Somatoform Dissociative Symptoms Have No Impact on the Outcome of Trauma-Focused Treatment for Severe PTSD
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Treatment
2.4. Measurements
2.5. Data Analyses
3. Results
3.1. Patient Characteristics
3.2. Influence of Somatoform Dissociation on Treatment Outcome
3.3. Change in Somatoform Dissociative Symptoms Associated with Treatment
3.4. Exploration of Follow-Up Data
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cloitre, M.; Petkova, E.; Wang, J.; Lu, F. An examination of the influence of a sequential treatment on the course and impact of dissociation among women with PTSD related to childhood abuse. Depress. Anxiety 2012, 29, 709–717. [Google Scholar] [CrossRef]
- Cloitre, M.; Garvert, D.W.; Brewin, C.R.; Bryant, R.A.; Maercker, A. Evidence for proposed ICD-11 PTSD and complex PTSD: A latent profile analysis. Eur. J. Psychotraumatol. 2013, 4, 20706. [Google Scholar] [CrossRef]
- Cloitre, M.; Koenen, K.C.; Cohen, L.R.; Han, H. Skills Training in Affective and Interpersonal Regulation Followed by Exposure: A Phase-Based Treatment for PTSD Related to Childhood Abuse. J. Consult. Clin. Psychol. 2002, 70, 1067–1074. [Google Scholar] [CrossRef]
- Bae, H.; Kim, D.; Park, Y.C. Dissociation predicts treatment response in eye-movement desensitization and reprocessing for posttraumatic stress disorder. J. Trauma Dissociation 2016, 17, 112–130. [Google Scholar] [CrossRef] [PubMed]
- Haagen, J.F.; van Rijn, A.; Knipscheer, J.W.; van der Aa, N.; Kleber, R.J. The dissociative post-traumatic stress disorder (PTSD) subtype: A treatment outcome cohort study in veterans with PTSD. Br. J. Clin. Psychol. 2018, 57, 203–222. [Google Scholar] [CrossRef] [PubMed]
- Halvorsen, J.Ø.; Stenmark, H.; Neuner, F.; Nordahl, H.M. Does dissociation moderate treatment outcomes of narrative exposure therapy for PTSD? A secondary analysis from a randomized controlled clinical trial. Behav. Res. Ther. 2014, 57, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Hoeboer, C.M.; De Kleine, R.A.; Molendijk, M.L.; Schoorl, M.; Oprel, D.; Mouthaan, J.; Van der Does, W.; Van Minnen, A. Impact of dissociation on the effectiveness of psychotherapy for post-traumatic stress disorder: Meta-analysis. BJPsych Open 2020, 6, e53. [Google Scholar] [CrossRef] [PubMed]
- Wolf, E.J.; Lunney, C.A.; Schnurr, P.P. The influence of the dissociative subtype of posttraumatic stress disorder on treatment efficacy in female veterans and active-duty service members. J. Consult. Clin. Psychol. 2016, 84, 95. [Google Scholar] [CrossRef] [Green Version]
- Zoet, H.A.; Wagenmans, A.; van Minnen, A.; de Jongh, A. Presence of the dissociative subtype of PTSD does not moderate the outcome of intensive trauma-focused treatment for PTSD. Eur. J. Psychotraumatol. 2018, 9, 1468707. [Google Scholar] [CrossRef] [Green Version]
