The Effect of Tranexamic Acid Administration on Early Endothelial Damage Following Posterior Lumbar Fusion Surgery
Abstract
1. Introduction
2. Materials and Methods
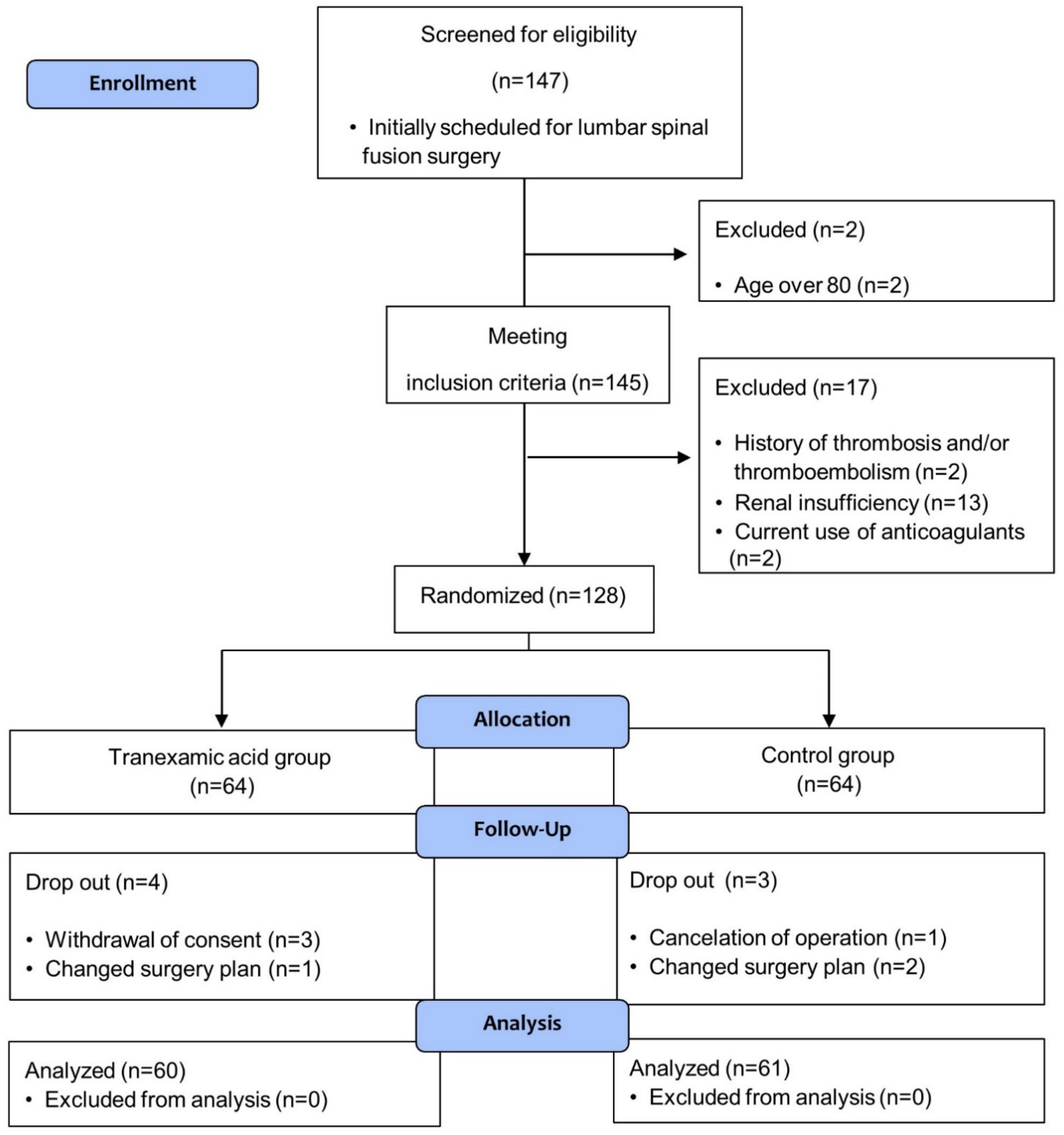
2.1. Patient Selection and Study Design
2.2. Study Endpoints
2.3. Sample Size Calculation
2.4. Statistical Analysis
3. Results
3.1. Participants and Descriptive Data
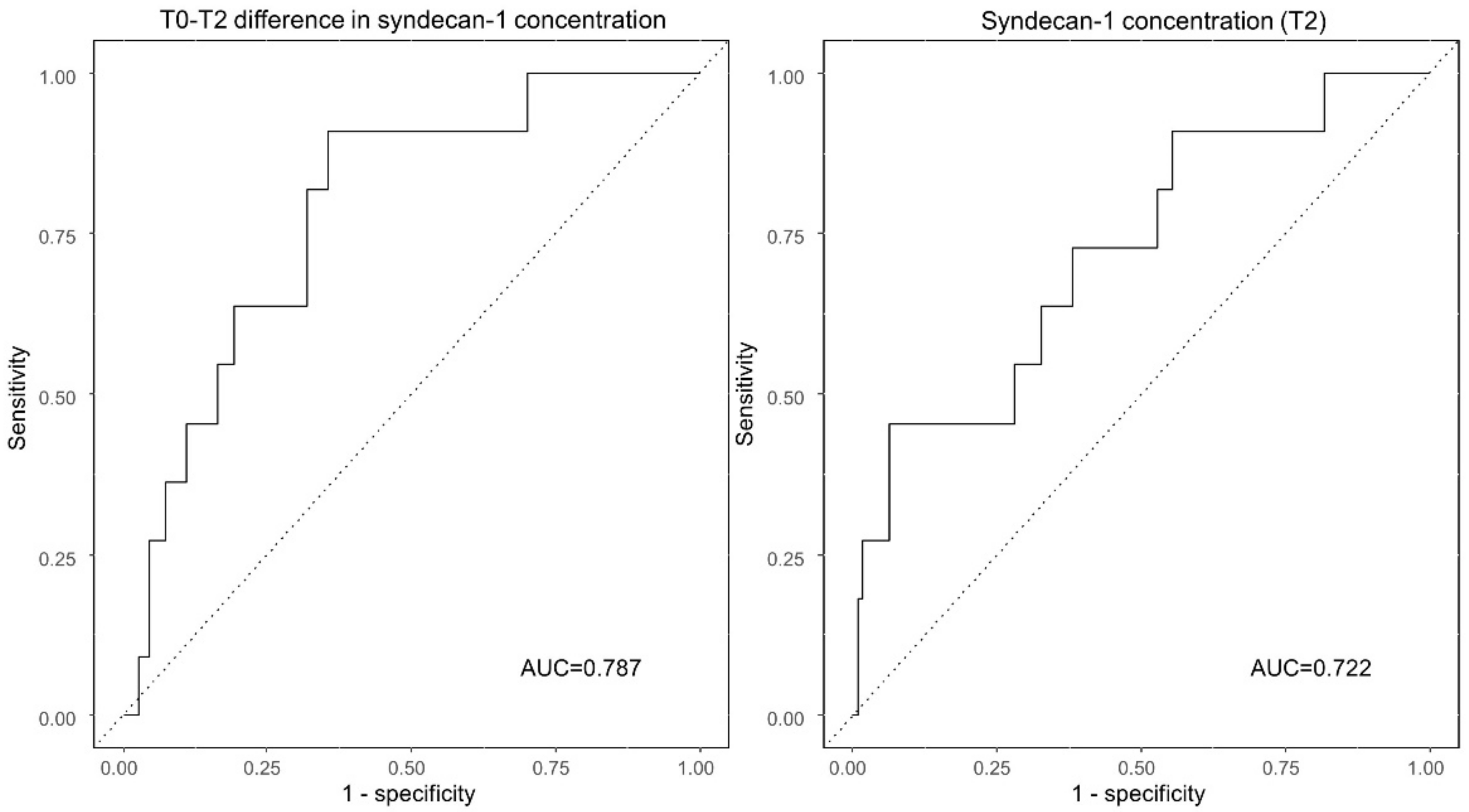
3.2. Changes in Plasma Concentrations of Endothelial Glycocalyx Markers
3.3. Early Postoperative Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bai, J.; Zhang, P.; Liang, Y.; Wang, J.; Wang, Y. Efficacy and safety of tranexamic acid usage in patients undergoing posterior lumbar fusion: A meta-analysis. BMC Musculoskelet. Disord. 2019, 20, 390. [Google Scholar] [CrossRef]
- Reikeras, O.; Borgen, P. Activation of Markers of Inflammation, Coagulation and Fibrinolysis in Musculoskeletal Trauma. PLoS ONE 2014, 9, e107881. [Google Scholar] [CrossRef]
- Lindberg-Larsen, V.; Ostrowski, S.R.; Rovsing, M.L.; Johansson, P.I.; Kehlet, H. The effect of pre-operative methylprednisolone on early endothelial damage after total knee arthroplasty: A randomised, double-blind, placebo-controlled trial. Anaesthesia 2017, 72, 1217–1224. [Google Scholar] [CrossRef] [PubMed]
- Cerny, V.; Astapenko, D.; Brettner, F.; Benes, J.; Hyspler, R.; Lehmann, C.; Zadak, Z. Targeting the endothelial glycocalyx in acute critical illness as a challenge for clinical and laboratory medicine. Crit. Rev. Clin. Lab. Sci. 2017, 54, 343–357. [Google Scholar] [CrossRef] [PubMed]
- Martin, L.; Koczera, P.; Zechendorf, E.; Schuerholz, T. The Endothelial Glycocalyx: New Diagnostic and Therapeutic Approaches in Sepsis. BioMed Res. Int. 2016, 2016, 1–8. [Google Scholar] [CrossRef]
- Yilmaz, O.; Afsar, B.; Ortiz, A.; Kanbay, M. The role of endothelial glycocalyx in health and disease. Clin. Kidney J. 2019, 12, 611–619. [Google Scholar] [CrossRef] [PubMed]
