Electrocardiographic Predictors of Primary Ventricular Fibrillation and 30-Day Mortality in Patients Presenting with ST-Segment Elevation Myocardial Infarction
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Alahmar, A.E.; Nelson, C.P.; Snell, K.I.; Yuyun, M.F.; Musameh, M.D.; Timmis, A.; Birkhead, J.S.; Chugh, S.S.; Thompson, J.R.; Squire, I.B.; et al. Resuscitated cardiac arrest and prognosis following myocardial infarction. Heart 2014, 100, 1125–1132. [Google Scholar] [PubMed]
- Kosmidou, I.; Embacher, M.; McAndrew, T.; Dizon, J.M.; Mehran, R.; Ben-Yehuda, O.; Mintz, G.S.; Stone, G.W. Early Ventricular Tachycardia or Fibrillation in Patients with ST Elevation Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention and Impact on Mortality and Stent Thrombosis (from the Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction Trial). Am. J. Cardiol. 2017, 120, 1755–1760. [Google Scholar] [PubMed]
- Mehta, R.H.; Starr, A.Z.; Lopes, R.D.; Hochman, J.S.; Widimsky, P.; Pieper, K.S.; Armstrong, P.W.; Granger, C.B. APEX AMI Investigators. Incidence of and outcomes associated with ventricular tachycardia or fibrillation in patients undergoing primary percutaneous coronary intervention. JAMA 2009, 301, 1779–1789. [Google Scholar] [CrossRef] [Green Version]
- Lawrie, D.M.; Higgins, M.R.; Godman, M.J.; Oliver, M.F.; Julian, D.G.; Donald, K.W. Ventricular fibrillation complicating acute myocardial infarction. Lancet 1968, 2, 523–528. [Google Scholar] [CrossRef]
- Volpi, A.; Cavalli, A.; Santoro, L.; Negri, E. Incidence and prognosis of early primary ventricular fibrillation in acute myocardial infarction—Results of the Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto Miocardico (GISSI-2) database. Am. J. Cardiol. 1998, 82, 265–271. [Google Scholar] [CrossRef]
- Thompson, C.A.; Yarzebski, J.; Goldberg, R.J.; Lessard, D.; Gore, J.M.; Dalen, J.E. Changes over time in the incidence and case-fatality rates of primary ventricular fibrillation complicating acute myocardial infarction: Perspectives from the Worcester Heart Attack Study. Am. Heart J. 2000, 139, 1014–1021. [Google Scholar] [CrossRef] [PubMed]
- Balci, B.; Yesildag, O. Correlation between clinical findings and the tombstoning electrocardiographic pattern in patients with anterior wall acute myocardial infarction. Am. J. Cardiol 2003, 92, 1316–1318. [Google Scholar] [CrossRef] [PubMed]
