Abstract
Coronavirus Disease 19 (COVID-19), due to severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) has become an on-going global health emergency affecting over 94 million cases with more than 2 million deaths globally. Primarily identified as atypical pneumonia, it has developed into severe acute respiratory distress syndrome (ARDS), a multi-organ dysfunction with associated fatality. Ever since its emergence, COVID-19 with its plethora of clinical presentations has signalled its dynamic nature and versatility of the disease process. Being a disease with droplet transmission has now assumed the proportion of a suspected airborne nature which, once proved, poses a Herculean task to control. Because of the wide distribution of the human angiotensin-converting enzyme-2 (hACE2) receptors, known for its transmission, we envisage its multiorgan spread and extensive disease distribution. Thus, an extensive review of the extrapulmonary organotropism of SARS-CoV-2 with organ-specific pathophysiology and associated manifestations like dermatological complications, myocardial dysfunction, gastrointestinal symptoms, neurologic illnesses, hepatic and renal injury is needed urgently. The plausible mechanism of site-specific viral invasion is also discussed to give a comprehensive understanding of disease complexity, to help us to focus on research priorities and therapeutic strategies to counter the disease progression. A note on the latest advancements in vaccine research will enlighten the scientific world and equip it for better preparedness.
Keywords:
SARS-CoV-2; COVID-19; ACE-2; neurological; hepatic; dermatological; pathogenesis; therapeutics; vaccines 1. Introduction
Coronavirus disease 2019 (COVID-19) is a novel emerging human infectious disease due to severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) first reported in Wuhan, China, in December 2019. Having been present for one year, SARS-CoV-2 had infected more than 94 million individuals with 2,031,875 deaths from 218 countries globally as of 17 January 2021 [1]. COVID-19 spread quickly across the world until a global emergency and pandemic were declared by the World Health Organization (WHO) on 30 January and 11 March 2020, respectively [2]. Untiring efforts are being invested to understand the origin, transmission, and pathogenesis of COVID-19 so that effective therapeutic agents, as well as an effective vaccine, can be developed. The R (reproductive number) for SARS-CoV-2 is estimated between 1.5–3.5 in comparison to 2.0 of SARS 2002, however, the case fatality rate (CFR) is around 2–3% in SARS-CoV-2 in comparison to 10% for SARS 2002 [3,4].
Of the seven coronaviruses (CoVs), 229E, NL63, OC43, and HKU1 are known for self-limiting upper respiratory tract infections [5], whereas Middle East respiratory syndrome coronavirus (MERS-CoV), SARS-CoV, and the novel SARS-CoV-2 end up with life-threatening respiratory failure and multi-organ dysfunction [6,7]. SARS-CoV-2 through spike (S) glycoproteins recognizes and binds specifically to the human angiotensin-converting enzyme 2 (hACE2) receptors expressed on type-II alveolar epithelial cells for its entry [8]. SARS-CoV-2 has a stronger binding affinity with ACE2 along with cellular transmembrane serine protease 2 (TMPRSS2) imparting virulence and aggressive properties. Following the SARS-CoV-2 binding to alveolar epithelial cells, the innate and adaptive immune system is activated leading to cytokine-release syndrome (CRS) or macrophage activation syndrome (MAS). Increased production of interleukin (IL-1, IL-6, IL-8) cytokines in plasma resulting in dyspnea, acute respiratory distress syndrome (ARDS), and death [9]. High levels of SARS-CoV-2 shedding in the upper respiratory tract, even among presymptomatic patients, is a key factor in the transmissibility of COVID-19.
4. Hepatic Manifestations of SARS-CoV-2
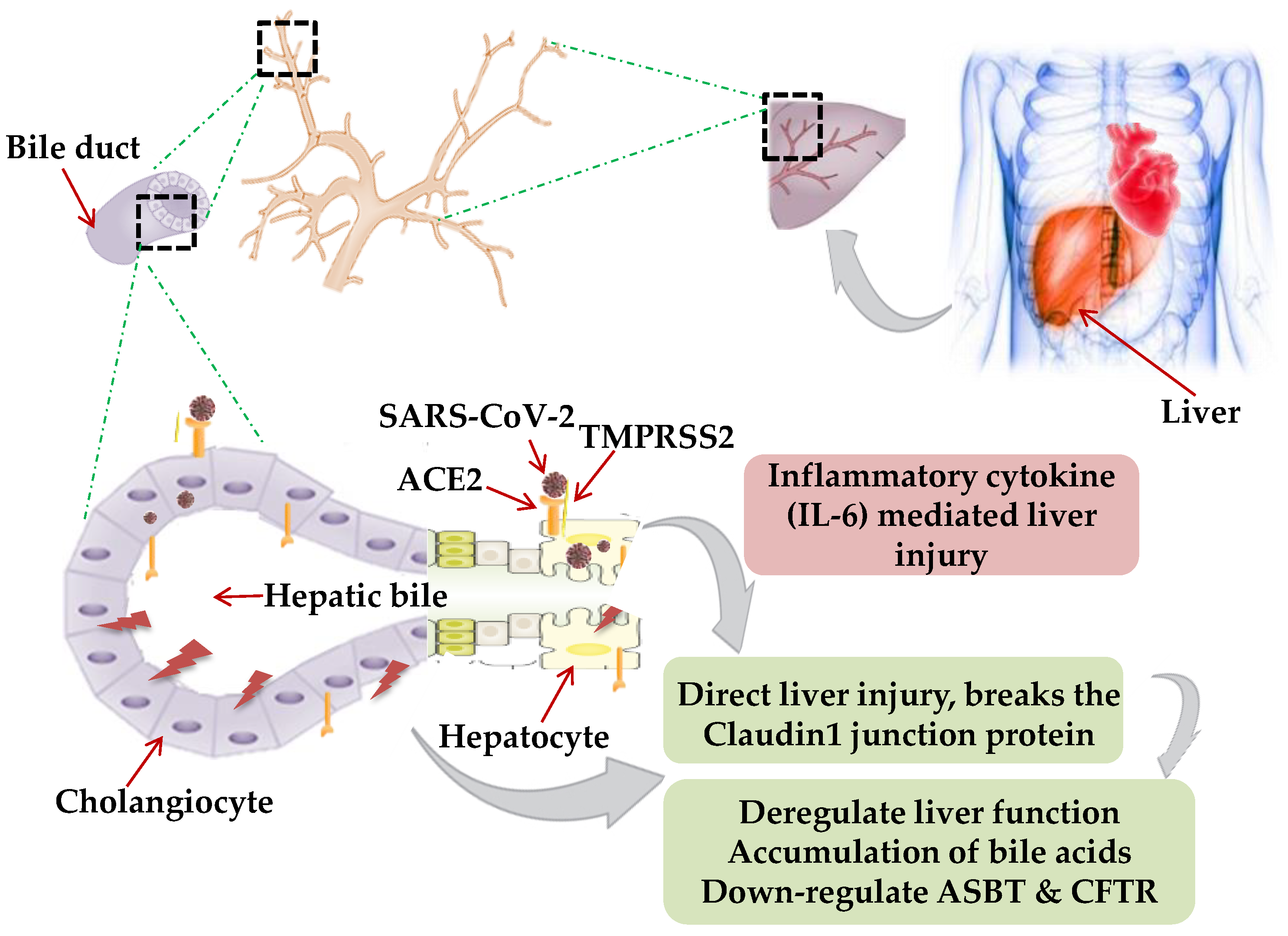
Though primarily a respiratory pathogen, shreds of evidence indicate the liver as an extra-pulmonary site for SARS-CoV-2 infection causing liver injury ranging between 14.8% to 78% [28,29]. The possible mechanism of hepatic injury in COVID-19 could either be virus related cytopathic effect or infection-induced cytokine storm. Two independent studies on healthy cohorts by single RNA sequencing data demonstrated significant ACE2 expression (59.7%) in cholangiocytes. SARS-CoV-2 binds to the ACE2 expressed cholangiocytes and being facilitated its entry by TMPRSS2 [30]. Higher coexpression of ACE-2 and TMPRSS2 in human trophoblast cell surface antigen 2 (TROP2high) cholangiocyte progenitor cells of the liver has been reported [31]. The human liver ductal organoid model revealed that cholangiocyte permissiveness for SARS-CoV-2 causes direct liver injury leading to the accumulation of bile acids [32]. In 54% of COVID-19 patients, the ACE2 expression was found to be high in bile duct cells as evidenced by elevated gamma-glutamyl transferase (GGT) levels [33]. Ablation of tight junction protein claudin 1 and down-regulation of apical sodium-dependent bile acid transporter (ASBT) and cystic fibrosis transmembrane conductance regulator (CFTR) might be the contributing factors towards liver injury in COVID-19 [32] (Figure 1).
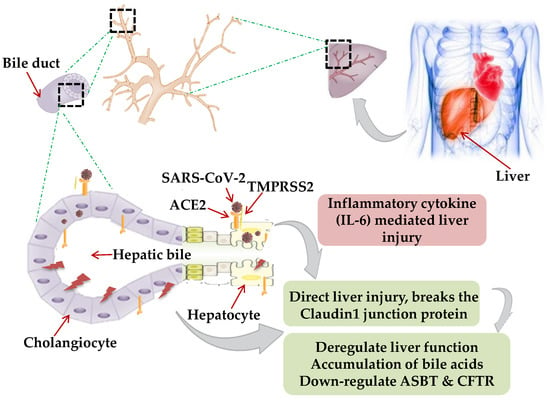
Figure 1.
Mechanism of hepatic injury: in coronavirus disease 2019 (COVID-19) patients, hepatic injury attributed by (i) direct virus-induced cytopathic effect; (ii) virus-mediated infection-induced cytokine storm. Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) binds to the angiotensin-converting enzyme 2 (ACE2), expressed on hepatocytes and cholangiocytes in the bile duct cells causing ablation of tight junction protein claudin 1 and down-regulation of apical sodium-dependent bile acid transporter (ASBT) and cystic fibrosis transmembrane conductance regulator (CFTR), leading to the accumulation of bile acids and contributing towards liver injury. Inflammatory cytokines (interleukin-6, IL-10, and IL-2) secretion by lymphocytes and macrophages aggravate inflammatory responses causing hepatic injury. Black dotted square frame in the figures denotes the selected area for the magnified portion.
A liver biopsy of a COVID-19 positive deceased patient revealed portal inflammation with microvesicular steatosis [34]. Virus-mediated persistent activation of lymphocytes and macrophages secretes inflammatory IL-6, IL-10, IL-2, and IFN-c causing CRS and hepatic injury [35].
