Risk of Hospital Readmission among Older Patients Discharged from the Rehabilitation Unit in a Rural Community Hospital: A Retrospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patients
2.2. Recovery Rehabilitation Unit
2.3. Measurements
2.4. Statistical Analysis
2.5. Ethical Considerations
3. Results
3.1. Patient Characteristics
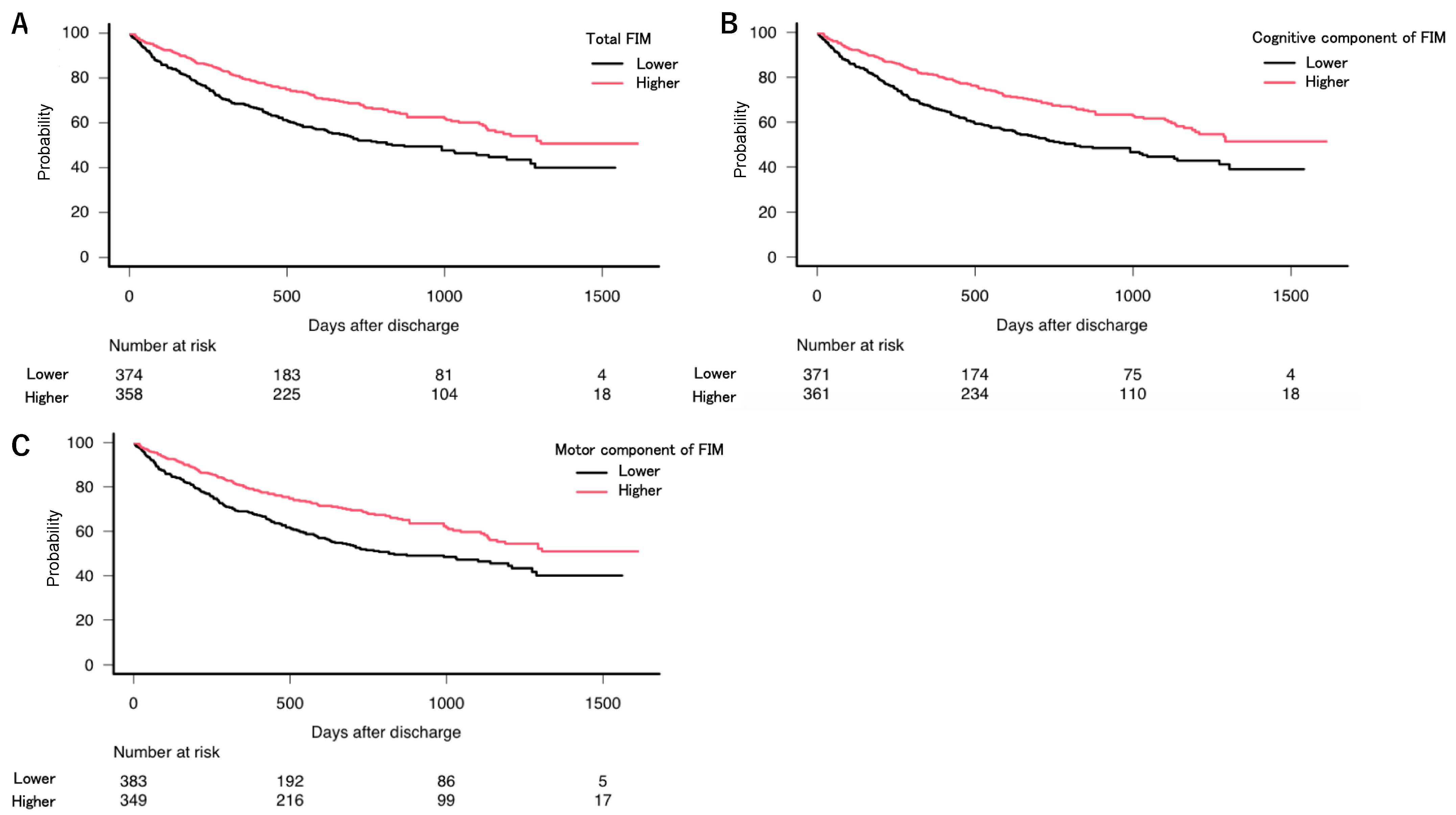
3.2. Regression Model Results
3.3. Reasons for Readmission to the Hospital
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hillier, S.; Inglis-Jassiem, G. Rehabilitation for Community-Dwelling People with Stroke: Home or Centre Based? A Systematic Review. Int. J. Stroke 2010, 5, 178–186. [Google Scholar] [CrossRef]
- Nguyen, T.A.; Page, A.; Aggarwal, A.; Henke, P. Social Determinants of Discharge Destination for Patients after Stroke with Low Admission FIM Instrument Scores. Arch. Phys. Med. Rehabil. 2007, 88, 740–744. [Google Scholar] [CrossRef] [PubMed]
- Prvu Bettger, J.A.; Stineman, M.G. Effectiveness of Multidisciplinary Rehabilitation Services in Postacute Care: State-of-the-Science. A Review. Arch. Phys. Med. Rehabil. 2007, 88, 1526–1534. [Google Scholar] [CrossRef] [PubMed]
- Wakabayashi, H.; Sakuma, K. Rehabilitation Nutrition for Sarcopenia with Disability: A Combination of Both Rehabilitation and Nutrition Care Management. J. Cachexia Sarcopenia Muscle 2014, 5, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Landers, S.H. Home Care: A Key to the Future of Family Medicine? Ann. Fam. Med. 2006, 4, 366–368. [Google Scholar] [CrossRef] [PubMed]
- Devi, R.; Martin, G.; Banerjee, J.; Butler, L.; Pattison, T.; Cruickshank, L.; Maries-Tillott, C.; Wilson, T.; Damery, S.; Meyer, J.; et al. Improving the Quality of Care in Care Homes Using the Quality Improvement Collaborative Approach: Lessons Learnt from Six Projects Conducted in the UK and The Netherlands. Int. J. Environ. Res. Public Health 2020, 17, 7601. [Google Scholar] [CrossRef] [PubMed]
- Ford, J.A.; Turley, R.; Porter, T.; Shakespeare, T.; Wong, G.; Jones, A.P.; Steel, N. Access to Primary Care for Socio-Economically Disadvantaged Older People in Rural Areas: A Qualitative Study. PLoS ONE 2018, 13, e0193952. [Google Scholar] [CrossRef]
- Ohta, R.; Ryu, Y.; Kitayuguchi, J.; Gomi, T.; Katsube, T. Challenges and Solutions in the Continuity of Home Care for Rural Older People: A Thematic Analysis. Home Health Care Serv. Q. 2020, 39, 126–139. [Google Scholar] [CrossRef]
