Ultrasound of the Uterosacral Ligament, Parametrium, and Paracervix: Disagreement in Terminology between Imaging Anatomy and Modern Gynecologic Surgery
Abstract
:1. Introduction
2. Anatomical Terminology
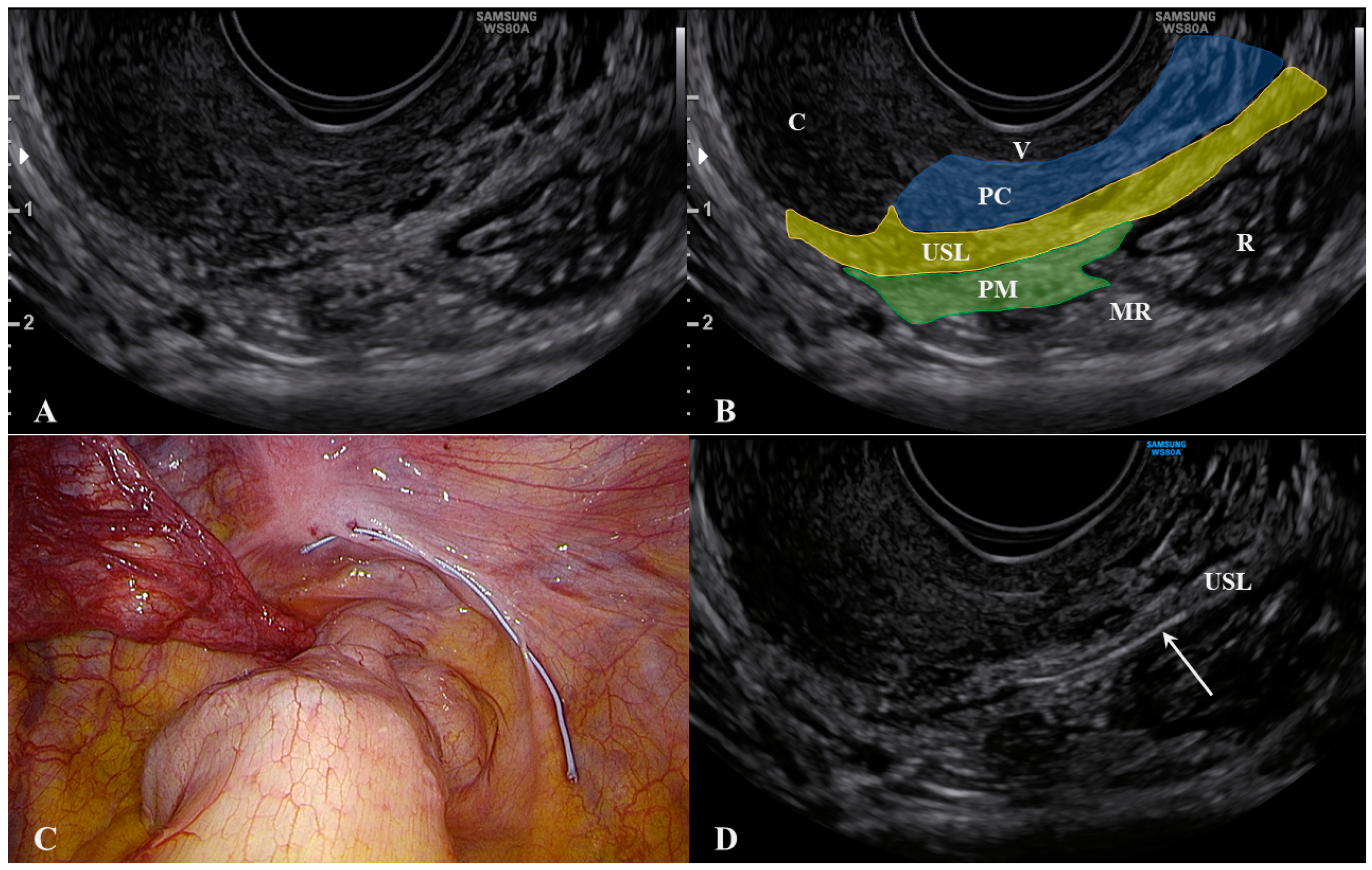
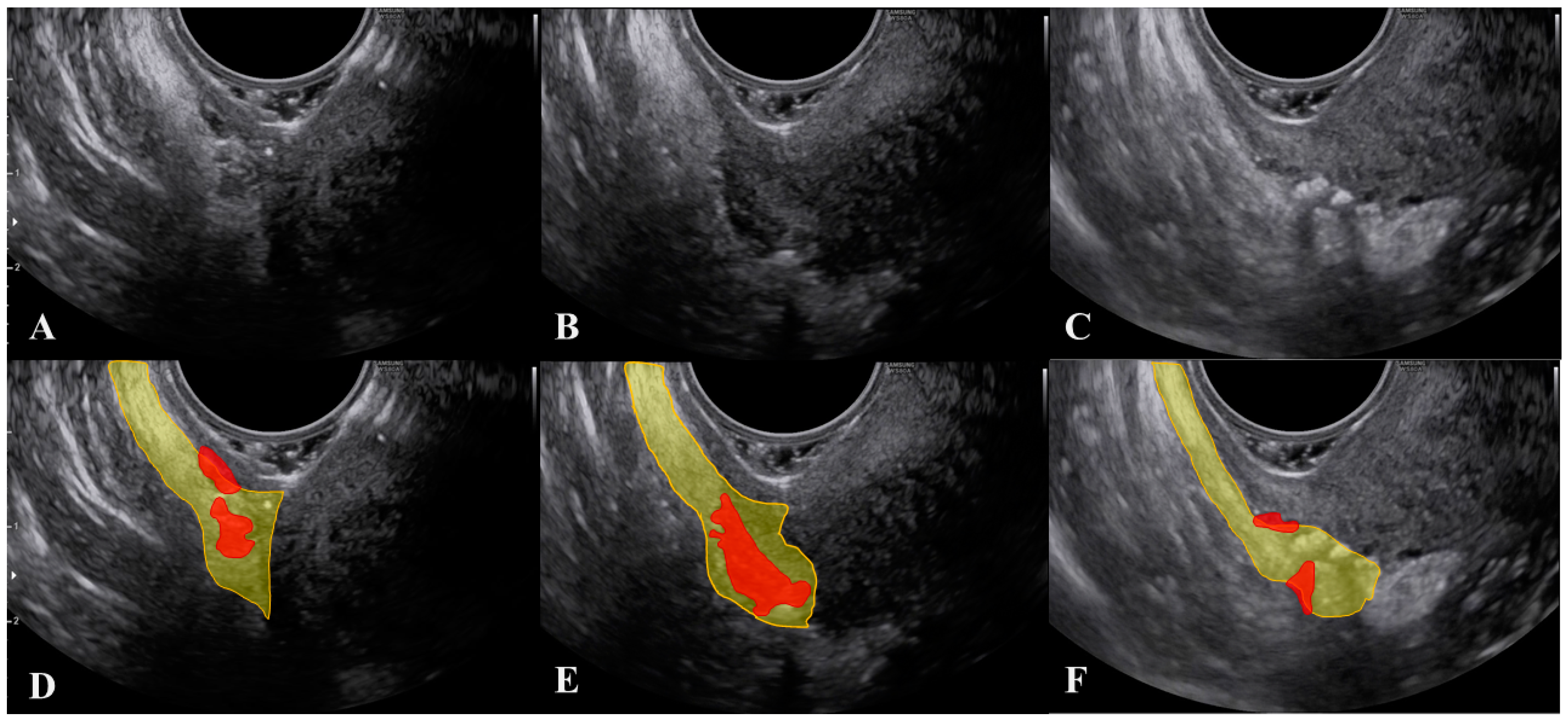
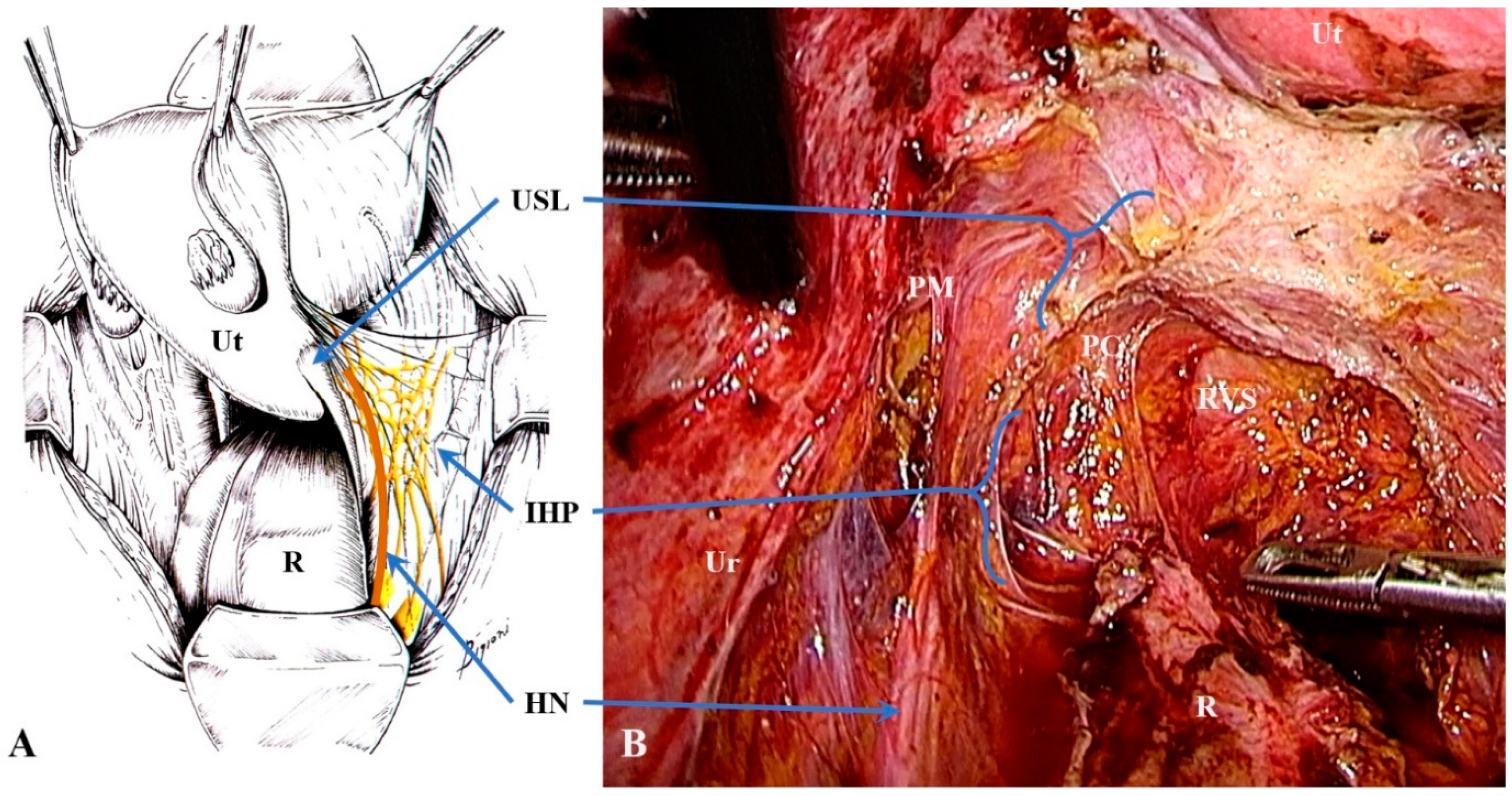
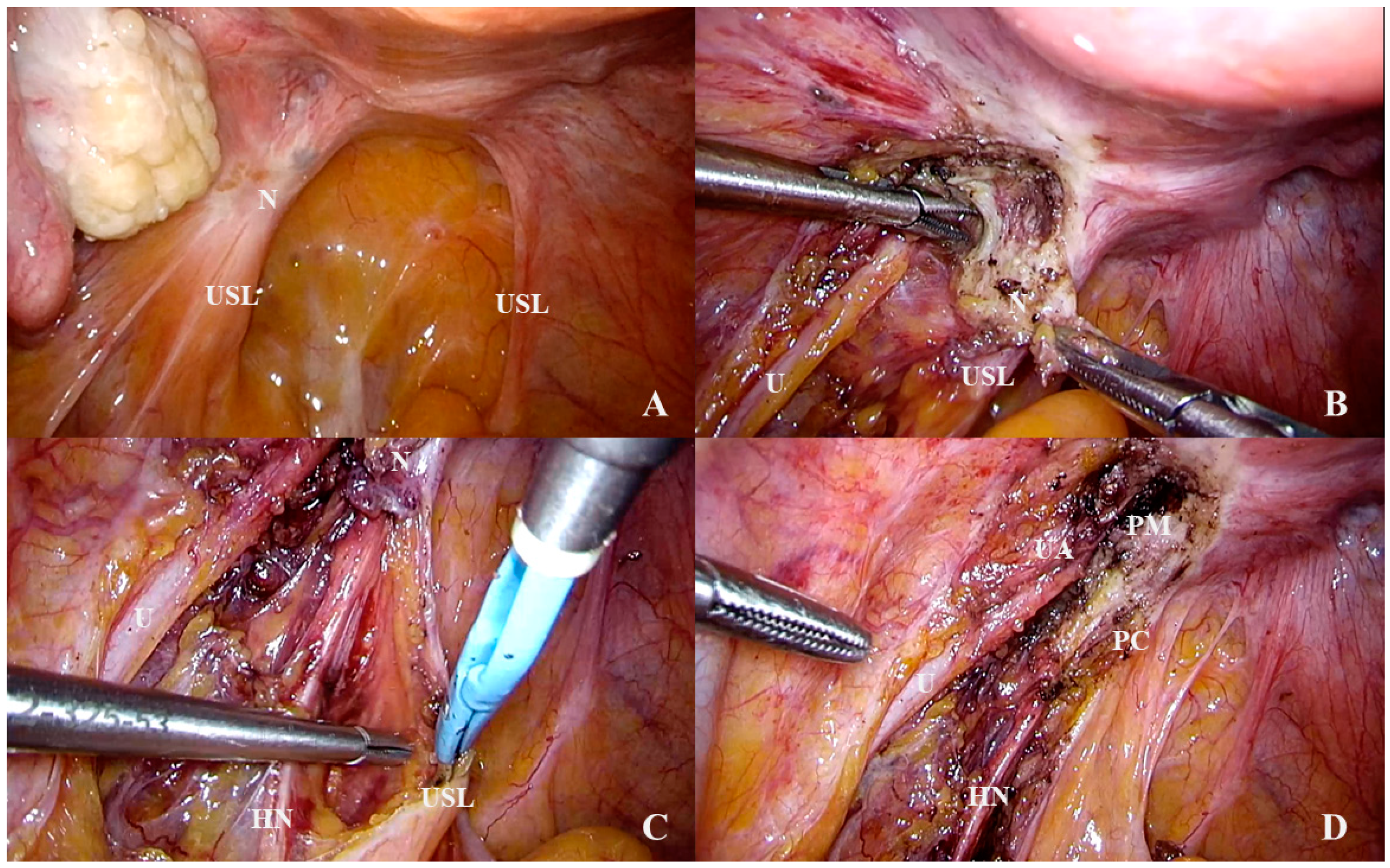
2.1. The Uterosacral Ligament
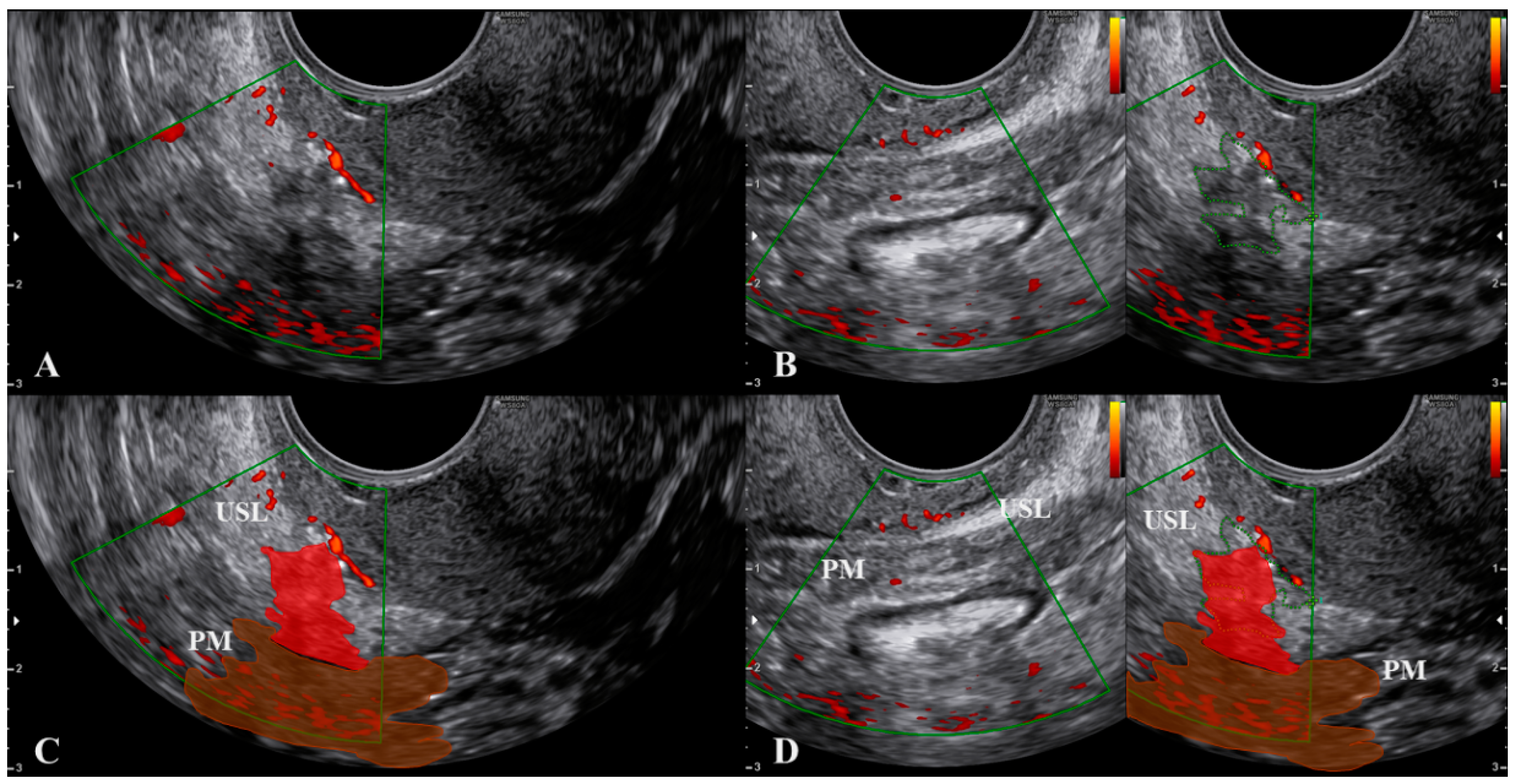
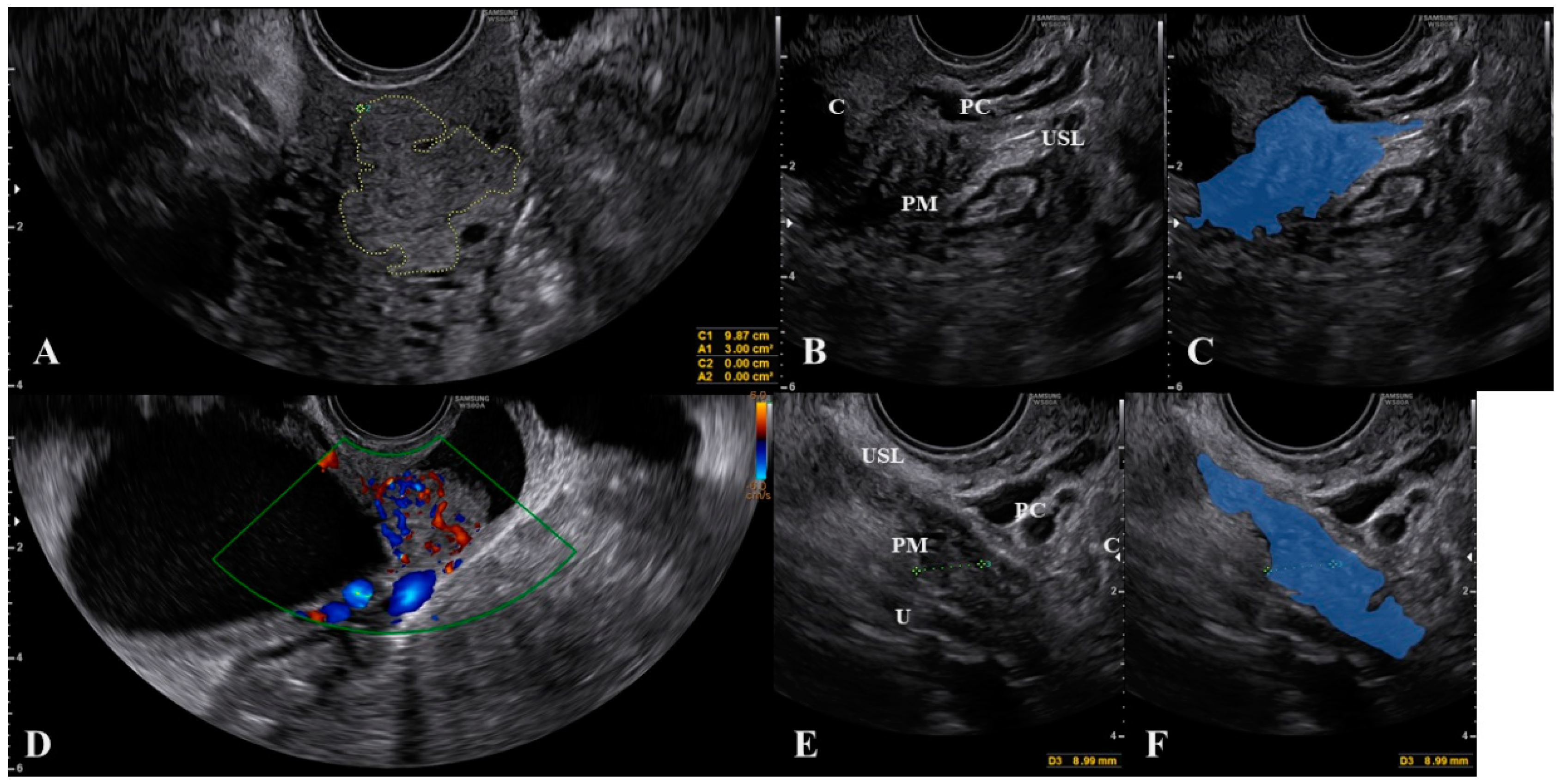
2.2. The Parametrium
2.3. The Paracervix
3. What Ultrasound Should Investigate and Detect
4. Anatomical Considerations and Surgical Implications
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Vu, D.; Haylen, B.T.; Tse, K.; Farnsworth, A. Surgical Anatomy of the Uterosacral Ligament. Int. Urogynecol. J. 2010, 21, 1123–1128. [Google Scholar] [CrossRef] [PubMed]
- Zondervan, K.T.; Becker, C.M.; Missmer, S.A. Endometriosis. N. Engl. J. Med. 2020, 382, 1244–1256. [Google Scholar] [CrossRef] [PubMed]
- Giudice, L.C.; Kao, L.C. Endometriosis. Lancet 2004, 364, 1789–1799. [Google Scholar] [CrossRef]
- Lima, R.; Abdalla-Ribeiro, H.; Nicola, A.L.; Eras, A.; Lobao, A.; Ribeiro, P.A. Endometriosis on the Uterosacral Ligament: A Marker of Ureteral Involvement. Fertil. Steril. 2017, 107, 1348–1354. [Google Scholar] [CrossRef] [Green Version]