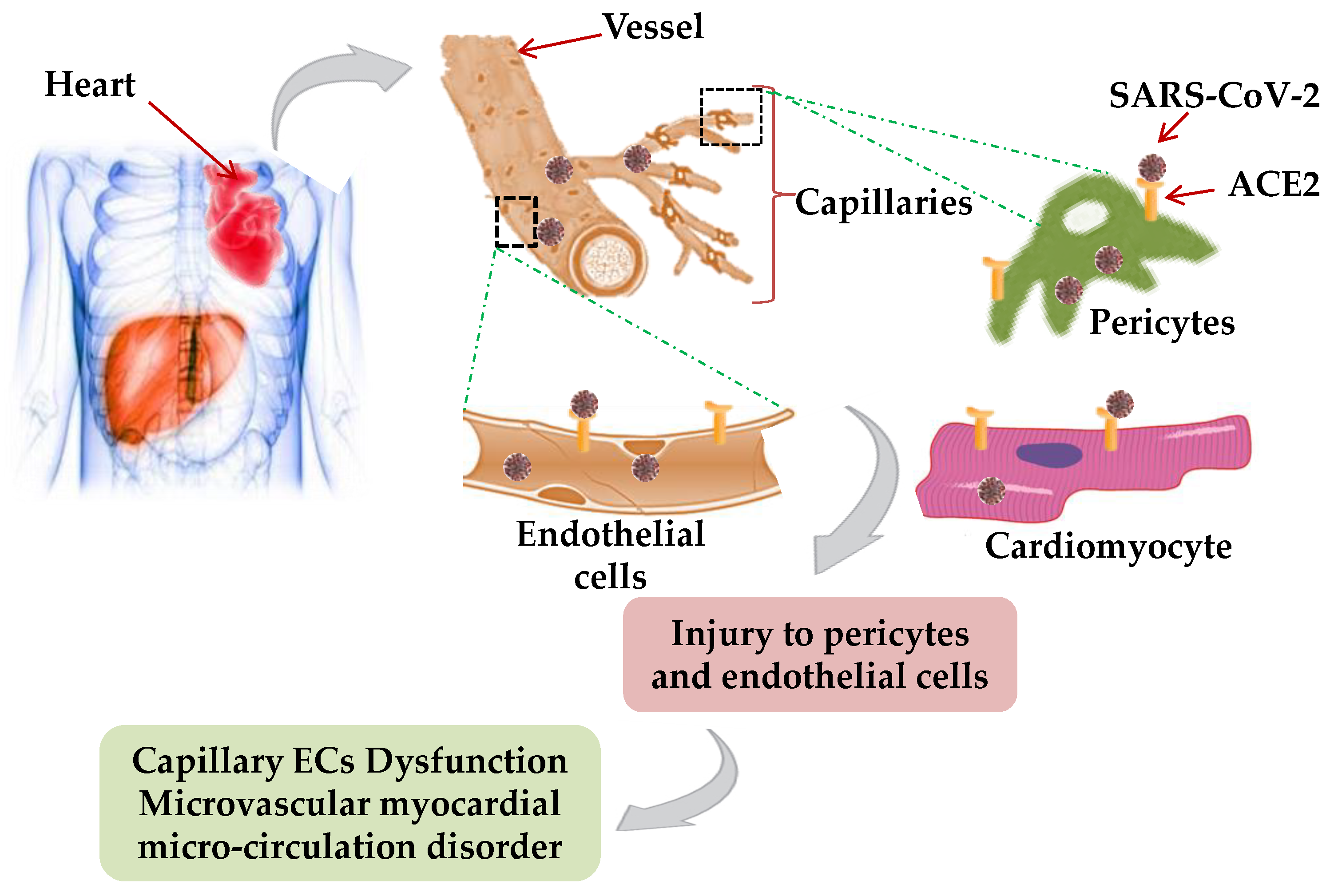
5. Cardiac Manifestations of SARS-CoV-2
Viral pathogens, especially SARS, are well-known for contributing to cardiovascular disease like acute myocarditis, acute myocardial infarction, and rapid-onset heart failure [36]. A wide range of cardiovascular events such as myocardial injury, acute coronary syndromes, cardiac arrhythmias, and heart failure are associated with COVID-19 [37,38]. In a study comprising 138 hospitalized COVID-19 patients, cardiac injury was reported in 7.2% of patients [12]. An investigation on 273 COVID-19 positive patients revealed that the higher concentration of creatine kinase isoenzyme- myocardial band (CK-MB), myohemoglobin, cardiac troponin I, and N-terminal pro-brain natriuretic peptide (NT-proBNP) in venous blood are the hallmark of heart injury [39]. A COVID-19 associated Brugada type I electrocardiographic pattern in a 61-year-old Hispanic male presented with a history of substernal chest pain, elevated CRP (150.7 mg/L) and BNP (19 pg/mL) were reported by Vidovich [40]. Sorgente et al. [41] observed an episode of supraventricular tachycardia in patients with Brugada syndrome, mostly due to plaque rupture, myocarditis, or microvascular thrombosis, resulting in virus-induced myocardial ischemia, inflammation, and ST elevation. Therefore, abnormal myocardial-associated fatalities necessitate careful monitoring of the myocardial enzyme profiles to reduce the COVID-19-associated complications in patients.
Possible Mechanism of Cardiac Manifestations
Single nuclear transcriptome analysis of the adult human heart identified the cardiomyocyte, endothelial cell (ECs), fibroblast, pericyte, and neuron-like cell (Neu) to be crucial for the proper functioning of the heart [42]. Moreover, the higher ACE2 expression in the cardiac pericytes illustrates the potential of SARS-CoV-2 to affect heart reflectory, indicating an intrinsic susceptibility of the heart to SARS-CoV-2 infection [43]. Therefore, during COVID-19 infection in the heart, SARS-CoV-2 mediated injury to pericytes and, capillary ECs dysfunction might induce microvascular myocardial microcirculation disorder [44] (Figure 2).
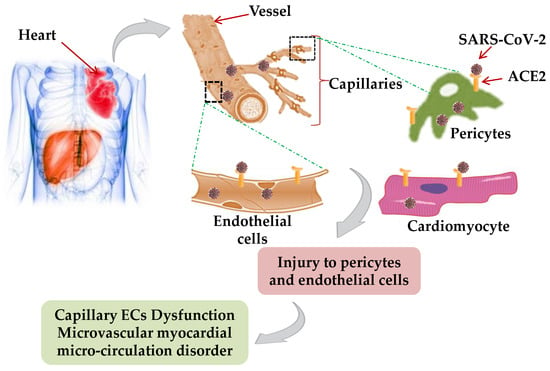
Figure 2.
Mechanism of cardiac injury: In COVID-19 patients, SARS-CoV-2 mediated injury to cardiomyocyte, pericytes, and, capillary endothelial cells by expressing ACE2 receptor and elevating the heart susceptibility to SARS-CoV-2 infection, which induce microvascular myocardial microcirculation disorder and other cardiac abnormalities.
6. Neurological Manifestations of SARS-CoV-2
SARS-CoV and MERS-CoV have neuro-invasive properties that can assist the virus to spread from the respiratory tract to the central nervous system CNS resulting in neurological manifestations in the form of febrile seizures, convulsions, and encephalitis [45]. From the epidemiological surveys, a latency period of 7 days for SARS-CoV-2 may be enough to enter and destroy the medullary neurons. Severe destructions manifested with involuntary breathing, hyposmia, ageusia, hypoxia, symptomatic seizures, status epilepticus, nausea, and vomiting accompanied by chronic respiratory distress [17]. Patients with COVID-19 have been reported with mild (anosmia and ageusia) to severe (encephalopathy) neurological features being exacerbated by smoking, due to co-expression of hACE2 and the nicotinic acetylcholine receptor (nAChR) [46]. Recent reports of SARS-CoV-2 detection in CSF of the COVID-19 patient reasonably validate the assumption of CNS being affected by SARS-CoV-2 [47]. A COVID-19 positive patient manifested with necrotizing hemorrhagic encephalopathy evidenced through a brain CT scan [48]. Viral encephalitis, infectious toxic encephalopathy, and acute cerebrovascular disease are some of the important CNS manifestations related to COVID-19. Viral encephalitis characterized by acute onset, headache, fever, vomiting, convulsions, and consciousness disorders speculation was clinically supported by the detection of SARS-CoV-2 in the CSF of COVID-19 patients [49]. Infectious toxic encephalopathy, a reversible brain dysfunction syndrome due to systemic toxemia, and hypoxia were reported in COVID-19 patients [50]. Additionally, brain autopsies showed tissue edema and partial neuronal degeneration in deceased patients of COVID-19 infection. The SARS-CoV-2 infection has been widely reported to cause CRS, leading to acute cerebrovascular disease. Also, elevated levels of D-dimer and reduced platelet count in critically ill SARS-CoV-2 patient predispose to acute cerebrovascular events. Recent case series from China and the US describe ischaemic or hemorrhagic stroke, Guillain-Barré syndrome (GBS), or acute necrotizing encephalopathy (ANE), as neurological symptoms among COVID-19 patients [51,52] (Table 1).

Table 1.
COVID-19 cases with neurological signs and manifestations.
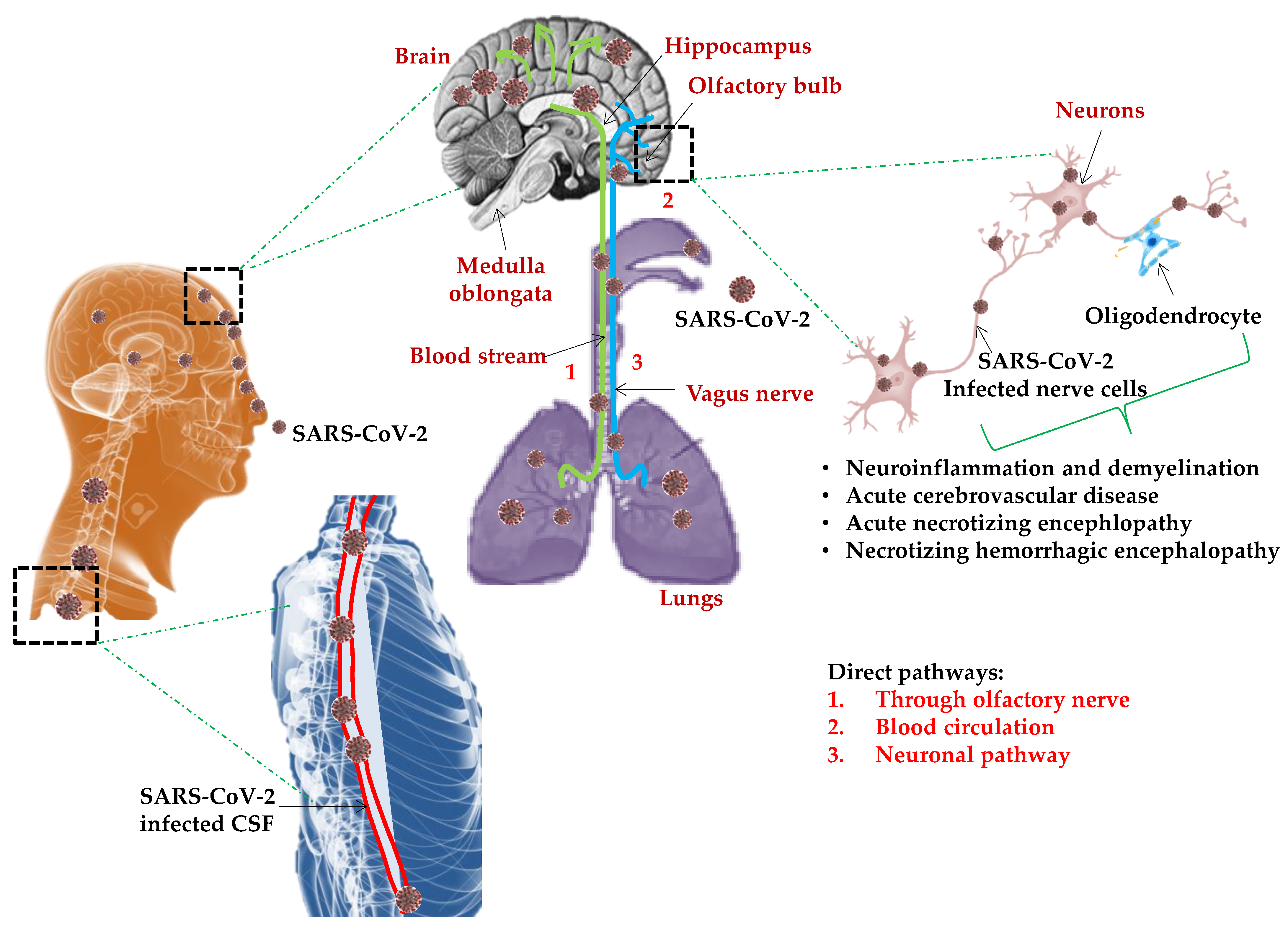
Mechanisms of Neurotropism and Neuroinvasion
Brain infiltration through the olfactory nerves following intranasal administration could be a possibility as with SARS-CoV and MERS-CoV in the transgenic mice model. There are numerous predicted pathways for CNS invasion by SARS-CoV-2 to cause neuronal damage (Figure 3).
