Extracorporeal Shock Wave Therapy Combined with Complex Decongestive Therapy in Patients with Breast Cancer-Related Lymphedema: A Systemic Review and Meta-Analysis
Abstract
:1. Introduction
- Does adjunctive ESWT provide additional benefits for BCRL patients compared to CDT alone? If so, in what manner?
- Can ESWT serve as a replacement for CDT in patients with BCRL? If so, in what aspect?
2. Materials and Methods
2.1. Identification and Selection of Studies
2.2. Assessment of the Characteristics of Studies
2.2.1. Quality
2.2.2. Participants
2.2.3. Intervention
2.2.4. Outcome Measures
2.2.5. Data Extraction and Data Analysis
3. Results
3.1. Study Selection Process
3.2. Characteristics of Selected Studies
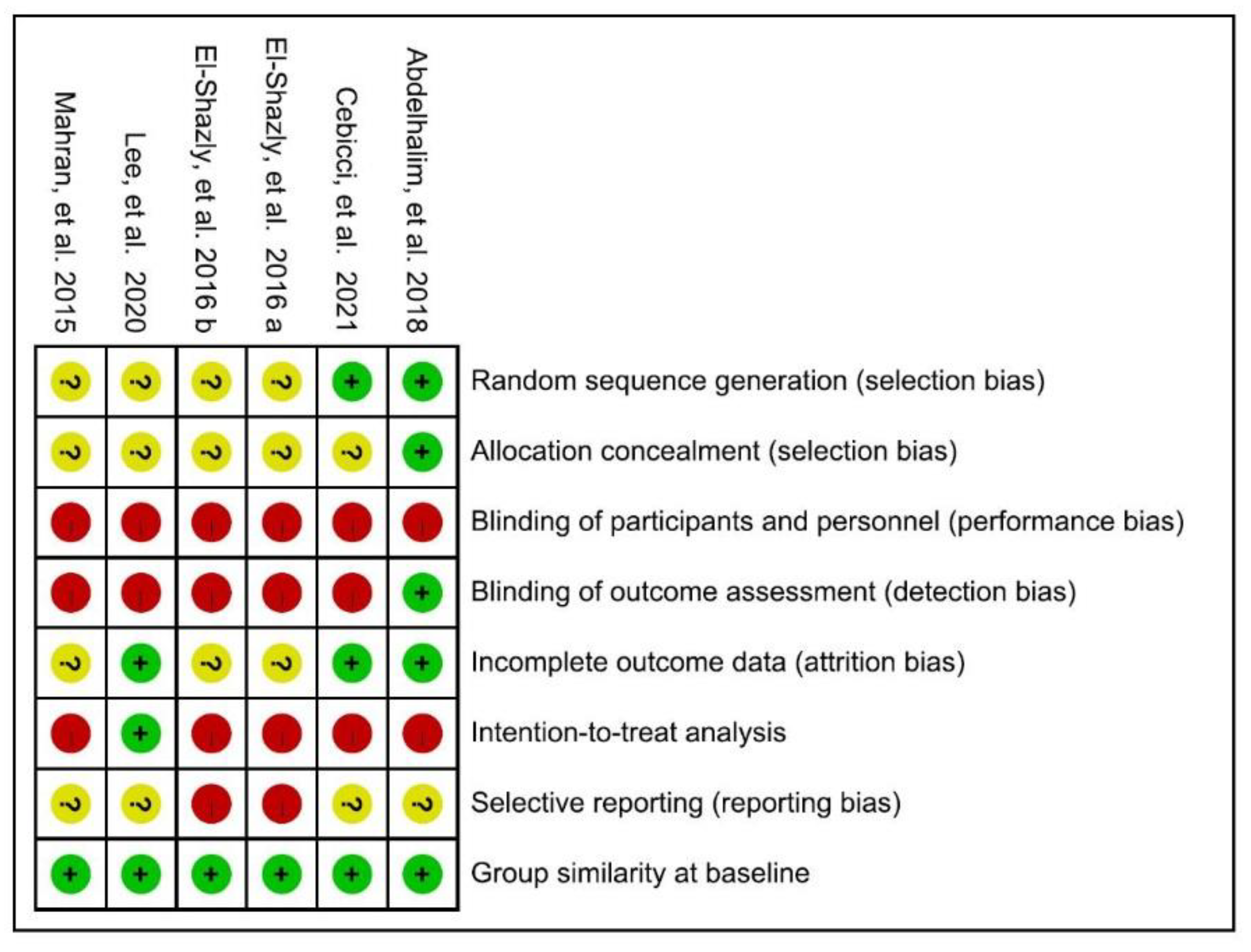
3.2.1. Quality
3.2.2. Participants
3.2.3. Intervention
3.2.4. Outcome Measures
3.3. Effect of Intervention
3.3.1. Primary Outcome: Volume of Lymphedema
3.3.2. Primary Outcome: Arm Circumference
3.3.3. Secondary Outcome: Skin Thickness
3.3.4. Secondary Outcome: Shoulder Range of Motion
3.3.5. Secondary Outcome: qDASH
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fitzmaurice, C.; Allen, C.; Barber, R.M.; Barregard, L.; Bhutta, Z.A.; Brenner, H.; Dicker, D.J.; Chimed-Orchir, O.; Dandona, R.; Dandona, L.; et al. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived with Disability, and Disability-Adjusted Life years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol. 2017, 3, 524–548. [Google Scholar] [PubMed]
- Azamjah, N.; Soltan-Zadeh, Y.; Zayeri, F. Global Trend of Breast Cancer Mortality Rate: A 25-Year Study. Asian Pac. J. Cancer Prev. 2019, 20, 2015–2020. [Google Scholar] [CrossRef] [PubMed]
- DiSipio, T.; Rye, S.; Newman, B.; Hayes, S. Incidence of unilateral arm lymphoedema after breast cancer: A systematic review and meta-analysis. Lancet Oncol. 2013, 14, 500–515. [Google Scholar] [CrossRef]
- Shah, C.; Vicini, F.A. Breast cancer-related arm lymphedema: Incidence rates, diagnostic techniques, optimal management and risk reduction strategies. Int. J. Radiat. Oncol. Biol. Phys. 2011, 81, 907–914. [Google Scholar] [CrossRef] [PubMed]
- Gillespie, T.C.; Sayegh, H.E.; Brunelle, C.L.; Daniell, K.M.; Taghian, A.G. Breast cancer-related lymphedema: Risk factors, precautionary measures, and treatments. Gland Surg. 2018, 7, 379–403. [Google Scholar] [CrossRef]
