When More Means Less: The Prognosis of Recurrent Acute Myocardial Infarctions
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Sources and Classifications
2.3. Study Groups
2.4. Follow-Up and Outcomes
2.5. Statistical Analysis
3. Results
3.1. Study Population and Groups
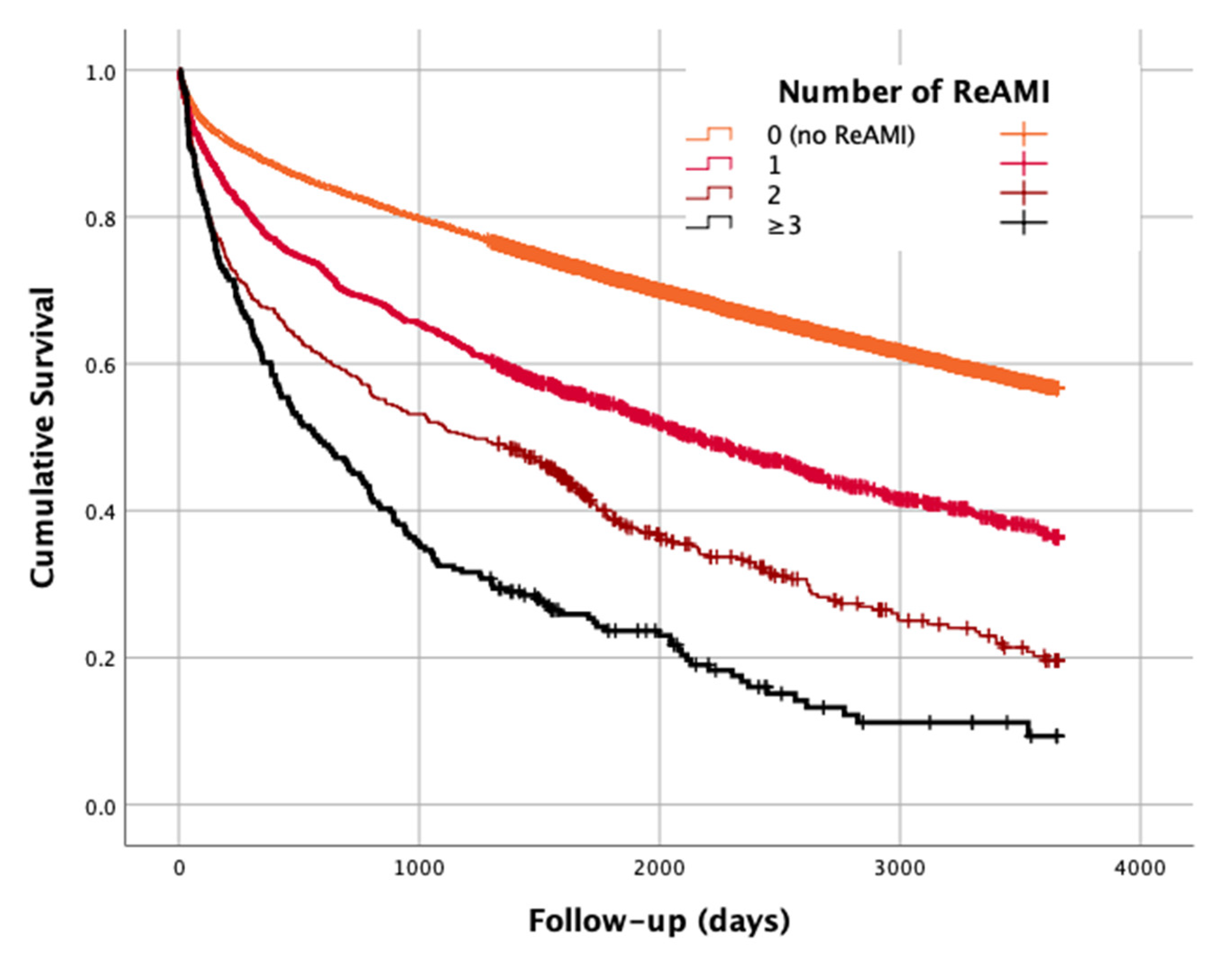
3.2. Follow-Up and Outcomes
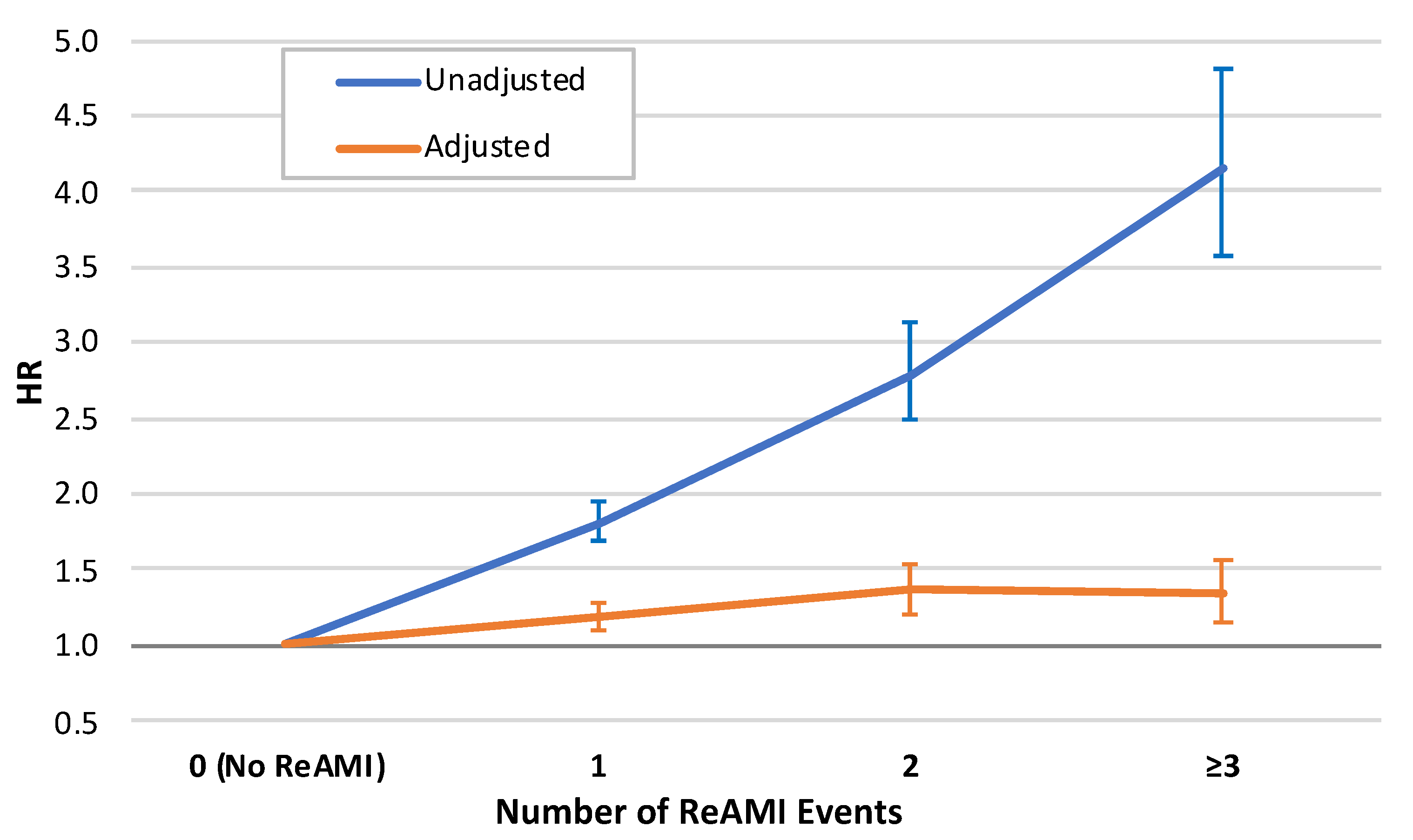
3.3. Multivariable Analysis
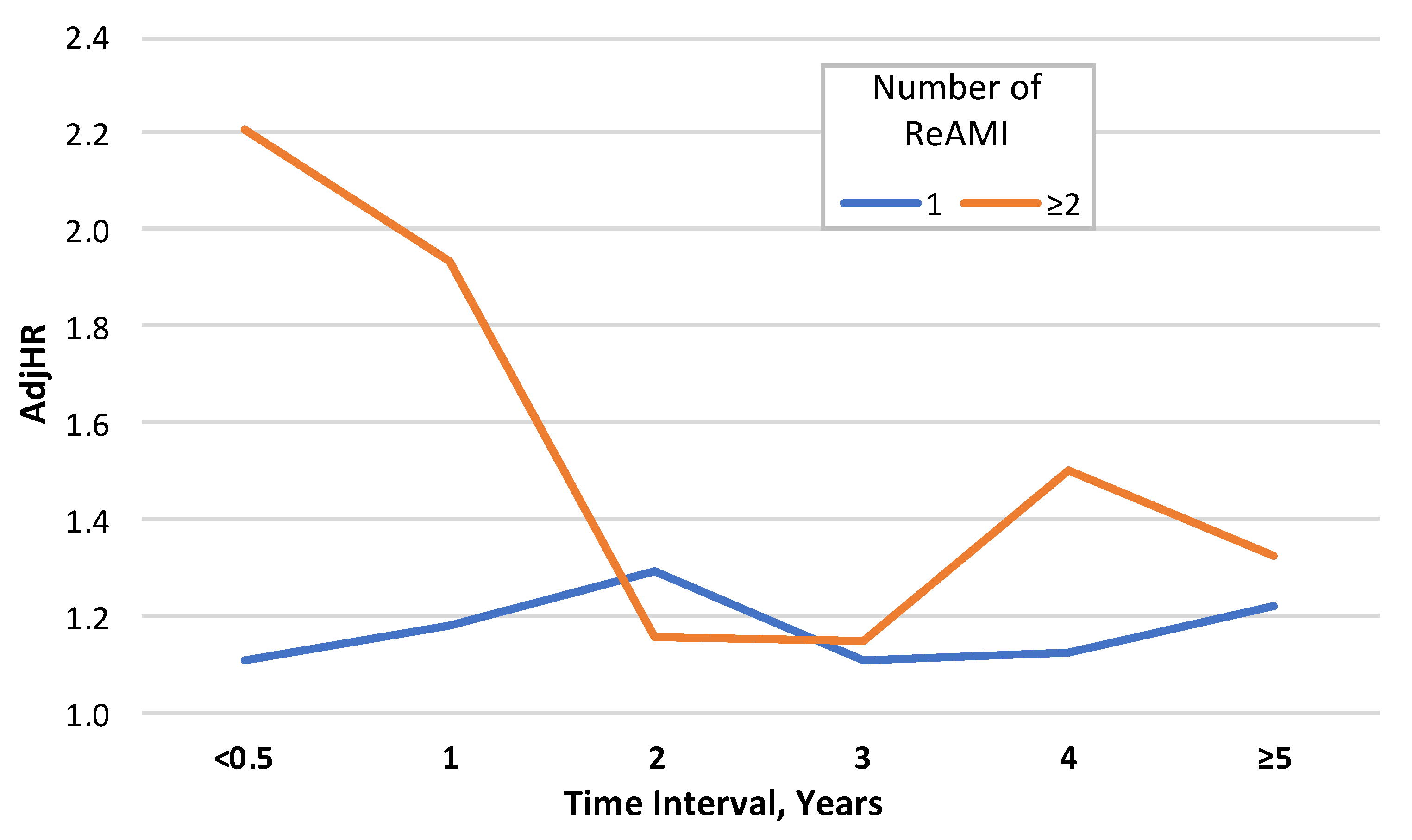
3.4. Sub-Group Analysis
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Peterson, E.D.; Shah, B.R.; Parsons, L.; Pollack, C.V., Jr.; French, W.J.; Canto, J.G.; Gibson, C.M.; Rogers, W.J. Trends in quality of care for patients with acute myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006. Am. Heart J. 2008, 156, 1045–1055. [Google Scholar] [CrossRef]
- Braunwald, E.; Antman, E.M.; Beasley, J.W.; Califf, R.M.; Cheitlin, M.D.; Hochman, J.S.; Jones, R.H.; Kereiakes, D.; Kupersmith, J.; Levin, T.N.; et al. ACC/AHA 2002 guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction—Summary article: A report of the American College of Cardiology/American Heart Association task force on practice guidelines (Committee on the Management of Patients with Unstable Angina). J. Am. Coll. Cardiol. 2002, 40, 1366–1374. [Google Scholar] [CrossRef] [Green Version]
- Kushner, F.G.; Hand, M.; Smith, S.C., Jr.; King, S.B., 3rd; Anderson, J.L.; Antman, E.M.; Bailey, S.R.; Bates, E.R.; Blankenship, J.C.; Casey, D.; et al. 2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2009, 54, 2205–2241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Plakht, Y.; Gilutz, H.; Shiyovich, A. Temporal trends in acute myocardial infarction: What about survival of hospital survivors? Disparities between STEMI & NSTEMI remain. Soroka acute myocardial infarction II (SAMI-II) project. Int. J. Cardiol. 2016, 203, 1073–1081. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Murugiah, K.; Hu, S.; Gao, Y.; Li, X.; Krumholz, H.M.; Zheng, X. Incidence, predictors, and prognostic impact of recurrent acute myocardial infarction in China. Heart 2020, 107, 313–318. [Google Scholar] [CrossRef] [PubMed]