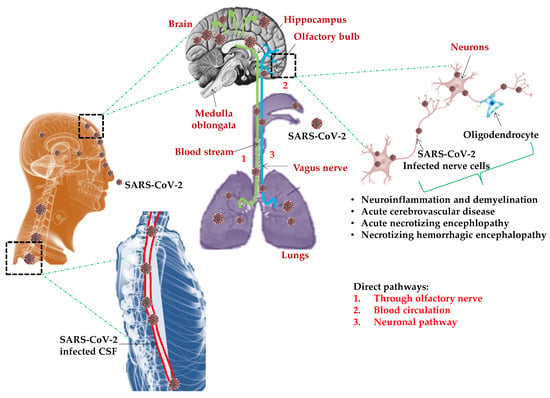
Figure 3.
Predictable model for SARS-CoV-2 induced neurological manifestations: Numerous pathways predicted for central nervous system CNS invasion by SARS-CoV-2 to cause neuronal damage. In the olfactory neuron transport, SARS-CoV-2 can infiltrate the CNS/brain through the olfactory tract by olfactory nerves in the nasal cavity/epithelium and the olfactory bulb in the forebrain, causing inflammation and demyelinating reactions. In the hematogenous route, SARS-CoV-2 binds to the receptor ACE2 expressed in the capillary endothelium and enters the CNS by a breach in the blood–brain barrier (BBB) resulting in high blood pressure with the risk of a cerebral hemorrhage. Infected and activated macrophages, microglia, astrocytes, and glial cells in the CNS induce a pro-inflammatory state by secretion of IL-6, IL-12, and IL-15 resulting in acute necrotizing encephalopathy (ANE), hyper inflammation, and encephalopathy.
In the hematogenous route, SARS-CoV-2 binds to the ACE2 expressing capillary endothelium and enters the CNS by a breach in the blood–brain barrier (BBB) resulting in high blood pressure with the risk of cerebral hemorrhage. Through dynein and kinesin motor proteins, SARS-CoV-2 infects sensory or motor nerve endings by retrograde or anterograde neuronal transport as a neuronal pathway [56,57]. In the olfactory neuron transport, SARS-CoV-2 can enter the CNS/brain through the olfactory tract by olfactory nerves in the nasal cavity/epithelium and the olfactory bulb in the forebrain, causing inflammation and demyelinating reactions. Moreover, diffusion of alveolar and interstitial inflammatory exudation, results in anabolic metabolism in brain cells, leading to hypoxia and ischemic stroke. Circumventricular organs and cerebrovascular endothelial cells expressing ACE2 receptors regulate multiple neurological functions including regulation of hormone formation, the sympathoadrenal system, vascular autoregulation, and cerebral blood flow [58,59]. COVID-19 results in a large number of fatalities, mostly due to multiple organ failure induced systemic inflammatory response syndrome (SIRS). The persistence and ability of SARS-CoV-2 to infect and activate macrophages, microglia, astrocytes, and glial cells in the CNS induces a pro-inflammatory state by secretion of IL-6, IL-12, IL-15, and tumor necrosis factor-α (TNF-α) [60]. The IL-6 mediated cytokine storm, results in acute necrotizing encephalopathy (ANE) causing neuroinflammation in addition to a surge in interleukin IL-2, IL-7, interferon-γ, monocyte chemoattractant protein 1, and TNF-α leading to hyper inflammation, encephalopathy, and even stroke [61].
7. Renal Manifestations
Renal injury is the commonly reported COVID-19 associated renal manifestations reflecting the renal tropism of SARS-CoV-2 [62]. The burden of acute kidney injury (AKI) with COVID-19 infection was relatively low, ranging from 3–9% to as high as 15% [63,64]. Further evidence supported the renal tropism of SARS-CoV-2 by the isolation of viral RNA from urine and albuminuria and hematuria in COVID-19 infection [65,66]. Puelles et al. [67] quantified the SARS-CoV-2 viral load in autopsy tissue samples obtained from 22 COVID-19 positive deceased patients; 17 (77%) had more than two coexisting conditions, which was associated with SARS-CoV-2 tropisms for the kidneys, even in patients without a history of chronic kidney disease. Three out of six patients on autopsy had a detectable SARS-CoV-2 viral load preferentially in glomerular cells as shown in Table 2.

Table 2.
COVID-19 positive cases showing renal manifestations.
The Potential Mechanisms of Renal Manifestations
In silico analysis of single-cell RNA sequencing revealed the enriched RNA expression of ACE2, TMPRSS2, and cathepsin L (CTSL) in podocytes and tubule epithelial cells which might facilitate the SARS-CoV-2 associated kidney injury [71,72]. ACE2 is expressed on the renal epithelial and bladder cells which counter the activation of the renin-angiotensin-aldosterone system (RAAS) [73]. SARS-CoV-2 can bind and injure the renal epithelial cells, thereby disrupting the body fluid and electrolyte homeostasis in addition to the erythropoietin and vitamin D production. Organ crosstalk (lung-kidney and heart-kidney), cytokine damage by IL-6, and systemic effects could be the underlying mechanisms for renal injury. During lung–kidney crosstalk, tubular epithelium enhances the IL-6 upregulation in serum resulting in increased alveolar-capillary permeability and pulmonary hemorrhage [74].
8. Gastrointestinal (GIT) Manifestations
Gastrointestinal (GIT) manifestations are revealed in 10.6% of patients with SARS and 30% of patients with MERS had diarrhea as the clinical symptoms [75]. The first case of SARS-CoV-2 infection with nausea, vomiting, and abdominal discomfort was reported from the U.S. where viral RNA was detected from the stool and respiratory specimen of a COVID-19 patient on day 7 of illness [76]. Clinically diarrhea was reported in 1–3.8% cases, diarrhea, and nausea in 10.1%, and vomiting in 3.6% [12].
Lin et al. [77] observed diarrhea and abdominal pain as evidenced in 20–50% of COVID-19 patients, which sometimes preceded respiratory symptoms. A 25-year-old female with respiratory symptoms was negative for SARS-CoV-2 in the pharyngeal aspirate but positive in the fecal sample. This might indicate feces as a source of virus transmission and the GIT region as an extrapulmonary site for virus replication [78]. Thus, early monitoring of viral RNA in the fecal specimens might benefit the disease prediction even before respiratory symptoms (Table 3).

Table 3.
Case studies showing gastrointestinal (GIT) manifestations in COVID-19 patients.
The presence of SARS-CoV-2 in stool samples even after 11 days of viral clearance from respiratory tract samples in over half of patients indicates the alternative route of excretion of the virus [83]. Similarly, Xu et al. [84] reported 8 of the 10 infected children having persistent positive SARS-CoV-2 in rectal swabs, where nasopharyngeal swabs were negative for the virus. In a multicentric study with 1992 patients, 34% of them experienced diarrhea whereas 53% experienced one of the GIT symptoms. However 74% of the cases were mild and not associated with severe clinical course [85]. Despite the ability of SARS-CoV-2 to establish a robust infection in GIT; it might be inactivated by human colonic fluids in the intestinal lumen, hence the viral RNA transiting through GIT and shedding through the feces may not be infectious [86]. However, live SARS-CoV-2 was detected using electron microscopy in stool samples from two patients, which might focus on the potentiality of fecal transmission [87]. Even though there is evidence of GI symptoms due to SARS-CoV-2, its role in the disease process is yet to be demonstrated.