- McLaughlin, S.A.; Brunelle, C.L.; Taghian, A. Breast Cancer-Related Lymphedema: Risk Factors, Screening, Management, and the Impact of Locoregional Treatment. J. Clin. Oncol. 2020, 38, 2341–2350. [Google Scholar] [CrossRef]
- Chen, C.E.; Chiang, N.J.; Perng, C.K.; Ma, H.; Lin, C.H. Review of preclinical and clinical studies of using cell-based therapy for secondary lymphedema. J. Surg. Oncol. 2020, 121, 109–120. [Google Scholar] [CrossRef] [Green Version]
- Binkley, J.M.; Harris, S.R.; Levangie, P.K.; Pearl, M.; Guglielmino, J.; Kraus, V.; Rowden, D.P. Patient perspectives on breast cancer treatment side effects and the prospective surveillance model for physical rehabilitation for women with breast cancer. Cancer 2012, 118 (Suppl. 8), 2207–2216. [Google Scholar] [CrossRef] [PubMed]
- Korpan, M.I.; Crevenna, R.; Fialka-Moser, V. Lymphedema: A therapeutic approach in the treatment and rehabilitation of cancer patients. Am. J. Phys. Med. Rehabil. 2011, 90 (Suppl. 1), S69–S75. [Google Scholar] [CrossRef]
- Leduc, O.; Leduc, A.; Bourgeois, P.; Belgrado, J.P. The physical treatment of upper limb edema. Cancer 1998, 83 (Suppl. 12), 2835–2839. [Google Scholar] [CrossRef]
- Tiwari, P.; Coriddi, M.; Salani, R.; Povoski, S.P. Breast and gynecologic cancer-related extremity lymphedema: A review of diagnostic modalities and management options. World J. Surg. Oncol. 2013, 11, 237. [Google Scholar] [CrossRef] [Green Version]
- Ko, D.S.; Lerner, R.; Klose, G.; Cosimi, A.B. Effective treatment of lymphedema of the extremities. Arch. Surg. 1998, 113, 452–458. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ezzo, J.; Manheimer, E.; McNeely, M.L.; Howell, D.M.; Weiss, R.; Johansson, K.I.; Bao, T.; Bily, L.; Tuppo, C.M.; Williams, A.F.; et al. Manual lymphatic drainage for lymphedema following breast cancer treatment. Cochrane Database Syst. Rev. 2015, 5, CD003475. [Google Scholar] [CrossRef] [Green Version]
- Valchanou, V.D.; Michailov, P. High energy shock waves in the treatment of delayed and nonunion of fractures. Int. Orthop. 1991, 15, 181–184. [Google Scholar] [CrossRef]
- Loew, M.; Jurgowski, W. Erste Erfahrungen mit der Extrakorporalen Stosswellen-Lithotripsie (ESWL) in der Behandlung der Tendinosis calcarea der Schulter [Initial experiences with extracorporeal shockwave lithotripsy (ESWL) in treatment of tendinosis calcarea of the shoulder]. Z. Orthop. Ihre Grenzgeb. 1993, 131, 470–473. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.S.; Ericson, K.J.; Shoskes, D.A. Retrospective comparison of focused shockwave therapy and radial wave therapy for men with erectile dysfunction. Transl. Androl. Urol. 2020, 9, 2122–2128. [Google Scholar] [CrossRef]