- Kukla, P.; Jastrzebski, M.; Sacha, J.; Bryniarski, L. Segment elevation in acute myocardial infarction: A new risk marker for ventricular fibrillation? Three case reports. Kardiol. Polska 2008, 66, 873–877. [Google Scholar]
- Aizawa, Y.; Jastrzebski, M.; Ozawa, T.; Kawecka-Jaszcz, K.; Kukla, P.; Mitsuma, W.; Chinushi, M.; Ida, T.; Aizawa, Y.; Ojima, K.; et al. Characteristics of electrocardiographic repolarization in acute myocardial infarction complicated by ventricular fibrillation. J. Electrocardiol. 2012, 45, 252–259. [Google Scholar] [CrossRef]
- Cipriani, A.; D’Amico, G.; Brunello, G.; Perazzolo Marra, M.; Migliore, F.; Cacciavillani, L.; Tarantini, G.; Bauce, B.; Iliceto, S.; Corrado, D.; et al. The electrocardiographic “triangular QRS-ST-T waveform” pattern in patients with ST-segment elevation myocardial infarction: Incidence, pathophysiology and clinical implications. J. Electrocardiol. 2018, 51, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Madias, J.E.; Krikelis, E.N. Transient giant R waves in the early phase of acute myocardial infarction: Association with ventricular fibrillation. Clin. Cardiol. 1981, 4, 339–349. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steg, P.G.; James, S.K.; Atar, D.; Badano, L.P.; Blömstrom-Lundqvist, C.; Borger, M.A.; Di Mario, C.; Dickstein, K.; Ducrocq, G.; Fernandez-Aviles, F.; et al. ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur. Heart J. 2012, 33, 2569–2619. [Google Scholar] [CrossRef] [PubMed]
- Wimalaratna, H.S.K. “Tombstoning” of ST segment in acute myocardial infarction (letter). Lancet 1993, 342, 496. [Google Scholar] [CrossRef]
- Eagle, K.A.; Lim, M.J.; Dabbous, O.H.; Pieper, K.S.; Goldberg, R.J.; Van de Werf, F.; Goodman, S.G.; Granger, C.B.; Steg, P.G.; Gore, J.M.; et al. A validated prediction model for all forms of acute coronary syndrome: Estimating the risk of 6-month postdischarge death in an international registry. JAMA 2004, 291, 2727–2733. [Google Scholar] [CrossRef] [PubMed]
- Zimetbaum, P.J.; Josephson, M.E. Use of the electrocardiogram in acute myocardial infarction. N. Engl. J. Med. 2003, 348, 933–940. [Google Scholar] [CrossRef] [Green Version]
- Yan, G.X.; Antzelevitch, C. Cellular basis for the Brugada syndrome and other mechanisms of arrhythmogenesis associated with ST-segment elevation. Circulation 1999, 100, 1660–1666. [Google Scholar] [CrossRef] [PubMed]