- Becker, B.F.; Chappell, D.; Bruegger, D.; Annecke, T.; Jacob, M. Therapeutic strategies targeting the endothelial glycocalyx: Acute deficits, but great potential. Cardiovasc. Res. 2010, 87, 300–310. [Google Scholar] [CrossRef]
- Chappell, D.; Dörfler, N.; Jacob, M.; Rehm, M.; Welsch, U.; Conzen, P.; Becker, B.F. Glycocalyx Protection Reduces Leukocyte Adhesion after Ischemia/Reperfusion. Shock 2010, 34, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Murphy, L.S.; Wickersham, N.; McNeil, J.B.; Shaver, C.M.; May, A.K.; Bastarache, J.A.; Ware, L.B. Endothelial glycocalyx degradation is more severe in patients with non-pulmonary sepsis compared to pulmonary sepsis and associates with risk of ARDS and other organ dysfunction. Ann. Intensive Care 2017, 7, 1–9. [Google Scholar] [CrossRef]
- De Oliveira Neves, F.M.; Meneses, G.C.; Araujo Sousa, N.E.; De Menezes, R.R.P.P.B.; Parahyba, M.C.; Martins, A.M.C.; Libório, A.B. Syndecan-1 in Acute Decompensated Heart Failure—Association with Renal Function and Mortality. Circ. J. 2015, 79, 1511–1519. [Google Scholar] [CrossRef]
- Puskarich, M.A.; Cornelius, D.C.; Tharp, J.; Nandi, U.; Jones, A.E. Plasma syndecan-1 levels identify a cohort of patients with severe sepsis at high risk for intubation after large-volume intravenous fluid resuscitation. J. Crit. Care 2016, 36, 125–129. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.-B.; Soh, S.; Kwak, Y.-L.; Bae, J.C.; Kang, S.H.; Song, J.W. High Preoperative Serum Syndecan-1, a Marker of Endothelial Glycocalyx Degradation, and Severe Acute Kidney Injury after Valvular Heart Surgery. J. Clin. Med. 2020, 9, 1803. [Google Scholar] [CrossRef]
- Lord, J.M.; Midwinter, M.J.; Chen, Y.-F.; Belli, A.; Brohi, K.; Kovacs, E.J.; Koenderman, L.; Kubes, P.; Lilford, R.J. The systemic immune response to trauma: An overview of pathophysiology and treatment. Lancet 2014, 384, 1455–1465. [Google Scholar] [CrossRef]
- Simmons, J.; Sikorski, R.A.; Pittet, J.-F. Tranexamic acid. Curr. Opin. Anaesthesiol. 2015, 28, 191–200. [Google Scholar] [CrossRef] [PubMed]