- Guerriero, S.; Condous, G.; Van den Bosch, T.; Valentin, L.; Leone, F.P.G.; Van Schoubroeck, D.; Exacoustos, C.; Installé, A.J.F.; Martins, W.P.; Abrao, M.S.; et al. Systematic Approach to Sonographic Evaluation of the Pelvis in Women with Suspected Endometriosis, Including Terms, Definitions and Measurements: A Consensus Opinion from the International Deep Endometriosis Analysis (IDEA) Group. Ultrasound Obstet. Gynecol. 2016, 48, 318–332. [Google Scholar] [CrossRef]
- Fratelli, N.; Scioscia, M.; Bassi, E.; Musola, M.; Minelli, L.; Trivella, G. Transvaginal Sonography for Preoperative Assessment of Deep Endometriosis. J. Clin. Ultrasound 2013, 41, 69–75. [Google Scholar] [CrossRef]
- Chopin, N.; Vieira, M.; Borghese, B.; Foulot, H.; Dousset, B.; Coste, J.; Mignon, A.; Fauconnier, A.; Chapron, C. Operative Management of Deeply Infiltrating Endometriosis: Results on Pelvic Pain Symptoms According to a Surgical Classification. J. Minim. Invasive Gynecol. 2005, 12, 106–112. [Google Scholar] [CrossRef]
- Fauconnier, A.; Chapron, C.; Dubuisson, J.-B.; Vieira, M.; Dousset, B.; Bréart, G. Relation between Pain Symptoms and the Anatomic Location of Deep Infiltrating Endometriosis. Fertil. Steril. 2002, 78, 719–726. [Google Scholar] [CrossRef]
- Mabrouk, M.; Raimondo, D.; Arena, A.; Iodice, R.; Altieri, M.; Sutherland, N.; Salucci, P.; Moro, E.; Seracchioli, R. Parametrial Endometriosis: The Occult Condition That Makes the Hard Harder. J. Minim. Invasive Gynecol. 2019, 26, 871–876. [Google Scholar] [CrossRef]