- Fish, J.M.; Antzelevitch, C. Brugada syndrome and ischemia-induced ST-segment elevation. Similarities and differences. J. Electrocardiol. 2005, 38, 14–17. [Google Scholar]
- Kosugi, S.; Shinouchi, K.; Ueda, Y.; Abe, H.; Sogabe, T.; Ishida, K.; Mishima, T.; Ozaki, T.; Takayasu, K.; Iida, Y.; et al. Clinical and Angiographic Features of Patients with Out-of-Hospital Cardiac Arrest and Acute Myocardial Infarction. J. Am. Coll Cardiol. 2020, 76, 1934–1943. [Google Scholar] [CrossRef]
- Gheeraert, P.J.; De Buyzere, M.L.; Taeymans, Y.M.; Gillebert, T.C.; Henriques, J.P.; De Backer, G.; De Bacquer, D. Risk factors for primary ventricular fibrillation during acute myocardial infarction: A systematic review and meta-analysis. Eur. Heart J. 2006, 27, 2499–2510. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jabbari, R.; Engstrøm, T.; Glinge, C.; Risgaard, B.; Jabbari, J.; Winkel, B.G.; Terkelsen, C.J.; Tilsted, H.H.; Jensen, L.O.; Hougaard, M.; et al. Incidence and risk factors of ventricular fibrillation before primary angioplasty in patients with first ST-elevation myocardial infarction: A nationwide study in Denmark. J. Am. Heart Assoc. 2015, 4, e001399. [Google Scholar] [CrossRef] [Green Version]
- Gheeraert, P.J.; Henriques, J.P.; De Buyzere, M.L.; Voet, J.; Calle, P.; Taeymans, Y.; Zijlstra, F. Out-of-hospital ventricular fibrillation in patients with acute myocardial infarction: Coronary angiographic determinants. J. Am. Coll. Cardiol. 2000, 35, 144–150. [Google Scholar] [CrossRef] [Green Version]
- Schwartz, P.J. Cardiac sympathetic denervation to prevent life-threatening arrhythmias. Nat. Rev. Cardiol. 2014, 11, 346–353. [Google Scholar] [CrossRef]
- Janse, M.J.; Schwartz, P.J.; Wilms-Schopman, F.; Peters, R.J.; Durrer, D. Effects of unilateral stellate ganglion stimulation and ablation on electrophysiologic changes induced by acute myocardial ischemia in dogs. Circulation 1985, 7, 585–595. [Google Scholar] [CrossRef] [Green Version]
- Saia, F.; Marrozzini, C.; Ortolani, P.; Palmerini, T.; Guastaroba, P.; Cortesi, P.; Pavesi, P.C.; Gordini, G.; Pancaldi, L.G.; Taglieri, N.; et al. Optimisation of therapeutic strategies for ST-segment elevation acute myocardial infarction: The impact of a territorial network on reperfusion therapy and mortality. Heart 2009, 95, 370–376. [Google Scholar]
