A Diagnostic Algorithm Based on a Simple Clinical Prediction Rule for the Diagnosis of Cranial Giant Cell Arteritis
Abstract
1. Introduction
2. Materials and Methods
2.1. Cohort Characteristics
2.2. Derivation of the Clinical Model
2.3. Validation of the Clinical Model in an Independent Cohort
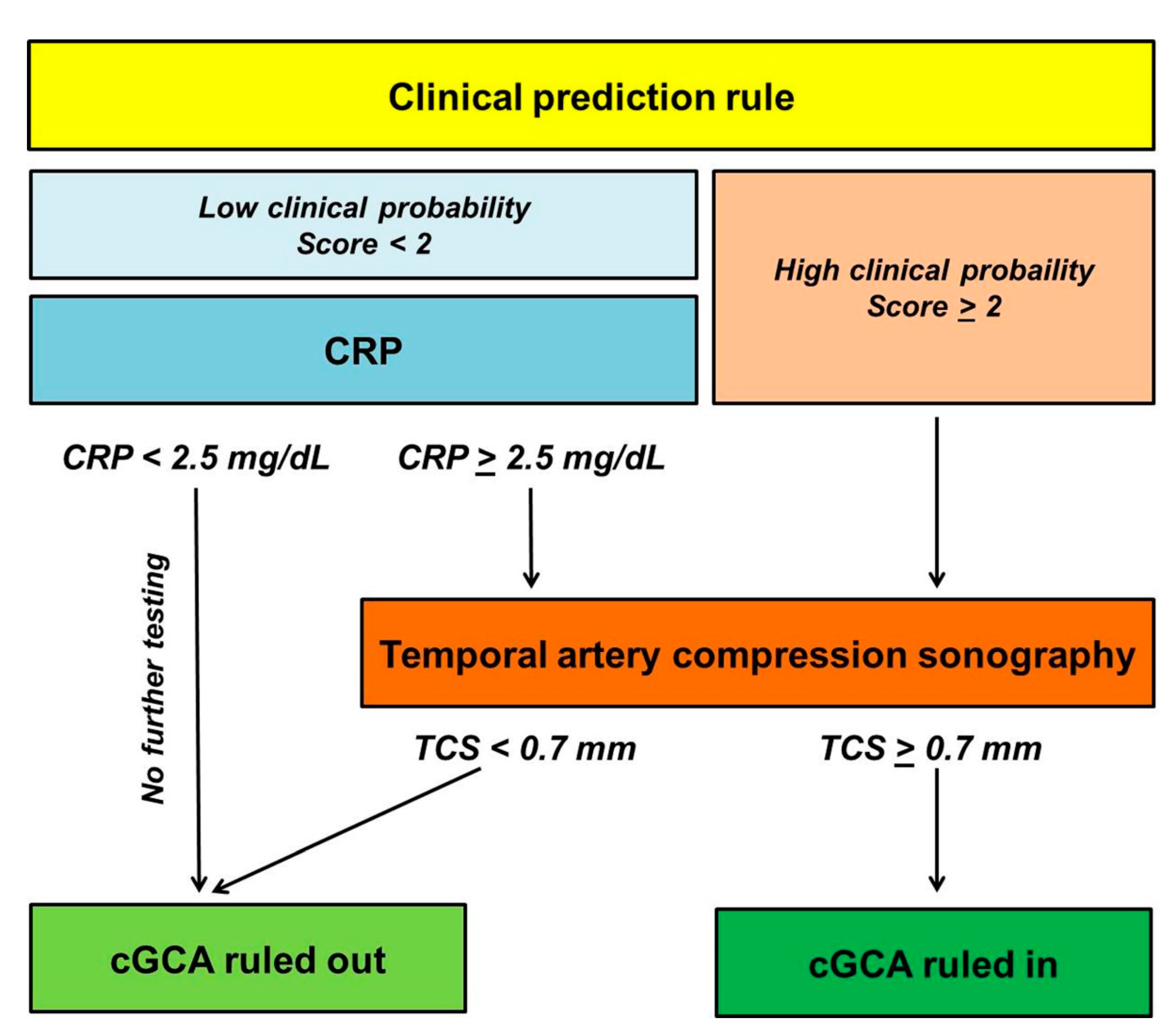
2.4. Stepwise Diagnostic Algorithm Integrating the Clinical Model, C-Reactive Protein and hrTCS
2.5. Statistical Analysis
3. Results
3.1. Derivation of the Clinical Model
3.2. Validation of the Logistic Model in an Independent Cohort
3.3. Stepwise Diagnostic Algorithm Integrating the Clinical Model, C-Reactive Protein, and hrTCS
3.4. Performance of the Diagnostic Algorithm in the Derivation Cohort
3.5. Performance of the Diagnostic Algorithm in the Validation Cohort
3.6. Test Performance of hrTCS Dependent on Pre-Test Probability
3.7. Extracranial GCA
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Crowson, C.S.; Matteson, E.L.; Myasoedova, E.; Michet, C.J.; Ernste, F.C.; Warrington, K.J.; Davis, J.M., 3rd; Hunder, G.G.; Therneau, T.M.; Gabriel, S.E. The lifetime risk of adult-onset rheumatoid arthritis and other inflammatory autoimmune rheumatic diseases. Arthritis Rheum. 2011, 63, 633–639. [Google Scholar] [CrossRef] [PubMed]
- Dejaco, C.; Ramiro, S.; Duftner, C.; Besson, F.L.; Bley, T.A.; Blockmans, D.; Brouwer, E.; Cimmino, M.A.; Clark, E.; Dasgupta, B.; et al. EULAR recommendations for the use of imaging in large vessel vasculitis in clinical practice. Ann. Rheum. Dis. 2018, 77, 636–643. [Google Scholar] [CrossRef]
- Hellmich, B.; Agueda, A.; Monti, S.; Buttgereit, F.; De Boysson, H.; Brouwer, E.; Cassie, R.; Cid, M.C.; Dasgupta, B.; Dejaco, C.; et al. 2018 Update of the EULAR recommendations for the management of large vessel vasculitis. Ann. Rheum. Dis. 2020, 79, 19–30. [Google Scholar] [CrossRef]
- Mackie, S.L.; Dejaco, C.; Appenzeller, S.; Camellino, D.; Duftner, C.; Gonzalez-Chiappe, S.; Mahr, A.; Mukhtyar, C.; Reynolds, G.; de Souza, A.W.S.; et al. British Society for Rheumatology guideline on diagnosis and treatment of giant cell arteritis. Rheumatology 2020, 59, e1–e23. [Google Scholar] [CrossRef]
- Mollan, S.P.; Paemeleire, K.; Versijpt, J.; Luqmani, R.; Sinclair, A.J. European Headache Federation recommendations for neurologists managing giant cell arteritis. J. Headache Pain 2020, 21, 28. [Google Scholar] [CrossRef]
- Schäfer, V.S.; Juche, A.; Ramiro, S.; Krause, A.; Schmidt, W.A. Ultrasound cut-off values for intima-media thickness of temporal, facial and axillary arteries in giant cell arteritis. Rheumatology 2017, 56, 1479–1483. [Google Scholar] [CrossRef]
- Ješe, R.; Rotar, Ž.; Tomšič, M.; Hočevar, A. The cut-off values for the intima-media complex thickness assessed by colour Doppler sonography in seven cranial and aortic arch arteries. Rheumatology 2020. [Google Scholar] [CrossRef]