- Stone, S.G.; Serrao, G.W.; Mehran, R.; Tomey, M.I.; Witzenbichler, B.; Guagliumi, G.; Peruga, J.Z.; Brodie, B.R.; Dudek, D.; Möckel, M.; et al. Incidence, predictors, and implications of reinfarction after primary percutaneous coronary intervention in ST-segment-elevation myocardial infarction: The Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction Trial. Circ. Cardiovasc. Interv. 2014, 7, 543–551. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benjamin, E.J.; Muntner, P.; Alonso, A.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Das, S.R.; et al. Heart Disease and Stroke Statistics—2019 Update: A Report From the American Heart Association. Circulation 2019, 139, e56–e528. [Google Scholar] [CrossRef] [PubMed]
- Jernberg, T.; Hasvold, P.; Henriksson, M.; Hjelm, H.; Thuresson, M.; Janzon, M. Cardiovascular risk in post-myocardial infarction patients: Nationwide real world data demonstrate the importance of a long-term perspective. Eur. Heart J. 2015, 36, 1163–1170. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Motivala, A.A.; Tamhane, U.; Ramanath, V.S.; Saab, F.; Montgomery, D.G.; Fang, J.; Kline-Rogers, E.; May, N.; Ng, G.; Froehlich, J.; et al. A prior myocardial infarction: How does it affect management and outcomes in recurrent acute coronary syndromes? Clin. Cardiol. 2008, 31, 590–596. [Google Scholar] [CrossRef]
- Wagner, S.; Burczyk, U.; Schiele, R.; Bergmeier, C.; Rustige, J.; Gottwik, M.; Senges, J. The 60 Minutes Myocardial Infarction Project. Characteristics on admission and clinical outcome in patients with reinfarction compared to patients with a first infarction. Eur. Heart J. 1998, 19, 879–884. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Leifheit, E.; Normand, S.T.; Krumholz, H.M. Association Between Subsequent Hospitalizations and Recurrent Acute Myocardial Infarction within 1 Year after Acute Myocardial Infarction. J. Am. Heart Assoc. 2020, 9, e014907. [Google Scholar] [CrossRef]