- Ravn Jacobsen, M.; Jabbari, R.; Glinge, C.; Kjær Stampe, N.; Butt, J.H.; Blanche, P.; Lønborg, J.; Wendelboe Nielsen, O.; Køber, L.; Torp-Pedersen, C.; et al. Potassium Disturbances and Risk of Ventricular Fibrillation Among Patients With ST-Segment-Elevation Myocardial Infarction. J. Am. Heart Assoc. 2020, 9, e014160. [Google Scholar] [CrossRef]
- Seghieri, C.; Mimmi, S.; Lenzi, J.; Fantini, M.P. 30-day in-hospital mortality after acute myocardial infarction in Tuscany (Italy): An observational study using hospital discharge data. BMC Med. Res. Methodol. 2012, 12, 170. [Google Scholar] [CrossRef] [Green Version]
- Yeh, R.W.; Sidney, S.; Chandra, M.; Sorel, M.; Selby, J.V.; Go, A.S. Population trends in the incidence and outcomes of acute myocardial infarction. N. Engl. J. Med. 2010, 362, 2155–2165. [Google Scholar] [CrossRef] [PubMed]
- Krumholz, H.M.; Wang, Y.; Chen, J.; Drye, E.E.; Spertus, J.A.; Ross, J.S.; Curtis, J.P.; Nallamothu, B.K.; Lichtman, J.H.; Havranek, E.P.; et al. Reduction in acute myocardial infarction mortality in the United States: Risk-standardized mortality rates from 1995–2006. JAMA 2009, 302, 767–773. [Google Scholar]
- Jernberg, T.; Johanson, P.; Held, C.; Svennblad, B.; Lindbäck, J.; Wallentin, L.; SWEDEHEART/RIKS-HIA. Association between adoption of evidence-based treatment and survival for patients with ST-elevation myocardial infarction. JAMA 2011, 305, 1677–1684. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gale, C.P.; Cattle, B.A.; Moore, J.; Dawe, H.; Greenwood, D.C.; West, R.M. Impact of missing data on standardised mortality ratios for acute myocardial infarction: Evidence from the Myocardial Ischaemia National Audit Project (MINAP) 2004–2007. Heart 2011, 97, 1926–1931. [Google Scholar] [CrossRef] [PubMed]
- Ng, V.G.; Lansky, A.J.; Meller, S.; Witzenbichler, B.; Guagliumi, G.; Peruga, J.Z.; Brodie, B.; Shah, R.; Mehran, R.; Stone, G.W. The prognostic importance of left ventricular function in patients with ST-segment elevation myocardial infarction: The Horizons-AMI trial. Eur. Heart J. Acute Cardiovasc. Care 2014, 3, 67–77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Study Population (n = 407) | |
|---|---|
| Male sex | 307 (75) |
| Age, years | 66 (56–75) |
| FMC to PCI, min | 101 (55–120) |
| Primary PCI | 346 (85) |
| Medical history | |
| Arterial hypertension | 261 (64) |
| Dyslipidemia | 176 (43) |