- Diebel, L.N.; Martin, J.V.; Liberati, D.M. Early tranexamic acid administration ameliorates the endotheliopathy of trauma and shock in an in vitro model. J. Trauma Acute Care Surg. 2017, 82, 1080–1086. [Google Scholar] [CrossRef]
- Diebel, M.E.; Martin, J.V.; Liberati, D.M.; Diebel, L.N. The temporal response and mechanism of action of tranexamic acid in endothelial glycocalyx degradation. J. Trauma Acute Care Surg. 2018, 84, 75–80. [Google Scholar] [CrossRef]
- Kellum, J.A.; Lameire, N.; Aspelin, P.; Barsoum, R.S.; Burdmann, E.A.; Goldstein, S.L.; Herzog, C.A.; Joannidis, M.; Kribben, A.; Levey, A.S.; et al. Kidney disease: Improving global outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int. Suppl. 2012, 2, 1–138. [Google Scholar] [CrossRef]
- Kim, H.-J.; Kim, E.; Baek, S.-H.; Kim, H.Y.; Kim, J.-Y.; Park, J.; Choi, E.-J. Sevoflurane did not show better protective effect on endothelial glycocalyx layer compared to propofol during lung resection surgery with one lung ventilation. J. Thorac. Dis. 2018, 10, 1468–1475. [Google Scholar] [CrossRef]
- Chelazzi, C.; Villa, G.; Mancinelli, P.; De Gaudio, A.R.; Adembri, C. Glycocalyx and sepsis-induced alterations in vascular permeability. Crit. Care 2015, 19, 26. [Google Scholar] [CrossRef]
- Burke-Gaffney, A.; Evans, T.W. Lest we forget the endothelial glycocalyx in sepsis. Crit. Care 2012, 16, 121. [Google Scholar] [CrossRef] [PubMed]
- Astapenko, D.; Benes, J.; Pouska, J.; Lehmann, C.; Islam, S.; Cerny, V. Endothelial glycocalyx in acute care surgery—What anaesthesiologists need to know for clinical practice. BMC Anesthesiol. 2019, 19, 238. [Google Scholar] [CrossRef]
- Martin, J.V.; Liberati, D.M.; Diebel, L.N. Disparate effects of catecholamines under stress conditions on endothelial glycocalyx injury: An in vitro model. Am. J. Surg. 2017, 214, 1166–1172. [Google Scholar] [CrossRef]
- Li, Z.-J.; Fu, X.; Xing, D.; Zhang, H.-F.; Zang, J.-C.; Ma, X.-L. Is tranexamic acid effective and safe in spinal surgery? A meta-analysis of randomized controlled trials. Eur. Spine J. 2013, 22, 1950–1957. [Google Scholar] [CrossRef]