- Ogden, J.A.; Tóth-Kischkat, A.; Schultheiss, R. Principles of shock wave therapy. Clin. Orthop. Relat. Res. 2001, 387, 8–17. [Google Scholar] [CrossRef]
- Rompe, J.D.; Furia, J.; Weil, L.; Maffulli, N. Shock wave therapy for chronic plantar fasciopathy. Br. Med. Bull. 2007, 81–82, 183–208. [Google Scholar] [CrossRef]
- Kwon, D.R. Regenerative Medicine in the Treatment of Sports Injuries: Prolotherapy and Extracorporeal Shock Wave Therapy. Korean J. Sports Med. 2016, 34, 1–9. [Google Scholar] [CrossRef]
- Mariotto, S.; Cavalieri, E.; Amelio, E.; Ciampa, A.R.; de Prati, A.C.; Marlinghaus, E.; Russo, S.; Suzuki, H. Extracorporeal shock waves: From lithotripsy to anti-inflammatory action by NO production. Nitric Oxide 2005, 12, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Yan, X.; Zeng, B.; Chai, Y.; Luo, C.; Li, X. Improvement of blood flow, expression of nitric oxide, and vascular endothelial growth factor by low-energy shockwave therapy in random-pattern skin flap model. Ann. Plast. Surg. 2008, 61, 646–653. [Google Scholar] [CrossRef] [PubMed]
- Tinazzi, E.; Amelio, E.; Marangoni, E.; Guerra, C.; Puccetti, A.; Codella, O.M.; Simeoni, S.; Cavalieri, E.; Montagnana, M.; Adani, R.; et al. Effects of shock wave therapy in the skin of patients with progressive systemic sclerosis: A pilot study. Rheumatol. Int. 2011, 31, 651–656. [Google Scholar] [CrossRef] [Green Version]
- Kubo, M.; Li, T.S.; Kamota, T.; Ohshima, M.; Shirasawa, B.; Hamano, K. Extracorporeal shock wave therapy ameliorates secondary lymphedema by promoting lymphangiogenesis. J. Vasc. Surg. 2010, 52, 429–434. [Google Scholar] [CrossRef]
- Rohringer, S.; Holnthoner, W.; Hackl, M.; Weihs, A.M.; Rünzler, D.; Skalicky, S.; Karbiener, M.; Scheideler, M.; Pröll, J.; Gabriel, C.; et al. Molecular and cellular effects of in vitro shockwave treatment on lymphatic endothelial cells. PLoS ONE 2014, 9, e114806. [Google Scholar] [CrossRef]
- Michelini, S.; Failla, A.; Moneta, G.; Zinicola, V.; Macaluso, B.; Cardone, M.; Antonucci, D. Treatment of lymphedema with shockwave therapy: Preliminary study. Eur. J. Lymphology Relat. Probl. 2007, 17, 29. [Google Scholar]
