Comparison of Intramedullary Magnetic Nail, Monolateral External Distractor, and Spatial External Fixator in Femur Lengthening in Adolescents with Congenital Diseases
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Guichet, J.M.; Spivak, J.M.; Trouilloud, P.; Grammont, P.M. Lower limb-length discrepancy. An epidemiologic study. Clin. Orthop. Relat. Res. 1991, 272, 235–241. [Google Scholar]
- Drnach, M.; Kreger, A.; Corliss, C.; Kocher, D. Limb length discrepancies among 8- to 12-year-old children who are developing typically. Pediatr. Phys. Ther. 2012, 24, 334–337. [Google Scholar] [CrossRef]
- Gross, R.H. Leg length discrepancy: How much is too much? Orthopedics 1978, 1, 307–310. [Google Scholar] [CrossRef] [PubMed]
- Knutson, G.A. Anatomic and functional leg-length inequality: A review and recommendation for clinical decision-making. Part I, anatomic leg-length inequality: Prevalence, magnitude, effects and clinical significance. Chiropr. Osteopat. 2005, 13, 11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hasler, C.C.; Krieg, A.H. Current concepts of leg lengthening. J. Child Orthop. 2012, 6, 89–104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hosny, G.A. Limb lengthening history, evolution, complications and current concepts. J. Orthop. Traumatol. 2020, 21, 3. [Google Scholar] [CrossRef] [PubMed]
- Sabharwal, S.; Green, S.; McCarthy, J.; Hamdy, R.C. What’s New in Limb Lengthening and Deformity Correction. J. Bone Jt. Surg. Am. 2011, 93, 213–221. [Google Scholar] [CrossRef]
- Salcedo Canovas, C. Bone elongation using monolateral external fixation: A practical guide. Strateg. Trauma Limb Reconstr. 2015, 10, 175–188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Szymczuk, V.L.; Hammouda, A.I.; Gesheff, M.G.; Standard, S.C.; Herzenberg, J.E. Lengthening With Monolateral External Fixation Versus Magnetically Motorized Intramedullary Nail in Congenital Femoral Deficiency. J. Pediatr. Orthop. 2019, 39, 458–465. [Google Scholar] [CrossRef] [PubMed]