- Mendis, S.; Thygesen, K.; Kuulasmaa, K.; Giampaoli, S.; Mähönen, M.; Blackett, K.N.; Lisheng, L.; Writing group on behalf of the participating experts of the WHO consultation for revision of WHO definition of myocardial infarction. World Health Organization definition of myocardial infarction: 2008–09 revision. Int. J. Epidemiol. 2011, 40, 139–146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakatani, D.; Sakata, Y.; Suna, S.; Usami, M.; Matsumoto, S.; Shimizu, M.; Sumitsuji, S.; Kawano, S.; Ueda, Y.; Hamasaki, T.; et al. Incidence, predictors, and subsequent mortality risk of recurrent myocardial infarction in patients following discharge for acute myocardial infarction. Circ. J. 2013, 77, 439–446. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mal, K.; Awan, I.D.; Shaukat, F. Evaluation of Risk Factors Associated with Reinfarction: A Multicenter Observational Study. Cureus 2019, 11, e6063. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Monteiro, A.V.; Ramos, R.; Fiarresga, A.; de Sousa, L.; Cacela, D.; Patrício, L.; Bernardes, L.; Soares, C.; Ferreira, R.C. Timing and long-term prognosis of recurrent MI after primary angioplasty: Stent thrombosis vs. non-stent-related reinfarction. Herz 2017, 42, 186–193. [Google Scholar] [CrossRef] [Green Version]
- Shiyovich, A.; Shlomo, N.; Cohen, T.; Iakobishvili, Z.; Kornowski, R.; Eisen, A. Temporal trends of patients with acute coronary syndrome and multi-vessel coronary artery disease-from the ACSIS registry. Int. J. Cardiol. 2020, 304, 8–13. [Google Scholar] [CrossRef]
- Cao, C.-F.; Li, S.-F.; Chen, H.; Song, J.-X. Predictors and in-hospital prognosis of recurrent acute myocardial infarction. J. Geriatr. Cardiol. 2016, 13, 836–839. [Google Scholar] [CrossRef]
- Nair, R.; Johnson, M.; Kravitz, K.; Huded, C.; Rajeswaran, J.; Anabila, M.; Blackstone, E.; Menon, V.; Lincoff, A.M.; Kapadia, S.; et al. Characteristics and Outcomes of Early Recurrent Myocardial Infarction After Acute Myocardial Infarction. J. Am. Heart Assoc. 2021, 10, e019270. [Google Scholar] [CrossRef] [PubMed]