- Bae, H.; Kim, H.J. Clinical outcomes of extracorporeal shock wave therapy in patients with secondary lymphedema: A pilot study. Ann. Rehabil. Med. 2013, 37, 229–234. [Google Scholar] [CrossRef]
- Cebicci, M.A.; Sutbeyaz, S.T.; Goksu, S.S.; Hocaoglu, S.; Oguz, A.; Atilabey, A. Extracorporeal Shock Wave Therapy for Breast Cancer-Related Lymphedema: A Pilot Study. Arch. Phys. Med. Rehabil. 2016, 97, 1520–1525. [Google Scholar] [CrossRef]
- Miccinilli, S.; Bravi, M.; Maselli, M.; Santacaterina, F.; Morrone, M.; Manco, D.; Toglia, R.; Sterzi, S.; Bressi, F. The effectiveness of extracorporeal shock wave therapy on breast cancer-related lymphedema: A literature review. Lymphology 2020, 53, 118–135. [Google Scholar] [CrossRef]
- Konrad, J.; Grygiel, M. Extracorporeal shock wave therapy as a potential therapeutic tool for breast cancer related lymphedema: Narrative review of intro, animal and clinical studies. Med. Sci. Pulse 2021, 15, 66–73. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (Updated February 2021). Available online: http://www.training.cochrane.org/handbook (accessed on 14 September 2021).
- de Morton, N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust. J. Physiother. 2009, 55, 129–133. [Google Scholar] [CrossRef] [Green Version]
- Oremus, M.; Wolfson, C.; Perrault, A.; Demers, L.; Momoli, F.; Moride, Y. Interrater reliability of the modified Jadad quality scale for systematic reviews of Alzheimer’s disease drug trials. Dement. Geriatr. Cogn. Disord. 2001, 12, 232–236. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Martins da Silva, R.C.; Rezende, L.F. Assessment of impact of late postoperative physical functional disabilities on quality of life in breast cancer survivors. Tumori 2014, 100, 87–90. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Kunz, R.; Vist, G.E.; Falck-Ytter, Y.; Schünemann, H.J. GRADE Working Group. What is “quality of evidence” and why is it important to clinicians? BMJ 2008, 336, 995–998. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schünemann, H.; Brozek, J.; Guyatt, G.; Oxman, A. Handbook for Grading the Quality of Evidence and the Strength of Recommendations Using the GRADE Approach (Updated October 2013). Available online: https://gdt.gradepro.org/app/handbook/handbook.html (accessed on 16 September 2021).
