Coaching via Telehealth: Caregiver-Mediated Interventions for Young Children on the Waitlist for an Autism Diagnosis Using Single-Case Design
Abstract
1. Introduction
1.1. Waitlists for Autism Diagnosis
1.2. Early Intervention for ASD
1.3. ABA Intervention Strategies for Higher-Order RRBIs
1.4. Vital Components for Accessible and Effective Early Intervention
1.5. Purpose of this Study
2. Participants, Materials, and Methods
2.1. Participants
2.2. Setting
2.3. Researcher Roles
2.4. Telehealth Equipment
2.5. Intervention Materials
2.6. General Procedures
2.6.1. Phase 1: Intake
2.6.2. Phase 2: Baseline
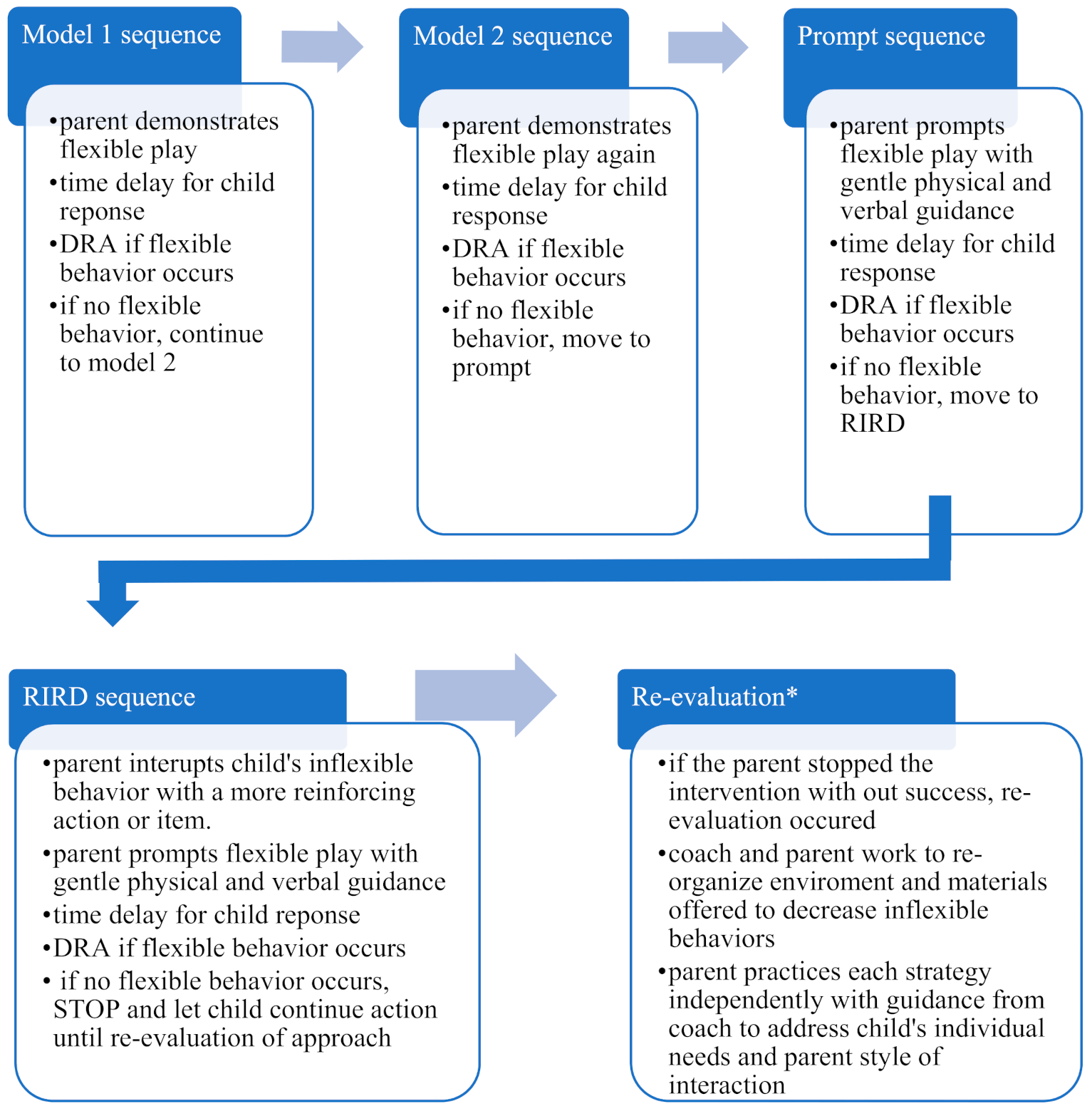
2.6.3. Phase 3: Intervention
2.6.4. Phase 4: Post-Intervention
2.7. Experimental Design, Analysis, and Response Measurement
2.7.1. Experimental Design and Analysis
2.7.2. Measures for the Dependent Variables
2.7.3. Pre and Post Measures
2.8. Fidelity, Reliability, and Social Validity
2.8.1. Coach Fidelity
2.8.2. Parent Treatment Fidelity
2.8.3. Reliability
2.8.4. Intervention Procedural Fidelity
2.8.5. Social Validity
3. Results
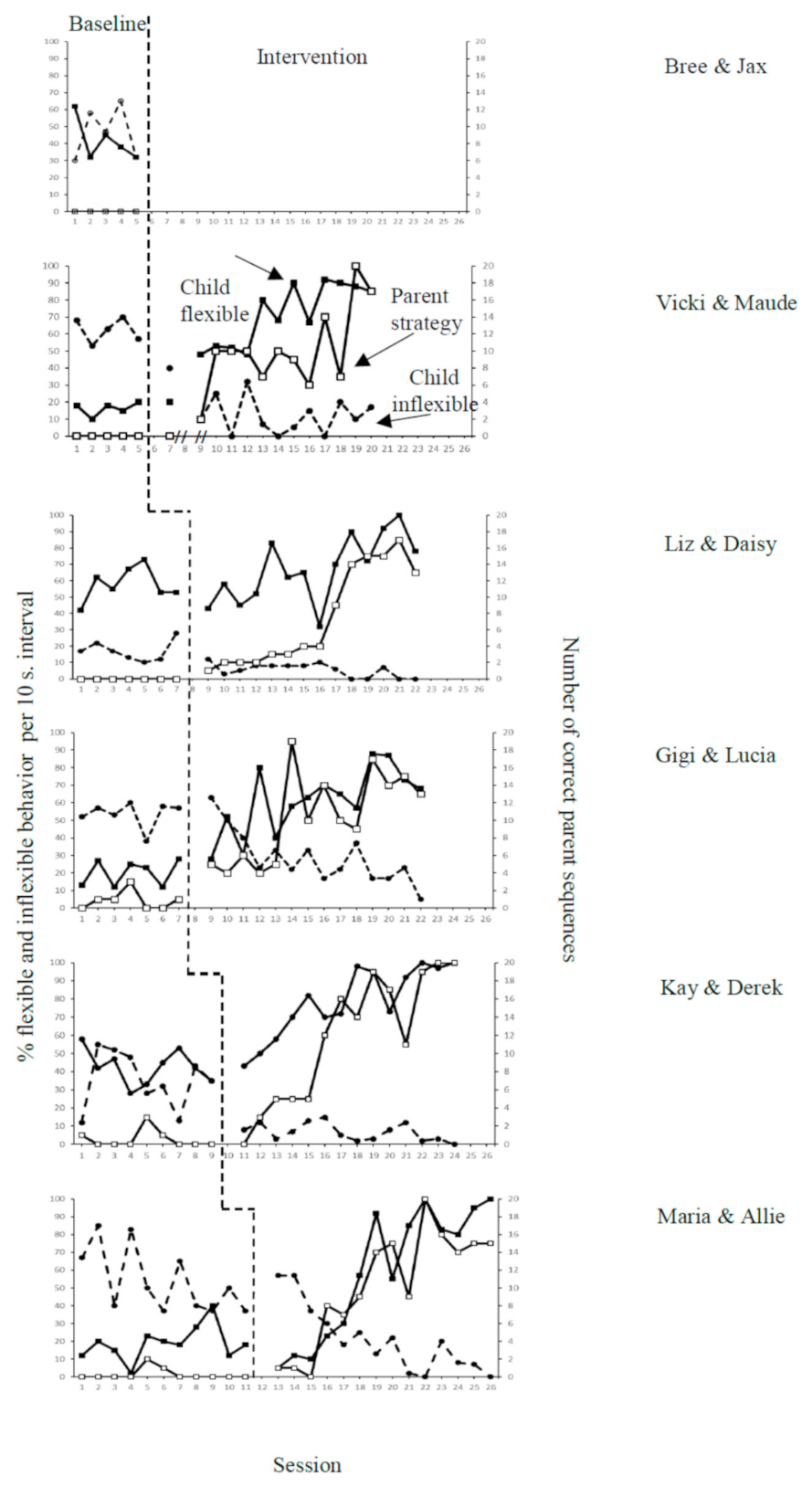
3.1. Descriptive Results