- Scioscia, M.; Bruni, F.; Ceccaroni, M.; Steinkasserer, M.; Stepniewska, A.; Minelli, L. Distribution of Endometriotic Lesions in Endometriosis Stage IV Supports the Menstrual Reflux Theory and Requires Specific Preoperative Assessment and Therapy. Acta Obstet. Gynecol. Scand 2011, 90, 136–139. [Google Scholar] [CrossRef]
- Chapron, C.; Fauconnier, A.; Vieira, M.; Barakat, H.; Dousset, B.; Pansini, V.; Vacher-Lavenu, M.C.; Dubuisson, J.B. Anatomical Distribution of Deeply Infiltrating Endometriosis: Surgical Implications and Proposition for a Classification. Hum. Reprod. 2003, 18, 157–161. [Google Scholar] [CrossRef] [PubMed]
- Revised American Society for Reproductive Medicine Classification of Endometriosis: 1996. Fertil. Steril. 1997, 67, 817–821. [CrossRef]
- Cohen, P.A.; Jhingran, A.; Oaknin, A.; Denny, L. Cervical Cancer. Lancet 2019, 393, 169–182. [Google Scholar] [CrossRef]
- Landy, R.; Pesola, F.; Castañón, A.; Sasieni, P. Impact of Cervical Screening on Cervical Cancer Mortality: Estimation Using Stage-Specific Results from a Nested Case–Control Study. Br. J. Cancer 2016, 115, 1140–1146. [Google Scholar] [CrossRef] [Green Version]
- Muallem, M.Z.; Diab, Y.; Sehouli, J.; Fujii, S. Nerve-Sparing Radical Hysterectomy: Steps to Standardize Surgical Technique. Int. J. Gynecol. Cancer 2019, 29, 1203–1208. [Google Scholar] [CrossRef]
- Yabuki, Y.; Sasaki, H.; Hatakeyama, N.; Murakami, G. Discrepancies between Classic Anatomy and Modern Gynecologic Surgery on Pelvic Connective Tissue Structure: Harmonization of Those Concepts by Collaborative Cadaver Dissection. Am. J. Obstet. Gynecol. 2005, 193, 7–15. [Google Scholar] [CrossRef]