- De Jongh, A.D.; Resick, P.A.; Zoellner, L.A.; Van Minnen, A.; Lee, C.W.; Monson, C.M.; Foa, E.B.; Wheeler, K.; Broeke, E.T.; Feeny, N.; et al. Critical analysis of the current treatment guidelines for complex PTSD in adults. Depress. Anxiety 2016, 33, 359–369. [Google Scholar] [CrossRef]
- Van der Hart, O.; Nijenhuis, E.; Steele, K.; Brown, D. Trauma-related dissociation: Conceptual clarity lost and found. Aust. N. Z. J. Psychiatry 2004, 38, 906–914. [Google Scholar] [CrossRef]
- Holmes, E.A.; Brown, R.J.; Mansell, W.; Fearon, R.P.; Hunter, E.C.; Frasquilho, F.; Oakley, D.A. Are there two qualitatively distinct forms of dissociation? A review and some clinical implications. Clin. Psychol. Rev. 2005, 25, 1–23. [Google Scholar] [CrossRef]
- Butler, C.; Dorahy, M.J.; Middleton, W. The Detachment and Compartmentalization Inventory (DCI): An assessment tool for two potentially distinct forms of dissociation. J. Trauma Dissociation 2019, 20, 526–547. [Google Scholar] [CrossRef]
- Daniels, J.K.; Frewen, P.; Theberge, J.; Lanius, R.A. Structural brain aberrations associated with the dissociative subtype of post-traumatic stress disorder. Acta Psychiatr. Scand. 2016, 133, 232–240. [Google Scholar] [CrossRef]
- Lanius, R.A.; Vermetten, E.; Loewenstein, R.J.; Brand, B.; Schmahl, C.; Bremmer, D.; Spiegel, D. Emotion modulation in PTSD: Clinical and neurobiological evidence for a dissociative subtype. Am. J. Psychiatry 2010, 167, 640–647. [Google Scholar] [CrossRef] [Green Version]
- Perez, D.L.; Matin, N.; Williams, B.; Tanev, K.; Makris, N.; LaFrance, W.C., Jr.; Dickerson, B.C. Cortical thickness alterations linked to somatoform and psychological dissociation in functional neurological disorders. Hum. Brain Mapp. 2018, 39, 428–439. [Google Scholar] [CrossRef] [Green Version]
- Etkin, A.; Wager, T.D. Functional neuroimaging of anxiety: A meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. Am. J. Psychiatry 2007, 164, 1476–1488. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stevens, F.L.; Hurley, R.A.; Taber, K.H. Anterior cingulate cortex: Unique role in cognition and emotion. J. Neuropsychiatry Clin. Neurosci. 2011, 23, 121–125. [Google Scholar] [CrossRef] [PubMed]
- Littel, M.; Remijn, M.; Tinga, A.M.; Engelhard, I.M.; van den Hout, M.A. Stress Enhances the Memory-Degrading Effects of Eye Movements on Emotionally Neutral Memories. Clin. Psychol. Sci. 2017, 5, 316–324. [Google Scholar] [CrossRef]
