [CrossRef]
- Carral, F.; Olveira, G.; Salas, J.; Garcia, L.; Sillero, A.; Aguilar, M. Care resource utilization and direct costs incurred by people with diabetes in a Spanish hospital. Diabetes Res. Clin. Pract. 2002, 56, 27–34. [Google Scholar] [CrossRef]
- Lind, M.; Garcia-Rodriguez, L.A.; Booth, G.L.; Cea-Soriano, L.; Shah, B.R.; Ekeroth, G.; Lipscombe, L.L. Mortality trends in patients with and without diabetes in Ontario, Canada and the UK from 1996 to 2009: A population-based study. Diabetologia 2013, 56, 2601–2608. [Google Scholar] [CrossRef]
- Rao Kondapally Seshasai, S.; Kaptoge, S.; Thompson, A.; Di Angelantonio, E.; Gao, P.; Sarwar, N.; Whincup, P.H.; Mukamal, K.J.; Gillum, R.F.; Holme, I.; et al. Diabetes Mellitus, fasting glucose, and risk of cause-specific death. N. Engl. J. Med. 2011, 364, 829–841. [Google Scholar] [PubMed]
- Rubin, D.J.; Shah, A.A. Predicting and Preventing Acute Care Re-Utilization by Patients with Diabetes. Curr. Diabetes Rep. 2021, 21, 34. [Google Scholar] [CrossRef]
- Caravaca, F.; Chávez, E.; Alvarado, R.; García-Pino, G.; Luna, E. Sudden cardiac death in non-dialysis chronic kidney disease patients. Nefrologia 2016, 36, 404–409. [Google Scholar] [CrossRef]
- Cheng, Y.; Borrego, M.E.; Frost, F.J.; Petersen, H.; Raisch, D.W. Predictors for mortality in hospitalized patients with chronic obstructive pulmonary disease. Springerplus 2014, 3, 359. [Google Scholar] [CrossRef]
- Elixhauser, A.; Steiner, C.; Harris, D.R.; Coffey, R.M. Comorbidity Measures for Use with Administrative Data. Med Care 1998, 36, 8–27. [Google Scholar] [CrossRef]
- Walicka, M.; Chlebus, M.; Śliwczyński, A.; Brzozowska, M.; Rutkowski, D.; Czech, M.; Tuszyńska, A.; Jacyna, A.; Puzianowska-Kuźnicka, M.; Franek, E. Predictors of in-hospital mortality in nonsurgical departments: A multivariable regression analysis of 2855029 hospitalizations. Pol. Arch. Intern. Med. 2020, 130, 268–275. [Google Scholar] [PubMed]
- Kaya, S.; Sain Guven, G.; Aydan, S.; Toka, O. Predictors of hospital readmissions in internal medicine patients: Application of Andersen’s Model. Int. J. Health Plan. Manag. 2019, 34, 370–383. [Google Scholar] [CrossRef]
- Berry, J.G.; Gay, J.C.; Joynt Maddox, K.; Coleman, E.A.; Bucholz, E.M.; O’Neill, M.R.; Blaine, K.; Hall, M. Age trends in 30 day hospital readmissions: US national retrospective analysis. BMJ 2018, 360, k497. [Google Scholar] [CrossRef] [PubMed]
- Soh, J.G.S.; Wong, W.P.; Mukhopadhyay, A.; Quek, S.C.; Tai, B.C. Predictors of 30-day unplanned hospital readmission among adult patients with diabetes mellitus: A systematic review with meta-analysis. BMJ Open Diabetes Res. Care 2020, 8, e001227. [Google Scholar] [CrossRef]
- Chen, J.Y.; Ma, Q.; Chen, H.; Yermilov, I. New bundled world: Quality of care and readmission in diabetes patients. J. Diabetes Sci. Technol. 2012, 6, 563–571. [Google Scholar] [CrossRef][Green Version]
- Karunakaran, A.; Zhao, H.; Rubin, D.J. Predischarge and postdischarge risk factors for hospital readmission among patients with diabetes. Med. Care 2018, 56, 634–642. [Google Scholar] [CrossRef]
- Rubin, D.J. Correction to: Hospital Readmission of Patients with Diabetes. Curr. Diabetes Rep. 2018, 18, 21. [Google Scholar] [CrossRef] [PubMed]
- Mudge, A.M.; Kasper, K.; Clair, A.; Redfern, H.; Bell, J.J.; Barras, M.A.; Dip, G.; Pachana, N.A. Recurrent readmissions in medical patients: A prospective study. J. Hosp. Med. 2011, 6, 61–67. [Google Scholar] [CrossRef]