- Black, S.R.; Kwon, M.S.; Cherkashin, A.M.; Samchukov, M.L.; Birch, J.G.; Jo, C.H. Lengthening in Congenital Femoral Deficiency: A Comparison of Circular External Fixation and a Motorized Intramedullary Nail. J. Bone Jt. Surg. Am. 2015, 97, 1432–1440. [Google Scholar] [CrossRef] [Green Version]
- Donnan, L.T.; Gomes, B.; Donnan, A.; Harris, C.; Torode, I.; Heidt, C. Ilizarov tibial lengthening in the skeletally immature patient. Bone Jt. J. 2016, 98, 1276–1282. [Google Scholar] [CrossRef] [PubMed]
- Marangoz, S.; Feldman, D.S.; Sala, D.A.; Hyman, J.E.; Vitale, M.G. Femoral deformity correction in children and young adults using Taylor Spatial Frame. Clin. Orthop. Relat. Res. 2008, 466, 3018–3024. [Google Scholar] [CrossRef] [Green Version]
- Dahl, M.T.; Morrison, S.G.; Laine, J.C.; Novotny, S.A.; Georgiadis, A.G. Extramedullary Motorized Lengthening of the Femur in Young Children. J. Pediatr. Orthop. 2020, 40, e978–e983. [Google Scholar] [CrossRef] [PubMed]
- Paley, D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin. Orthop. Relat. Res. 1990, 81–104. [Google Scholar] [CrossRef]
- Paley, D.; Herzenberg, J.E.; Paremain, G.; Bhave, A. Femoral lengthening over an intramedullary nail. A matched-case comparison with Ilizarov femoral lengthening. J. Bone Jt. Surg. Am. 1997, 79, 1464–1480. [Google Scholar] [CrossRef]
- Kristiansen, L.P.; Steen, H. Lengthening of the tibia over an intramedullary nail, using the Ilizarov external fixator. Major complications and slow consolidation in 9 lengthenings. Acta Orthop. Scand. 1999, 70, 271–274. [Google Scholar] [CrossRef] [PubMed]
- Schiedel, F.M.; Vogt, B.; Tretow, H.L.; Schuhknecht, B.; Gosheger, G.; Horter, M.J.; Rodl, R. How precise is the PRECICE compared to the ISKD in intramedullary limb lengthening? Reliability and safety in 26 procedures. Acta Orthop. 2014, 85, 293–298. [Google Scholar] [CrossRef] [PubMed]
- Teulieres, M.; Langlais, T.; de Gauzy, J.S.; Rolfing, J.D.; Accadbled, F. Bone Lengthening with a Motorized Intramedullary Nail in 34 Patients with Posttraumatic Limb Length Discrepancies. J. Clin. Med. 2021, 10, 2393. [Google Scholar] [CrossRef]