- Dantas, I.; Santana, R.; Sarmento, J.; Aguiar, P. The Impact of Multiple Chronic Diseases on Hospitalizations for Ambulatory Care Sensitive Conditions. BMC. Health Serv. Res. 2016, 16, 348. [Google Scholar] [CrossRef]
- Ohta, R.; Maeki, N.; Maniwa, S.; Miyakoshi, K. Predicting Factors of Elderly Patients’ Discharge to Home After Rehabilitation in Rural Japan: A Retrospective Cohort Study. Rural Remote Health 2021, 21, 6406. [Google Scholar]
- Reidt, S.L.; Holtan, H.S.; Larson, T.A.; Thompson, B.; Kerzner, L.J.; Salvatore, T.M.; Adam, T.J. Interprofessional Collaboration to Improve Discharge from Skilled Nursing Facility to Home: Preliminary Data on Postdischarge Hospitalizations and Emergency Department Visits. J. Am. Geriatr. Soc. 2016, 64, 1895–1899. [Google Scholar] [CrossRef] [PubMed]
- Shih, S.L.; Gerrard, P.; Goldstein, R.; Mix, J.; Ryan, C.M.; Niewczyk, P.; Kazis, L.; Hefner, J.; Ackerly, D.C.; Zafonte, R.; et al. Functional Status Outperforms Comorbidities in Predicting Acute Care Readmissions in Medically Complex Patients. J. Gen. Intern. Med. 2015, 30, 1688–1695. [Google Scholar] [CrossRef] [PubMed]
- Slocum, C.; Gerrard, P.; Black-Schaffer, R.; Goldstein, R.; Singhal, A.; DiVita, M.A.; Ryan, C.M.; Mix, J.; Purohit, M.; Niewczyk, P.; et al. Functional Status Predicts Acute Care Readmissions from Inpatient Rehabilitation in the Stroke Population. PLoS ONE 2015, 10, e0142180. [Google Scholar] [CrossRef] [PubMed]
- Hoyer, E.H.; Needham, D.M.; Miller, J.; Deutschendorf, A.; Friedman, M.; Brotman, D.J. Functional Status Impairment Is Associated with Unplanned Readmissions. Arch. Phys. Med. Rehabil. 2013, 94, 1951–1958. [Google Scholar] [CrossRef]
- Hoyer, E.H.; Needham, D.M.; Atanelov, L.; Knox, B.; Friedman, M.; Brotman, D.J. Association of Impaired Functional Status at Hospital Discharge and Subsequent Rehospitalization. J. Hosp. Med. 2014, 9, 277–282. [Google Scholar] [CrossRef]
- Puts, M.T.E.; Toubasi, S.; Andrew, M.K.; Ashe, M.C.; Ploeg, J.; Atkinson, E.; Ayala, A.P.; Roy, A.; Rodríguez Monforte, M.; Bergman, H.; et al. Interventions to Prevent or Reduce the Level of Frailty in Community-Dwelling Older Adults: A Scoping Review of the Literature and International Policies. Age Ageing 2017, 46, 383–392. [Google Scholar] [CrossRef]
- Duner, A. Care Planning and Decision-Making in Teams in Swedish Elderly Care: A Study of Interprofessional Collaboration and Professional Boundaries. J. Interprof. Care 2013, 27, 246–253. [Google Scholar] [CrossRef]