- Ceccaroni, M.; Clarizia, R.; Roviglione, G.; Ruffo, G. Neuro-Anatomy of the Posterior Parametrium and Surgical Considerations for a Nerve-Sparing Approach in Radical Pelvic Surgery. Surg. Endosc. 2013, 27, 4386–4394. [Google Scholar] [CrossRef]
- Ercoli, A.; Delmas, V.; Fanfani, F.; Gadonneix, P.; Ceccaroni, M.; Fagotti, A.; Mancuso, S.; Scambia, G. Terminologia Anatomica versus Unofficial Descriptions and Nomenclature of the Fasciae and Ligaments of the Female Pelvis: A Dissection-Based Comparative Study. Am. J. Obstet. Gynecol. 2005, 193, 1565–1573. [Google Scholar] [CrossRef]
- Leonardi, M.; Martins, W.P.; Espada, M.; Arianayagam, M.; Condous, G. Proposed Technique to Visualize and Classify Uterosacral Ligament Deep Endometriosis with and without Infiltration into Parametrium or Torus Uterinus. Ultrasound Obstet. Gynecol. 2020, 55, 137–139. [Google Scholar] [CrossRef] [Green Version]
- Guerriero, S.; Ajossa, S.; Minguez, J.A.; Jurado, M.; Mais, V.; Melis, G.B.; Alcazar, J.L. Accuracy of Transvaginal Ultrasound for Diagnosis of Deep Endometriosis in Uterosacral Ligaments, Rectovaginal Septum, Vagina and Bladder: Systematic Review and Meta-Analysis. Ultrasound Obstet. Gynecol. 2015, 46, 534–545. [Google Scholar] [CrossRef]