- Mahran, H.G.; Thabet, A.A. Extracorporeal Shockwave Therapy for Post-Menopausal Patients with Breast Cancer-Related Lymphedema. Int. J. Cancer Res. 2015, 49, 1618–1625. [Google Scholar]
- El-Shazly, M.; Borhan, W.H.; Thabet, W.N.; Hassan, A. Response of Post-Mastectomy Lymphedema to Extracorporeal Shockwave Therapy. J. Surg. 2016, 4, 14–20. [Google Scholar] [CrossRef] [Green Version]
- El-Shazly, M.; Borhan, W.H.; Thabet, W.N.; Ashraaf, H. Response of Skin Thickness in Cases of Post-Mastectomy Lymphedema to Extracorporeal Shockwave Therapy. Med. J. Cairo. Univ. 2016, 84, 459–463. [Google Scholar]
- Abdelhalim, N.M.; Samhan, A.F. Comparison of Extracorporeal Shock Waves Therapy Versus Intermittent Pneumatic Compression Therapy in Breast Cancer-related Lymphedema. Int. J. Cancer Res. 2018, 14, 77–85. [Google Scholar]
- Lee, K.W.; Kim, S.B.; Lee, J.H.; Kim, Y.S. Effects of Extracorporeal Shockwave Therapy on Improvements in Lymphedema, Quality of Life, and Fibrous Tissue in Breast Cancer-Related Lymphedema. Ann. Rehabil. Med. 2020, 44, 386–392. [Google Scholar] [CrossRef] [PubMed]
- Cebicci, M.A.; Dizdar, M. A comparison of the effectiveness of complex decongestive therapy and extracorporeal shock wave therapy in the treatment of lymphedema secondary to breast cancer. Indian J. Surg. 2021, 83, 749–753. [Google Scholar] [CrossRef]
- Joos, E.; Vultureanu, I.; Nonneman, T.; Adriaenssens, N.; Hamdi, M.; Zeltzer, A. Low-Energy Extracorporeal Shockwave Therapy as a Therapeutic Option for Patients with a Secondary Late-Stage Fibro-Lymphedema After Breast Cancer Therapy: A Pilot Study. Lymphat. Res. Biol. 2021, 19, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Dayan, J.H.; Ly, C.L.; Kataru, R.P.; Mehrara, B.J. Lymphedema: Pathogenesis and Novel Therapies. Annu. Rev. Med. 2018, 69, 263–276. [Google Scholar] [CrossRef] [PubMed]
- Planas-Paz, L.; Lammert, E. Mechanical forces in lymphatic vascular development and disease. Cell. Mol. Life Sci. 2013, 70, 4341–4354. [Google Scholar] [CrossRef] [PubMed]
- Cui, H.S.; Joo, S.Y.; Cho, Y.S.; Park, J.H.; Ro, Y.M.; Kim, J.B.; Seo, C.H. Effect of extracorporeal shock wave therapy on keratinocytes derived from human hypertrophic scars. Sci. Rep. 2021, 11, 17296. [Google Scholar] [CrossRef] [PubMed]
- Serizawa, F.; Ito, K.; Matsubara, M.; Sato, A.; Shimokawa, H.; Satomi, S. Extracorporeal shock wave therapy induces therapeutic lymphangiogenesis in a rat model of secondary lymphoedema. Eur. J. Vasc. Endovasc. Surg. 2011, 42, 254–260. [Google Scholar] [CrossRef] [Green Version]
- Deutsch, M.; Flickinger, J.C. Shoulder and arm problems after radiotherapy for primary breast cancer. Am. J. Clin. Oncol. 2001, 24, 172–176. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.S.; Kilbreath, S.L.; Refshauge, K.M.; Herbert, R.D.; Beith, J.M. Prognosis of the upper limb following surgery and radiation for breast cancer. Breast Cancer Res. Treat. 2008, 110, 19–37. [Google Scholar] [CrossRef]