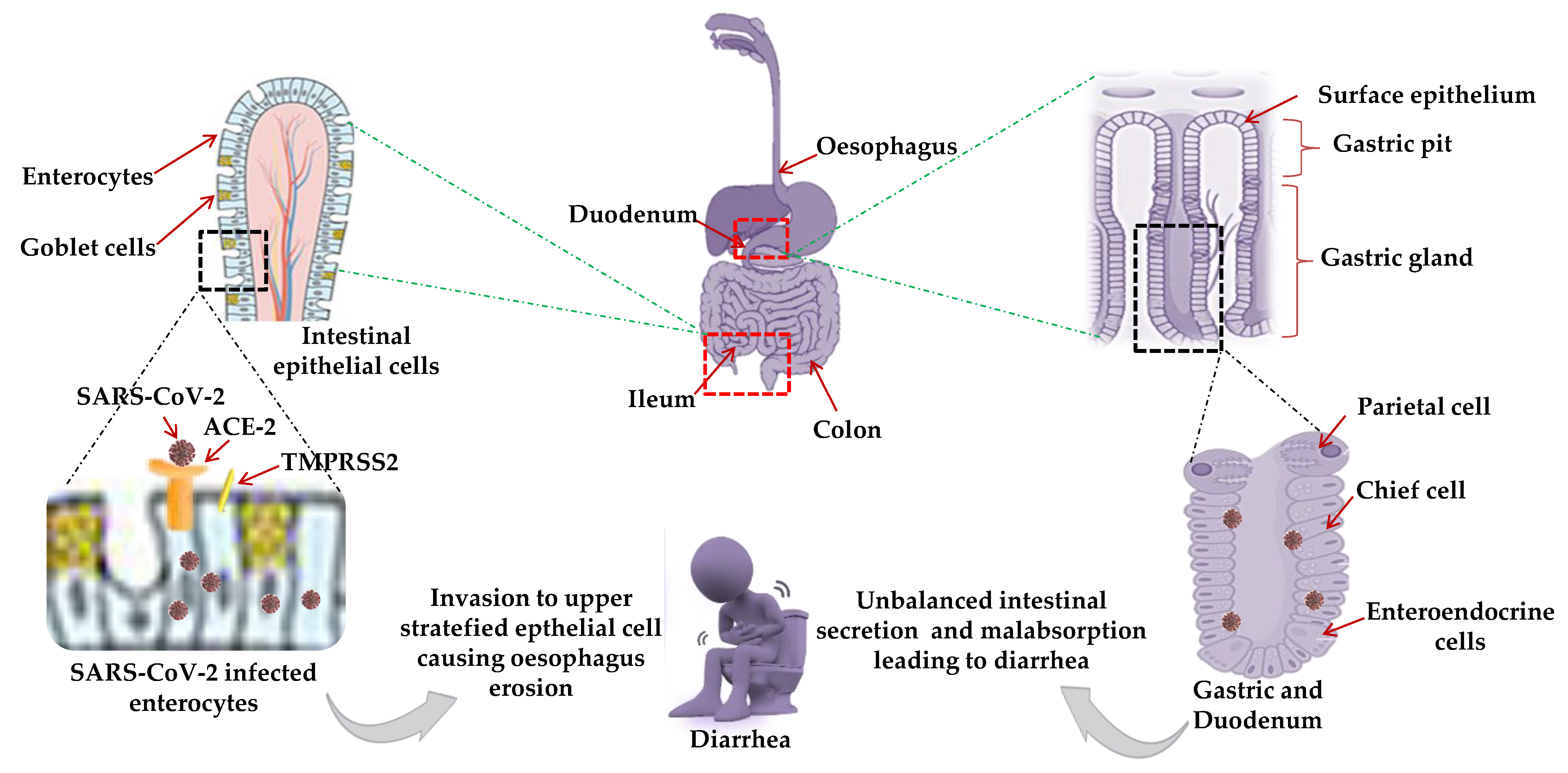
Possible Mechanism for GIT Manifestations
The causative mechanism for GIT manifestation in COVID-19 positive patients is not well studied. Single-cell transcriptomic analysis of GIT (stomach, colon, ileum, and esophagus) indicated high ACE2 expression in absorptive intestinal epithelial cells (IECs) in the ileum and colon [88]. The ACE2 receptor indirectly regulates intestinal inflammation whereas TMPRSS2 is crucial for viral fusion [89]. Various hypothetical models were predicted: Higher co-expression of ACE2 and TMPRSS2 and stronger binding efficiency of SARS-CoV-2 for ACE2, located on the mature enterocytes in the ileum and colon, triggers epithelial cell fusion by TMPRSS2 and TMPRSS4 (inducing S cleavage and enhancing the fusogenic activity of the virus) suggesting the viral invasion of enterocytes of the digestive tract and stratified epithelial cells of the esophagus, resulting in oesophageal erosion [90] (Figure 4).
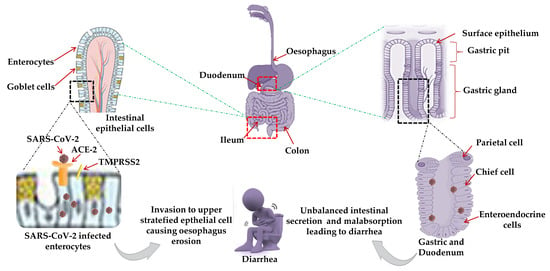
Figure 4.
A predictive model for gastrointestinal (GIT) manifestations: High ACE2 expression and stronger binding efficiency of SARS-CoV-2 for ACE2 in absorptive intestinal epithelial cells (IECs), enterocytes in the ileum and colon, indirectly regulate intestinal inflammation and oesophageal erosion suggested the viral invasion to enterocytes of the digestive tract and stratified epithelial cells of the esophagus. High-expression of ACE2 receptors in the glandular cells of the gastric and duodenal epithelium, or proximal and distal enterocytes, leads to unbalanced intestinal secretion and mal-absorption resulting in diarrhea as a common GIT manifestation. Red dotted square frame in the figures denotes the selected area for the magnified portion.
High expression and possible interaction of ACE2 receptors with SARS-CoV-2 in the glandular cells of gastric and duodenal epithelial cells, or in proximal and distal enterocytes, leads to unbalanced intestinal secretion and malabsorption resulting in diarrhea [91] The abundant and ubiquitous presence of ACE2 in human epithelial (small intestine) and endothelial cells might provide possible routes of transmission accounting for high transmission capacity.
9. Hematological Manifestations of SARS-CoV-2
Hematological parameters like alterations in immune cell population and coagulation factors in COVID-19 patients could suggest disease progression [92]. Lymphocytopenia seems to be the most common characteristic in adult patients with severe COVID-19 infection possibly due to the destruction of lymphoid organs [93]. Platelets are important in modulating inflammatory responses. A meta-analytical study showed the association of reduced platelets with COVID-19 severity, resulting in thrombocytopenia due to increased destruction or decreased platelet production [94,95]. Elevation in the levels of D-dimer is commonly observed in severe patients. Such patients are at high risk of developing thrombosis, endothelium damage, and hemorrhagic complications [96]. SARS-CoV-2 mediated endothelium injury, initiates the protective clotting cascade to minimize the internal injury, which subsequently forms undesirable internal blood clots resulting in thrombosis [97]. Angiogenesis associated ARDS was reported in the lung autopsies of 7 COVID-19 patients. It was marked by diffuse alveolar damage with perivascular T-cell infiltration and microthrombosis. Also, the severe endothelial injury was associated with intussuscepted vascular angiogenesis in the lungs [98]; 5% of large-vessel stroke incidences were reported among hospitalized patients in a single-centric study from China where coagulopathy and vascular endothelial dysfunction was the crucial presentation [52].
10. Unusual Manifestations of SARS-CoV-2
Subacute thyroiditis, oral lesions, large vessel stroke, rheumatologic skin disease, immune thrombocytopenia, endothelitis, pulmonary thromboembolism, pedo, and angiogenesis associated ARDS were also reported with SARS-CoV-2 as depicted in Table 4. Irregular oral lesions have been described as an early COVID-19 symptom, which needs to be proven with more pieces of evidence. Self-limited subacute thyroiditis (SAT) is characterized by neck pain, and thyroid dysfunction is usually preceded by an upper respiratory tract infection [99,100].

Table 4.
Unusual manifestations of SARS-CoV-2.
Previous studies showed cross-reaction of SARS-CoV-2 antigen and antibodies in patients with rheumatoid arthritis, systemic sclerosis, and systemic lupus erythematosus (SLE) [108] so there is the possibility of viral arthritis and musculoskeletal pain in COVID-19 patients, possibly due to posttranslational modification of peptides, or molecular mimicry activating T cells or epitope spreading due to T-cell associated damage by the virus leading to autoreactive T cells. SARS-CoV-2 through the ACE2 receptor directly infects the endothelial cell and facilitates the induction of endothelitis in several organs. Diffuse endothelial inflammation by host inflammatory response results in the recruitment of immune cells causing widespread endothelial dysfunction associated with apoptosis and pyroptosis. This results in shifting of vascular endothelium equilibrium towards vasoconstriction (microvascular dysfunction), resulting in inflammation with associated tissue edema, and a procoagulant state explaining the systemic impaired microcirculatory function in different vascular beds [109].
SARS-CoV-2 also directly attacks human epithelial cells of alveoli, large and small arteries, small intestine, and vascular endothelial cells. Counteracting the innate immune system activates and induces cytokine storms (IL-6) damaging the microvascular system. It activates the coagulation system while inhibiting fibrinolysis and anticoagulation systems that stimulate the liver to synthesize more thrombopoietin, fibrinogen leading to extensive thrombosis in microvessels [110]. Antiphospholipid antibodies result in endothelial injury, platelet activation, and thrombosis, with hypercoagulation. COVID-19 patients with high D-dimer levels and hypercoagulable state were associated with sudden onset of oxygen deterioration, respiratory distress, and reduced blood pressure resulting in pulmonary thromboembolism (PTE) [111].
11. COVID-19 in Immunocompromised Solid-Organ Transplant Recipients
Solid-organ transplant (SOT) recipients are high-risk individuals, usually on immunosuppressive therapy. Interestingly, in 2003 SARS-CoV in 2003 and 2012 MERS-CoV pandemic, SOT recipients did not appear to be associated with adverse outcomes. The role of different immunosuppressive agents such as calcineurin inhibitors and intravenous immunoglobulin (IVIG) in COVID-19 disease has not been established due to limited data on COVID-19 in transplant recipients. The typical presentation of COVID-19 in SOT recipients is the classic triad of fever, fatigue, and dry cough. A 75-year-old male and a 52-year-old female at 120 and 8 months post-transplant, respectively were diagnosed with stable graft function in males and AKI in females respectively. Extensive bilateral ground-glass opacities were the common lung abnormality reported in both cases [112].
A case of a 50-year-old COVID-19 positive man with 3rd kidney transplant recipient with IgA nephropathy induced end-stage renal disease manifested with the gastrointestinal viral disease (3–5%) and fever, further progressing to respiratory symptoms in 48 h [113]. A 39-year-old diabetic dual-organ (heart/kidney) transplant recipient positive for COVID-19 had a mild clinical course with minimal supportive care with no evidence of any graft rejection despite being on three immunosuppressive agents. The patient had additional risk factors of hypertension, diabetes mellitus, and morbid obesity, lymphopenia, elevated CRP, IL-6, D-dimer, and troponin I levels [114]. Li et al. [115] reported two heart transplant recipients with COVID-19 from Wuhan, were successfully treated, and survived.
12. Co-Infections with COVID-19: Viral, Bacterial, and Fungal
Diagnosing co-infections is complex owing to the clinical conditions of the infected patients [116]. During the 2003 SARS-CoV outbreak, invasive pulmonary aspergillosis was reported in only 4 among the 8422 probable SARS cases [117]. The risk of developing invasive pulmonary aspergillosis in COVID-19 patients is high as described in France where 9 out of 27 (33%) COVID-19 patients with invasive pulmonary aspergillosis admitted to an intensive care unit (ICU) [118] and 5 in Germany (26% of 19 admitted) proved in histopathology of autopsy [119]. Zhou et al. [120] showed that 50% of patients with COVID-19 died due to secondary bacterial infections. Patients with chronic obstructive pulmonary disease (COPD) will have underlying chronic bacterial infections before SARS-CoV-2 infection. Wang et al. [121] reported a case of a 37-year-old man, from Wuhan infected by SARS-CoV-2 and human immunodeficiency virus (HIV) simultaneously, highlighting the co-infection might damage T lymphocytes, impairing the immune system, B-cell dysfunction resulting in abnormal polyclonal activation and prolongation of the disease process (2 months). Chest CT showing multiple infiltrations in both lungs while nasopharyngeal swab positivity confirmed the SARS-CoV-2 infection, accompanied by dyspnea, chest pain, and palpitation. The significant decrease in the total number of immune cells i.e., B cells, T cells, and NK cells were also correlated with COVID-19 severity.