- Guerriero, S.; Saba, L.; Pascual, M.A.; Ajossa, S.; Rodriguez, I.; Mais, V.; Alcazar, J.L. Transvaginal Ultrasound vs Magnetic Resonance Imaging for Diagnosing Deep Infiltrating Endometriosis: Systematic Review and Meta-Analysis. Ultrasound Obstet. Gynecol. 2018, 51, 586–595. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alcazar, J.L.; García, E.; Machuca, M.; Quintana, R.; Escrig, J.; Chacón, E.; Mínguez, J.A.; Chiva, L. Magnetic Resonance Imaging and Ultrasound for Assessing Parametrial Infiltration in Cervical Cancer. A Systematic Review and Meta-Analysis. Med. Ultrason. 2020, 22, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Millischer, A.-E.; Salomon, L.J.; Santulli, P.; Borghese, B.; Dousset, B.; Chapron, C. Fusion Imaging for Evaluation of Deep Infiltrating Endometriosis: Feasibility and Preliminary Results: Fusion Imaging of Endometriosis. Ultrasound Obstet. Gynecol. 2015, 46, 109–117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moro, F.; Gui, B.; Arciuolo, D.; Bertoldo, V.; Borzi, R.; Romeo, P.; Petta, F.; Cambi, F.; Pasciuto, T.; Zannoni, G.F.; et al. Fusion Imaging of Ultrasound and MRI in the Assessment of Locally Advanced Cervical Cancer: A Prospective Study. Int. J. Gynecol. Cancer 2020, 30, 456–465. [Google Scholar] [CrossRef] [PubMed]
- Scioscia, M.; Virgilio, B.A.; Scardapane, A.; Pontrelli, G. Fusion Imaging: A Novel Diagnostic Tool for Nerve-Sparing Surgery for Deep Infiltrating Endometriosis. J. Minim. Invasive Gynecol. 2020, 27, 246–247. [Google Scholar] [CrossRef]