- Chi, W.C.; Wolff, J.; Greer, R.; Dy, S. Multimorbidity and Decision-Making Preferences among Older Adults. Ann. Fam. Med. 2017, 15, 546–551. [Google Scholar] [CrossRef]
- Bookey-Bassett, S.; Markle-Reid, M.; Mckey, C.A.; Akhtar-Danesh, N. Understanding Interprofessional Collaboration in the Context of Chronic Disease Management for Older Adults Living in Communities: A Concept Analysis. J. Adv. Nurs. 2017, 73, 71–84. [Google Scholar] [CrossRef]
- Logue, E.; Smucker, W.; Regan, C. Admission Data Predict High Hospital Readmission Risk. J. Am. Board Fam. Med. 2016, 29, 50–59. [Google Scholar] [CrossRef] [PubMed]
- Hosking, F.J.; Carey, I.M.; DeWilde, S.; Harris, T.; Beighton, C.; Cook, D.G. Preventable Emergency Hospital Admissions Among Adults with Intellectual Disability in England. Ann. Fam. Med. 2017, 15, 462–470. [Google Scholar] [CrossRef] [PubMed]
- Roderick, P.; Low, J.; Day, R.; Peasgood, T.; Mullee, M.A.; Turnbull, J.C.; Villar, T.; Raftery, J. Stroke Rehabilitation After Hospital Discharge: A Randomized Trial Comparing Domiciliary and Day-Hospital Care. Age Ageing 2001, 30, 303–310. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yoon, D.H.; Hwang, S.S.; Lee, D.W.; Lee, C.G.; Song, W. Physical Frailty and Cognitive Functioning in Korea Rural Community-Dwelling Older Adults. J. Clin. Med. 2018, 7, 405. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.H.; Kim, B.R.; Nam, K.W.; Lee, S.Y.; Beom, J.; Lee, S.Y.; Suh, M.J.; Lim, J.Y. Effectiveness of a Home-Based Fragility Fracture Integrated Rehabilitation Management (FIRM) Program in Patients Surgically Treated for Hip Fractures. J. Clin. Med. 2020, 10, 18. [Google Scholar] [CrossRef]
- Ohta, R.; Ryu, Y.; Kataoka, D.; Sano, C. Effectiveness and Challenges in Local Self-Governance: Multifunctional Autonomy in Japan. Int. J. Environ. Res. Public Health 2021, 18, 574. [Google Scholar] [CrossRef] [PubMed]
- Onoue, H.; Koyama, T.; Zamami, Y.; Hagiya, H.; Tatebe, Y.; Mikami, N.; Shinomiya, K.; Kitamura, Y.; Hinotsu, S.; Sendo, T.; et al. Trends in Polypharmacy in Japan: A Nationwide Retrospective Study. J. Am. Geriatr. Soc. 2018, 66, 2267–2273. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A New Method of Classifying Prognostic Comorbidity in Longitudinal Studies: Development and Validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Shimizutani, S. The Future of Long-Term Care in Japan. Asia Pac. Rev. 2014, 21, 88–119. [Google Scholar] [CrossRef]