- Gregory, N.S.; Seley, J.J.; Dargar, S.K.; Galla, N.; Gerber, L.M.; Lee, J.I. Strategies to prevent readmission in high-risk patients with diabetes: The importance of an interdisciplinary approach. Curr. Diabetes Rep. 2018, 18, 54. [Google Scholar] [CrossRef] [PubMed]
- Kirby, S.E.; Dennis, S.M.; Jayasinghe, U.W.; Harris, M.F. Patient related factors in frequent readmissions: The influence of condition, access to services and patient choice. BMC Health Serv. Res. 2010, 10, 216. [Google Scholar] [CrossRef] [PubMed]
- Alqahtani, J.S.; Njoku, C.M.; Bereznicki, B.; Wimmer, B.C.; Peterson, G.M.; Kinsman, L.; Aldabayan, Y.S.; Alrajeh, A.M.; Aldhahir, A.M.; Mandal, S.; et al. Risk factors for all-cause hospital readmission following exacerbation of COPD: A systematic review and meta-analysis. Eur. Respir. Rev. 2020, 29, 190166. [Google Scholar] [CrossRef]
- Dakour Aridi, H.N.; Locham, S.; Nejim, B.; Ghajar, N.S.; Alshaikh, H.; Malas, M.B. Indications, risk factors, and outcomes of 30-day readmission after infrarenal abdominal aneurysm repair. J. Vasc. Surg. 2018, 67, 747–758.e7. [Google Scholar] [CrossRef]
- Bansal, V.; Mottalib, A.; Pawar, T.K.; Abbasakoor, N.; Chuang, E.; Chaudhry, A.; Sakr, M.; Gabbay, R.A.; Hamdy, O. Inpatient diabetes management by specialized diabetes team versus primary service team in non-critical care units: Impact on 30-day readmission rate and hospital cost. BMJ Open Diabetes Res. Care 2018, 6, e000460. [Google Scholar] [CrossRef] [PubMed]
- Healy, S.J.; Black, D.; Harris, C.; Lorenz, A.; Dungan, K.M. Inpatient diabetes education is associated with less frequent hospital readmission among patients with poor glycemic control. Diabetes Care 2013, 36, 2960–2967. [Google Scholar] [CrossRef]
- Davies, M.; Dixon, S.; Currie, C.J.; Davis, R.E.; Peters, J.R. Evaluation of a hospital diabetes specialist nursing service: A randomized controlled trial. Diabetes Med. 2001, 18, 301–307. [Google Scholar] [CrossRef] [PubMed]
- Wierzba, W.; Śliwczynski, A.; Pinkas, J.; Jawien, A.; Karnafel, W. Diabetes mellitus increases the risk of ruptured abdominal aortic aneurism. Diabetes Vasc. Dis. Res. 2017, 14, 463–464. [Google Scholar] [CrossRef]
- Ram, E.; Sternik, L.; Klempfner, R.; Iakobishvili, Z.; Fisman, E.Z.; Tenenbaum, A.; Zuroff, E.; Peled, Y.; Raanani, E. Type 2 diabetes mellitus increases the mortality risk after acute coronary syndrome treated with coronary artery bypass surgery. Cardiovasc. Diabetol. 2020, 19, 86. [Google Scholar] [CrossRef]
- Holman, N.; Hillson, R.; Young, R.J. Excess mortality during hospital stays among patients with recorded diabetes compared with those without diabetes. Diabetes Med. 2013, 30, 1393–1402. [Google Scholar] [CrossRef]
- Papazafiropoulou, A.; Tentolouris, N.; Bousboulas, S.; Sotiropoulos, A.; Tamvakos, E.; Peppas, T.; Kardara, M.; Pappas, S. In-hospital mortality in a tertiary referral hospital: Causes of death and comparison between patients with and without diabetes. Exp. Clin. Endocrinol. Diabetes 2010, 118, 315–319. [Google Scholar] [CrossRef]
- Mukherjee, T.; Robbins, T.; Lim Choi Keung, S.N.; Sankar, S.; Randeva, H.; Arvanitis, T.N. A systematic review considering risk factors for mortality of patients discharged from hospital with a diagnosis of diabetes. J. Diabetes Complicat. 2020, 34, 107705. [Google Scholar] [CrossRef] [PubMed]
- Tazmini, K.; Nymo, S.H.; Louch, W.E.; Ranhoff, A.H.; Øie, E. Electrolyte imbalances in an unselected population in an emergency department: A retrospective cohort study. PLoS ONE 2019, 14, e0215673. [Google Scholar] [CrossRef]