- Czihal, M.; Schröttle, A.; Baustel, K.; Lottspeich, C.; Dechant, C.; Treitl, K.-M.; Treitl, M.; Schulze-Koops, H.; Hoffmann, U. B-mode sonography wall thickness assessment of the temporal and axillary arteries for the diagnosis of giant cell arteritis: A cohort study. Clin. Exp. Rheumatol. 2017, 103, 128–133. [Google Scholar]
- De Miguel, E.; Beltran, L.M.; Monjo, I.; Deodati, F.; Schmidt, W.A.; Garcia-Puig, J. Atherosclerosis as a potential pitfall in the diagnosis of giant cell arteritis. Rheumatology 2018, 57, 318–321. [Google Scholar] [CrossRef]
- Czihal, M.; Köhler, A.; Lottspeich, C.; Prearo, I.; Hoffmann, U.; Schulze-Koops, H.; Priglinger, S.G.; Mackert, M.J.; Dechant, C. Temporal artery compression sonography for the diagnosis of giant cell arteritis in elderly patients with acute ocular arterial occlusions. Rheumatology 2020. [Google Scholar] [CrossRef] [PubMed]
- Griner, P.F.; Mayewski, R.J.; Mushlin, A.I.; Greenland, P. Selection and interpretation of diagnostic tests and procedures. Principles and applications. Ann. Intern. Med. 1981, 94, 557–592. [Google Scholar]
- Hayreh, S.S.; Podhajsky, P.A.; Raman, R.; Zimmerman, B. Giant Cell Arteritis: Validity and Reliability of Various Diagnostic Criteria. Am. J. Ophthalmol. 1997, 123, 285–296. [Google Scholar] [CrossRef]
- Smetana, G.W.; Shmerling, R.H. Does this patient have temporal arteritis? JAMA 2002, 287, 92–101. [Google Scholar] [CrossRef]
- Moutray, T.N.; Williams, M.A.; Best, J.L. Suspected giant cell arteritis: A study of referrals for temporal artery biopsy. Can. J. Ophthalmol. 2008, 43, 445–448. [Google Scholar] [CrossRef] [PubMed]
- González-López, J.J.; González-Moraleja, J.; Burdaspal-Moratilla, A.; Rebolleda, G.; Núñez-Gómez-Álvarez, M.T.; Muñoz-Negrete, F.J. Factors associated to temporal artery biopsy result in suspects of giant cell arteritis: A retrospective, multicenter, case-control study. Acta Ophthalmol. 2013, 91, 763–768. [Google Scholar] [CrossRef]
- Grossman, C.; Barshack, I.; Koren-Morag, N.; Ben-Zvi, I.; Bornstein, G. Baseline clinical predictors of an ultimate giant cell arteritis diagnosis in patients referred to temporal artery biopsy. Clin. Rheumatol. 2016, 35, 1817–1822. [Google Scholar] [CrossRef]
- Ing, E.B.; Luna, G.L.; Toren, A.; Ing, R.; Chen, J.J.; Arora, N.; Torun, N.; Jakpor, O.A.; Fraser, J.A.; Tyndel, F.J.; et al. Multivariable prediction model for suspected giant cell arteritis: Development and validation. Clin. Ophthalmol. 2017, 11, 2031–2042. [Google Scholar] [CrossRef]
- Weis, E.; Toren, A.; Jordan, D.; Patel, V.; Gilberg, S. Development of a predictive model for temporal artery biopsies. Can. J. Ophthalmol. 2017, 52, 599–605. [Google Scholar] [CrossRef] [PubMed]