- Niikawa, H.; Okamura, T.; Ito, K.; Ura, C.; Miyamae, F.; Sakuma, N.; Ijuin, M.; Inagaki, H.; Sugiyama, M.; Awata, S. Association Between Polypharmacy and Cognitive Impairment in an Elderly Japanese Population Residing in an Urban Community. Geriatr. Gerontol. Int. 2017, 17, 1286–1293. [Google Scholar] [CrossRef]
- Nakaguchi, T.; Ishimoto, T.; Akazawa, N. Minimal Clinically Important Difference for Functional Independence Measure Gain in Post-Acute Rehabilitation Ward Patients with Motor Disorders. Rigakuryoho Kagaku 2018, 33, 235–240. [Google Scholar] [CrossRef][Green Version]
- Hayashi, H.; Iwai, M.; Matsuoka, H.; Nakashima, D.; Nakamura, S.; Kubo, A.; Tomiyama, N. Factors Affecting the Discharge Destination of Hip Fracture Patients Who Live Alone and Have Been Admitted to an Inpatient Rehabilitation Unit. J. Phys. Ther. Sci. 2016, 28, 1228–1232. [Google Scholar] [CrossRef] [PubMed]
- Field, P.E.; Franklin, R.C.; Barker, R.N.; Ring, I.; Leggat, P.A. Cardiac Rehabilitation Services for People in Rural and Remote Areas: An Integrative Literature Review. Rural Remote Health 2018, 18, 4738. [Google Scholar] [CrossRef]
- Kanda, Y. Investigation of the Freely Available Easy-to-Use Software ‘EZR’ for Medical Statistics. Bone Marrow Transplant. 2013, 48, 452–458. [Google Scholar] [CrossRef] [PubMed]
- Ifejika, N.L.; Bhadane, M.; Cai, C.C.; Watkins, J.N.; Grotta, J.C. Characteristics of Acute Stroke Patients Readmitted to Inpatient Rehabilitation Facilities: A Cohort Study. PM R 2020. [Google Scholar] [CrossRef] [PubMed]
- Ogbolu, Y.; Scrandis, D.A.; Fitzpatrick, G. Barriers and Facilitators of Care for Diverse Patients: Nurse Leader Perspectives and Nurse Manager Implications. J. Nurs. Manag. 2018, 26, 3–10. [Google Scholar] [CrossRef]
- Ottenbacher, K.J.; Graham, J.E.; Ottenbacher, A.J.; Lee, J.; Al Snih, S.; Karmarkar, A.; Reistetter, T.; Ostir, G.V. Hospital Readmission in Persons with Stroke Following Postacute Inpatient Rehabilitation. J. Gerontol. A Biol. Sci. Med. Sci. 2012, 67, 875–881. [Google Scholar] [CrossRef]
- Robinson, D.M.; Bazzi, M.S.; Millis, S.R.; Bitar, A.A. Predictors of Readmission to Acute Care during Inpatient Rehabilitation for Non-Traumatic Spinal Cord Injury. J. Spinal Cord Med. 2018, 41, 444–449. [Google Scholar] [CrossRef] [PubMed]
- Campbell, J.C.; Ikegami, N. Long-Term Care Insurance Comes to Japan. Health Aff. 2000, 19, 26–39. [Google Scholar] [CrossRef]
- Daras, L.C.; Ingber, M.J.; Deutsch, A.; Hefele, J.G.; Perloff, J. Geographic Region and Profit Status Drive Variation in Hospital Readmission Outcomes Among Inpatient Rehabilitation Facilities in the United States. Arch. Phys. Med. Rehabil. 2018, 99, 1060–1066. [Google Scholar] [CrossRef]