- Chiantera, V.; Petrillo, M.; Abesadze, E.; Sozzi, G.; Dessole, M.; Catello Di Donna, M.; Scambia, G.; Sehouli, J.; Mechsner, S. Laparoscopic Neuronavigation for Deep Lateral Pelvic Endometriosis: Clinical and Surgical Implications. J. Minim. Invasive Gynecol. 2018, 25, 1217–1223. [Google Scholar] [CrossRef]
- Aurore, V.; Röthlisberger, R.; Boemke, N.; Hlushchuk, R.; Bangerter, H.; Bergmann, M.; Imboden, S.; Mueller, M.D.; Eppler, E.; Djonov, V. Anatomy of the Female Pelvic Nerves: A Macroscopic Study of the Hypogastric Plexus and Their Relations and Variations. J. Anat. 2020, joa.13206. [Google Scholar] [CrossRef]
- Rob, L.; Halaska, M.; Robova, H. Nerve-Sparing and Individually Tailored Surgery for Cervical Cancer. Lancet Oncol. 2010, 11, 292–301. [Google Scholar] [CrossRef]
- Ceccaroni, M.; Pontrelli, G.; Scioscia, M.; Ruffo, G.; Bruni, F.; Minelli, L. Nerve-Sparing Laparoscopic Radical Excision of Deep Endometriosis with Rectal and Parametrial Resection. J. Minim. Invasive Gynecol. 2010, 17, 14–15. [Google Scholar] [CrossRef]
- Ceccaroni, M.; Clarizia, R.; Alboni, C.; Ruffo, G.; Bruni, F.; Roviglione, G.; Scioscia, M.; Peters, I.; De Placido, G.; Minelli, L. Laparoscopic Nerve-Sparing Transperitoneal Approach for Endometriosis Infiltrating the Pelvic Wall and Somatic Nerves: Anatomical Considerations and Surgical Technique. Surg. Radiol. Anat. 2010, 32, 601–604. [Google Scholar] [CrossRef]
- Muallem, M.Z.; Jöns, T.; Seidel, N.; Sehouli, J.; Diab, Y.; Querleu, D. A Concise Paradigm on Radical Hysterectomy: The Comprehensive Anatomy of Parametrium, Paracolpium and the Pelvic Autonomic Nerve System and Its Surgical Implication. Cancers 2020, 12, 1839. [Google Scholar] [CrossRef] [PubMed]