- Chappell, D.; Bruegger, D.; Potzel, J.; Jacob, M.; Brettner, F.; Vogeser, M.; Conzen, P.; Becker, B.F.; Rehm, M. Hypervolemia increases release of atrial natriuretic peptide and shedding of the endothelial glycocalyx. Crit. Care 2014, 18, 1–8. [Google Scholar] [CrossRef]
- Jimenez, J.J.; Iribarren, J.L.; Lorente, L.; Rodriguez, J.M.; Hernandez, D.; Nassar, I.; Perez, R.; Brouard, M.; Milena, A.; Martinez, R.; et al. Tranexamic acid attenuates inflammatory response in cardiopulmonary bypass surgery through blockade of fibrinolysis: A case control study followed by a randomized double-blind controlled trial. Crit. Care 2007, 11, R117. [Google Scholar] [CrossRef]
- Lei, Y.-T.; Xie, J.-W.; Huang, Q.; Huang, W.; Pei, F.-X. The antifibrinolytic and anti-inflammatory effects of a high initial-dose tranexamic acid in total knee arthroplasty: A randomized controlled trial. Int. Orthop. 2019, 44, 477–486. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.; Hu, Q.; Ma, J.; Huang, Q.; Pei, F. Multiple boluses of intravenous tranexamic acid to reduce hidden blood loss and the inflammatory response following enhanced-recovery primary total hip arthroplasty. Bone Jt. J. 2017, 99-B, 1442–1449. [Google Scholar] [CrossRef] [PubMed]
- Roberts, I.; Shakur, H.; Coats, T.; Hunt, B.; Balogun, E.; Barnetson, L.; Cook, L.; Kawahara, T.; Perel, P.; Prieto-Merino, D.; et al. The CRASH-2 trial: A randomised controlled trial and economic evaluation of the effects of tranexamic acid on death, vascular occlusive events and transfusion requirement in bleeding trauma patients. Health Technol. Assess. 2013, 17, 1–79. [Google Scholar] [CrossRef] [PubMed]
- Morrison, J.J.; DuBose, J.J.; Rasmussen, T.E.; Midwinter, M.J. Military Application of Tranexamic Acid in Trauma Emergency Resuscitation (MATTERs) Study. Arch. Surg. 2012, 147, 113–119. [Google Scholar] [CrossRef]