- Tamakoshi, A.; Tamakoshi, K.; Lin, Y.; Yagyu, K.; Kikuchi, S.; JACC Study Group. Healthy Lifestyle and Preventable Death: Findings from the Japan Collaborative Cohort (JACC) Study. Prev. Med. 2009, 48, 486–492. [Google Scholar] [CrossRef]
- Fujishima, I.; Fujiu-Kurachi, M.; Arai, H.; Hyodo, M.; Kagaya, H.; Maeda, K.; Mori, T.; Nishioka, S.; Oshima, F.; Ogawa, S.; et al. Sarcopenia and Dysphagia: Position Paper by Four Professional Organizations. Geriatr. Gerontol. Int. 2019, 19, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.; Kim, M.; Lee, Y.; Won, C.W. Prevalence of Physical Frailty and Its Multidimensional Risk Factors in Korean Community-Dwelling Older Adults: Findings from Korean Frailty and Aging Cohort Study. Int. J. Environ. Res. Public Health 2020, 17, 7883. [Google Scholar] [CrossRef]
- Yoshimura, Y.; Wakabayashi, H.; Nagano, F.; Bise, T.; Shimazu, S.; Kudo, M.; Shiraishi, A. Sarcopenic Obesity Is Associated with Activities of Daily Living and Home Discharge in Post-Acute Rehabilitation. J. Am. Med. Dir. Assoc. 2020, 21, 1475–1480. [Google Scholar] [CrossRef]
- Ohta, R.; Ryu, Y.; Katsube, T. Care Managers in Rural Japan: Challenges to Interprofessional Collaboration. Home Health Care Serv. Q. 2019, 38, 270–285. [Google Scholar] [CrossRef] [PubMed]
- Ohta, R.; Sakamoto, N.; Maeno, T. Home Care Workers’ Judgment of Acute Conditions in Home Care Patients: A Retrospective Cohort Study. Home Health Care Manag. Pract. 2020, 32, 3–9. [Google Scholar] [CrossRef]
- Ohta, R.; Ryu, Y.; Katsube, T. Challenges for Japanese Rural Home Care Workers in Interprofessional Collaboration: A Qualitative Study. Home Health Care Serv. Q. 2018, 37, 313–324. [Google Scholar] [CrossRef] [PubMed]
- Ohta, R.; Ryu, Y.; Yoshimura, M. Realist Evaluation of Interprofessional Education in Primary Care through Transprofessional Role Play: What Primary Care Professionals Learn together. Educ. Prim. Care 2020, 1–9. [Google Scholar] [CrossRef]
- Ohta, R.; Yoshinori, R.; Sato, M.; Maeno, T. Challenges of Using ICT Regarding Acute Conditions in Rural Home Care: A Thematic Analysis. J. Interprof. Educ. Pract. 2020, 20, 100349. [Google Scholar]
- Enderlin, C.A.; McLeskey, N.; Rooker, J.L.; Steinhauser, C.; D’Avolio, D.; Gusewelle, R.; Ennen, K.A. Review of Current Conceptual Models and Frameworks to Guide Transitions of Care in Older Adults. Geriatr. Nurs. 2013, 34, 47–52. [Google Scholar] [CrossRef]
