Sex-Specific Associations between Blood Pressure and Risk of Atrial Fibrillation Subtypes in the Tromsø Study
Abstract
:1. Introduction
2. Materials and Methods
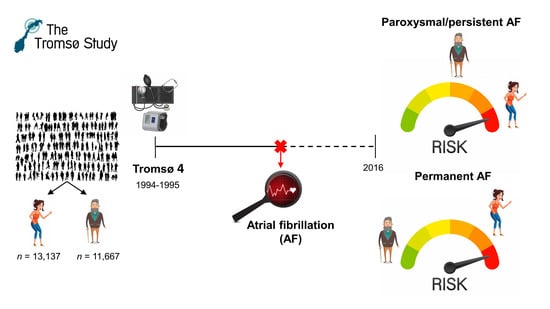
2.1. Study Design and Participants
2.2. Data Collection
2.3. Follow-Up and Detection of Incident Atrial Fibrillation
2.4. Statistical Analyses
3. Results
3.1. Baseline Characteristic
3.2. Systolic Blood Pressure and Incident Atrial Fibrillation Subtypes
3.3. Hypertension and Incident Atrial Fibrillation Subtypes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gillis, A.M. Atrial Fibrillation and Ventricular Arrhythmias. Circulation 2017, 135, 593–608. [Google Scholar] [CrossRef]
- Chugh, S.S.; Havmoeller, R.; Narayanan, K.; Singh, D.; Rienstra, M.; Benjamin, E.J.; Gillum, R.F.; Kim, Y.-H.; McAnulty, J.H.; Zheng, Z.-J.; et al. Worldwide Epidemiology of Atrial Fibrillation. Circulation 2014, 129, 837–847. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nyrnes, A. Atrial Fibrillation in the Tromsø Study 1994–2007: Risk Factors, Occurrence and Gender Differences. Ph.D. Thesis, UiT The Arctic University of Norway, Tromsø, Norway, 2016. [Google Scholar]
- Ball, J.; Carrington, M.J.; McMurray, J.J.; Stewart, S. Atrial fibrillation: Profile and burden of an evolving epidemic in the 21st century. Int. J. Cardiol. 2013, 167, 1807–1824. [Google Scholar] [CrossRef] [PubMed]
- Kjerpeseth, L.J.; Ellekjær, H.; Selmer, R.; Ariansen, I.; Furu, K.; Skovlund, E. Trends in use of warfarin and direct oral anticoagulants in atrial fibrillation in Norway, 2010 to 2015. Eur. J. Clin. Pharmacol. 2017, 73, 1417–1425. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huxley, R.R.; Lopez, F.L.; Folsom, A.R.; Agarwal, S.K.; Loehr, L.R.; Soliman, E.Z.; MacLehose, R.; Konety, S.; Alonso, A. Absolute and Attributable Risks of Atrial Fibrillation in Relation to Optimal and Borderline Risk Factors. Circulation 2011, 123, 1501–1508. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verdecchia, P.; Staessen, J.A.; Angeli, F.; de Simone, G.; Achilli, A.; Ganau, A.; Mureddu, G.; Pede, S.; Maggioni, A.P.; Lucci, D.; et al. Usual versus tight control of systolic blood pressure in non-diabetic patients with hypertension (Cardio-Sis): An open-label randomised trial. Lancet 2009, 374, 525–533. [Google Scholar] [CrossRef]
- Ogunsua, A.A.; Shaikh, A.Y.; Ahmed, M.; McManus, D.D. Atrial Fibrillation and Hypertension: Mechanistic, Epidemiologic, and Treatment Parallels. Methodist DeBakey Cardiovasc. J. 2015, 11, 228–234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kato, T.; Yamashita, T.; Sagara, K.; Iinuma, H.; Fu, L.-T. Progressive Nature of Paroxysmal Atrial Fibrillation. Circ. J. 2004, 68, 568–572. [Google Scholar] [CrossRef] [Green Version]
- de Vos, C.B.; Pisters, R.; Nieuwlaat, R.; Prins, M.H.; Tieleman, R.G.; Coelen, R.-J.S.; Heijkant, A.C.V.D.; Allessie, M.A.; Crijns, H.J. Progression From Paroxysmal to Persistent Atrial Fibrillation. J. Am. Coll. Cardiol. 2010, 55, 725–731. [Google Scholar] [CrossRef] [Green Version]