- Anderson, T.N.; Hinson, H.E.; Dewey, E.N.; Rick, E.A.; Schreiber, M.A.; Rowell, S.E. Early Tranexamic Acid Administration After Traumatic Brain Injury Is Associated with Reduced Syndecan-1 and Angiopoietin-2 in Patients with Traumatic Intracranial Hemorrhage. J. Head Trauma Rehabil. 2020, 35, 317–323. [Google Scholar] [CrossRef]
- Yoo, J.S.; Ahn, J.; Karmarkar, S.S.; Lamoutte, E.H.; Singh, K. The use of tranexamic acid in spine surgery. Ann. Transl. Med. 2019, 7, S172. [Google Scholar] [CrossRef] [PubMed]
- Diebel, M.E.; Diebel, L.N.; Manke, C.W.; Liberati, D.M.; Whittaker, J.R. Early tranexamic acid administration: A protective effect on gut barrier function following ischemia/reperfusion injury. J. Trauma Acute Care Surg. 2015, 79, 1015–1022. [Google Scholar] [CrossRef] [PubMed]
- Grassin-Delyle, S.; Tremey, B.; Abe, E.; Fischler, M.; Alvarez, J.C.; Devillier, P.; Urien, S. Population pharmacokinetics of tranexamic acid in adults undergoing cardiac surgery with cardiopulmonary bypass. Br. J. Anaesth. 2013, 111, 916–924. [Google Scholar] [CrossRef] [PubMed]
- Potter, D.R.; Jiang, J.; Damiano, E.R. The Recovery Time Course of the Endothelial Cell Glycocalyx In Vivo and Its Implications In Vitro. Circ. Res. 2009, 104, 1318–1325. [Google Scholar] [CrossRef] [PubMed]
- Rahbar, E.; Cardenas, J.C.; Baimukanova, G.; Usadi, B.; Bruhn, R.; Pati, S.; Ostrowski, S.R.; Johansson, P.I.; Holcomb, J.B.; Wade, C.E. Endothelial glycocalyx shedding and vascular permeability in severely injured trauma patients. J. Transl. Med. 2015, 13, 1–7. [Google Scholar] [CrossRef] [PubMed]
| Variable | Tranexamic Acid n = 60 | Control n = 61 |
|---|---|---|
| Patient demographic data | ||
| Age (years) | 67 ± 8 | 68 ± 8 |
| Female gender | 36 (60.0%) | 33 (54.1%) |
| Height (cm) | 159.7 ± 8.5 | 158.6 ± 8.1 |
| Weight (kg) | 65.4 ± 10.6 | 63.8 ± 10.5 |
| Hypertension | 33 (55.0%) | 40 (65.6%) |
| Diabetes mellitus | 11 (18.3%) | 19 (31.1%) |
| Cerebrovascular accident | 0 (0.0%) | 2 (3.3%) |
| Asthma | 1 (1.7%) | 3 (4.9%) |
| Cancer | 3 (5.0%) | 6 (9.8%) |
| Preoperative medications | ||
| Beta blocker | 5 (8.3%) | 8 (13.1%) |
| Calcium channel blocker | 14 (23.3%) | 16 (26.2%) |