- Gauer, R.; Meyers, B.K. Heat-Related Illnesses. Am. Fam. Phys. 2019, 99, 482–489. [Google Scholar]
- Guillot, J.; Maumus-Robert, S.; Marceron, A.; Noize, P.; Pariente, A.; Bezin, J. The Burden of Potentially Inappropriate Medications in Chronic Polypharmacy. J. Clin. Med. 2020, 9, 3728. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.; Wong, E.; Ciummo, F. Polypharmacy in Older Adults: Practical Applications alongside a Patient Case. J. Nurse Pract. 2020, 16, 205–209. [Google Scholar] [CrossRef]
- Wouters, H.; Scheper, J.; Koning, H.; Brouwer, C.; Twisk, J.W.; van der Meer, H.; Boersma, F.; Zuidema, S.U.; Taxis, K. Discontinuing Inappropriate Medication Use in Nursing Home Residents: A Cluster Randomized Controlled Trial. Ann. Intern. Med. 2017, 167, 609–617. [Google Scholar] [CrossRef] [PubMed]
- Mannucci, P.M.; Nobili, A. Multimorbidity and Polypharmacy in the Elderly: Lessons from REPOSI. Intern. Emerg. Med. 2014, 9, 723–734. [Google Scholar] [CrossRef] [PubMed]
- Houlind, M.B.; Andersen, A.L.; Treldal, C.; Jørgensen, L.M.; Kannegaard, P.N.; Castillo, L.S.; Christensen, L.D.; Tavenier, J.; Rasmussen, L.J.H.; Ankarfeldt, M.Z.; et al. A Collaborative Medication Review Including Deprescribing for Older Patients in an Emergency Department: A Longitudinal Feasibility Study. J. Clin. Med. 2020, 9, 348. [Google Scholar] [CrossRef] [PubMed]
- Coronado-Vázquez, V.; Gómez-Salgado, J.; Cerezo-Espinosa de Los Monteros, J.; Ayuso-Murillo, D.; Ruiz-Frutos, C. Shared Decision-Making in Chronic Patients with Polypharmacy: An Interventional Study for Assessing Medication Appropriateness. J. Clin. Med. 2019, 8, 904. [Google Scholar] [CrossRef]

| Readmission | ||||
|---|---|---|---|---|
| Factor | Yes | No | p Value | |
| n | 732 | 311 | 421 | |
| Readmission (%) | 311 (42.5) | 311 (100.0) | 0 (0.0) | <0.001 |
| Days from discharge, mean (SD) | 647.52 (438.84) | 368.35 (320.62) | 853.75 (398.71) | <0.001 |
| Age, mean (SD) | 84.00 (8.06) | 85.58 (7.45) | 82.83 (8.30) | <0.001 |
| Male sex (%) | 239 (32.7) | 95 (30.5) | 144 (34.2) | 0.301 |
| Albumin, mean (SD) | 3.74 (0.56) | 3.66 (0.59) | 3.79 (0.53) | 0.003 |
| BMI, mean (SD) | 21.40 (4.96) | 20.65 (3.87) | 21.99 (5.60) | <0.001 |
| CCI ≥ 5 (%) | 447 (61.1) | 209 (67.2) | 238 (6.5) | 0.004 |
| CCI (%) | ||||
| 1 | 5 (0.7) | 3 (0.9) | 2 (0.4) | |
| 2 | 17 (2.3) | 7 (2.3) | 10 (2.4) | |
| 3 | 57 (7.8) | 16 (5.1) | 41 (9.7) | |
| 4 | 206 (28.1) | 76 (24.4) | 130 (30.9) | |
| 5 | 154 (21.0) | 63 (20.3) | 91 (21.6) | |
| 6 | 148 (20.2) | 69 (22.2) | 79 (18.8) | |