13. Advancements in Vaccine Research
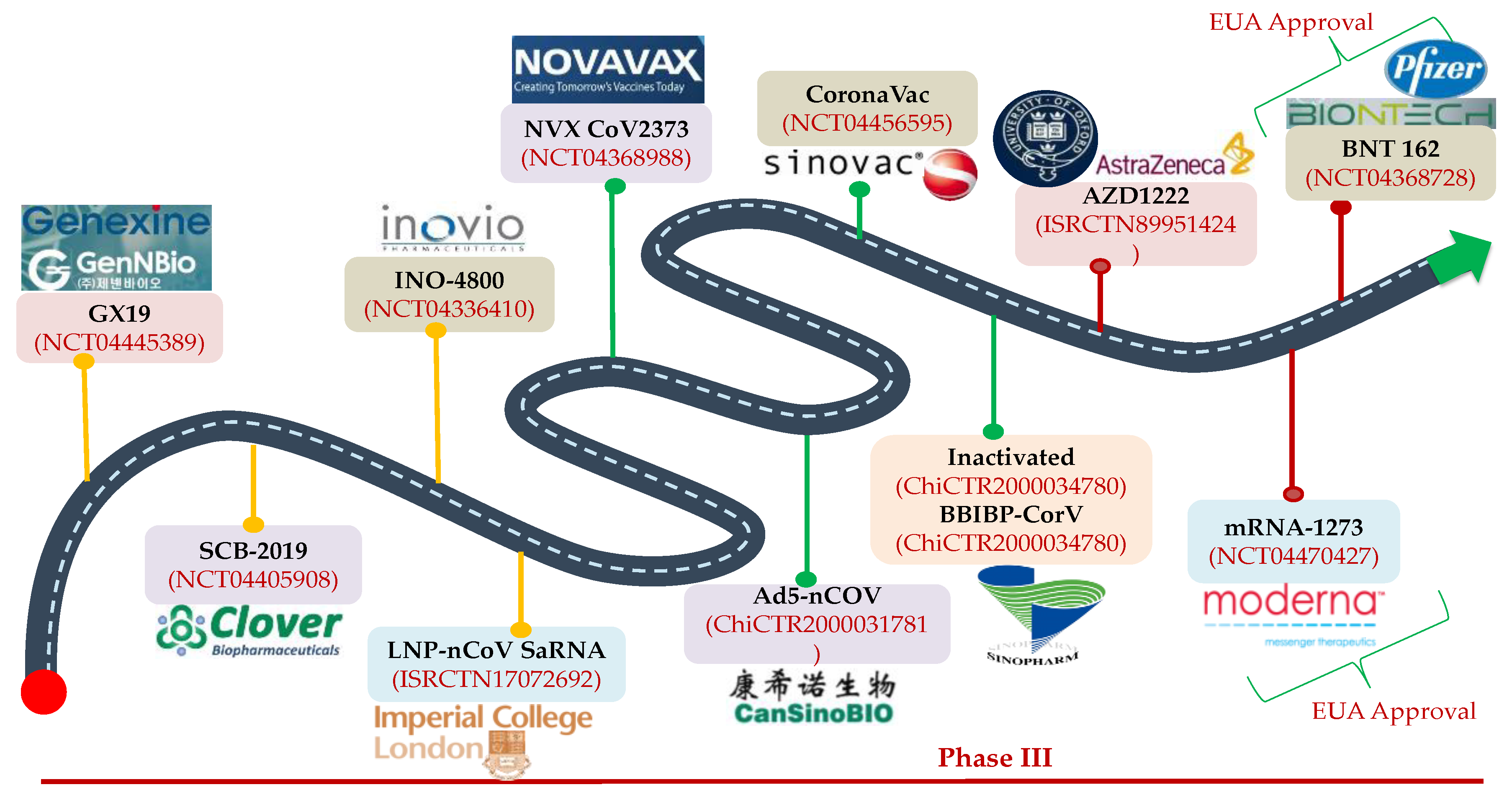
As per the draft landscape of COVID-19 [122] dated 15 January 2021; 63 candidate vaccines are in line with clinical evaluations with 13 vaccines currently at phase 3 trial. Two mRNA vaccines i.e., 3LNP-mRNA by Pfizer-BioNTech and RNA LNP encapsulated mRNA vaccine jointly by Moderna and National Institute of Health (NIH) demonstrated an efficacy of 95% and were recently approved for the emergency use under the Emergency Use Authorization (EUA) by the US Food and Drug Administration (FDA). Another promising vaccine i.e., ChAdOx1 (chimpanzee adenovirus vaccine vector) with comparable efficacy has been developed by AstraZeneca with Oxford University, which is a non-replicating version of adenovirus containing the genetic sequence of surface spike protein which is produced after vaccination and prime the immune system to attack against the SARS-CoV-2 viral infection.
The other important vaccine candidates undergoing clinical trials are the inactivated SARS-CoV-2 vaccines (Vero cells) developed by Sinopharm in collaboration with China National Biotec Group Corporation and Wuhan Institute of Biological Products, inactivated SARS-CoV-2 vaccines by Sinovac Research and Development Co. Ltd., Beijing, China and Gam-COVID-Vac Adeno-based (rAd26-S+rAdS-S) by Gamaleya Research Institute, Moscow, Russia etc. and these are depicted in Figure 5. Recently, two vaccine candidates were approved in India for clinical trials. Bharat Biotech International Limited developed an indigenous inactivated BBV152 (COVAXIN) COVID vaccine candidate with the collaborative work of the National Institute of Virology and Indian Council of Medical Research. The other one is ZyCov-D from Zydus Cadila, Ahmedabad, India which is also promising. India is also working with FluGen, Madison, USA and the University of Wisconsin-Madison, Madison, USA on an intranasal vaccine called CoroFlu with the S gene of SARS-CoV-2 insertion, built on the backbone of M2sr, a self-limiting version of influenza virus that induces immunity against COVID-19 and influenza (expressing H protein), lacking the M2 gene by restricting the replication with one cycle only. Besides, more than 173 vaccine candidates are in the pre-clinical stage. Considering the efforts, and the preliminary results from the various studies, hopefully by early 2021 we may have an approved effective vaccine available for human use to control the pandemic.
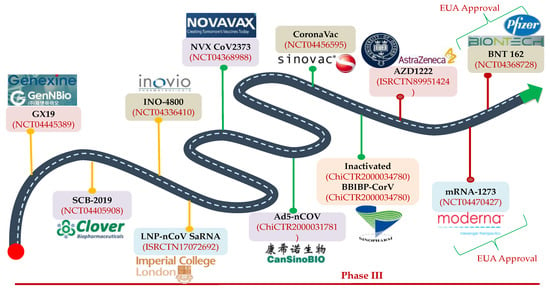
Figure 5.
Landscape representation of COVID-19 vaccine candidates in phase III clinical trials: BNT162b2 and mRNA 1273 vaccines are in the forefront and have been granted the Emergency Use Authorization (EUA) status. Adeno based vaccine by AstraZeneca is also the promising vaccines that may be soon approved for emergency use. Other COVID-19 vaccine players are Sinovac Biotech. Ltd (Beijing, China), CasSin Biologics Inc. (Tianjin, China), Novavax (Maryland, US), Inovio (San Diego, CA, US), Clover Biopharmaceuticals (Zhejiang, China), and GenNBio Inc. (Daegu, South Korea).
14. Conclusions
Since the emergence of COVID-19, the understanding of the clinical presentation of this disease is that it evolves with extrapulmonary involvement. Limited but unusual clinical cases involving the eyes, central nervous system, kidney, and liver suffice the organotropism of SARS-CoV-2. The probable explanation is the ubiquitous presence of ACE2 receptors in the various specialized cells of different organs which facilitates the binding and entry of SARS-CoV-2 inside the different cells. Unrestricted viral replication inside the cell releases the infectious virions from the cell resulting in cellular damage and eliciting the cytokine storm. The COVID-19 extra-pulmonary manifestations such as acute encephalitis in the brain, rashes on the dermis, acute renal and hepatic injury, conjunctivitis in the eyes, blood clots in the blood vessels, and loss of smell and taste are attributed by SARS-CoV-2. Understanding the different mechanisms causing organ-specific injury by SARS-CoV-2 and the route through which the virus transfers to the different locations will help the clinicians and scientists to design the treatment modality considering the critical situation of the severe COVID-19 patients. Such patients admitted to ICUs need critical monitoring of the functioning of different organs in addition to supportive oxygen therapy and antiviral administration. This will ultimately help to reduce the mortality related to COVID-19 induced acute respiratory distress syndrome and multiorgan failure until the world finds an effective and FDA-approved COVID-19 vaccine.
Author Contributions
Conceptualization, V.T. and R.K.R.; Collection of information, V.T., R.K.R., P.K. and S.K.S.; Planning, V.T., R.K.R., P.K., S.K.B. and S.M.; Writing-original draft preparation, V.T., R.K.R., I.B. and G.K.M.; Formal analysis, V.T., R.K.R., S.K.B., M.D., D.Y., and S.M.; Writing—review and editing, V.T., R.K.R., S.K.S., P.K., I.B., G.K.M., S.K.B., M.D., D.Y., and S.M.; Supervision, R.K.R., S.K.S. and S.K.B. All authors have read and approved the final submitted version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
The authors’ would like to thank the administrative support from the Department of Virology, PGIMER, Chandigarh.
Conflicts of Interest
The authors declare no conflict of interest in the submitted manuscript.
References
- Coronavirus Update (Live): 94,993,884 Cases and 2,031,875 Deaths from COVID-19 Virus Pandemic—Worldometer. Available online: https://www.worldometers.info/coronavirus/ (accessed on 17 January 2021).