- Amier, R.P.; Smulders, M.W.; van der Flier, W.M.; Bekkers, S.C.; Zweerink, A.; Allaart, C.P.; Demirkiran, A.; Roos, S.T.; Teunissen, P.; Appelman, Y.; et al. Long-Term Prognostic Implications of Previous Silent Myocardial Infarction in Patients Presenting with Acute Myocardial Infarction. JACC Cardiovasc. Imaging 2018, 11, 1773–1781. [Google Scholar] [CrossRef]
- Bansilal, S.; Castellano, J.M.; Garrido, E.; Wei, H.G.; Freeman, A.; Spettell, C.; Garcia-Alonso, F.; Lizano, I.; Arnold, R.J.; Rajda, J.; et al. Assessing the Impact of Medication Adherence on Long-Term Cardiovascular Outcomes. J. Am. Coll. Cardiol. 2016, 68, 789–801. [Google Scholar] [CrossRef]
- Du, L.; Cheng, Z.; Zhang, Y.; Li, Y.; Mei, D. The impact of medication adherence on clinical outcomes of coronary artery disease: A meta-analysis. Eur. J. Prev. Cardiol. 2017, 24, 962–970. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Song, X.; Raposeiras-Roubín, S.; Abu-Assi, E.; Henriques, J.P.S.; D’Ascenzo, F.; Saucedo, J.; González-Juanatey, J.R.; Wilton, S.B.; Kikkert, W.J.; et al. The impact of optimal medical therapy on patients with recurrent acute myocardial infarction: Subanalysis from the BleeMACS study. Int. J. Cardiol. 2020, 318, 1–6. [Google Scholar] [CrossRef]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.-M.; Capodanno, D.; et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef] [PubMed]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, A.B.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [CrossRef] [PubMed]
- Shiraishi, J.; Kohno, Y.; Sawada, T.; Takeda, M.; Arihara, M.; Hyogo, M.; Yagi, T.; Shima, T.; Okada, T.; Nakamura, T.; et al. Predictors of in-hospital outcome after primary percutaneous coronary intervention for recurrent myocardial infarction. Circ. J. 2008, 72, 1225–1229. [Google Scholar] [CrossRef] [Green Version]
- Gong, F.F.; Vaitenas, I.; Malaisrie, S.C.; Maganti, K. Mechanical Complications of Acute Myocardial Infarction: A Review. JAMA Cardiol. 2021, 6, 341–349. [Google Scholar] [CrossRef]
- Krumholz, H.M. Post-Hospital Syndrome—An Acquired, Transient Condition of Generalized Risk. N. Engl. J. Med. 2013, 368, 100–102. [Google Scholar] [CrossRef] [Green Version]