- Thomas, M.C.; Dublin, S.; Kaplan, R.C.; Glazer, N.L.; Lumley, T.; Longstreth, W.T.; Smith, N.L.; Psaty, B.M.; Siscovick, D.S.; Heckbert, S.R. Blood Pressure Control and Risk of Incident Atrial Fibrillation. Am. J. Hypertens. 2008, 21, 1111–1116. [Google Scholar] [CrossRef]
- Sandhu, R.K.; Conen, D.; Tedrow, U.B.; Fitzgerald, K.C.; Pradhan, A.D.; Ridker, P.M.; Glynn, R.J.; Albert, C.M. Predisposing Factors Associated With Development of Persistent Compared with Paroxysmal Atrial Fibrillation. J. Am. Heart Assoc. 2014, 3, e000916. [Google Scholar] [CrossRef] [Green Version]
- Schnabel, R.B.; Yin, X.; Gona, P.; Larson, M.G.; Beiser, A.S.; McManus, D.D.; Newton-Cheh, C.; Lubitz, S.A.; Magnani, J.W.; Ellinor, P.T.; et al. 50 year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham Heart Study: A cohort study. Lancet 2015, 386, 154–162. [Google Scholar] [CrossRef] [Green Version]
- Magnussen, C.; Niiranen, T.J.; Ojeda, F.M.; Gianfagna, F.; Blankenberg, S.; Njølstad, I.; Vartiainen, E.; Sans, S.; Pasterkamp, G.; Hughes, M.; et al. Sex Differences and Similarities in Atrial Fibrillation Epidemiology, Risk Factors, and Mortality in Community Cohorts. Results From the BiomarCaRE Consortium. Circulation 2017, 136, 1588–1597. [Google Scholar] [CrossRef] [Green Version]
- Madan, N.; Itchhaporia, D.; Albert, C.M.; Aggarwal, N.T.; Volgman, A.S. Atrial Fibrillation and Heart Failure in Women. Heart Fail. Clin. 2019, 15, 55–64. [Google Scholar] [CrossRef]
- Sharashova, E.; Wilsgaard, T.; Ball, J.; Morseth, B.; Gerdts, E.; Hopstock, L.A.; Mathiesen, E.B.; Schirmer, H.; Løchen, M.-L. Long-term blood pressure trajectories and incident atrial fibrillation in women and men: The Tromsø Study. Eur. Heart J. 2020, 41, 1554–1562. [Google Scholar] [CrossRef]
- Conen, D.; Tedrow, U.B.; Koplan, B.A.; Glynn, R.J.; Buring, J.E.; Albert, C.M. Influence of Systolic and Diastolic Blood Pressure on the Risk of Incident Atrial Fibrillation in Women. Circulation 2009, 119, 2146–2152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strandberg, T.E.; Pitkala, K. What is the most important component of blood pressure: Systolic, diastolic or pulse pressure? Curr. Opin. Nephrol. Hypertens. 2003, 12, 293–297. [Google Scholar] [CrossRef] [PubMed]
- Kannel, W.B. Elevated systolic blood pressure as a cardiovascular risk factor. Am. J. Cardiol. 2000, 85, 251–255. [Google Scholar] [CrossRef]
- Nyrnes, A.; Mathiesen, E.B.; Njølstad, I.; Wilsgaard, T.; Løchen, M.-L. Palpitations are predictive of future atrial fibrillation. An 11-year follow-up of 22,815 men and women: The Tromsø Study. Eur. J. Prev. Cardiol. 2013, 20, 729–736. [Google Scholar] [CrossRef] [Green Version]
- Jacobsen, B.K.; Eggen, A.E.; Mathiesen, E.B.; Wilsgaard, T.; Njølstad, I. Cohort profile: The Tromsø Study. Int. J. Epidemiol. 2011, 41, 961–967. [Google Scholar] [CrossRef]
- Morseth, B.; Ahmed, L.A.; Bjørnerem, Å.; Emaus, N.; Jacobsen, B.K.; Joakimsen, R.M.; Størmer, J.; Wilsgaard, T.; Jørgensen, L. Leisure time physical activity and risk of non-vertebral fracture in men and women aged 55 years and older: The Tromsø Study. Eur. J. Epidemiol. 2012, 27, 463–471. [Google Scholar] [CrossRef] [PubMed]