- Calder, P.R.; McKay, J.E.; Timms, A.J.; Roskrow, T.; Fugazzotto, S.; Edel, P.; Goodier, W.D. Femoral lengthening using the Precice intramedullary limb-lengthening system: Outcome comparison following antegrade and retrograde nails. Bone Jt. J. 2019, 101, 1168–1176. [Google Scholar] [CrossRef] [PubMed]
- Khamis, S.; Carmeli, E. The effect of simulated leg length discrepancy on lower limb biomechanics during gait. Gait Posture 2018, 61, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Gurney, B.; Mermier, C.; Robergs, R.; Gibson, A.; Rivero, D. Effects of limb-length discrepancy on gait economy and lower-extremity muscle activity in older adults. J. Bone Jt. Surg. Am. 2001, 83, 907–915. [Google Scholar] [CrossRef] [PubMed]
- Stanitski, D.F. Limb-length inequality: Assessment and treatment options. J. Am. Acad Orthop. Surg. 1999, 7, 143–153. [Google Scholar] [CrossRef]
- El-Husseini, T.F.; Ghaly, N.A.; Mahran, M.A.; Al Kersh, M.A.; Emara, K.M. Comparison between lengthening over nail and conventional Ilizarov lengthening: A prospective randomized clinical study. Strateg. Trauma Limb Reconstr. 2013, 8, 97–101. [Google Scholar] [CrossRef] [Green Version]
- Rozbruch, S.R.; Kleinman, D.; Fragomen, A.T.; Ilizarov, S. Limb lengthening and then insertion of an intramedullary nail: A case-matched comparison. Clin. Orthop. Relat. Res. 2008, 466, 2923–2932. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shabtai, L.; Specht, S.C.; Standard, S.C.; Herzenberg, J.E. Internal lengthening device for congenital femoral deficiency and fibular hemimelia. Clin. Orthop. Relat. Res. 2014, 472, 3860–3868. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prince, D.E.; Herzenberg, J.E.; Standard, S.C.; Paley, D. Lengthening With External Fixation Is Effective in Congenital Femoral Deficiency. Clin. Orthop. Relat. Res. 2015, 473, 3261–3271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Horn, J.; Grimsrud, O.; Dagsgard, A.H.; Huhnstock, S.; Steen, H. Femoral lengthening with a motorized intramedullary nail. Acta Orthop. 2015, 86, 248–256. [Google Scholar] [CrossRef] [PubMed]