| Diabetes mellitus | 75 (18) |
| Familiar CAD | 153 (38) |
| Smoke | 139 (34) |
| Previous AMI | 35 (9) |
| CKD | 36 (9) |
| Severe COPD | 13 (3) |
| ECG at first medical contact | |
| Anterior STEMI (V1–V4) | 189 (46) |
| Anterior (V1–V4) and lateral (V5- V5–V6, I, aVL V6, I, aVL) | 23 (6) |
| Lateral (V5–V6, I, aVL) | 14 (3) |
| Inferior (II/aVF/III) | 117 (29) |
| Inferior (II/aVF/III) and lateral (V5–V6, I, aVL) | 59 (14) |
| Posterior | 5 (1) |
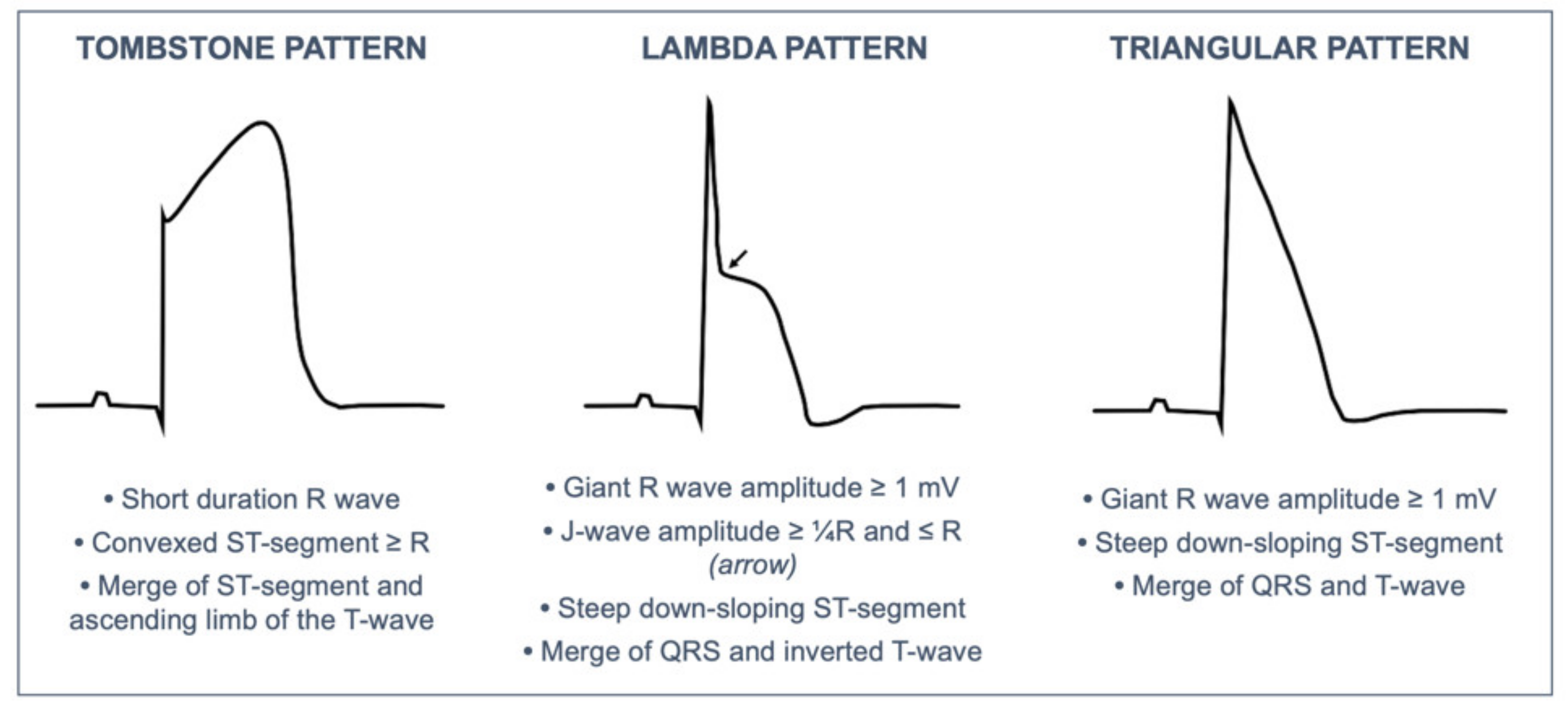
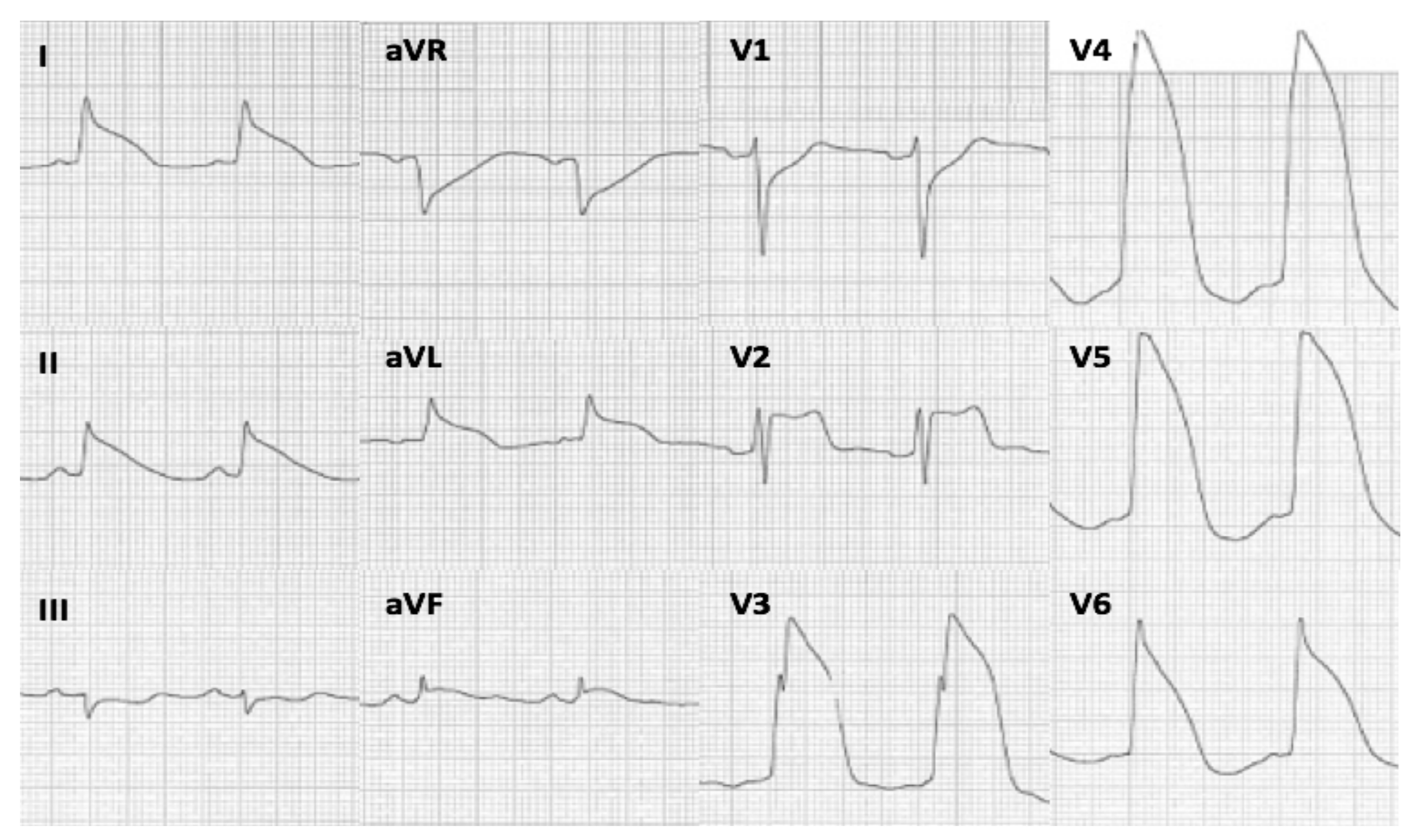
| Tombstone pattern | 45 (11) |
| Triangular-Lambda pattern | 14 (3) |
| R-wave ≥ 1.0 mV | 125 (31) |
| Culprit coronary vessel | |
| Left main | 21 (5) |
| LAD | 197 (48) |
| Left circumflex | 52 (13) |
| Ramus intermedius | 3 (1) |
| Right coronary | 134 (33) |
| Clinical variables | |
| LVEF, % | 47 (40–55) |
| GFR, mL/min/1.73 m2 | 75 (61–90) |
| Killip class ≥ III | 24 (6) |
| Peak Troponin I, ug/L | 70 (26–150) |
| Events | |
| PVF | 39 (10) |
| 30-day mortality | 28 (7) |
| No PVF n = 368 (90%) | PVF n = 39 (10%) | p Value | |
|---|---|---|---|
| Anamnestic and clinical variables | |||
| Age, years | 65.4 (52.1, 78.5) | 61.2 (50.2, 73.3) | 0.033 * |
| Sex, male | 273 (74.2) | 34 (87.2) | 0.073 |
| Arterial hypertension | 236 (64.1) | 25 (64.1) | 0.563 |
| Dyslipidemia | 157 (42.7) | 17 (43.6) | 0.288 |
| Diabetes mellitus | 68 (18.5) | 7 (17.9) | 0.569 |
| Familiar CAD | 141 (38.3) | 12 (30.8) | 0.228 |
| Smoking | 122 (33.2) | 17 (43.6) | 0.130 |
| Severe COPD | 12 (3.3) | 1 (2.6) | 0.641 |
| CKD | 33 (9.0) | 3 (7.7) | 0.539 |
| Previous AMI | 30 (8.2) | 5 (12.8) | 0.234 |
| Killip class ≥3 | 15 (4.1) | 9 (23.1) | <0.001 * |
| ECG variables | |||
| New onset AF | 24 (6.5) | 5 (12.8) | 0.132 |
| Advanced AV block | 11 (3.0) | 1 (2.6) | 0.678 |
| Anterior STEMI | 163 (44.3) | 25 (64.1) | 0.014 * |
| Lateral STEMI | 21 (5.7) | 2 (5.1) | 0.238 |
| Inferior STEMI | 108 (29.3) | 9 (23.1) | 0.267 |
| Posterior STEMI | 5 (1.4) | 0 (0) | - |
| Tombstone pattern | 38 (10.3) | 7 (17.9) | 0.175 |
| Triangular-Lambda pattern | 7 (1.9) | 7 (17.9) | <0.001 * |
| Giant R wave | 107 (29.1) | 18 (46.2) | 0.024 * |
| Primary Ventricular Fibrillation | Univariate Logistic Regression | Multivariate Logistic Regression | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| Age | 0.74 | 0.57, 0.97 | 0.030 | |||