- Levine, S.K.; Sachs, G.A.; Jin, L.; Meltzer, D. A Prognostic Model for 1-Year Mortality in Older Adults after Hospital Discharge. Am. J. Med. 2007, 120, 455–460. [Google Scholar] [CrossRef]
- Piette, J.D.; Kerr, E.A. The Impact of Comorbid Chronic Conditions on Diabetes Care. Diabetes Care 2006, 29, 725–731. [Google Scholar] [CrossRef]
- Sasso, F.C.; Pafundi, P.C.; Simeon, V.; De Nicola, L.; Chiodini, P.; Galiero, R.; Rinaldi, L.; Nevola, R.; Salvatore, T.; Sardu, C.; et al. Efficacy and durability of multifactorial intervention on mortality and MACEs: A randomized clinical trial in type-2 diabetic kidney disease. Cardiovasc. Diabetol. 2021, 20, 145. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, M.A.; Sidhu, K.S.; Rudge, G.; Stevens, A.J. Weekend admission to hospital has a higher risk of death in the elective setting than in the emergency setting: A retrospective database study of national health service hospitals in England. BMC Health Serv. Res. 2012, 12, 87. [Google Scholar] [CrossRef]
- Freemantle, N.; Ray, D.; McNulty, D.; Rosser, D.; Bennett, S.; Keogh, B.E.; Pagano, D. Increased mortality associated with weekend hospital admission: A case for expanded seven day services? BMJ 2015, 351, h4596. [Google Scholar] [CrossRef] [PubMed]
- López Pardo, P.; Socorro García, A.; Baztán Cortés, J.J. Influence of length of hospital stay on mortality after discharge in older patients with acute medical diseases. Gac. Sanit. 2016, 30, 375–378. [Google Scholar] [CrossRef]
- Sud, M.; Yu, B.; Wijeysundera, H.C.; Austin, P.C.; Ko, D.T.; Braga, J.; Cram, P.; Spertus, J.A.; Domanski, M.; Lee, D.S. Associations between short or long length of stay and 30-day readmission and mortality in hospitalized patients with heart failure. JACC Heart Fail. 2017, 5, 578–588. [Google Scholar] [CrossRef] [PubMed]
- Nikkel, L.E.; Kates, S.L.; Schreck, M.; Maceroli, M.; Mahmood, B.; Elfar, J.C. Length of hospital stay after hip fracture and risk of early mortality after discharge in New York state: Retrospective cohort study. BMJ 2015, 351, h6246. [Google Scholar] [CrossRef] [PubMed]

| Variable. | Description | Reference Group | Definition |
|---|---|---|---|
| Medical History | |||
| ALCO | Diseases related to alcohol abuse | No ALCO | F10, E52, G62.1, I42.6, K29.2, K70.0, K70.3, K70.9, T51, Z50.2, Z71.4, Z72.1 |
| ACDH | Hospitalization due to acute complications of diabetes | Hospitalization not caused by acute complications of diabetes | E10.0, E11.0, E12.1, E13.0, E14.0, E10.1, E11.1, E12.1, E13.1, E14.1 |
| BLA | Anemia due to chronic blood loss | No BLA | D50.0 |
| CACD | Cardiac arrhythmias and conduction disturbances | No CACD | I44.1, I44.2, I44.3, I45.6, I45.9, I47, I48, I49, R00.0, R00.1, R00.8, T82.1, Z45.0, Z95.0 |
| Cancer | Solid tumors without metastases | No cancer and/or metastases | C00, C01, C02, C03, C04, C05, C06, C07, C08, C09, C10, C11, C12, C13, C14, C15, C16, C17, C18, C19, C20, C21, C22, C23, C24, C25, C26, C30, C31, C32, C33, C34, C37, C38, C39, C40, C41, C43, C45, C46, C47, C48, C49, C50, C51. C52, C53, C54, C55, C56, C57, C58, C60, C61, C62, C63, C64, C65, C66, C67, C68, C69, C70, C71, C72, C73, C74, C75, C76, C97 |
| COAG | Coagulation disorders, purpura, and others hemorrhagic diatheses | No COAG | D65, D66, D67, D68, D69.1, D69.3, D69.4, D69.5, D69.6 |
| CD-LRT | Chronic diseases of the lower respiratory tract | No CD-LRT | I27.8, I27.9, J40, J41, J42, J43, J44, J45, J46, J47, J60, J61, J62, J63, J64, J65, J66, J67, J68.4, J70.1, J70.3 |
| DA | Iron deficiency anemia | No DA | D50.8, D50.9, D51, D52, D53 |