- Ho, P.M.; Tsai, T.T.; Maddox, T.M.; Powers, J.D.; Carroll, N.M.; Jackevicius, C.; Go, A.S.; Margolis, K.L.; DeFor, T.A.; Rumsfeld, J.S.; et al. Delays in filling clopidogrel prescription after hospital discharge and adverse outcomes after drug-eluting stent implantation: Implications for transitions of care. Circ. Cardiovasc. Qual. Outcomes 2010, 3, 261–266. [Google Scholar] [CrossRef] [Green Version]
- Ong, S.B.; Hernández-Reséndiz, S.; Crespo-Avilan, G.E.; Mukhametshina, R.T.; Kwek, X.Y.; Cabrera-Fuentes, H.A.; Hausenloy, D.J. Inflammation following acute myocardial infarction: Multiple players, dynamic roles, and novel therapeutic opportunities. Pharmacol. Ther. 2018, 186, 73–87. [Google Scholar] [CrossRef] [PubMed]
- Frangogiannis, N.G. The inflammatory response in myocardial injury, repair, and remodelling. Nat. Rev. Cardiol. 2014, 11, 255–265. [Google Scholar] [CrossRef] [Green Version]
| Characteristic | Number of ReAMIs | Total | p-for-Trend | |||
|---|---|---|---|---|---|---|
| 0 | 1 | 2 | ≥3 | |||
| n | 9973 | 1647 | 446 | 231 | 12,297 | |
| Demographics | ||||||
| Age, Mean (SD) | 65.19 (14.10) | 69.18 (13.82) | 70.96 (13.32) | 73.01 (11.99) | 66.08 (14.13) | <0.001 |
| <65 | 5091 (51.0) | 660 (40.1) | 148 (33.2) | 64 (27.7) | 5963 (48.5) | <0.001 |
| 65–75 | 2181 (21.9) | 377 (22.9) | 118 (26.5) | 53 (22.9) | 2729 (22.2) | |
| ≥75 | 2701 (27.1) | 610 (37.0) | 180 (40.4) | 114 (49.4) | 3605 (29.3) | |
| Sex, Males | 6833 (68.5) | 1101 (66.8) | 285 (63.9) | 136 (58.9) | 8355 (67.9) | <0.001 |
| Ethnicity, Minorities | 1884 (18.9) | 348 (21.1) | 104 (23.3) | 54 (23.4) | 2390 (19.4) | 0.001 |
| Cardiac diseases | ||||||
| Cardiomegaly | 762 (7.6) | 271 (16.5) | 123 (27.6) | 86 (37.2) | 1242 (10.1) | <0.001 |
| Supraventricular arrhythmias | 1548 (15.5) | 366 (22.2) | 102 (22.9) | 53 (22.9) | 2069 (16.8) | <0.001 |
| CHF | 1491 (15.0) | 457 (27.7) | 192 (43.0) | 129 (55.8) | 2269 (18.5) | <0.001 |
| Pulmonary heart disease | 784 (7.9) | 270 (16.4) | 117 (26.2) | 85 (36.8) | 1256 (10.2) | <0.001 |