- Kirchhof, P.; Benussi, S.; Kotecha, D.; Ahlsson, A.; Atar, D.; Casadei, B.; Castella, M.; Christoph-Diener, H.; Heidbuchel, H.; Hendriks, J.; et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur. Heart J. 2016, 37, 2893–2962. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Charitos, E.I.; Pürerfellner, H.; Glotzer, T.V.; Ziegler, P.D. Clinical Classifications of Atrial Fibrillation Poorly Reflect Its Temporal Persistence. J. Am. Coll. Cardiol. 2014, 63, 2840–2848. [Google Scholar] [CrossRef] [Green Version]
- O’Neal, W.T.; Soliman, E.Z.; Qureshi, W.; Alonso, A.; Heckbert, S.R.; Herrington, D. Sustained pre–hypertensive blood pressure and incident atrial fibrillation: The Multi–Ethnic Study of Atherosclerosis. J. Am. Soc. Hypertens. 2015, 9, 191–196. [Google Scholar] [CrossRef] [Green Version]
- Okin, P.M.; Hille, D.A.; Larstorp, A.C.K.; Wachtell, K.; Kjeldsen, S.E.; Dahlöf, B.; Devereux, R.B. Effect of Lower On-Treatment Systolic Blood Pressure on the Risk of Atrial Fibrillation in Hypertensive Patients. Hypertension 2015, 66, 368–373. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ko, D.; Rahman, F.; Schnabel, R.B.; Yin, X.; Benjamin, E.J.; Christophersen, I.E. Atrial fibrillation in women: Epidemiology, pathophysiology, presentation, and prognosis. Nat. Rev. Cardiol. 2016, 13, 321–332. [Google Scholar] [CrossRef]
- Verdecchia, P.; Reboldi, G.; Gattobigio, R.; Bentivoglio, M.; Borgioni, C.; Angeli, F.; Carluccio, E.; Sardone, M.G.; Porcellati, C. Atrial Fibrillation in Hypertension. Hypertension 2003, 41, 218–223. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yildiz, M.; Oktay, A.A.; Stewart, M.H.; Milani, R.V.; Ventura, H.O.; Lavie, C.J. Left ventricular hypertrophy and hypertension. Prog. Cardiovasc. Dis. 2020, 63, 10–21. [Google Scholar] [CrossRef]
- Westerman, S. Gender Differences in Atrial Fibrillation: A Review of Epidemiology, Management, and Outcomes. Curr. Cardiol. Rev. 2019, 15, 136–144. [Google Scholar] [CrossRef]
- Schnabel, R.B.; Pecen, L.; Ojeda, F.M.; Lucerna, M.; Rzayeva, N.; Blankenberg, S.; Darius, H.; Kotecha, D.; De Caterina, R.; Kirchhof, P. Gender differences in clinical presentation and 1-year outcomes in atrial fibrillation. Heart 2017, 103, 1024–1030. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lip, G.Y.; Laroche, C.; Boriani, G.; Cimaglia, P.; Dan, G.-A.; Santini, M.; Kalarus, Z.; Rasmussen, L.H.; Popescu, M.I.; Tica, O.; et al. Sex-related differences in presentation, treatment, and outcome of patients with atrial fibrillation in Europe: A report from the Euro Observational Research Programme Pilot survey on Atrial Fibrillation. Europace 2014, 17, 24–31. [Google Scholar] [CrossRef]
- Gerdts, E.; Regitz-Zagrosek, V. Sex differences in cardiometabolic disorders. Nat. Med. 2019, 25, 1657–1666. [Google Scholar] [CrossRef] [PubMed]
- Peters, S.A.E.; Woodward, M. Established and novel risk factors for atrial fibrillation in women compared with men. Heart 2018, 105, 226–234. [Google Scholar] [CrossRef]
- Gerdts, E.; Okin, P.M.; De Simone, G.; Cramariuc, D.; Wachtell, K.; Boman, K.; Devereux, R.B. Gender Differences in Left Ventricular Structure and Function During Antihypertensive Treatment. Hypertension 2008, 51, 1109–1114. [Google Scholar] [CrossRef] [Green Version]