| DM-INS | Diabetes and hyperglycemic conditions treated with Insulin | Lack of diabetes and hyperglycemic conditions | Purchase of insulin (at least once) by the patient within a year before hospitalization |
| DM | Diabetes and hyperglycemic conditions treated with medication or controlled by diet | Lack of diabetes and hyperglycemic conditions | Purchase (at least once) by the patient of antidiabetic drugs or test strips in the year prior to hospitalization and, at the same time, not buying insulin within a year before hospitalization |
| DEP | Depression and depressive disorders | No DEP | F20.4, F31.3, F31.4, F31.5, F32, F33, F34.1, F41.2, F43.2 |
| DRUG | Drug use | No DRUG | F11, F12, F13, F14, F15, F16, F18, F19, Z71.5, Z72.2 |
| FED | Fluid, electrolyte and acid-base imbalance | No FED | E22.2, E86, E87 |
| HDM-AC | Hospitalization for acute complications of diabetes within 365 days prior to index admission | No hospitalization due acute complications of diabetes in the annual medical history of the patient | |
| HF | Heart failure | No HF | I09.9, I11.0, I13.0, I13.2, I25.5, I42.0, I42.5, I42.6, I42.7, I42.8, I42.9, I43, I50, P29.0 |
| HIV | Disease caused by Human Immunodeficiency Virus (HIV) | No HIV | B20, B21, B22, B24 |
| HTH | Subclinical and clinical hypothyroidism | No HTH | E00, E01, E02, E03, E89.0 |
| HTC | Complicated or secondary hypertension | No HTC or HTU | I11, I12, I13, I15 |
| HP | Primary hypertension | No HTC or HTP | I10 |
| LD | Liver diseases and their complications | No LD | B18, I85, I86.4, I98.2, K70, K71.1, K71.3, K71.4, K71.5, K71.7, K72, K73, K74, K76.0, K76.2, K76.3, K76.4, |
| LYMP | Malignant tumors of the lymphatic, hematopoietic, and related systems | No LYMP | C81, C82, C83, C84, C85, C88, C96, C90.0, C90.2 |
| META | Metastatic tumors or carcinoma of unknown primary | No cancer and/or metastases | C77, C78, C79, C80 |
| NEU | Other neurological diseases | No NEU | G10, G11, G12, G13, G20, G21, G22, G25.4, G25.5, G31.2, G31.8, G31.9, G32, G35, G36, G37, G40, G41, G93.1, G93.4, R47.0, R56 |
| OBE | Obesity | No OBE | E66 |
| PARAS | Paralytic syndromes | No PTS | G04.1, G11.4, G80.1, G80.2, G81, G82, G83.0, G83.1, G83.2, G83.3, G83.4, G83.9 |
| PCD | Pulmonary circulation disorders | No PCD | I26, I27, I28.0, I28.8, I28.9 |
| PSYCH | Psychotic disorders | No PSYCH | F20, F22, F23, F24, F25, F28, F29, F30.2, F31.2, F31.5 |
| PUD | Peptic ulcers without hemorrhage and perforation | No PUD | K25.7, K25.9, K26.7, K26.9, K27.7, K27.9, K28.7, K28.9 |
| PVD | Peripheral vascular diseases | No PVD | I70, I71, I73.1, I73.8, I73.9, I77.1, I79.0, I79.2, K55.1, K55.8, K55.9, K95.8, Z95.9 |
| RF | Renal failure | No RF | I12.0, I13.1, N18, N19, N25.0, Z49.0, Z49.1, Z49.2, Z94.0, Z99.2 |
| RHEU | Arthropathies and connective tissue diseases | No RHEU | L94.0, L94.1, L94.3, M05, M06, M08, M12.0, M12.3, M30, M31.0, M31.1, M31.2, M31.3, M32, M33, M34, M35, M45, M46.1, M46.8, M46.9 |
| VD | Heart valve defects | No VD | A52.0, I05, I06, I07, I08, I09.1, I09.8, I34, I35, I36, I37, I38, I39, Q23.0, Q23.1, Q23.2, Q23.3, Z95.2, Z95.3, Z95.4 |
| WL | Malnutrition or unintended weight loss | No WL | E40, E41, E42, E43, E44, E45, E46, R63.4, R64 |
| Demographics | |||
| Place of residence | Patient’s place of residence—rural/city | City | |
| MG | Male gender | Female | |
| Hospitalization | |||
| Experience | Experience of the center | Percentage of diabetes hospitalizations carried out by the center relative to all hospitalizations due to diabetes in Poland standardized by a mean and standard deviation | |