| AV block | 358 (3.6) | 61 (3.7) | 23 (5.2) | 8 (3.5) | 450 (3.7) | 0.321 |
| Cardiovascular risk factors | ||||||
| Renal diseases | 792 (7.9) | 263 (16.0) | 95 (21.3) | 65 (28.1) | 1215 (9.9) | <0.001 |
| Diabetes mellitus | 3796 (38.1) | 872 (52.9) | 270 (60.5) | 166 (71.9) | 5104 (41.5) | <0.001 |
| Dyslipidemia | 8011 (80.3) | 1418 (86.1) | 395 (88.6) | 211 (91.3) | 10,035 (81.6) | <0.001 |
| Hypertension | 5103 (51.2) | 1060 (64.4) | 339 (76.0) | 200 (86.6) | 6702 (54.5) | <0.001 |
| Obesity | 2263 (22.7) | 353 (21.4) | 77 (17.3) | 43 (18.6) | 2736 (22.2) | 0.003 |
| Smoking | 4250 (42.6) | 736 (44.7) | 207 (46.4) | 106 (45.9) | 5299 (43.1) | 0.026 |
| PVD | 960 (9.6) | 259 (15.7) | 89 (20.0) | 60 (26.0) | 1368 (11.1) | <0.001 |
| Family history of IHD | 1008 (10.1) | 172 (10.4) | 33 (7.4) | 13 (5.6) | 1226 (10.0) | 0.027 |
| Other disorders | ||||||
| COPD | 746 (7.5) | 229 (13.9) | 87 (19.5) | 64 (27.7) | 1126 (9.2) | <0.001 |
| Neurological disorders | 1559 (15.6) | 370 (22.5) | 120 (26.9) | 77 (33.3) | 2126 (17.3) | <0.001 |
| Malignancy | 393 (3.9) | 67 (4.1) | 16 (3.6) | 10 (4.3) | 486 (4.0) | 0.924 |
| Anemia | 4080 (40.9) | 815 (49.5) | 250 (56.1) | 134 (58.0) | 5279 (42.9) | <0.001 |
| GI bleeding | 198 (2.0) | 46 (2.8) | 13 (2.9) | 5 (2.2) | 262 (2.1) | 0.066 |
| Schizophrenia/Psychosis | 182 (1.8) | 27 (1.6) | 8 (1.8) | 7 (3.0) | 224 (1.8) | 0.574 |
| Alcohol/drug addiction | 212 (2.1) | 33 (2.0) | 8 (1.8) | 3 (1.3) | 256 (2.1) | 0.341 |
| History of malignancy | 538 (5.4) | 113 (6.9) | 36 (8.1) | 27 (11.7) | 714 (5.8) | <0.001 |
| Clinical characteristics of AMI | ||||||
| Type of AMI, STEMI | 4691 (47.0) | 447 (27.1) | 78 (17.5) | 18 (7.8) | 5234 (42.6) | <0.001 |
| Results of echocardiography | ||||||
| Echocardiography performance | 8004 (80.3) | 950 (57.7) | 236 (52.9) | 106 (45.9) | 9296 (75.6) | <0.001 |
| Severe LV dysfunction | 756 (9.4) | 150 (15.8) | 64 (27.1) | 33 (31.1) | 1003 (10.8) | <0.001 |
| LV hypertrophy | 451 (5.6) | 56 (5.9) | 23 (9.7) | 11 (10.4) | 541 (5.8) | 0.004 |
| Mitral regurgitation | 389 (4.9) | 76 (8.0) | 23 (9.7) | 11 (10.4) | 499 (5.4) | <0.001 |