- Laubscher, M.; Mitchell, C.; Timms, A.; Goodier, D.; Calder, P. Outcomes following femoral lengthening: An initial comparison of the Precice intramedullary lengthening nail and the LRS external fixator monorail system. Bone Jt. J. 2016, 98, 1382–1388. [Google Scholar] [CrossRef] [Green Version]
- Kirane, Y.M.; Fragomen, A.T.; Rozbruch, S.R. Precision of the PRECICE internal bone lengthening nail. Clin. Orthop. Relat. Res. 2014, 472, 3869–3878. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Farsetti, P.; De Maio, F.; Potenza, V.; Efremov, K.; Marsiolo, M.; Caterini, A.; Ippolito, E. Lower limb lengthening over an intramedullary nail: A long-term follow-up study of 28 cases. J. Orthop. Traumatol. 2019, 20, 30. [Google Scholar] [CrossRef]
- Kocaoglu, M.; Eralp, L.; Kilicoglu, O.; Burc, H.; Cakmak, M. Complications encountered during lengthening over an intramedullary nail. J. Bone Jt. Surg. Am. 2004, 86, 2406–2411. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simpson, A.H.; Cole, A.S.; Kenwright, J. Leg lengthening over an intramedullary nail. J. Bone Jt. Surg. Br 1999, 81, 1041–1045. [Google Scholar] [CrossRef]
- Horn, J.; Steen, H.; Huhnstock, S.; Hvid, I.; Gunderson, R.B. Limb lengthening and deformity correction of congenital and acquired deformities in children using the Taylor Spatial Frame. Acta Orthop. 2017, 88, 334–340. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abdelgawad, A.A.; Jauregui, J.J.; Standard, S.C.; Paley, D.; Herzenberg, J.E. Prophylactic Intramedullary Rodding Following Femoral Lengthening in Congenital Deficiency of the Femur. J. Pediatr. Orthop. 2017, 37, 416–423. [Google Scholar] [CrossRef]
- Popkov, A.; Foster, P.; Gubin, A.; Borzunov, D.; Popkov, D. The use of flexible intramedullary nails in limb lengthening. Expert Rev. Med. Devices 2017, 14, 741–753. [Google Scholar] [CrossRef] [PubMed]
- Popkov, A.; Pietrzak, S.; Antonov, A.; Parol, T.; Lazovic, M.; Podeszwa, D.; Popkov, D. Limb Lengthening for Congenital Deficiencies Using External Fixation Combined With Flexible Intramedullary Nailing: A Multicenter Study. J. Pediatr. Orthop. 2021, 41, e439–e447. [Google Scholar] [CrossRef] [PubMed]