- Hunder, G.G.; Bloch, D.A.; Michel, B.A.; Stevens, M.B.; Arend, W.P.; Calabrese, L.H.; Edworthy, S.M.; Fauci, A.S.; Leavitt, R.Y.; Lie, J.T.; et al. The American College of Rheumatology 1990 criteria for the classification of giant cell arteritis. Arthritis Rheum. 1990, 33, 1122–1128. [Google Scholar] [CrossRef] [PubMed]
- Gabriel, S.E.; O’Fallon, W.M.; Achkar, A.A.; Lie, J.T.; Hunder, G.G. The use of clinical characteristics to predict the results of temporal artery biopsy among patients with suspected giant cell arteritis. J. Rheumatol. 1995, 22, 93–96. [Google Scholar] [PubMed]
- Rodriguez-Valverde, V.; Sarabia, J.M.; González-Gay, M.A.; Figueroa, M.; Armona, J.; Blanco, R.; Fernández-Sueiro, J.L.; Martínez-Taboada, V.M. Risk Factors and Predictive Models of Giant Cell Arteritis in Polymyalgia Rheumatica. Am. J. Med. 1997, 102, 331–336. [Google Scholar] [CrossRef]
- Niederkohr, R.D.; Levin, L.A. Management of the Patient with Suspected Temporal Arteritis. A Decision-Analytic Approach. Ophthalmology 2005, 112, 744–756. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Pla, A.; Rosselló-Urgell, J.; Bosch-Gil, J.A.; Huguet-Redecilla, P.; Vilardell-Tarres, M. Proposal to decrease the number of negative temporal artery biopsies. Scand. J. Rheumatol 2007, 36, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Rieck, K.L.; Kermani, T.A.; Thomsen, K.M.; Harmsen, W.S.; Karban, M.J.; Warrington, K.J. Evaluation for Clinical Predictors of Positive Temporal Artery Biopsy in Giant Cell Arteritis. J. Oral Maxillofac. Surg. 2011, 69, 36–40. [Google Scholar] [CrossRef] [PubMed]
- El-Dairi, M.A.; Chang, L.; Proia, A.D.; Cummings, T.J.; Stinnett, S.S.; Bhatti, M.T. Diagnostic Algorithm for Patients With Suspected Giant Cell Arteritis. J. Neuro-Ophthalmol. 2015, 35, 246–253. [Google Scholar] [CrossRef]
- Toren, A.; Weis, E.; Patel, V.; Monteith, B.; Gilberg, S.; Jordan, D. Clinical predictors of positive temporal artery biopsy. Can. J. Ophthalmol. 2016, 51, 476–481. [Google Scholar] [CrossRef]
- Ing, E.B.; Miller, N.R.; Nguyen, A.; Su, W.; Bursztyn, L.L.C.D.; Poole, M.; Kansal, V.; Toren, A.; Albreiki, D.; Mouhanna, J.G.; et al. Neural network and logistic regression diagnostic prediction models for giant cell arteritis: Development and validation. Clin. Ophthalmol. 2019, 13, 421–430. [Google Scholar] [CrossRef] [PubMed]
- Laskou, F.; Coath, F.; Mackie, S.L.; Banerjee, S.; Aung, T.; Dasgupta, B. A probability score to aid the diagnosis of suspected giant cell arteritis. Clin. Exp. Rheumatol. 2019, 117, 104–108. [Google Scholar]
- Sebastian, A.; Tomelleri, A.; Kayani, A.; Prieto-Pena, D.; Ranasinghe, C.; Dasgupta, B. Probability-based algorithm using ultrasound and additional tests for suspected GCA in a fast-track clinic. RMD Open 2020, 6, e001297. [Google Scholar] [CrossRef]
- Monti, S.; Ponte, C.; Pereira, C.; Manzoni, F.; Klersy, C.; Rumi, F.; Carrara, G.; Hutchings, A.; A Schmidt, W.; Dasgupta, B.; et al. The impact of disease extent and severity detected by quantitative ultrasound analysis in the diagnosis and outcome of giant cell arteritis. Rheumatology 2020, 59, 2299–2307. [Google Scholar] [CrossRef]