| Tricuspid regurgitation | 282 (3.5) | 47 (4.9) | 21 (8.9) | 10 (9.4) | 360 (3.9) | <0.001 |
| Pulmonary hypertension | 552 (6.9) | 103 (10.8) | 41 (17.4) | 26 (24.5) | 722 (7.8) | <0.001 |
| Results of angiography | ||||||
| Angiography performance | 7096 (71.2) | 885 (53.7) | 215 (48.2) | 93 (40.3) | 8289 (67.4) | <0.001 |
| Measure of CAD, No or non-significant | 390 (5.5) | 37 (4.2) | 8 (3.7) | 6 (6.5) | 441 (5.3) | <0.001 |
| One vessel | 2122 (29.9) | 185 (20.9) | 32 (14.9) | 12 (12.9) | 2351 (28.4) | |
| Two vessels | 2008 (28.3) | 258 (29.2) | 58 (27.0) | 22 (23.7) | 2346 (28.3) | |
| Three vessels/ LM | 2576 (36.3) | 405 (45.8) | 117 (54.4) | 53 (57.0) | 3151 (38.0) | |
| Type of treatment | ||||||
| Noninvasive | 2523 (25.3) | 658 (40.0) | 208 (46.6) | 132 (57.1) | 3521 (28.6) | <0.001 |
| PCI | 6182 (62.0) | 851 (51.7) | 213 (47.8) | 92 (39.8) | 7338 (59.7) | |
| CABG | 1268 (12.7) | 138 (8.4) | 25 (5.6) | 7 (3.0) | 1438 (11.7) | |
| Parameter | B (SE) | HR | (95% CI) | p |
|---|---|---|---|---|
| Number of AMI Events: | ||||
| 0 (no ReAMI) | 1 (ref.) | |||
| 2 | 0.167 (0.039) | 1.181 | (1.095; 1.274) | <0.001 |
| 3 | 0.309 (0.062) | 1.362 | (1.207; 1.538) | <0.001 |
| ≥3 | 0.290 (0.079) | 1.336 | (1.144; 1.561) | <0.001 |
| Age, Years: | ||||
| >65 | 1 (ref.) | |||
| 65–75 | 0.803 (0.044) | 2.232 | (2.048; 2.434) | <0.001 |
| ≥75 | 1.301 (0.043) | 3.672 | (3.373; 3.998) | <0.001 |
| Sex, Male vs. Female | −0.067 (0.031) | 0.935 | (0.881; 0.992) | 0.027 |
| Cardiomegaly | 0.180 (0.041) | 1.197 | (1.105; 1.297) | <0.001 |
| Supraventricular arrhythmias | 0.203 (0.032) | 1.226 | (1.150; 1.306) | <0.001 |
| CHF | 0.241 (0.033) | 1.273 | (1.194; 1.357) | <0.001 |
| Pulmonary heart disease | 0.094 (0.042) | 1.098 | (1.011; 1.193) | 0.027 |
| Renal diseases | 0.388 (0.038) | 1.474 | (1.367; 1.588) | <0.001 |
| Diabetes mellitus | 0.290 (0.03) | 1.337 | (1.261; 1.417) | <0.001 |
| Dyslipidemia | −0.194 (0.034) | 0.823 | (0.771; 0.880) | <0.001 |
| Hypertension | −0.076 (0.031) | 0.927 | (0.873; 0.984) | 0.013 |