- Schiedel, F.; Elsner, U.; Gosheger, G.; Vogt, B.; Rodl, R. Prophylactic titanium elastic nailing (TEN) following femoral lengthening (Lengthening then rodding) with one or two nails reduces the risk for secondary interventions after regenerate fractures: A cohort study in monolateral vs. bilateral lengthening procedures. BMC Musculoskelet. Disord. 2013, 14, 302. [Google Scholar] [CrossRef] [Green Version]
- Montpetit, K.; Hamdy, R.C.; Dahan-Oliel, N.; Zhang, X.; Narayanan, U.G. Measurement of health-related quality of life in children undergoing external fixator treatment for lower limb deformities. J. Pediatr. Orthop. 2009, 29, 920–926. [Google Scholar] [CrossRef]
- Kim, S.J.; Balce, G.C.; Agashe, M.V.; Song, S.H.; Song, H.R. Is bilateral lower limb lengthening appropriate for achondroplasia?: Midterm analysis of the complications and quality of life. Clin. Orthop. Relat. Res. 2012, 470, 616–621. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gomez, C.; Nelson, S.; Speirs, J.; Barnes, S. Magnetic Intramedullary Lengthening Nails and MRI Compatibility. J. Pediatr. Orthop. 2018, 38, e584–e587. [Google Scholar] [CrossRef]

| IMN (n = 11) | MRS (n = 11) | TSF (n = 17) | p-Value | |
|---|---|---|---|---|
| Males/Females | 5/6 | 7/4 | 9/8 | 0.69 * |
| Age (years) | 14 (11–15.5) | 14 (13–15.5) | 13.6 (11–16) | 0.65 ** |
| Weight (kg) | 56 (53–58.8) | 54 (42–62.5) | 53 (46.5–63.5) | 0.9 ** |
| BMI (kg/m2) | 22.5 (19.4–23.6) | 26.7 (22.9–27.3) | 21.8 (19.3–22.7) | 0.002 ** |
| Hospital stay (days) | 12 (10.5–13.8) | 9 (9–11) | 10.3 (9–12) | 0.19 ** |
| Time of surgery (min) | 125 (113–130) | 80 (55–89) | 101 (80–115) | <0.005 ** |
| Distraction parameters | ||||
| Distraction aim (mm) | 50 (33.5–54.5) | 55 (45–55) | 42 (30–50) | 0.07 ** |
| Achieved distraction (mm) | 45 (33.5–53.8) | 55 (45–55) | 42 (30–50) | 0.08 ** |
| Distraction time (days) | 45 (33–53) | 55 (53–59) | 42 (29–51) | 0.03 ** |
| Distraction index (mm/d) | 0.85 (0.81–0.86) | 0.85 (0.73–0.89) | 0.85 (0.83–0.88) | 0.89 ** |
| Lengthening index (days/cm) | 24.3 (21.8–33.1) | 44.2 (42–50.9) | 48.4 (38.6–63.5) | <0.001 ** |
| Consolidation index (days/cm) | 12.9 (10.7–21.3) | 32.9 (30.2–37.6) | 36.9 (26.6–51.5) | <0.001 ** |