| Arterial hypertension | 0.99 | 0.50, 1.99 | 0.997 | |||
| Diabetes Mellitus | 0.76 | 0.41, 2.28 | 0.935 | |||
| Killip class ≥ 3 | 7.06 | 2.85, 17.50 | <0.001 | 6.19 | 2.37, 16.1 | 0.035 |
| Anterior STEMI | 2.26 | 1.15, 4.59 | 0.021 | |||
| Triangular-Lambda wave | 11.3 | 3.72, 34.2 | <0.001 | 9.64 | 2.99, 31.0 | 0.027 |
| R-wave ≥ 1.0 mV | 2.09 | 1.06, 4.08 | 0.030 | |||
| Alive n = 379 (93%) | Dead n = 28 (7%) | p Value | |
|---|---|---|---|
| Anamnestic variables | |||
| Age, years | 64.6 (51.4, 79.1) | 70.1 (56.7, 83.2) | 0.043 * |
| Male sex | 284 (74.9) | 23 (82.1) | 0.273 |
| Arterial hypertension | 238 (62.8) | 23 (82.1) | 0.028 * |
| Dyslipidemia | 168 (44.3) | 8 (28.6) | 0.075 |
| Diabetes mellitus | 66 (17.4) | 9 (32.1) | 0.073 |
| Familiar CAD | 148 (39.1) | 5 (17.9) | 0.180 |
| Smoking | 129 (34.0) | 10 (35.7) | 0.503 |
| Previous AMI | 34 (9.0) | 1 (3.6) | 0.283 |
| CKD | 32 (8.4) | 4 (14.3) | 0.227 |
| Severe COPD | 10 (2.6) | 3 (10.7) | 0.052 |
| Clinical and instrumental variables | |||
| Killip class ≥3 | 15 (4.0) | 9 (32.1) | <0.001 * |
| Grace score | 140 (18, 210) | 191 (60, 250) | <0.001 * |
| GFR mL/min/1.73 m2 | 81 (62, 90) | 45 (36, 75) | <0.001 * |
| Peak Troponin I, ug/L | 67.2 (1, 579) | 115 (22, 400) | 0.005 * |
| Delayed FMC-PCI > 120 min | 39 (10.3) | 5 (17.9) | 0.283 |
| Culprit lesion | |||
| Left main | 16 (4.7) | 4 (22.2) | 0.013 * |
| LAD | 181 (52.6) | 11 (61.1) | 0.324 |
| Left Circumflex | 45 (13.1) | 5 (27.8) | 0.086 |
| RCA | 127 (36.9) | 3 (16.7) | 0.063 |
| Ramus Intermedius | 2 (0.6) | 1 (5.6) | 0.142 |
| EF (%) | 49 (20, 71) | 26.5 (9, 54) | <0.001 * |
| Tombstone pattern | 40 (10.6) | 5 (17.9) | 0.218 |
| Triangular-Lambda pattern | 8 (2.1) | 6 (21.4) | <0.001 * |
| Giant R wave | 114 (30.1) | 11 (39.3) | 0.208 |
| PVF | 31 (8.2) | 8 (28.6) | 0.003 * |
| AF | 24 (6.3) | 5 (17.9) | 0.054 |
| Advanced AV block | 10 (2.6) | 2 (7.1) | 0.197 |
| 30 Days Death | Univariate Logistic Regression | Multivariate Logistic Regression | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| Age | 1.03 | 1.00, 1.07 | 0.036 * | |||
| Arterial hypertension | 2.73 | 1.01, 7.33 | 0.047 * | |||
| Grace score | 1.03 | 1.02, 1.04 | <0.001 * | |||
| Killip class ≥3 | 11.5 | 4.46, 29.6 | <0.001 * | |||
| GFR | 0.96 | 0.94, 0.97 | <0.001 * | |||
| LVEF | 0.86 | 0.82, 0.90 | <0.001 * | 0.86 | 0.82, 0.90 | <0.001 * |