- Walvick, M.D.; Walvick, M.P. Giant cell arteritis: Laboratory predictors of a positive temporal artery biopsy. Ophthalmology 2011, 118, 1201–1204. [Google Scholar] [CrossRef] [PubMed]
- Kermani, T.A.; Schmidt, J.; Crowson, C.S.; Ytterberg, S.R.; Hunder, G.G.; Matteson, E.L.; Warrington, K.J. Utility of erythrocyte sedimentation rate and C-reactive protein for the diagnosis of giant cell arteritis. Semin. Arthritis Rheum. 2012, 41, 866–871. [Google Scholar] [CrossRef] [PubMed]
- Manzo, C. Widespread headache as the first clinical manifestation of giant cell arteritis in patients affected by polymyalgia rheumatica. Reumatologia 2016, 54, 236–238. [Google Scholar] [CrossRef]
- Hočevar, A.; Ješe, R.; Tomšič, M.; Rotar, Ž. Risk factors for severe cranial ischaemic complications in giant cell arteritis. Rheumatology 2020, 59, 2953–2959. [Google Scholar] [CrossRef] [PubMed]
- Soriano, A.; Muratore, F.; Pipitone, N.; Boiardi, L.; Cimino, L.; Salvarani, C. Visual loss and other cranial ischaemic complications in giant cell arteritis. Nat. Rev. Rheumatol. 2017, 13, 476–484. [Google Scholar] [CrossRef]
- De Boysson, H.; Lambert, M.; Liozon, E.; Boutemy, J.; Maigné, G.; Ollivier, Y.; Ly, K.; Manrique, A.; Bienvenu, B.; Aouba, A. Giant-cell arteritis without cranial manifestations: Working diagnosis of a distinct disease pattern. Medicine 2016, 95, e3818. [Google Scholar] [CrossRef]
- van der Geest, K.S.M.; Borg, F.; Kayani, A.; Paap, D.; Gondo, P.; Schmidt, W.; Luqmani, R.A.; Dasgupta, B. Novel ultrasonographic Halo Score for giant cell arteritis: Assessment of diagnostic accuracy and association with ocular ischaemia. Ann. Rheum. Dis. 2020, 79, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Junek, M.; Hu, A.; Garner, S.; Rebello, R.; Legault, K.; Beattie, K.; Khalidi, N. Contextualizing temporal arterial magnetic resonance angiography in the diagnosis of giant cell arteritis: A retrospective cohort study. Rheumatology 2021. [Google Scholar] [CrossRef]
- Sanders, S.L.; Rathbone, J.; Bell, K.J.L.; Glasziou, P.P.; Doust, J.A. Systematic review of the effects of care provided with and without diagnostic clinical prediction rules. Diagn. Progn. Res. 2017, 1, 13. [Google Scholar] [CrossRef] [PubMed]


| Cohort 1, Final Diagnosis of cGCA n = 26 | Cohort 1, Final Diagnosis Not cGCA n = 61 | Cohort 2, Final Diagnosis of cGCA n = 30 | Cohort 2, Final Diagnosis Not cGCA n = 84 | |
|---|---|---|---|---|
| Age, years (mean ± SD) | 73.2 (9.2) | 66.1 (11.2) | 77.5 (6.7) | 73.6 (10.2) |
| Female sex (n, %) | 15 (57.7) | 33 (54.1) | 19 (63.3) | 40 (47.6) |
| New onset headache (n, %) | 21 (80.8) | 11 (18) | 19 (63.3) | 13 (15.5) |
| Jaw claudication (n, %) | 16 (61.5) | 2 (3.3) | 18 (60) | 0 |