| 7 | 78 (10.7) | 41 (13.2) | 37 (8.8) | |
| 8 | 37 (5.1) | 21 (6.8) | 16 (3.8) | |
| 9 | 20 (2.7) | 12 (3.9) | 8 (1.9) | |
| 10 | 9 (1.2) | 3 (1.0) | 6 (1.4) | |
| 12 | 1 (0.1) | 0 (0.0) | 1 (0.2) | |
| Heart failure (%) | 97 (13.3) | 46 (14.8) | 51 (12.1) | 0.321 |
| Asthma (%) | 34 (4.6) | 16 (5.1) | 18 (4.3) | 0.598 |
| Kidney diseases (%) | 143 (19.5) | 62 (19.9) | 81 (19.2) | 0.851 |
| Liver diseases (%) | 24 (3.2) | 13 (4.2) | 11 (2.6) | 0.282 |
| COPD (%) | 24 (3.3) | 9 (2.9) | 15 (3.6) | 0.679 |
| DM (%) | 133 (18.2) | 54 (17.4) | 79 (18.8) | 0.698 |
| Brain hemorrhage (%) | 84 (11.5) | 34 (10.9) | 50 (11.9) | 0.726 |
| Brain infarction (%) | 163 (22.3) | 72 (23.2) | 91 (21.6) | 0.654 |
| Hemiplegia (%) | 26 (3.6) | 10 (3.2) | 16 (3.8) | 0.84 |
| Dementia (%) | 65 (8.9) | 29 (9.3) | 36 (8.6) | 0.793 |
| Connective diseases (%) | 35 (4.8) | 16 (5.1) | 19 (4.5) | 0.728 |
| Cancer (%) | 124 (16.9) | 55 (17.7) | 69 (16.4) | 0.797 |
| Dependent condition (%) | 210 (28.7) | 121 (38.9) | 89 (21.1) | <0.001 |
| Care level (%) | ||||
| 0 | 522 (71.3) | 190 (61.1) | 332 (78.9) | |
| 1 | 39 (5.3) | 17 (5.5) | 22 (5.2) | |
| 2 | 71 (9.7) | 43 (13.8) | 28 (6.7) | |
| 3 | 47 (6.4) | 25 (8.0) | 22 (5.2) | |
| 4 | 28 (3.8) | 17 (5.5) | 11 (2.6) | |
| 5 | 25 (3.4) | 19 (6.1) | 6 (1.4) | |
| Reason for admission | ||||
| Medicine-related | 393 (53.7) | 163 (52.4) | 230 (54.6) | 0.600 |
| Orthopedic | 339 (46.3) | 148 (47.6) | 191 (45.4) | |
| Locations of discharge (%) | ||||
| Nursing facility | 129 (17.6) | 57 (18.3) | 72 (17.1) | 0.695 |
| Home | 603 (82.4) | 254 (81.7) | 349 (82.9) | |
| Number of medicines taken, mean (SD) | 5.89 (2.36) | 6.14 (2.47) | 5.70 (2.26) | 0.014 |
| Number of patients with polypharmacy, n (%) | 538 (73.5) | 240 (77.2) | 298 (70.8) | 0.062 |
| FIM score at discharge | ||||
| Total FIM score (median) | 109 (18, 126) | 104(18, 126) | 111 (18, 126) | 0.005 |
| Motor domain score (median) | 31.00 (13, 35) | 30.00 (13, 35) | 32.00 (13, 35) | 0.014 |
| Cognitive domain score (median) | 78 (5, 91) | 74 (5, 91) | 79 (13, 91) | 0.005 |
| Duration of rehabilitation (median) | 52 (3, 228) | 49 (5, 228) | 57(3, 189) | 0.015 |
| Factor | n = 732 | Percentage | Cumulated Percentage |
|---|---|---|---|
| Interval | 311 | 42.49% | |
| <30 days | 23 | 3.14% | 3.14% |
| 30 to 90 days | 46 | 6.28% | 9.42% |
| 91 to 180 days | 39 | 5.33% | 14.75% |
| 181 to 365 days (1 year) | 79 | 10.79% | 25.54% |
| 366 to 730 days (2 years) | 80 | 10.93% | 36.47% |