- Collins, B.G.; Ankola, A.; Gola, S.; McGillen, K.L. Transvaginal US of Endometriosis: Looking Beyond the Endometrioma with a Dedicated Protocol. Radiographics 2019, 39, 1549–1568. [Google Scholar] [CrossRef] [PubMed]
- Deslandes, A.; Parange, N.; Childs, J.T.; Osborne, B.; Bezak, E. Current Status of Transvaginal Ultrasound Accuracy in the Diagnosis of Deep Infiltrating Endometriosis Before Surgery: A Systematic Review of the Literature. J. Ultrasound Med. 2020, 39, 1477–1490. [Google Scholar] [CrossRef] [PubMed]
- Guerriero, S.; Pascual, M.A.; Ajossa, S.; Rodriguez, I.; Zajicek, M.; Rolla, M.; Rams Llop, N.; Yulzari, V.; Bardin, R.; Buonomo, F.; et al. Learning Curve for Ultrasonographic Diagnosis of Deep Infiltrating Endometriosis Using Structured Offline Training Program. Ultrasound Obstet. Gynecol. 2019, 54, 262–269. [Google Scholar] [CrossRef]
- Eisenberg, V.H.; Alcazar, J.L.; Arbib, N.; Schiff, E.; Achiron, R.; Goldenberg, M.; Soriano, D. Applying a Statistical Method in Transvaginal Ultrasound Training: Lessons from the Learning Curve Cumulative Summation Test (LC-CUSUM) for Endometriosis Mapping. Gynecol. Surg. 2017, 14, 19. [Google Scholar] [CrossRef] [Green Version]