- Koehler, L.A.; Haddad, T.C.; Hunter, D.W.; Tuttle, T.M. Axillary web syndrome following breast cancer surgery: Symptoms, complications, and management strategies. Breast Cancer (Dove Med. Press) 2018, 11, 13–19. [Google Scholar] [CrossRef] [Green Version]
- Ryans, K.; Davies, C.C.; Gaw, G.; Lambe, C.; Henninge, M.; VanHoose, L. Incidence and predictors of axillary web syndrome and its association with lymphedema in women following breast cancer treatment: A retrospective study. Support Care Cancer 2020, 28, 5881–5888. [Google Scholar] [CrossRef] [PubMed]
- Davies, C.; Levenhagen, K.; Ryans, K.; Perdomo, M.; Gilchrist, L. Interventions for Breast Cancer-Related Lymphedema: Clinical Practice Guideline From the Academy of Oncologic Physical Therapy of APTA. Phys. Ther. 2020, 100, 1163–1179. [Google Scholar] [CrossRef] [PubMed]
- Crevenna, R.; Mickel, M.; Keilani, M. Extracorporeal shock wave therapy in the supportive care and rehabilitation of cancer patients. Support Care Cancer 2019, 27, 4039–4041. [Google Scholar] [CrossRef] [PubMed] [Green Version]






| Inclusion | Exclusion | |
|---|---|---|
| Design | Randomized controlled trials Cohort studies Observational studies | Preclinical study |
| Participants | People with Breast-Cancer-Related Lymphedema | Lymphedema not related to breast cancer surgery |
| Intervention | Extracorporeal shockwave therapy with or without other management | |
| Outcomes measures | Primary: volume or arm circumference Secondary: shoulder joint ROM, other quantification of symptoms, impact on QOL | |
| Language | English or Chinese with an abstract in English | Other languages |
| Study | Design | Participants (Stage of LE) | No. of Patient (ESWT/Control Group) | Age (Mean ± SD, Year) | LE Duration (Mean ± SD, Month) |
|---|---|---|---|---|---|
| Mahran et al., 2015 (Egypt) [38] | RCT | BCRL (N/A) | ESWT + CDT: 20 CDT: 20 | 52.13 ± 4.0 53.80 ± 3.4 | 15.60 ± 2.82 14.73 ± 2.86 |
| El-Shazly et al., 2016 (Egypt) [39] | RCT | BCRL (Stage 2, 3) | ESWT + CDT: 30 CDT: 30 | 30–50 (Only range) | N/A |
| El-Shazly et al., 2016 (Egypt) [40] | RCT | BCRL (Stage 2, 3) | ESWT + CDT: 30 CDT: 30 | 30–50 (Only range) | N/A |
| Abdelhalim et al., 2018 (Egypt) [41] | RCT | BCRL (N/A) | ESWT + CDT: 21 CDT: 22 | 48.71 ± 3.07 49.55 ± 2.77 | 10.95 ± 1.59 11.17 ± 1.61 |
| Lee et al., 2020 (South Korea) [42] | RCT | BCRL (Stage 2) | ESWT + CDT: 15 CDT: 15 | 53.13 ± 10.85 52.24 ± 8.60 | 12.83 ± 8.21 14.40 ± 10.63 |
| Cebicci et al., 2021 (Turkey) [43] | RCT | BCRL (N/A) | ESWT: 10 CDT: 10 | 51.61 ± 6.6 57.90 ± 6.9 | 32.7 ± 31.1 31.6 ± 30.0 |
| Cebicci et al., 2016 (Turkey) [27] | Prospective pilot study | BCRL (N/A) | ESWT: 11 | 50.63 ± 7.03 | 12 (Range: 6–84) |
| Joos et al., 2020 (Belgium) [44] | Prospective pilot study | BCRL (Stage 3) | ESWT + CDT: 10 | 62.1 ± 8.21 | 61.9 ± 17.55 |