| RAS inhibitor | 21 (35.0%) | 24 (39.3%) |
| Diuretics | 4 (6.7%) | 4 (6.6%) |
| ASA class | 2 (2–2) | 2 (2–2) |
| Preoperative Laboratory Data | ||
| Serum C-reactive protein level (mg/L) | 1.0 (0.5–2.4) | 0.7 (0.4–1.7) |
| Serum creatinine level (mg/dL) | 0.75 ± 0.17 | 0.80 ± 0.18 |
| Estimated GFR | 88.7 ± 11.4 | 85.0 ± 12.7 |
| Variable | Tranexamic Acid n = 60 | Control n = 61 | p-Value |
|---|---|---|---|
| Intraoperative Data | |||
| Levels fused | 2 (1–3) | 2 (1–2) | 0.605 |
| Duration of anesthesia (min) | 240 ± 71 | 240 ± 68 | 0.996 |
| Duration of operation (min) | 186 ± 65 | 183 ± 63 | 0.819 |
| Crystalloids (mL) | 1475 (1050–1825) | 1400 (1050–1650) | 0.773 |
| Colloids (mL) | 250 (0–500) | 100 (0–500) | 0.716 |
| Urine output (ml) | 300 (150–535) | 260 (150–500) | 0.646 |
| Blood loss (mL) | 500 (300–800) | 500 (300–650) | 0.598 |
| Transfused red blood cell (mL) | 0 (0–0) | 0 (0–0) | 0.099 |
| Number of patient requiring vasopressor support * | 41 (68.3%) | 47 (77.0%) | 0.282 |
| Early postoperative complications | |||
| Hypotension requiring vasopressor support | 0 (0.0%) | 2 (3.3%) | 0.496 |
| Desaturation | 3 (5.0%) | 5 (8.2%) | 0.717 |
| Acute kidney injury | 0 (0.0%) | 3 (4.9%) | 0.244 |
| Total † | 3 (5.0%) | 8 (13.1%) | 0.121 |
| Variable | Tranexamic Acid n = 60 | Control n = 61 | p-Value † | ||
|---|---|---|---|---|---|
| Syndecan-1 (ng/mL) | p-Value * | p-Value * | |||
| T0 | 30.0 (19.6–41.2) | 27.3 (19.4–37.1) | |||
| T1 | 28.4 (18.7–38.0) | 0.063 | 28.8 (19.7–36.9) | 0.005 | 0.617 |
| T2 | 32.6 (20.1–43.0) | 0.324 | 30.7 (22.1–40.9) | <0.001 | 0.907 |
| T0-T1 difference | −1.6 (−5.3–2.6) | 2.2 (−0.7–4.8) | 0.001 | ||
| T0-T2 difference | 0.0 (−3.3–5.5) | 3.6 (−0.1–9.3) | 0.013 | ||
| Heparan sulfate (ng/mL) | |||||
| T0 | 1.7 (1.0–2.5) | 1.6 (0.9–2.9) | 0.762 | ||
| T1 | 2.2 (1.3–4.2) | <0.001 | 1.9 (1.1–3.4) | <0.001 | 0.544 |
| T2 | 2.7 (1.8–4.2) | <0.001 | 2.7 (1.5–4.4) | <0.001 | 0.893 |
| T0-T1 difference | 0.4 (0.1–1.0) | 0.2 (0.0–0.9) | 0.272 | ||