| Amaurosis fugax (n, %) | 4 (15.4) | 7 (11.5) | 2 (6.7) | 4 (4.8) |
| Permanent sight loss (n, %) | 19 (73.1) | 18 (29.5) | 30 (100) | 84 (100) |
| AION (n, %) | 16 (61.5) | 7 (11.4) | 28 (93.3) | 26 (31) |
| Bilateral AION (n, %) | 3 (11.5) | 1 (1.6) | 6 (20) | 3 (3.6) |
| PMR (n, %) | 10 (38.5) | 21 (34.4) | 6 (20) | 1 (1.2) |
| Constitutional symptoms (n, %) | 12 (46.2) | 19 (31.1) | 13 (43.3) | 4 (4.8) |
| CRP (mg/dL, mean ± SD) | 5.2 (5.3) | 4.2 (5.6) | 5.1 (5.7) | 0.8 (0.9) |
| TAB performed (n, %) | 13 (50) | 6 (9.8) | 8 (26.7) | 9 (10.7) |
| TAB positive (n, %) | 10 (38.5) | 0 | 5 (16.7) | 0 |
| Variable | Description | Score |
|---|---|---|
| Age (years) | <70 years | 0 |
| >70 years | 1 | |
| New onset persistent headache | No | 0 |
| Yes | 1 | |
| Jaw claudication | No | 0 |
| Yes | 1 | |
| Permanent vision impairment due to AION | No | 0 |
| Unilateral | 1 | |
| Bilateral | 2 | |
| Score (range 0–6) | Low clinical probability | ≤1 point |
| High clinical probability | ≥2 points |
| Score | Proportion of Patients (n, %) | Prevalence of cGCA (n, %) | PPV | NPV |
|---|---|---|---|---|
| 0 | 39 (18.8) | 1 (2.6) | 50 | 100 |
| 1 | 74 (35.7) | 2 (2.7) | 11.1 | 98.4 |
| 2 | 39 (18.8) | 11 (28.2) | 69.2 | 92.3 |
| 3 | 17 (8.2) | 10 (58.8) | 75 | 80 |
| 4 | 14 (6.8) | 14 (100) | 100 | / * |
| 5 | 13 (6.3) | 13 (100) | 100 | / * |
| 6 | 5 (2.4) | 5 (100) | 100 | / * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Czihal, M.; Lottspeich, C.; Bernau, C.; Henke, T.; Prearo, I.; Mackert, M.; Priglinger, S.; Dechant, C.; Schulze-Koops, H.; Hoffmann, U. A Diagnostic Algorithm Based on a Simple Clinical Prediction Rule for the Diagnosis of Cranial Giant Cell Arteritis. J. Clin. Med. 2021, 10, 1163. https://doi.org/10.3390/jcm10061163
Czihal M, Lottspeich C, Bernau C, Henke T, Prearo I, Mackert M, Priglinger S, Dechant C, Schulze-Koops H, Hoffmann U. A Diagnostic Algorithm Based on a Simple Clinical Prediction Rule for the Diagnosis of Cranial Giant Cell Arteritis. Journal of Clinical Medicine. 2021; 10(6):1163. https://doi.org/10.3390/jcm10061163
Chicago/Turabian StyleCzihal, Michael, Christian Lottspeich, Christoph Bernau, Teresa Henke, Ilaria Prearo, Marc Mackert, Siegfried Priglinger, Claudia Dechant, Hendrik Schulze-Koops, and Ulrich Hoffmann. 2021. "A Diagnostic Algorithm Based on a Simple Clinical Prediction Rule for the Diagnosis of Cranial Giant Cell Arteritis" Journal of Clinical Medicine 10, no. 6: 1163. https://doi.org/10.3390/jcm10061163
APA StyleCzihal, M., Lottspeich, C., Bernau, C., Henke, T., Prearo, I., Mackert, M., Priglinger, S., Dechant, C., Schulze-Koops, H., & Hoffmann, U. (2021). A Diagnostic Algorithm Based on a Simple Clinical Prediction Rule for the Diagnosis of Cranial Giant Cell Arteritis. Journal of Clinical Medicine, 10(6), 1163. https://doi.org/10.3390/jcm10061163