| Study | Type of ESWT | ED (mJ/mm2) | Impulse Frequency | Dosage and Location | Interval and Sessions | |
|---|---|---|---|---|---|---|
| Mahran et al., 2015 (Egypt) [38] | rESWT | 2 bar | 4 Hz | 750 250 1500 | Axillary LN Cubital LN Arm, Forearm, Hand | 2/wk for 16 sessions |
| El-Shazly et al., 2016 (Egypt) [39] | fEWST | 0.040–0.069 | 5 Hz | 1000 1000 | Most fibrotic tissue Lesser fibrotic tissue | 2/wk for 12 sessions |
| El-Shazly et al., 2016 (Egypt) [40] | fEWST | 0.040–0.069 | 4 Hz | 1000 1000 | Most fibrotic tissue Lesser fibrotic tissue | 2/wk for 12 sessions |
| Abdelhalim et al., 2018 (Egypt) [41] | rESWT | 2 bar | 4 Hz | 750 250 1500 | Axillary LN Cubital LN Arm, Forearm, Hand | 3/wk for 12 sessions |
| Lee et al., 2020 (South Korea) [42] | fEWST | 0.056–0.068 | NA | 1000 1500 | Most fibrotic areaCubital LN, forearm | 2/wk for 6 sessions |
| Cebicci et al., 2021 (Turkey) [43] | rESWT | 2 bar | 4 Hz | 750 250 1500 | Axillary LN Cubital LN Arm, Forearm, Hand | 3/wk for 12 sessions |
| Cebicci et al., 2016 (Turkey) [27] | rESWT | 2 bar | 4 Hz | 750 250 1500 | Axillary LN Cubital LN Arm, Forearm, Hand | 3/wk for 12 sessions |
| Joos et al., 2020 (Belgium) [44] | fEWST | 0.1 | 4 Hz | 1800 800 | Most fibrotic area Grid pattern around this area | 2/wk for 8 sessions |
| Study | Study Type | Volume | Arm Circumference | Skin Thickness | qDASH | ROM |
|---|---|---|---|---|---|---|
| Mahran et al., 2015 (Egypt) [38] | RCT | Yes | Yes | No | No | Yes |
| El-Shazly et al., 2016 (Egypt) [39] | RCT | Yes | No | No | No | Yes |
| El-Shazly et al., 2016 (Egypt) [40] | RCT | No | No | Yes | No | No |
| Abdelhalim et al., 2018 (Egypt) [41] | RCT | No | Yes | Yes | No | No |
| Lee et al., 2020 (South Korea) [42] | RCT | Yes | Yes | Yes | Yes | No |
| Cebicci et al., 2021 (Turkey) [43] | RCT | Yes | Yes | No | Yes | No |
| Cebicci et al., 2016 (Turkey) [27] | Prospective pilot study | Yes | No | No | Yes | No |
| Joos et al., 2020 (Belgium) [44] | Prospective pilot study | Yes | Yes | No | No | No |
| Study | Design | No. of Patients (ESWT/Control Group) | Measurement | Volume (Mean ± SD, mL) | Intragroup Difference | Intergroup Difference | |
|---|---|---|---|---|---|---|---|
| Baseline | Post-Intervention | ||||||
| Mahran et al., 2015 (Egypt) [38] | RCT | ESWT + CDT: 20 | Difference of healthy and affected arm (15 cm above olecranon) | 811.9 ± 68.18 | 285.6 ± 30.06 | Yes | Yes |
| CDT: 20 | 797.7 ± 80.33 | 363.7 ± 24.40 | Yes | ||||
| El-Shazly et al., 2016 (Egypt) [39] | RCT | ESWT + CDT: 30 | Affected arm (N/A) | 1219.33 ± 83.42 | 924.04 ± 94.71 | Yes | Yes |
| CDT: 30 | 1235.40 ± 84.12 | 1043.85 ± 90.32 | Yes | ||||
| Lee et al., 2020 (South Korea) [42] | RCT | ESWT + CDT: 15 | Difference of healthy and affected arm (axillary level) | 840.42 ± 181.33 | 802.80 ± 149.70 | Yes | Yes |
| CDT: 15 | 822.00 ± 144.68 | 810.00 ± 156.90 | No | ||||