| 731 to 1095 days (3 years) | 28 | 3.83% | 40.30% |
| >1096 days | 16 | 2.19% | 42.49% |
| Factor | Hazard Ratio | 95% CI | p Value |
|---|---|---|---|
| Age | 1.01 | 0.99–1.02 | 0.49 |
| Male sex | 0.84 | 0.65–1.08 | 0.16 |
| Albumin | 0.89 | 0.72–1.10 | 0.28 |
| BMI | 0.95 | 0.92–0.98 | <0.001 |
| CCI ≥ 5 | 1.21 | 0.94–1.57 | 0.14 |
| Dependent condition | 2.01 | 1.56–2.59 | <0.001 |
| Discharge to home | 1.08 | 0.78–1.49 | 0.64 |
| FIM score | |||
| Higher cognitive domain score | 0.71 | 0.53–0.94 | 0.019 |
| Higher motor domain score | 0.93 | 0.68–1.27 | 0.66 |
| Polypharmacy | 1.36 | 1.04–1.79 | 0.026 |
| Length of rehabilitation | 1 | 0.99–1.00 | 0.077 |
| Diagnosis | Number | Percentage | Diagnosis | Number | Percentage |
|---|---|---|---|---|---|
| Pyelonephritis | 37 | 11.9% | Pseudogout | 6 | 1.9% |
| Pneumonia * | 34 | 10.9% | Ileus | 6 | 1.9% |
| Compression fracture | 33 | 10.6% | Epilepsy | 5 | 1.6% |
| Heat stroke | 26 | 8.4% | Liver failure | 4 | 1.3% |
| Cerebral stroke * | 25 | 8.0% | Renal failure | 3 | 1.0% |
| Other infections * | 24 | 7.7% | LSS | 3 | 1.0% |
| Femoral fracture | 22 | 7.1% | Peripheral vertigo | 2 | 0.6% |
| Other fractures * | 19 | 6.1% | Osteoarthritis | 2 | 0.6% |
| Trauma | 17 | 5.5% | Asthma | 2 | 0.6% |
| Dehydration | 16 | 5.1% | Peptic ulcer* | 2 | 0.6% |
| Cancer * | 11 | 3.5% | Ischemic colitis | 1 | 0.3% |
| Autoimmune diseases * | 10 | 3.2% | Angina | 1 | 0.3% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ohta, R.; Sano, C. Risk of Hospital Readmission among Older Patients Discharged from the Rehabilitation Unit in a Rural Community Hospital: A Retrospective Cohort Study. J. Clin. Med. 2021, 10, 659. https://doi.org/10.3390/jcm10040659
Ohta R, Sano C. Risk of Hospital Readmission among Older Patients Discharged from the Rehabilitation Unit in a Rural Community Hospital: A Retrospective Cohort Study. Journal of Clinical Medicine. 2021; 10(4):659. https://doi.org/10.3390/jcm10040659
Chicago/Turabian StyleOhta, Ryuichi, and Chiaki Sano. 2021. "Risk of Hospital Readmission among Older Patients Discharged from the Rehabilitation Unit in a Rural Community Hospital: A Retrospective Cohort Study" Journal of Clinical Medicine 10, no. 4: 659. https://doi.org/10.3390/jcm10040659
APA StyleOhta, R., & Sano, C. (2021). Risk of Hospital Readmission among Older Patients Discharged from the Rehabilitation Unit in a Rural Community Hospital: A Retrospective Cohort Study. Journal of Clinical Medicine, 10(4), 659. https://doi.org/10.3390/jcm10040659