| Obesity | −0.120 (0.037) | 0.887 | (0.824; 0.954) | 0.001 |
| PVD | 0.333 (0.037) | 1.395 | (1.297; 1.501) | <0.001 |
| Family history of IHD | −0.382 (0.093) | 0.682 | (0.569; 0.818) | <0.001 |
| COPD | 0.525 (0.040) | 1.691 | (1.565; 1.827) | <0.001 |
| Neurological disorders | 0.448 (0.032) | 1.564 | (1.470; 1.665) | <0.001 |
| Malignancy | 0.591 (0.055) | 1.806 | (1.621; 2.011) | <0.001 |
| Anemia | 0.295 (0.031) | 1.343 | (1.264; 1.427) | <0.001 |
| GI bleeding | 0.228 (0.077) | 1.256 | (1.080; 1.460) | 0.003 |
| Schizophrenia/Psychosis | 0.435 (0.082) | 1.546 | (1.316; 1.816) | <0.001 |
| Alcohol/drug addiction | 0.550 (0.095) | 1.734 | (1.439; 2.088) | <0.001 |
| Type of AMI: STEMI vs. NSTEMI | −0.148 (0.034) | 0.863 | (0.807; 0.922) | <0.001 |
| LOS: >7 days vs. ≤7 days | 0.161 (0.031) | 1.174 | (1.105; 1.247) | <0.001 |
| Type of treatment: | ||||
| Noninvasive | 1 (ref.) | |||
| PCI | −0.661 (0.035) | 0.517 | (0.482; 0.553) | <0.001 |
| CABG | −1.055 (0.062) | 0.348 | (0.308; 0.393) | <0.001 |
| Severe LV dysfunction | 0.422 (0.048) | 1.526 | (1.389; 1.676) | <0.001 |
| LV hypertrophy | 0.189 (0.064) | 1.208 | (1.067; 1.368) | 0.003 |
| Mitral regurgitation | 0.223 (0.060) | 1.250 | (1.112; 1.405) | <0.001 |
| Pulmonary hypertension | 0.219 (0.055) | 1.244 | (1.118; 1.385) | <0.001 |
| Year of the index event (one year increase) | −0.013 (0.004) | 0.987 | (0.980; 0.994) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Plakht, Y.; Gilutz, H.; Shiyovich, A. When More Means Less: The Prognosis of Recurrent Acute Myocardial Infarctions. J. Clin. Med. 2021, 10, 5889. https://doi.org/10.3390/jcm10245889
Plakht Y, Gilutz H, Shiyovich A. When More Means Less: The Prognosis of Recurrent Acute Myocardial Infarctions. Journal of Clinical Medicine. 2021; 10(24):5889. https://doi.org/10.3390/jcm10245889
Chicago/Turabian StylePlakht, Ygal, Harel Gilutz, and Arthur Shiyovich. 2021. "When More Means Less: The Prognosis of Recurrent Acute Myocardial Infarctions" Journal of Clinical Medicine 10, no. 24: 5889. https://doi.org/10.3390/jcm10245889