| Cebicci et al., 2021 (Turkey) [43] | RCT | ESWT: 10 | Difference of healthy and affected arm (axillary level) | 932.0 ± 341.9 | 795.0 ± 360.9 | Yes | No |
| CDT: 10 | 800.0 ± 402.7 | 675.0 ± 345.8 | Yes | ||||
| Cebicci et al., 2016 (Turkey) [27] | Prospective pilot study | ESWT: 11 | Difference of healthy and affected arm (axillary level) | 870.4 ± 115.1 | 736.36 ± N/A | Yes | N/A |
| Joos et al., 2020 (Belgium) [44] | Prospective pilot study | ESWT + CDT: 10 | Affected arm (N/A) | 3086.4 ± 539.47 | 2909.1 ± 471.60 | No | N/A |
| Study | Design | No. of Patients (ESWT/Control Group) | Measurement | Intragroup Difference | Intergroup Difference | |
|---|---|---|---|---|---|---|
| Mahran et al., 2015 (Egypt) [38] | RCT | ESWT + CDT: 20 | Total circumferential differences | 20 cm AE 15 cm AE 10 cm AE 10 cm BE 15 cm BE 20 cm BE | Yes | Yes |
| CDT: 20 | Yes | |||||
| Abdelhalim et al., 2018 (Egypt) [41] | RCT | ESWT + CDT: 30 | Difference of healthy and affected arm | 10 cm below axilla 10 cm AE 7 cm BE 7 cm above wrist | Yes | Yes |
| CDT: 30 | Yes | |||||
| Lee et al., 2020 (South Korea) [42] | RCT | ESWT + CDT: 15 | Affected arm | 10 cm AE Elbow 10 cm BE Wrist MCP | Yes (only 10 cm BE) | No |
| CDT: 15 | No | |||||
| Cebicci et al., 2021 (Turkey) [43] | RCT | ESWT: 10 | Difference of healthy and affected arm | 15 cm AE 10 cm BE Wrist MCP | Yes | No |
| CDT: 10 | Yes (only 10 cm BE and wrist) | |||||
| Joos et al., 2020 (Belgium) [44] | Prospectivepilot study | ESWT + CDT: 10 | Affected arm | 10 cm AE Elbow 10 cm BE | No | N/A |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsai, Y.L.; I, T.J.; Chuang, Y.C.; Cheng, Y.Y.; Lee, Y.C. Extracorporeal Shock Wave Therapy Combined with Complex Decongestive Therapy in Patients with Breast Cancer-Related Lymphedema: A Systemic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 5970. https://doi.org/10.3390/jcm10245970
Tsai YL, I TJ, Chuang YC, Cheng YY, Lee YC. Extracorporeal Shock Wave Therapy Combined with Complex Decongestive Therapy in Patients with Breast Cancer-Related Lymphedema: A Systemic Review and Meta-Analysis. Journal of Clinical Medicine. 2021; 10(24):5970. https://doi.org/10.3390/jcm10245970
Chicago/Turabian StyleTsai, Yu Lin, Ting Jie I, Ya Chi Chuang, Yuan Yang Cheng, and Yu Chun Lee. 2021. "Extracorporeal Shock Wave Therapy Combined with Complex Decongestive Therapy in Patients with Breast Cancer-Related Lymphedema: A Systemic Review and Meta-Analysis" Journal of Clinical Medicine 10, no. 24: 5970. https://doi.org/10.3390/jcm10245970
APA StyleTsai, Y. L., I, T. J., Chuang, Y. C., Cheng, Y. Y., & Lee, Y. C. (2021). Extracorporeal Shock Wave Therapy Combined with Complex Decongestive Therapy in Patients with Breast Cancer-Related Lymphedema: A Systemic Review and Meta-Analysis. Journal of Clinical Medicine, 10(24), 5970. https://doi.org/10.3390/jcm10245970