- Cucinotta, D.; Vanelli, M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [CrossRef] [PubMed]
- Petersen, E.; Koopmans, M.; Go, U.; Hamer, D.H.; Petrosillo, N.; Castelli, F.; Storgaard, M.; Khalili, S.A.; Simonsen, L. Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics. Lancet Infect. Dis. 2020, 20, e238–e244. [Google Scholar] [CrossRef]
- Wang, C.; Horby, P.W.; Hayden, F.G.; Gao, G.F. A novel coronavirus outbreak of global health concern. Lancet 2020, 395, 470–473. [Google Scholar] [CrossRef]
- Corman, V.M.; Muth, D.; Niemeyer, D.; Drosten, C. Hosts and Sources of Endemic Human Coronaviruses. In Advances in Virus Research; Academic Press Inc.: New York, NY, USA, 2018; Volume 100, pp. 163–188. [Google Scholar]
- Gralinski, L.E.; Baric, R.S. Molecular pathology of emerging coronavirus infections. J. Pathol. 2015, 235, 185–195. [Google Scholar] [CrossRef] [PubMed]
- Neerukonda, S.N.; Katneni, U. A Review on SARS-CoV-2 Virology, Pathophysiology, Animal Models, and Anti-Viral Interventions. Pathogens 2020, 9, 426. [Google Scholar] [CrossRef]
- Xia, S.; Zhu, Y.; Liu, M.; Lan, Q.; Xu, W.; Wu, Y.; Ying, T.; Liu, S.; Shi, Z.; Jiang, S.; et al. Fusion mechanism of 2019-nCoV and fusion inhibitors targeting HR1 domain in spike protein. Cell. Mol. Immunol. 2020, 17, 765–767. [Google Scholar] [CrossRef]
- Zhang, C.; Wu, Z.; Li, J.W.; Zhao, H.; Wang, G.Q. Cytokine release syndrome in severe COVID-19: Interleukin-6 receptor antagonist tocilizumab may be the key to reduce mortality. Int. J. Antimicrob. Agents 2020, 55. [Google Scholar] [CrossRef]
- Wu, Z.; McGoogan, J.M. Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72314 Cases from the Chinese Center for Disease Control and Prevention. JAMA J. Am. Med. Assoc. 2020, 323, 1239–1242. [Google Scholar] [CrossRef]
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA J. Am. Med. Assoc. 2020, 323, 1061–1069. [Google Scholar] [CrossRef]
- Gandhi, M.; Yokoe, D.S.; Havlir, D.V. Asymptomatic Transmission, the Achilles’ Heel of Current Strategies to Control Covid-19. N. Engl. J. Med. 2020, 382, 2158–2160. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Pei, S.; Chen, B.; Song, Y.; Zhang, T.; Yang, W.; Shaman, J. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2). Science 2020, 368, 489–493. [Google Scholar] [CrossRef] [PubMed]
- Madjid, M.; Safavi-Naeini, P.; Solomon, S.D.; Vardeny, O. Potential Effects of Coronaviruses on the Cardiovascular System: A Review. JAMA Cardiol. 2020, 5, 831–840. [Google Scholar] [CrossRef] [PubMed]
- Rothan, H.A.; Byrareddy, S.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J. Autoimmun. 2020, 109. [Google Scholar] [CrossRef]
- Li, Y.C.; Bai, W.Z.; Hashikawa, T. The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients. J. Med. Virol. 2020, 92, 552–555. [Google Scholar] [CrossRef]
- Yeo, C.; Kaushal, S.; Yeo, D. Enteric involvement of coronaviruses: Is faecal–oral transmission of SARS-CoV-2 possible? Lancet Gastroenterol. Hepatol. 2020, 5, 335–337. [Google Scholar] [CrossRef]
- Sahin, A.R. 2019 Novel Coronavirus (COVID-19) Outbreak: A Review of the Current Literature. Eurasian J. Med. Oncol. 2020. [Google Scholar] [CrossRef]
- Tang, Y.W.; Schmitz, J.E.; Persing, D.H.; Stratton, C.W. Laboratory diagnosis of COVID-19: Current issues and challenges. J. Clin. Microbiol. 2020, 58. [Google Scholar] [CrossRef]
- Recalcati, S. Cutaneous manifestations in COVID-19: A first perspective. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e212–e213. [Google Scholar] [CrossRef]
- Guan, W.; Ni, Z.; Hu, Y.; Liang, W.; Ou, C.; He, J.; Liu, L.; Shan, H.; Lei, C.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- Fernandez-Nieto, D.; Ortega-Quijano, D.; Segurado-Miravalles, G.; Pindado-Ortega, C.; Prieto-Barrios, M.; Jimenez-Cauhe, J. Comment on: Cutaneous manifestations in COVID-19: A first perspective. Safety concerns of clinical images and skin biopsies. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e252–e254. [Google Scholar] [CrossRef] [PubMed]
- Marzano, A.V.; Genovese, G.; Fabbrocini, G.; Pigatto, P.; Monfrecola, G.; Piraccini, B.M.; Veraldi, S.; Rubegni, P.; Cusini, M.; Caputo, V.; et al. Varicella-like exanthem as a specific COVID-19–associated skin manifestation: Multicenter case series of 22 patients. J. Am. Acad. Dermatol. 2020, 83, 280–285. [Google Scholar] [CrossRef] [PubMed]
- Joob, B.; Wiwanitkit, V. COVID-19 can present with a rash and be mistaken for dengue. J. Am. Acad. Dermatol. 2020, 82, e177. [Google Scholar] [CrossRef] [PubMed]
- Estébanez, A.; Pérez-Santiago, L.; Silva, E.; Guillen-Climent, S.; García-Vázquez, A.; Ramón, M.D. Cutaneous manifestations in COVID-19: A new contribution. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e250–e251. [Google Scholar] [CrossRef] [PubMed]
- Joob, B.; Wiwanitkit, V. Reply to: ‘Various forms of skin rash in COVID-19: Petechial rash in a patient with COVID-19 infection’. J. Am. Acad. Dermatol. 2020, 83, e143. [Google Scholar] [CrossRef]
- Cai, Q.; Huang, D.; Ou, P.; Yu, H.; Zhu, Z.; Xia, Z.; Su, Y.; Ma, Z.; Zhang, Y.; Li, Z.; et al. COVID-19 in a designated infectious diseases hospital outside Hubei Province, China. Allergy Eur. J. Allergy Clin. Immunol. 2020, 75, 1742–1752. [Google Scholar] [CrossRef]
- Zhang, B.; Zhou, X.; Qiu, Y.; Song, Y.; Feng, F.; Feng, J.; Song, Q.; Jia, Q. Clinical characteristics of 82 cases of death from COVID-19. PLoS ONE 2020, 15, e0235458. [Google Scholar] [CrossRef]
- Chai, X.; Hu, L.; Zhang, Y.; Han, W.; Lu, Z.; Ke, A.; Zhou, J.; Shi, G.; Fang, N.; Fan, J.; et al. Specific ACE2 expression in cholangiocytes may cause liver damage after 2019-nCoV infection. bioRxiv 2020. [Google Scholar] [CrossRef]
- Wen Seow, J.J.; Pai, R.; Mishra, A.; Shepherdson, E.; Lim Hon, T.K.; Goh Brian, K.P.; Chan Jerry, K.Y.; Chow Pierce, K.H.; Ginhoux, F.; DasGupta, R.; et al. scRNA-seq reveals ACE2 and TMPRSS2 expression in TROP2 + Liver Progenitor Cells: Implications in COVID-19 associated Liver Dysfunction. bioRxiv 2020. [Google Scholar] [CrossRef]
- Zhao, B.; Ni, C.; Gao, R.; Wang, Y.; Yang, L.; Wei, J.; Lv, T.; Liang, J.; Zhang, Q.; Xu, W.; et al. Recapitulation of SARS-CoV-2 infection and cholangiocyte damage with human liver ductal organoids. Protein Cell 2020, 11, 771–775. [Google Scholar] [CrossRef]
- Zhang, C.; Shi, L.; Wang, F.S. Liver injury in COVID-19: Management and challenges. Lancet Gastroenterol. Hepatol. 2020, 5, 428–430. [Google Scholar] [CrossRef]
- Xu, Z.; Shi, L.; Wang, Y.; Zhang, J.; Huang, L.; Zhang, C.; Liu, S.; Zhao, P.; Liu, H.; Zhu, L.; et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020, 8, 420–422. [Google Scholar] [CrossRef]
- Liu, J.; Li, S.; Liu, J.; Liang, B.; Wang, X.; Wang, H.; Li, W.; Tong, Q.; Yi, J.; Zhao, L.; et al. Longitudinal characteristics of lymphocyte responses and cytokine profiles in the peripheral blood of SARS-CoV-2 infected patients. EBioMedicine 2020, 55. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.; O’Kane, A.M.; Peng, H.; Bi, Y.; Motriuk-Smith, D.; Ren, J. SARS-CoV-2 and cardiovascular complications: From molecular mechanisms to pharmaceutical management. Biochem. Pharmacol. 2020, 178, 114114. [Google Scholar] [CrossRef] [PubMed]
- Bonow, R.O.; Fonarow, G.C.; O’Gara, P.T.; Yancy, C.W. Association of Coronavirus Disease 2019 (COVID-19) with Myocardial Injury and Mortality. JAMA Cardiol. 2020, 5, 751–753. [Google Scholar] [CrossRef]
- Inciardi, R.M.; Lupi, R.; Zaccone, G.; Italia, L.; Raffo, M.; Tomasoni, D.; Cani, D.S.; Cerini, M.; Farina, D.; Gavazzi, E.; et al. Cardiac Involvement in a Patient with Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 819–824. [Google Scholar] [CrossRef]
- Han, H.; Xie, L.; Liu, R.; Yang, J.; Liu, F.; Wu, K.; Chen, L.; Hou, W.; Feng, Y.; Zhu, C. Analysis of heart injury laboratory parameters in 273 COVID-19 patients in one hospital in Wuhan, China. J. Med. Virol. 2020, 92, 819–823. [Google Scholar] [CrossRef]
- Vidovich, M.I. Transient Brugada-Like Electrocardiographic Pattern in a Patient with COVID-19. JACC Case Rep. 2020, 2, 1245–1249. [Google Scholar] [CrossRef]
- Sorgente, A.; Capulzini, L.; Brugada, P. The Known Into the Unknown. JACC Case Rep. 2020, 2, 1250–1251. [Google Scholar] [CrossRef]
- Chen, L.; Li, X.; Chen, M.; Feng, Y.; Xiong, C. The ACE2 expression in human heart indicates new potential mechanism of heart injury among patients infected with SARS-CoV-2. Cardiovasc. Res. 2020, 116, 1097–1100. [Google Scholar] [CrossRef]
- Zheng, Y.Y.; Ma, Y.T.; Zhang, J.Y.; Xie, X. COVID-19 and the cardiovascular system. Nat. Rev. Cardiol. 2020, 17, 259–260. [Google Scholar] [CrossRef] [PubMed]
- Bilimoria, J.; Singh, H. The Angiopoietin ligands and Tie receptors: Potential diagnostic biomarkers of vascular disease. J. Recept. Signal Transduct. 2019, 39, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Desforges, M.; Coupanec, A.L.; Dubeau, P.; Bourgouin, A.; Lajoie, L.; Dube, M.; Talbot, P.J. Human coronaviruses and other respiratory viruses: Underestimated opportunistic pathogens of the central nervous system? Viruses 2019, 12, 14. [Google Scholar] [CrossRef] [PubMed]
- Kabbani, N.; Olds, J.L. Does COVID19 Infect the Brain? If So, Smokers Might Be at a Higher Risk. Mol. Pharmacol. 2020, 97, 351–353. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Zhang, M.; Wang, J.; Gao, J. Sars-Cov-2: Underestimated damage to nervous system. Travel Med. Infect. Dis. 2020, 36. [Google Scholar] [CrossRef]
- Poyiadji, N.; Shahin, G.; Noujaim, D.; Stone, M.; Patel, S.; Griffith, B. COVID-19-associated acute hemorrhagic necrotizing encephalopathy: Imaging features. Radiology 2020, 296, E119–E120. [Google Scholar] [CrossRef]
- Miller, E.H.; Namale, V.S.; Kim, C.; Dugue, R.; Waldrop, G.; Ciryam, P.; Chong, A.M.; Zucker, J.; Miller, E.C.; Bain, J.M.; et al. Cerebrospinal Analysis in Patients With COVID-19. Open Forum Infect. Dis. 2020, 7. [Google Scholar] [CrossRef]
- Wu, Y.; Xu, X.; Chen, Z.; Duan, J.; Hashimoto, K.; Yang, L.; Liu, C.; Yang, C. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav. Immun. 2020, 87, 18–22. [Google Scholar] [CrossRef]
- Mao, L.; Jin, H.; Wang, M.; Hu, Y.; Chen, S.; He, Q.; Chang, J.; Hong, C.; Zhou, Y.; Wang, D.; et al. Neurologic Manifestations of Hospitalized Patients with Coronavirus Disease 2019 in Wuhan, China. JAMA Neurol. 2020, 77, 683–690. [Google Scholar] [CrossRef]
- Li, Y.; Li, M.; Wang, M.; Zhou, Y.; Chang, J.; Xian, Y.; Wang, D.; Mao, L.; Jin, H.; Hu, B. Acute cerebrovascular disease following COVID-19: A single center, retrospective, observational study. Stroke Vasc. Neurol. 2020, 5, 279–284. [Google Scholar] [CrossRef]
- Sharifi-Razavi, A.; Karimi, N.; Rouhani, N. COVID-19 and intracerebral haemorrhage: Causative or coincidental? New Microbes New Infect. 2020, 35, 100669. [Google Scholar] [CrossRef] [PubMed]
- Moriguchi, T.; Harii, N.; Goto, J.; Harada, D.; Sugawara, H.; Takamino, J.; Ueno, M.; Sakata, H.; Kondo, K.; Myose, N.; et al. A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. Int. J. Infect. Dis. 2020, 94, 55–58. [Google Scholar] [CrossRef] [PubMed]
- Ye, M.; Ren, Y.; Lv, T. Encephalitis as a clinical manifestation of COVID-19. Brain Behav. Immun. 2020, 88, 945–946. [Google Scholar] [CrossRef] [PubMed]
- Baig, A.M.; Khaleeq, A.; Ali, U.; Syeda, H. Evidence of the COVID-19 Virus Targeting the CNS: Tissue Distribution, Host-Virus Interaction, and Proposed Neurotropic Mechanisms. ACS Chem. Neurosci. 2020, 11, 995–998. [Google Scholar] [CrossRef] [PubMed]
- Portals of Viral Entry into the Central Nervous System. In The Blood-Brain Barrier in Health and Disease, Volume Two; CRC Press: Boca Raton, FL, USA, 2015; pp. 37–61.