- Schnyder, U.; Ehlers, A.; Elbert, T.; Foa, E.B.; Gersons, B.P.; Resick, P.A.; Shapiro, F.; Cloitre, M. Psychotherapies for PTSD: What do they have in common? Eur. J. Psychotraumatol. 2015, 6, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Jepsen, E.K.; Langeland, W.; Heir, T. Early traumatized inpatients high in psychoform and somatoform dissociation: Characteristics and treatment response. J. Trauma Dissociation 2014, 15, 572–587. [Google Scholar] [CrossRef] [PubMed]
- Myers, L.; Vaidya-Mathur, U.; Lancman, M. Prolonged exposure therapy for the treatment of patients diagnosed with psychogenic non-epileptic seizures (PNES) and post-traumatic stress disorder (PTSD). Epilepsy Behav. 2016, 66, 86–92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Minnen, A.; Van der Vleugel, B.; Van den Berg, D.; De Bont, P.; De Roos, C.; Van der Gaag, M.; De Jongh, A. Effectiveness of trauma-focused treatment for patients with psychosis with and without the dissociative subtype of post-traumatic stress disorder. Br. J. Psychiatry 2016, 209, 347–348. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association Publishing: Washington, DC, USA, 2013. [Google Scholar]
- De Jongh, A.; Ten Broeke, E. Handboek EMDR: Een Geprotocolleerde Behandelmethode Voorde Gevolgen van Psychotrauma [Handbook EMDR: A Protocoled Treatment Method for the Consequences of Psychotrauma]; Pearson Assessment and Information B.V.: Amsterdam, The Netherlands, 2013. [Google Scholar]
- Foa, E.B.; Hembree, E.A.; Rothbaum, B.O. Prolonged Exposure Therapy for PTSD: Emotional Processing of Traumatic Experiences: Therapist Guide; Oxford University Press: Oxford, UK, 2007. [Google Scholar] [CrossRef]
- Van Minnen, A.; Hendriks, L.; Kleine, R.D.; Hendriks, G.J.; Verhagen, M.; De Jongh, A. Therapist rotation: A novel approach for implementation of trauma-focused treatment in post-traumatic stress disorder. Eur. J. Psychotraumatol. 2018, 9, 1492836. [Google Scholar] [CrossRef] [Green Version]
- Van Woudenberg, C.; Voorendonk, E.M.; Bongaerts, H.; Zoet, H.A.; Verhagen, M.; Lee, C.W.; Van Minnen, A.; De Jongh, A. Effectiveness of an intensive treatment programme combining prolonged exposure and eye movement desensitization and reprocessing for severe post-traumatic stress disorder. Eur. J. Psychotraumatol. 2018, 9, 1487225. [Google Scholar] [CrossRef]
- Boeschoten, M.A.; Van der Aa, N.; Bakker, A.; Ter Heide, F.J.J.; Hoofwijk, M.C.; Jongedijk, R.A.; Van Minnen, A.; Elzinga, B.M.; Olff, M. Development and evaluation of the Dutch Clinician-administered PTSD scale for DSM-5 (CAPS-5). Eur. J. Psychotraumatol. 2018, 9. [Google Scholar] [CrossRef]
- Weathers, F.W.; Bovin, M.J.; Lee, D.J.; Sloan, D.M.; Schnurr, P.P.; Kaloupek, D.G.; Keane, T.M.; Marx, B.P. The Clinician-Administered PTSD Scale for DSM–5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Psychol. Assess. 2018, 30, 383–395. [Google Scholar] [CrossRef]