| T0-T2 difference | 0.8 (0.3–1.8) | 0.9 (0.4–1.7) | 0.998 | ||
| Unadjusted OR (95% CI) | p-Value | Adjusted OR * (95% CI) | p-Value | |
|---|---|---|---|---|
| Syndecan-1 (ng/mL) | ||||
| T0 | 1.02 (0.99–1.05) | 0.128 | 1.02 (0.99–1.05) | 0.139 |
| T1 | 1.02 (1.00–1.04) | 0.102 | 1.02 (1.00–1.04) | 0.093 |
| T2 | 1.03 (1.00–1.06) | 0.024 | 1.03 (1.00–1.06) | 0.023 |
| T0-T1 difference | 1.03 (0.99–1.08) | 0.147 | 1.04 (0.99–1.09) | 0.123 |
| T0-T2 difference | 1.08 (1.02–1.14) | 0.006 | 1.08 (1.03–1.15) | 0.005 |
| Heparan sulfate (ng/mL) | ||||
| T0 | 1.09 (0.97–1.21) | 0.154 | 1.10 (0.98–1.23) | 0.114 |
| T1 | 1.08 (0.95–1.22) | 0.255 | 1.09 (0.96–1.24) | 0.205 |
| T2 | 1.10 (0.97–1.25) | 0.157 | 1.11 (0.97–1.27) | 0.120 |
| T0-T1 difference | 0.65 (0.40–1.10) | 0.111 | 0.62 (0.36–1.07) | 0.088 |
| T0-T2 difference | 0.94 (0.65–1.34) | 0.715 | 0.93 (0.64–1.35) | 0.696 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.J.; Lee, B.; Lee, B.H.; Kim, S.Y.; Jun, B.; Choi, Y.S. The Effect of Tranexamic Acid Administration on Early Endothelial Damage Following Posterior Lumbar Fusion Surgery. J. Clin. Med. 2021, 10, 1415. https://doi.org/10.3390/jcm10071415
Kim HJ, Lee B, Lee BH, Kim SY, Jun B, Choi YS. The Effect of Tranexamic Acid Administration on Early Endothelial Damage Following Posterior Lumbar Fusion Surgery. Journal of Clinical Medicine. 2021; 10(7):1415. https://doi.org/10.3390/jcm10071415
Chicago/Turabian StyleKim, Hye Jin, Bora Lee, Byung Ho Lee, So Yeon Kim, Byongnam Jun, and Yong Seon Choi. 2021. "The Effect of Tranexamic Acid Administration on Early Endothelial Damage Following Posterior Lumbar Fusion Surgery" Journal of Clinical Medicine 10, no. 7: 1415. https://doi.org/10.3390/jcm10071415
APA StyleKim, H. J., Lee, B., Lee, B. H., Kim, S. Y., Jun, B., & Choi, Y. S. (2021). The Effect of Tranexamic Acid Administration on Early Endothelial Damage Following Posterior Lumbar Fusion Surgery. Journal of Clinical Medicine, 10(7), 1415. https://doi.org/10.3390/jcm10071415