- Gerdts, E.; Izzo, R.; Mancusi, C.; Losi, M.A.; Manzi, M.V.; Canciello, G.; De Luca, N.; Trimarco, B.; de Simone, G. Left ventricular hypertrophy offsets the sex difference in cardiovascular risk (the Campania Salute Network). Int. J. Cardiol. 2018, 258, 257–261. [Google Scholar] [CrossRef] [PubMed]
- Kannel, W.B.; Abbott, R.D.; Savage, D.D.; McNamara, P.M. Coronary heart disease and atrial fibrillation: The Framingham Study. Am. Heart J. 1983, 106, 389–396. [Google Scholar] [CrossRef]
- Larstorp, A.C.K.; Stokke, I.M.; Kjeldsen, S.E.; Olsen, M.H.; Okin, P.M.; Devereux, R.B.; Wachtell, K. Antihypertensive therapy prevents new-onset atrial fibrillation in patients with isolated systolic hypertension: The LIFE study. Blood Press. 2019, 28, 317–326. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.; Mancia, G.; Spiering, W.; Rosei, E.A.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.F.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef]
- Myers, M.G.; Asmar, R.; Staessen, J.A. Office blood pressure measurement in the 21st century. J. Clin. Hypertens. 2018, 20, 1104–1107. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Women | Men | |||||||
|---|---|---|---|---|---|---|---|---|
| Characteristics | No AF | Parox/Pers | Perm | p-Value | No AF | Parox/Pers | Perm | p-Value |
| n (%) | 12.223 (93.0) | 501 (3.8) | 413 (3.1) | 10.563 (90.5) | 606 (5.2) | 498 (4.3) | ||
| Age, years | 44.4 (14.0) | 62.3 (11.9) | 67.3 (9.2) | <0.001 | 43.8 (13.0) | 56.7 (12.7) | 60.7 (10.8) | <0.001 |
| Systolic blood pressure, mmHg | 130.3 (20.2) | 137.1 (25.6) | 138.1 (24.0) | <0.001 | 136.3 (15.8) | 140.7 (21.4) | 139.3 (21.5) | <0.001 |
| Diastolic blood pressure, mmHg | 75.7 (11.9) | 78.3 (14.2) | 77.7 (13.5) | <0.001 | 79.4 (11.1) | 81.3 (12.4) | 81.0 (13.1) | <0.001 |
| Hypertension a, n (%) | 3051 (21.4) | 340 (33.1) | 326 (34.9) | <0.001 | 3879 (38.4) | 364 (47.7) | 325 (48.5) | <0.001 |
| Antihypertensive medication use, n (%) | 481 (2.6) | 94 (5.2) | 115 (6.7) | <0.001 | 413 (2.9) | 90 (5.6) | 88 (5.7) | <0.001 |
| Body mass index, kg/m2 | 24.6 (4.1) | 25.6 (4.7) | 26.6 (5.4) | <0.001 | 25.5 (3.2) | 26.1 (3.6) | 26.9 (3.5) | <0.001 |
| Total cholesterol, mmol/L | 6.00 (1.35) | 6.06 (1.34) | 5.84 (1.22) | 0.014 | 6.02 (1.21) | 6.00 (1.14) | 5.97 (1.13) | 0.677 |
| HDL cholesterol, mmol/L | 1.64 (0.40) | 1.61 (0.41) | 1.60 (0.48) | 0.043 | 1.35 (0.35) | 1.31 (0.35) | 1.32 (0.37) | 0.023 |
| Triglycerides, mmol/L | 1.31 (0.81) | 1.45 (1.18) | 1.45 (1.08) | <0.001 | 1.77 (1.19) | 1.77 (0.99) | 1.82 (1.15) | 0.726 |
| Current daily smoking, n (%) | 4612 (36.9) | 159 (38.4) | 79 (25.8) | <0.001 | 4070 (38.2) | 174 (30.1) | 144 (30.9) | <0.001 |
| Leisure time physical activity n (%) | ||||||||
| Inactive | 1020 (7.6) | 76 (7.2) | 76 (7.5) | 0.875 | 822 (7.9) | 51 (6.4) | 47 (6.8) | 0.221 |
| Low activity | 5201 (43.0) | 214 (43.5) | 176 (43.2) | 0.977 | 4168 (39.7) | 223 (37.4) | 174 (36.2) | 0.212 |
| Moderate activity | 5367 (43.9) | 184 (41.8) | 146 (41.6) | 0.526 | 4472 (42.9) | 286 (46.6) | 233 (46.5) | 0.088 |