- Nijenhuis, E.R.; Spinhoven, P.; Van Dyck, R.; Van Der Hart, O.; Vanderlinden, J. The development and psychometric characteristics of the Somatoform Dissociation Questionnaire (SDQ-20). J. Nerv. Ment. Dis. 1996, 184, 688–694. [Google Scholar] [CrossRef] [PubMed]
- Nijenhuis, E.R. The scoring and interpretation of the SDQ-20 and SDQ-5. Act. Nerv. Super. 2010, 52, 24–28. [Google Scholar] [CrossRef] [Green Version]
- Boeschoten, M.A.; Bakker, A.; Jongedijk, R.A.; Olff, M. PTSD checklist for DSM-5-Nederlandstalige versie. Diemen Arq Psychotrauma Expert Groep 2014. [Google Scholar]
- Weathers, F.W.; Litz, B.T.; Keane, T.M.; Palmieri, P.A.; Marx, B.P.; Schnurr, P.P. The PTSD Checklist for dsm-5 (pcl-5). Scale available from the National Center for PTSD; 2013. Available online: https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp (accessed on 4 April 2021).
- Blevins, C.A.; Weathers, F.W.; Davis, M.T.; Witte, T.K.; Domino, J.L. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. J. Trauma. Stress 2015, 28, 489–498. [Google Scholar] [CrossRef]
- Overbeek, T.; Schruers, K.; Griez, E. MINI. Mini International Neuropsychiatric Interview. Dutch Version 5.0.0 DSM-IV; University of Maastricht: Maastricht, The Netherlands, 1999. [Google Scholar]
- Sheehan, D.V.; Lecrubier, Y.; Sheehan, K.H.; Amorim, P.; Janavs, J.; Weiller, E.; Hergueta, T.; Baker, R.; Dunbar, G.C. The Mini-International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry 1998, 59 (Suppl. 20), 22–33. [Google Scholar]
- Lecrubier, Y.; Sheehan, D.V.; Weiller, E.; Amorim, P.; Bonora, I.; Sheehan, K.H.; Janavs, J.; Dunbar, G.C. The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: Reliability and validity according to the CIDI. Eur. Psychiatry 1997, 12, 224–231. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analyses for the Social Sciences; Lawrence Erlbauni Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Hyland, P.; Shevlin, M.; Fyvie, C.; Cloitre, M.; Karatzias, T. The relationship between ICD-11 PTSD, complex PTSD, and dissociative experiences. J. Trauma Dissociation 2020, 21, 62–72. [Google Scholar] [CrossRef]
- Hansen, M.; Ross, J.; Armour, C. Evidence of the dissociative PTSD subtype: A systematic literature review of latent class and profile analytic studies of PTSD. J. Affect. Disord. 2017, 213, 59–69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lynch, S.M.; Forman, E.; Mendelsohn, M.; Herman, J. Attending to dissociation: Assessing change in dissociation and predicting treatment outcome. J. Trauma Dissociation 2008, 9, 301–319. [Google Scholar] [CrossRef]
- Knefel, M.; Tran, U.S.; Lueger-Schuster, B. The association of posttraumatic stress disorder, complex posttraumatic stress disorder, and borderline personality disorder from a network analytical perspective. J. Anxiety Disord. 2016, 43, 70–78. [Google Scholar] [CrossRef]