- Saavedra, J.M. Brain angiotensin II: New developments, unanswered questions and therapeutic opportunities. Cell. Mol. Neurobiol. 2005, 25, 485–512. [Google Scholar] [CrossRef]
- Butowt, R.; Bilinska, K. SARS-CoV-2: Olfaction, Brain Infection, and the Urgent Need for Clinical Samples Allowing Earlier Virus Detection. ACS Chem. Neurosci. 2020. [Google Scholar] [CrossRef]
- Wan, S.; Yi, Q.; Fan, S.; Lv, J.; Zhang, X.; Guo, L.; Lang, C.; Xiao, Q.; Xiao, K.; Yi, Z.; et al. Characteristics of lymphocyte subsets and cytokines in peripheral blood of 123 hospitalized patients with 2019 novel coronavirus pneumonia (NCP). medRxiv 2020. [Google Scholar] [CrossRef]
- Mehta, P.; McAuley, D.F.; Brown, M.; Sanchez, E.; Tattersall, R.S.; Manson, J.J. COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet 2020, 395, 1033–1034. [Google Scholar] [CrossRef]
- Pei, G.; Zhang, Z.; Peng, J.; Liu, L.; Zhang, C.; Yu, C.; Ma, Z.; Huang, Y.; Liu, Y.; Yao, Y.; et al. Renal involvement and early prognosis in patients with COVID-19 pneumonia. J. Am. Soc. Nephrol. 2020, 31, 1157–1165. [Google Scholar] [CrossRef]
- Cheng, Y.; Luo, R.; Wang, K.; Zhang, M.; Wang, Z.; Dong, L.; Li, J.; Yao, Y.; Ge, S.; Xu, G. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020, 97, 829–838. [Google Scholar] [CrossRef]
- Gabarre, P.; Dumas, G.; Dupont, T.; Darmon, M.; Azoulay, E.; Zafrani, L. Acute kidney injury in critically ill patients with COVID-19. Intensive Care Med. 2020, 46, 1339–1348. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Zhu, A.; Li, H.; Zheng, K.; Zhuang, Z.; Chen, Z.; Shi, Y.; Zhang, Z.; Chen, S.; Liu, X.; et al. Isolation of infectious SARS-CoV-2 from urine of a COVID-19 patient. Emerg. Microbes Infect. 2020, 9, 991–993. [Google Scholar] [CrossRef] [PubMed]
- Ling, Y.; Xu, S.B.; Lin, Y.X.; Tian, D.; Zhu, Z.Q.; Dai, F.H.; Wu, F.; Song, Z.G.; Huang, W.; Chen, J.; et al. Persistence and clearance of viral RNA in 2019 novel coronavirus disease rehabilitation patients. Chin. Med. J. 2020, 133, 1039–1043. [Google Scholar] [CrossRef]
- Puelles, V.G.; Lutgehetmann, M.; Lindenmeyer, M.T.; Sperhake, J.P.; Wong, M.N.; Allweiss, L.; Chilla, S.; Heinemann, A.; Wanner, N.; Liu, S.; et al. Multiorgan and Renal Tropism of SARS-CoV-2. N. Engl. J. Med. 2020, 383, 590–592. [Google Scholar] [CrossRef] [PubMed]
- Diao, B.; Wang, C.; Wang, R.; Feng, Z.; Tan, Y.; Wang, H.; Wang, C.; Liu, L.; Liu, Y.; Wang, G.; et al. Human kidney is a target for novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. medRxiv 2020. [Google Scholar] [CrossRef]
- Wang, R.; Liao, C.; He, H.; Hu, C.; Wei, Z.; Hong, Z.; Zhang, C.; Liao, M.; Shui, H. COVID-19 in Hemodialysis Patients: A Report of 5 Cases. Am. J. Kidney Dis. 2020, 76, 141–143. [Google Scholar] [CrossRef]
- Wang, H. Maintenance Hemodialysis and COVID-19: Saving Lives With Caution, Care, and Courage. Kidney Med. 2020, 2, 365–366. [Google Scholar] [CrossRef]
- He, Q.; Mok, T.N.; Yun, L.; He, C.; Li, J.; Pan, J. Single-cell RNA sequencing analysis of human kidney reveals the presence of ACE2 receptor: A potential pathway of COVID-19 infection. Mol. Genet. Genom. Med. 2020, 8. [Google Scholar] [CrossRef]
- Lin, W.; Hu, L.; Zhang, Y.; Ooi, J.D.; Meng, T.; Jin, P.; Sing, X.; Peng, L.; Song, L.; Xiao, Z.; et al. Single-cell Analysis of ACE2 Expression in Human Kidneys and Bladders Reveals a Potential Route of 2019-nCoV Infection. bioRxiv 2020. [Google Scholar] [CrossRef]
- Fan, C.; Li, K.; Ding, Y.; Lu, W.; Wang, J. ACE2 Expression in Kidney and Testis May Cause Kidney and Testis Damage after 2019-nCoV Infection. MedRxiv 2020. [Google Scholar] [CrossRef]
- Husain-Syed, F.; Slutsky, A.S.; Ronco, C. Lung-kidney cross-talk in the critically ill patient. Am. J. Respir. Crit. Care Med. 2016, 194, 402–414. [Google Scholar] [CrossRef] [PubMed]
- Leung, W.K.; To, K.F.; Chan, P.K.S.; Chan, H.L.Y.; Wu, A.K.L.; Lee, N.; Yuen, K.Y.; Sung, J.J.Y. Enteric involvement of severe acute respiratory syndrome-associated coronavirus infection. Gastroenterology 2003, 1251011–1251017. [Google Scholar] [CrossRef]
- Holshue, M.L.; DeBolt, C.; Lindquist, S.; Lofy, K.H.; Wiesman, J.; Bruce, H.; Spitters, C.; Ericson, K.; Wilkerson, S.; Tural, A.; et al. First Case of 2019 Novel Coronavirus in the United States. N. Engl. J. Med. 2002, 382, 929–936. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.; Jiang, X.; Zhang, Z.; Huang, S.; Zhang, Z.; Fang, Z.; Gu, Z.; Gao, L.; Shi, H.; Mai, L.; et al. Gastrointestinal symptoms of 95 cases with SARS-CoV-2 infection. Gut 2020, 69, 997–1001. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Lou, J.; Bai, Y.; Wang, M. COVID-19 disease with positive fecal and negative pharyngeal and sputum viral tests. Am. J. Gastroenterol. 2020, 115, 790. [Google Scholar] [CrossRef] [PubMed]
- Wei, X.-S.; Wang, X.; Niu, Y.R.; Ye, L.L.; Peng, W.B.; Wang, Z.H.; Yang, W.B.; Yang, B.H.; Zhang, J.C.; Ma, W.L.; et al. Clinical Characteristics of SARS-CoV-2 Infected Pneumonia with Diarrhea. SSRN Electron. J. 2020. [Google Scholar] [CrossRef]
- Pan, L.; Mu, M.; Yang, P.; Sun, Y.; Wang, R.; Yan, J.; Li, P.; Hu, B.; Wang, J.; Hu, C.; et al. Clinical Characteristics of COVID-19 Patients With Digestive Symptoms in Hubei, China. Am. J. Gastroenterol. 2020, 115, 766–773. [Google Scholar] [CrossRef]
- Jin, X.; Lian, J.S.; Hu, J.H.; Gao, J.; Zheng, L.; Zhang, Y.M.; Hao, S.R.; Jia, H.Y.; Cai, H.; Zhang, X.L.; et al. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut 2020, 69, 1002–1009. [Google Scholar] [CrossRef]
- Luo, S.; Zhang, X.; Xu, H. Don’t Overlook Digestive Symptoms in Patients With 2019 Novel Coronavirus Disease (COVID-19). Clin. Gastroenterol. Hepatol. 2020, 18, 1636–1637. [Google Scholar] [CrossRef]
- Wu, Y.; Guo, C.; Tang, L.; Hong, Z.; Zhou, J.; Dong, X.; Yin, H.; Xiao, Q.; Tang, Y.; Qu, X.; et al. Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. Lancet Gastroenterol. Hepatol. 2020, 5, 434–435. [Google Scholar] [CrossRef]
- Xu, Y.; Li, X.; Zhu, B.; Liang, H.; Fang, C.; Gong, Y.; Guo, Q.; Sun, X.; Zhao, D.; Shen, J.; et al. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat. Med. 2020, 26, 502–505. [Google Scholar] [CrossRef] [PubMed]
- Elmunzer, B.J.; Spitzer, R.L.; Foster, L.D.; Merchant, A.A.; Howard, E.F.; Patel, V.A.; West, M.K.; Qayed, E.; Nustas, R.; Zakaria, A.; et al. Digestive Manifestations in Patients Hospitalized with COVID-19. Clin. Gastroenterol. Hepatol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Wölfel, R.; Corman, V.M.; Guggemos, W.; Seilmaier, M.; Zange, S.; Muller, M.A.; Niemeyer, D.; Jones, T.C.; Vollmar, P.; Rothe, C.; et al. Virological assessment of hospitalized patients with COVID-2019. Nature 2020, 581, 465–469. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Xu, Y.; Gao, R.; Lu, R.; Han, K.; Wu, G.; Tan, W. Detection of SARS-CoV-2 in Different Types of Clinical Specimens. JAMA J. Am. Med. Assoc. 2020, 323, 1843–1844. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Kang, Z.; Gong, H.; Xu, D.; Wang, J.; Li, Z.; Li, Z.; Cui, X.; Xiao, J.; Zhan, J.; et al. Digestive system is a potential route of COVID-19: An analysis of single-cell coexpression pattern of key proteins in viral entry process. Gut 2020, 69, 1010–1018. [Google Scholar] [CrossRef]