| Diab/Endo | A department of diabetes or endocrinology in a center or hospital that has a diabetology or endocrinology service | A facility that does not have a diabetology or endocrinology ward | |
| Diab/Endo Teach | Teaching hospital with diabetology/endocrinology ward and service | A nonteaching facility or no services in the field of diabetology or endocrinology | |
| Teach | Category of hospitalization facility: teaching | A nonteaching facility | |
| LH one_d | Length of hospitalization: one day | Patient was discharged between the 1st and 7th day from the date of admission | Date of the patient’s discharge is the same as the date of admission |
| LH 1–7 d | Length of hospitalization: 1–7 d | Patient was discharged between the 1st and 7th day from the date of admission | |
| LH 8–14 d | Length of hospitalization: 8–14 d | Patient was discharged between the 1st and 7th day from the date of admission | Patient was discharged between the 8th and 14th day from the date of admission |
| LH +14 d | Length of hospitalization: +14 d | Patient was discharged between the 1st and 7th day from the date of admission | Patient was discharged at least 15 days from the date of admission |
| Secondary hospitalization | Secondary hospitalization | Hospitalization is not secondary | |
| WA | Admission on weekend | Admission between Monday and Thursday | Admission on Friday, Saturday, or Sunday |
| Variable | Description | Reference Group |
|---|---|---|
| Demographics | ||
| Age 36–50 | Patient of age 36–50 | Adult patient below the age 36 |
| Age 50+ | Patient over the age 50 | Adult patient below the age 36 |
| Hospitalization | ||
| Emergency | Emergency or urgent mode of admission (emergency—patient was brought by ambulance, urgent—other urgent admissions) | Planned admission |
| Variable | Description | Reference Group |
|---|---|---|
| Demographics | ||
| Age std | Standardized age with the mean (avg = 63.26) and standard deviation (std = 16.78) | |
| Age std sq | Standardized age with the mean (avg = 63.26) and standard deviation (std = 16.78) squared | |
| Hospitalization | ||
| Emergency | Mode of admission (patient brought by ambulance) | Planned admission |
| Urgent | Mode of admission | Planned admission |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kozioł, M.; Towpik, I.; Żurek, M.; Niemczynowicz, J.; Wasążnik, M.; Sanchak, Y.; Wierzba, W.; Franek, E.; Walicka, M. Predictors of Rehospitalization and Mortality in Diabetes-Related Hospital Admissions. J. Clin. Med. 2021, 10, 5814. https://doi.org/10.3390/jcm10245814
Kozioł M, Towpik I, Żurek M, Niemczynowicz J, Wasążnik M, Sanchak Y, Wierzba W, Franek E, Walicka M. Predictors of Rehospitalization and Mortality in Diabetes-Related Hospital Admissions. Journal of Clinical Medicine. 2021; 10(24):5814. https://doi.org/10.3390/jcm10245814
Chicago/Turabian StyleKozioł, Milena, Iwona Towpik, Michał Żurek, Jagoda Niemczynowicz, Małgorzata Wasążnik, Yaroslav Sanchak, Waldemar Wierzba, Edward Franek, and Magdalena Walicka. 2021. "Predictors of Rehospitalization and Mortality in Diabetes-Related Hospital Admissions" Journal of Clinical Medicine 10, no. 24: 5814. https://doi.org/10.3390/jcm10245814
APA StyleKozioł, M., Towpik, I., Żurek, M., Niemczynowicz, J., Wasążnik, M., Sanchak, Y., Wierzba, W., Franek, E., & Walicka, M. (2021). Predictors of Rehospitalization and Mortality in Diabetes-Related Hospital Admissions. Journal of Clinical Medicine, 10(24), 5814. https://doi.org/10.3390/jcm10245814