| High activity | 505 (3.7) | 20 (6.3) | 11 (5.1) | 0.046 | 997 (8.7) | 45 (9.1) | 37 (10.3) | 0.602 |
| Education, n (%) | ||||||||
| Primary/partly secondary education | 4097 (33.8) | 300 (33.6) | 296 (38.7) | 0.207 | 2963 (28.8) | 253 (30.0) | 202 (25.3) | 0.145 |
| Upper secondary education | 4388 (34.6) | 126 (33.7) | 67 (25.2) | 0.005 | 4028 (37.3) | 192 (35.5) | 181 (42.0) | 0.079 |
| College/university less than 4 years | 1832 (12.8) | 37 (12.8) | 23 (12.4) | 0.992 | 1791 (16.1) | 73 (14.2) | 66 (16.7) | 0.465 |
| College/university 4 years or more | 1857 (13.1) | 34 (11.4) | 22 (11.4) | 0.563 | 1756 (15.3) | 85 (17.4) | 47 (13.1) | 0.223 |
| History of myocardial infarction, n (%) | 97 (0.3) | 21 (0.6) | 18 (0.5) | 0.085 | 251 (1.4) | 53 (2.3) | 52 (2.2) | 0.001 |
| History of angina pectoris, n (%) | 249 (0.7) | 58 (1.3) | 51 (1.0) | <0.001 | 286 (1.5) | 84 (3.6) | 67 (2.7) | <0.001 |
| History of stroke, n (%) | 99 (0.5) | 18 (1.0) | 9 (0.4) | 0.090 | 110 (0.7) | 9 (0.4) | 23 (1.2) | 0.028 |
| History of diabetes mellitus, n (%) | 128 (0.8) | 28 (1.8) | 19 (1.2) | <0.001 | 113 (0.8) | 24 (1.4) | 13 (0.8) | 0.045 |
| Women | Men | |||||||
|---|---|---|---|---|---|---|---|---|
| Paroxysmal/Persistent AF | Permanent AF | Paroxysmal/Persistent AF | Permanent AF | |||||
| HT Group a | HR (95% CI) | p-Value | HR (95% CI) | p-Value | HR (95% CI) | p-Value | HR (95% CI) | p-Value |
| Normotensive | Reference | Reference | Reference | Reference | ||||
| Controlled HT | 1.71 (0.92−3.16) | 0.088 | 3.22 (1.87−5.55) | <0.001 | 1.24 (0.73−2.09) | 0.426 | 1.82 (1.11−2.98) | 0.018 |
| Uncontrolled HT | 2.53 (1.85−3.46) | <0.001 | 3.11 (2.23−4.35) | <0.001 | 1.89 (1.41−2.52) | <0.001 | 1.66 (1.22−2.27) | 0.001 |
| Untreated HT | 1.70 (1.35−2.15) | <0.001 | 1.58 (1.19−2.09) | 0.002 | 1.24 (1.03−1.49) | 0.022 | 1.15 (0.93−1.42) | 0.195 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Espnes, H.; Ball, J.; Løchen, M.-L.; Wilsgaard, T.; Njølstad, I.; Mathiesen, E.B.; Gerdts, E.; Sharashova, E. Sex-Specific Associations between Blood Pressure and Risk of Atrial Fibrillation Subtypes in the Tromsø Study. J. Clin. Med. 2021, 10, 1514. https://doi.org/10.3390/jcm10071514
Espnes H, Ball J, Løchen M-L, Wilsgaard T, Njølstad I, Mathiesen EB, Gerdts E, Sharashova E. Sex-Specific Associations between Blood Pressure and Risk of Atrial Fibrillation Subtypes in the Tromsø Study. Journal of Clinical Medicine. 2021; 10(7):1514. https://doi.org/10.3390/jcm10071514
Chicago/Turabian StyleEspnes, Hilde, Jocasta Ball, Maja-Lisa Løchen, Tom Wilsgaard, Inger Njølstad, Ellisiv B. Mathiesen, Eva Gerdts, and Ekaterina Sharashova. 2021. "Sex-Specific Associations between Blood Pressure and Risk of Atrial Fibrillation Subtypes in the Tromsø Study" Journal of Clinical Medicine 10, no. 7: 1514. https://doi.org/10.3390/jcm10071514
APA StyleEspnes, H., Ball, J., Løchen, M. -L., Wilsgaard, T., Njølstad, I., Mathiesen, E. B., Gerdts, E., & Sharashova, E. (2021). Sex-Specific Associations between Blood Pressure and Risk of Atrial Fibrillation Subtypes in the Tromsø Study. Journal of Clinical Medicine, 10(7), 1514. https://doi.org/10.3390/jcm10071514