- Indrielle-Kelly, T.; Frühauf, F.; Fanta, M.; Burgetova, A.; Lavu, D.; Dundr, P.; Cibula, D.; Fischerova, D. Application of International Deep Endometriosis Analysis (IDEA) Group Consensus in Preoperative Ultrasound and Magnetic Resonance Imaging of Deep Pelvic Endometriosis. Ultrasound Obstet. Gynecol. 2020, 56, 115–116. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scioscia, M.; Scardapane, A.; Virgilio, B.A.; Libera, M.; Lorusso, F.; Noventa, M. Ultrasound of the Uterosacral Ligament, Parametrium, and Paracervix: Disagreement in Terminology between Imaging Anatomy and Modern Gynecologic Surgery. J. Clin. Med. 2021, 10, 437. https://doi.org/10.3390/jcm10030437
Scioscia M, Scardapane A, Virgilio BA, Libera M, Lorusso F, Noventa M. Ultrasound of the Uterosacral Ligament, Parametrium, and Paracervix: Disagreement in Terminology between Imaging Anatomy and Modern Gynecologic Surgery. Journal of Clinical Medicine. 2021; 10(3):437. https://doi.org/10.3390/jcm10030437
Chicago/Turabian StyleScioscia, Marco, Arnaldo Scardapane, Bruna A. Virgilio, Marco Libera, Filomenamila Lorusso, and Marco Noventa. 2021. "Ultrasound of the Uterosacral Ligament, Parametrium, and Paracervix: Disagreement in Terminology between Imaging Anatomy and Modern Gynecologic Surgery" Journal of Clinical Medicine 10, no. 3: 437. https://doi.org/10.3390/jcm10030437
APA StyleScioscia, M., Scardapane, A., Virgilio, B. A., Libera, M., Lorusso, F., & Noventa, M. (2021). Ultrasound of the Uterosacral Ligament, Parametrium, and Paracervix: Disagreement in Terminology between Imaging Anatomy and Modern Gynecologic Surgery. Journal of Clinical Medicine, 10(3), 437. https://doi.org/10.3390/jcm10030437