| Peak Troponin I | 1.02 | 1.01, 1.08 | 0.012 * | |||
| PVF | 4.49 | 1.63, 11.0 | 0.001 * | 4.61 | 1.49, 14.3 | 0.042 * |
| Triangular/Lambda pattern | 12.6 | 4.03, 39.6 | <0.001 * | |||
| Effect | Estimate | 95% CI | p | % Mediation |
|---|---|---|---|---|
| Indirect | 0.063 | −0.013, 0.140 | 0.108 | 17.0 |
| Direct | 0.305 | 0.058, 0.590 | 0.016 * | 83.0 |
| Total | 0.369 | 0.088, 0.650 | 0.008 * | 100.0 |
| Effect | Estimate | 95% CI | p | % Mediation |
|---|---|---|---|---|
| Indirect | 0.235 | 0.113, 0.350 | <0.001 | 62.7 |
| Direct | 0.139 | −0.039, 0.360 | 0.112 | 37.3 |
| Total | 0.374 | 0.114, 0.640 | 0.008 * | 100.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cipriani, A.; D’Amico, G.; Brunetti, G.; Vescovo, G.M.; Donato, F.; Gambato, M.; Dall’Aglio, P.B.; Cardaioli, F.; Previato, M.; Martini, N.; et al. Electrocardiographic Predictors of Primary Ventricular Fibrillation and 30-Day Mortality in Patients Presenting with ST-Segment Elevation Myocardial Infarction. J. Clin. Med. 2021, 10, 5933. https://doi.org/10.3390/jcm10245933
Cipriani A, D’Amico G, Brunetti G, Vescovo GM, Donato F, Gambato M, Dall’Aglio PB, Cardaioli F, Previato M, Martini N, et al. Electrocardiographic Predictors of Primary Ventricular Fibrillation and 30-Day Mortality in Patients Presenting with ST-Segment Elevation Myocardial Infarction. Journal of Clinical Medicine. 2021; 10(24):5933. https://doi.org/10.3390/jcm10245933
Chicago/Turabian StyleCipriani, Alberto, Gianpiero D’Amico, Giulia Brunetti, Giovanni Maria Vescovo, Filippo Donato, Marco Gambato, Pietro Bernardo Dall’Aglio, Francesco Cardaioli, Martina Previato, Nicolò Martini, and et al. 2021. "Electrocardiographic Predictors of Primary Ventricular Fibrillation and 30-Day Mortality in Patients Presenting with ST-Segment Elevation Myocardial Infarction" Journal of Clinical Medicine 10, no. 24: 5933. https://doi.org/10.3390/jcm10245933
APA StyleCipriani, A., D’Amico, G., Brunetti, G., Vescovo, G. M., Donato, F., Gambato, M., Dall’Aglio, P. B., Cardaioli, F., Previato, M., Martini, N., Perazzolo Marra, M., Iliceto, S., Cacciavillani, L., Corrado, D., & Zorzi, A. (2021). Electrocardiographic Predictors of Primary Ventricular Fibrillation and 30-Day Mortality in Patients Presenting with ST-Segment Elevation Myocardial Infarction. Journal of Clinical Medicine, 10(24), 5933. https://doi.org/10.3390/jcm10245933