- Ross, J.; Armour, C.; Kerig, P.K.; Kidwell, M.C.; Kilshaw, R.E. A Network Analysis of Posttraumatic Stress Disorder and Dissociation in Trauma-Exposed Adolescents. J. Anxiety Disord. 2020, 102222. [Google Scholar] [CrossRef] [PubMed]
- Espirito Santo HM AD, E.; Pio-Abreu, J.L. Dissociative disorders and other psychopathological groups: Exploring the differences through the Somatoform Dissociation Questionnaire (SDQ-20). Braz. J. Psychiatry 2007, 29, 354–358. [Google Scholar]
- Maaranen, P.; Tanskanen, A.; Haatainen, K.; Koivumaa-Honkanen, H.; Hintikka, J.; Viinamäki, H. Somatoform dissociation and adverse childhood experiences in the general population. J. Nerv. Ment. Dis. 2004, 192, 337–342. [Google Scholar] [CrossRef] [PubMed]




| Total Sample (n = 219) | Positive Screen on SDQ-20 (n = 29) | Negative Screen on SDQ-20 (n = 190) | |
|---|---|---|---|
| Gender Women (%) | 174 (79.5%) | 25 (86.2%) | 149 (78.4%) |
| Mean age (SD) | 39.73 (12.27) | 36.34 (11.51) | 40.25 (12.32) |
| Three most frequent types of trauma (%) | |||
| Physical abuse | 90% | 96.6% | 88.9% |
| Sexual abuse | 82.2% | 100% | 79.5% |
| Armed violence | 55.3% | 62.1% | 54.2% |
| Comorbidity | |||
| Depression | 53.0% | 62.1% | 51.6% |
| Anxiety disorder | 48.4% | 31.0% | 51.1% |
| Suicidality | 74.4% | 89.7% | 72.1% |
| Dissociative subtype (%) | 101 (46.1%) | 22 (75.9%) | 79 (41.6%) |
| Pre-Treatment M (SD) | Post-Treatment M (SD) | Cohen’s d | ||
|---|---|---|---|---|
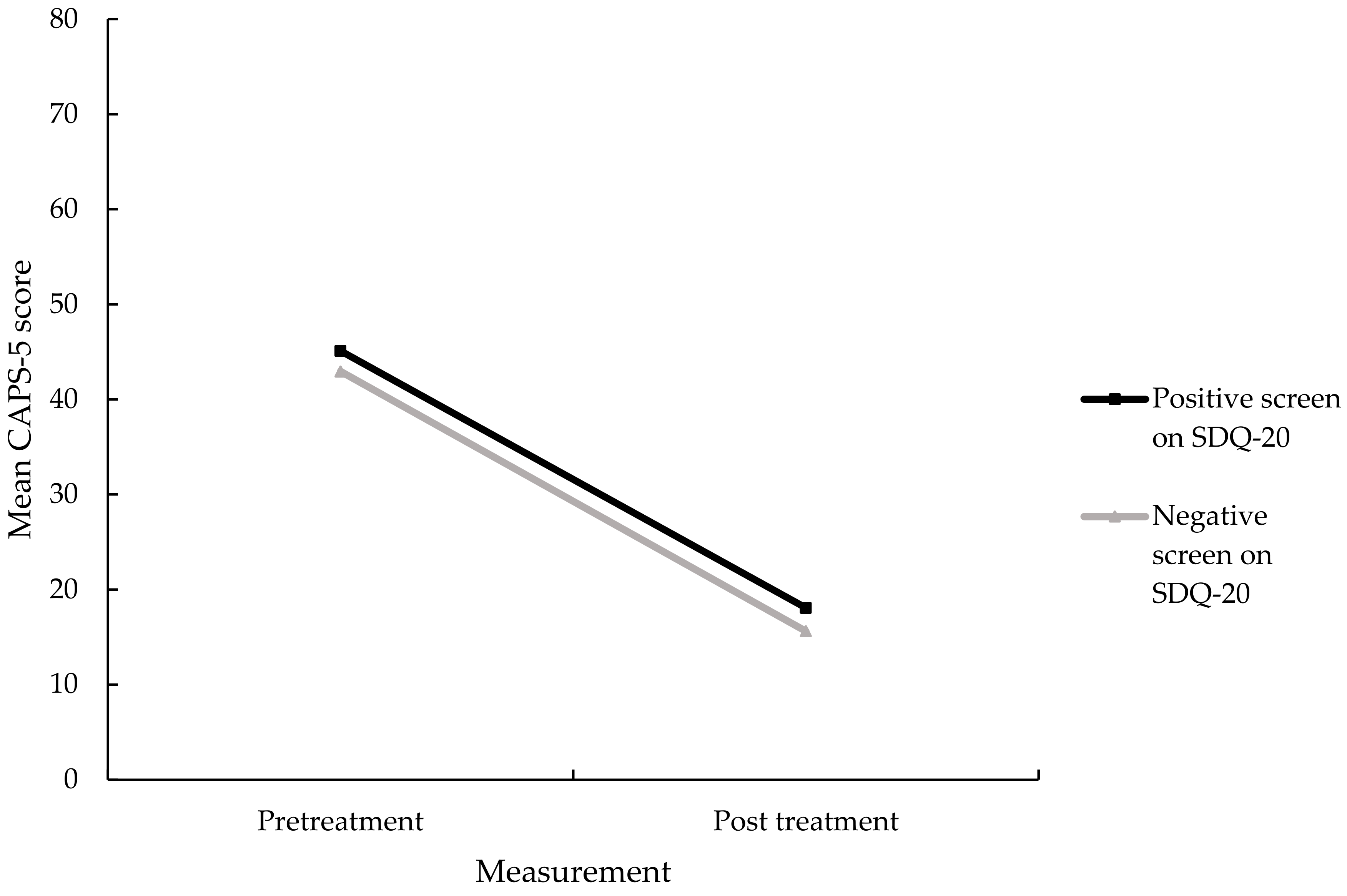
| CAPS (SD) | Positive screen | 45.10 (7.16) | 18.07 (13.30) | 2.53 |
| Negative screen | 42.94 (7.49) | 15.62 (14.88) | 2.32 | |
| Total | 43.22 (7.47) | 15.94 (14.68) | 2.34 | |
| SDQ-20 (SD) | Positive screen | 40.93 (6.50) | 27.38 (6.82) | 2.03 |
| Negative screen | 25.39 (4.13) | 22.59 (3.56) | 0.79 | |
| Total | 27.45 (6.93) | 23.22 (4.43) | 0.73 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zoet, H.A.; de Jongh, A.; van Minnen, A. Somatoform Dissociative Symptoms Have No Impact on the Outcome of Trauma-Focused Treatment for Severe PTSD. J. Clin. Med. 2021, 10, 1553. https://doi.org/10.3390/jcm10081553
Zoet HA, de Jongh A, van Minnen A. Somatoform Dissociative Symptoms Have No Impact on the Outcome of Trauma-Focused Treatment for Severe PTSD. Journal of Clinical Medicine. 2021; 10(8):1553. https://doi.org/10.3390/jcm10081553
Chicago/Turabian StyleZoet, Harmen A., Ad de Jongh, and Agnes van Minnen. 2021. "Somatoform Dissociative Symptoms Have No Impact on the Outcome of Trauma-Focused Treatment for Severe PTSD" Journal of Clinical Medicine 10, no. 8: 1553. https://doi.org/10.3390/jcm10081553