- Hashimoto, T.; Perlot, T.; Rehman, A.; Trichereay, J.; Ishiguro, H.; Paolino, M.; Sigl, V.; Hanada, T.; Hanada, R.; Lipinski, S.; et al. ACE2 links amino acid malnutrition to microbial ecology and intestinal inflammation. Nature 2012, 487, 477–481. [Google Scholar] [CrossRef]
- Hoffmann, M.; Kleine-Weber, H.; Schroeder, S.; Kruger, N.; Herrler, T.; Erichsen, S.; Schiergens, T.S.; Herrler, G.; Wu, N.H.; Nitsche, A.; et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020, 181, 271–280.e8. [Google Scholar] [CrossRef]
- Liang, W.; Feng, Z.; Rao, S.; Xiao, C.; Xue, X.; Lin, Z.; Zhang, Q.; Qi, W. Diarrhoea may be underestimated: A missing link in 2019 novel coronavirus. Gut 2020, 69, 1141–1143. [Google Scholar] [CrossRef]
- Słomka, A.; Kowalewski, M.; Żekanowska, E. Coronavirus disease 2019 (COVID–19): A short review on hematological manifestations. Pathogens 2020, 9, 493. [Google Scholar] [CrossRef]
- Ludvigsson, J.F. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. Int. J. Paediatr. 2020, 109, 1088–1095. [Google Scholar] [CrossRef]
- Xu, P.; Zhou, Q.; Xu, J. Mechanism of thrombocytopenia in COVID-19 patients. Ann. Hematol. 2020, 99, 1205–1208. [Google Scholar] [CrossRef] [PubMed]
- Lippi, G.; Plebani, M.; Henry, B.M. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: A meta-analysis. Clin. Chim. Acta 2020, 506, 2020. [Google Scholar] [CrossRef] [PubMed]
- Maier, C.L.; Truong, A.D.; Auld, S.C.; Polly, D.M.; Tanksley, C.L.; Duncan, A. COVID-19-associated hyperviscosity: A link between inflammation and thrombophilia? Lancet 2020, 395, 1758–1759. [Google Scholar] [CrossRef]
- Biswas, S.; Thakur, V.; Kaur, P.; Khan, A.; Kulshrestha, S.; Kumar, P. Blood clots in COVID-19 patients: Simplifying the curious mystery. Med. Hypotheses 2020, 146, 110371. [Google Scholar] [CrossRef]
- Ackermann, M.; Verleden, S.E.; Kuehnel, M.; Haverich, A.; Welte, T.; Laenger, F.; Vanstapel, A.; Werlein, C.; Stark, H.; Tzankov, A.; et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19. N. Engl. J. Med. 2020, 383, 120–128. [Google Scholar] [CrossRef]
- Wei, L.; Sun, S.; Xu, C.H.; Zhang, J.; Xu, Y.; Zhu, H.; Peh, S.C.; Korteweg, C.; McNutt, M.A.; Gu, J. Pathology of the thyroid in severe acute respiratory syndrome. Hum. Pathol. 2007, 38, 95–102. [Google Scholar] [CrossRef]
- Benbassat, C.A.; Olchovsky, D.; Tsvetov, G.; Shimon, I. Subacute thyroiditis: Clinical characteristics and treatment outcome in fifty-six consecutive patients diagnosed between 1999 and 2005. J. Endocrinol. Investig. 2007, 30, 631–635. [Google Scholar] [CrossRef]
- Chaux-Bodard, A.-G.; Deneuve, S.; Desoutter, A. Oral manifestation of Covid-19 as an inaugural symptom? J. Oral Med. Oral Surg. 2020, 26, 18. [Google Scholar] [CrossRef]
- Brancatella, A.; Ricci, D.; Viola, N.; Sgrò, D.; Santini, F.; Latrofa, F. Subacute Thyroiditis After Sars-COV-2 Infection. J. Clin. Endocrinol. Metab. 2020, 105, 2367–2370. [Google Scholar] [CrossRef]
- Oxley, T.J.; Mocco, J.; Majidi, S.; Kellner, C.P.; Shoirah, H.; Singh, I.P.; De Leacy, R.A.; Shigematsu, T.; Ladner, T.R.; Yaeger, K.A.; et al. Large-Vessel Stroke as a Presenting Feature of Covid-19 in the Young. N. Engl. J. Med. 2020, 382, e60. [Google Scholar] [CrossRef]
- Varga, Z.; Flammer, A.J.; Steiger, P.; Haberecker, M.; Andermatt, R.; Zinkernagel, A.S.; Mehra, M.R.; Schuepbach, R.A.; Ruschitzka, F.; Moch, H. Endothelial cell infection and endotheliitis in COVID-19. Lancet 2020, 395, 1417–1418. [Google Scholar] [CrossRef]
- Tsao, H.S.; Chason, H.M.; Fearon, D.M. Immune thrombocytopenia (ITP) in a pediatric patient positive for SARS-CoV-2. Pediatrics 2020, 146. [Google Scholar] [CrossRef]
- Zulfiqar, A.-A.; Lorenzo-Villalba, N.; Hassler, P.; Andrès, E. Immune Thrombocytopenic Purpura in a Patient with Covid-19. N. Engl. J. Med. 2020, 382, e43. [Google Scholar] [CrossRef]
- Nirenberg, M.S.; Del Mar Ruiz Herrera, M. Foot Manifestations in a COVID-19 Positive Patient: A Case Study. J. Am. Podiatr. Med. Assoc. 2020. [Google Scholar] [CrossRef]
- Arora, G.; Kassir, M.; Jafferany, M.; Galadari, H.; Lotti, T.; Satolli, F.; Sadoughifar, R.; Sitkowska, Z.; Goldust, M. The COVID-19 outbreak and rheumatologic skin diseases. Dermatol. Ther. 2020, 33. [Google Scholar] [CrossRef]
- Flammer, A.J.; Anderson, T.; Celermajer, D.S.; Creager, M.A.; Deanfield, J.; Ganz, P.; Hamburg, N.M.; Luscher, T.F.; Shechter, M.; Taddei, S.; et al. The assessment of endothelial function: From research into clinical practice. Circulation 2012, 126, 753–767. [Google Scholar] [CrossRef]
- Zhou, Y.; Fu, B.; Zheng, X.; Wang, D.; Zhao, C.; Qi, Y.; Sun, R.; Tian, Z.; Xu, X.; Wei, H. Aberrant pathogenic GM-CSF + T cells and inflammatory CD14+ CD16+ monocytes in severe pulmonary syndrome patients of a new coronavirus. Natl. Sci. Rev. 2020. [Google Scholar] [CrossRef]
- Danzi, G.B.; Loffi, M.; Galeazzi, G.; Gherbesi, E. Acute pulmonary embolism and COVID-19 pneumonia: A random association? Eur. Heart J. 2020, 41, 1858. [Google Scholar] [CrossRef]
- Gandolfini, I.; Delsante, M.; Fiaccadori, E.; Zaza, G.; Manenti, L.; Antoni, A.D.; Peruzzi, L.; Riella, L.V.; Cravedi, P.; Maggiore, U. COVID-19 in kidney transplant recipients. Am. J. Transpl. 2020, 20, 1941–1943. [Google Scholar] [CrossRef]
- Guillen, E.; Pineiro, G.J.; Revuelta, I.; Rodriguez, D.; Bodro, M.; Moreno, A.; Campistol, J.M.; Diekmann, F.; Ventura-Aguiar, P. Case report of COVID-19 in a kidney transplant recipient: Does immunosuppression alter the clinical presentation? Am. J. Transplant. 2002, 20, 1875–1878. [Google Scholar] [CrossRef]
- Hsu, J.J.; Gaynor, P.; Kamath, M.; Fan, A.; Al-Saffar, F.; Criz, D.; Nsair, A. COVID-19 in a high-risk dual heart and kidney transplant recipient. Am. J. Transplant. 2020, 20, 1911–1915. [Google Scholar] [CrossRef]
- Li, F.; Cai, J.; Dong, N. First cases of COVID-19 in heart transplantation from China. J. Heart Lung Transpl. 2020, 39, 496–497. [Google Scholar] [CrossRef]
- Cox, M.J.; Loman, N.; Bogaert, D.; O’Grady, J. Co-infections: Potentially lethal and unexplored in COVID-19. Lancet Microbe 2020, 1, e11. [Google Scholar] [CrossRef]
- Wang, H.; Ding, Y.; Li, X.; Yang, L.; Zhang, W.; Kang, W. Fatal Aspergillosis in a Patient with SARS Who Was Treated with Corticosteroids. N. Engl. J. Med. 2003, 349, 507–508. [Google Scholar] [CrossRef]
- Alanio, A.; Dellière, S.; Fodil, S.; Bretagne, S.; Mégarbane, B. Prevalence of putative invasive pulmonary aspergillosis in critically ill patients with COVID-19. Lancet Respir. Med. 2020, 8, e48–e49. [Google Scholar] [CrossRef]
- Koehler, P.; Cornely, A.A.; Bottiger, B.E.; Dusse, F.; Eichenauer, A.S.; Fuchs, F.; Hallek, M.; Jung, N.; Klein, F.; Persigehl, T.; et al. COVID-19 associated pulmonary aspergillosis. Mycoses 2002, 63, 528–534. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Wang, M.; Luo, L.; Bu, H.; Xia, H. One case of coronavirus disease 2019 (COVID-19) in a patient co-infected by HIV with a low CD4+ T-cell count. Int. J. Infect. Dis. 2020, 96, 148–150. [Google Scholar] [CrossRef]
- Draft Landscape of COVID-19 Candidate Vaccines. Available online: https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines (accessed on 18 January 2021).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).