| Time to device removal (days) | N/A | 179 (172.5–195.8) | 150 (128–165) | 0.002 *** |
| Time to full weight bearing (days) | 106 (90–118) | 227 (202–232) | 174 (152–214.5) | 0.001 ** |
| Follow-up (months) | 10 (9.5–13.5) | 17 (10.5–25) | 15 (9–21.5) | 0.2 ** |
| Diagnosis | ||||
| CFD | 7 | 3 | 10 | |
| Achondroplasia | - | 6 | - | |
| Hypochondroplasia | - | 1 | 1 | |
| Fibular hemimelia | - | 1 | 3 | |
| Congenital dislocation of the hip | 2 | - | 3 | |
| Beckwith–Wiedemann syndrome | 2 | - | - | |
| IMN (n = 11) | MRS (n = 11) | TSF (n = 17) | |
|---|---|---|---|
| Problems | None | 2 (18%)—pinsite/superficial infection | 5 (29%)—pin site/superficial infection 1 (6%)—heterotopic intramuscular ossifications in pin places |
| Obstacles | 1 (9%)—delayed consolidation | 2 (18%)—frame Destabilization 1(9%)—pre-consolidation | 2 (12%)—bone bending |
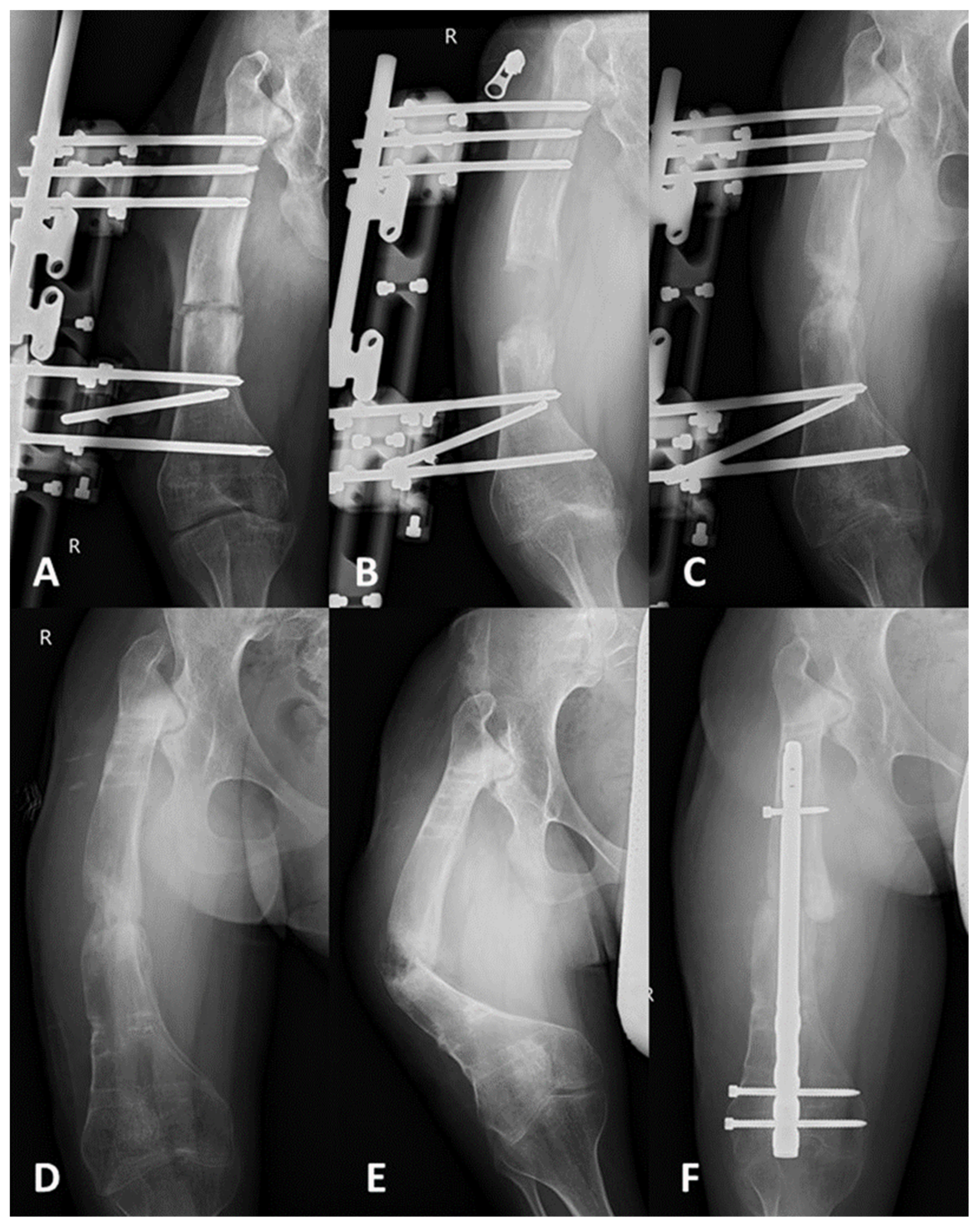
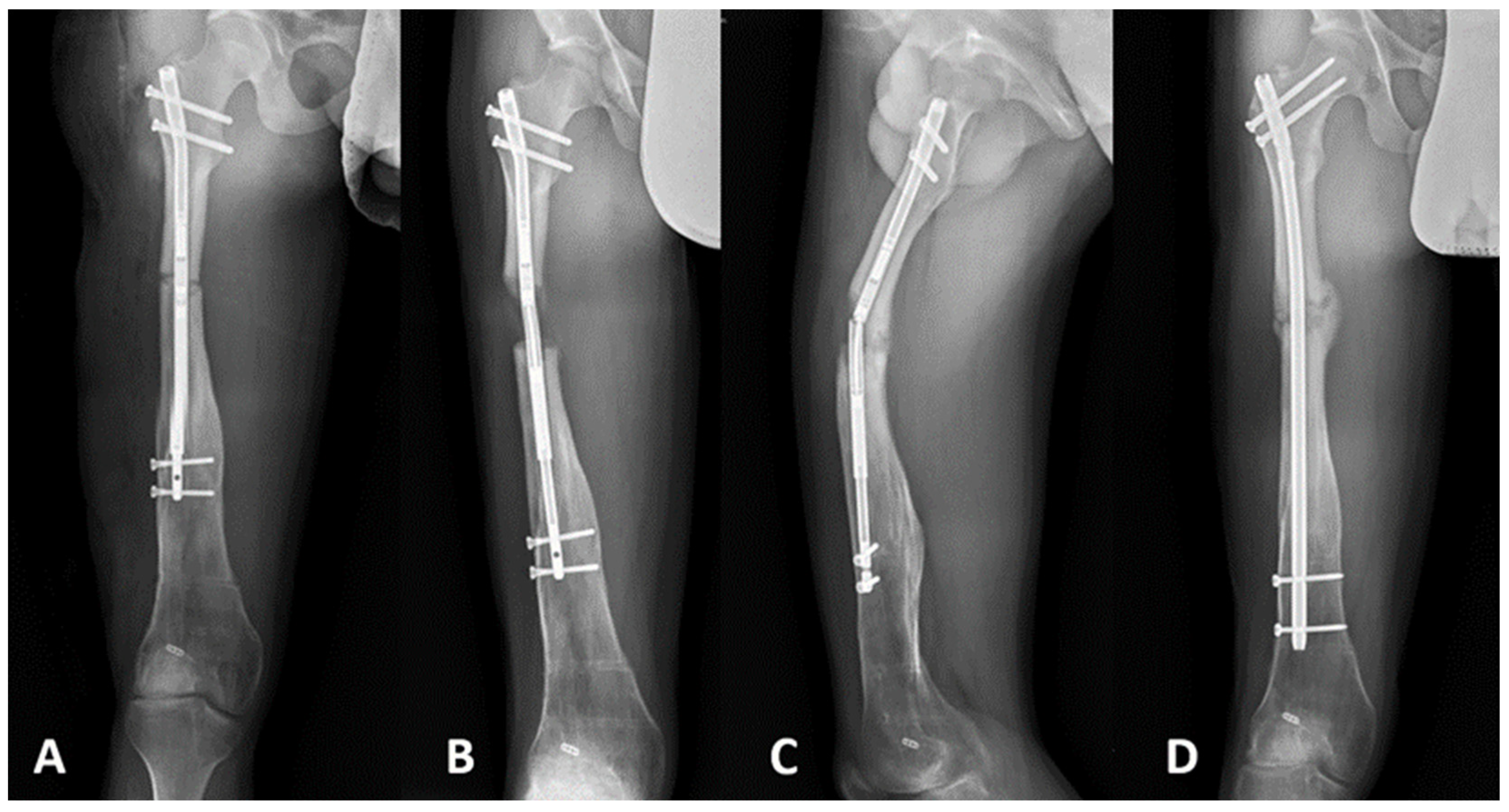
| Complications | 1 (9%)—hardware failure (broken nail and regenerate fracture) (Figure 2) | 1 (9%)—malunion 1 (9%)—fracture post removal (Figure 3) | 2 (12%)—fracture post removal |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pietrzak, S.; Grzelecki, D.; Parol, T.; Czubak, J. Comparison of Intramedullary Magnetic Nail, Monolateral External Distractor, and Spatial External Fixator in Femur Lengthening in Adolescents with Congenital Diseases. J. Clin. Med. 2021, 10, 5957. https://doi.org/10.3390/jcm10245957
Pietrzak S, Grzelecki D, Parol T, Czubak J. Comparison of Intramedullary Magnetic Nail, Monolateral External Distractor, and Spatial External Fixator in Femur Lengthening in Adolescents with Congenital Diseases. Journal of Clinical Medicine. 2021; 10(24):5957. https://doi.org/10.3390/jcm10245957
Chicago/Turabian StylePietrzak, Szymon, Dariusz Grzelecki, Tomasz Parol, and Jarosław Czubak. 2021. "Comparison of Intramedullary Magnetic Nail, Monolateral External Distractor, and Spatial External Fixator in Femur Lengthening in Adolescents with Congenital Diseases" Journal of Clinical Medicine 10, no. 24: 5957. https://doi.org/10.3390/jcm10245957