3.1.1. Dyad 1: Bree and Jax
3.1.2. Dyad 2: Vicki and Maude
3.1.3. Dyad 3: Liz and Daisy
3.1.4. Dyad 4: Gigi and Lucia
3.1.5. Dyad 5: Kay and Derek
3.1.6. Dyad 6: Maria and Allie
3.2. Standard Mean Difference (Between-Case Effect Size)
3.3. Non-Experimental Results
3.4. Social Validity
4. Discussion
4.1. Parent Strategy Use
4.2. Child Flexible and Inflexible Behavior
4.3. Parent Strategy Use as a Moderator for Child Flexibility
4.4. Parent-Reported Autism Symptomology and Diagnosis
4.5. Limitations
4.6. Implications for Research and Practice
4.7. Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5, 5th ed.; American Psychiatric Publishing: Washington, DC, USA, 2013. [Google Scholar]
- Maenner, M.J.; Saw, K.A.; Baio, J.; Washington, A.; Patrick, M.; DiRienzo, M.; Pettygrove, S.; Andrews, J.G.; Lopez, M.; Hudson, A.; et al. Prevalence of autism spectrum disorder among children aged 8 years. Autism Dev. Dis. Monit. Netw. 2020. [Google Scholar] [CrossRef]
- World Health Organization. Available online: https://www.who.int/news-room/fact-sheets/detail/autism-spectrum-disorders (accessed on 28 December 2020).
- Connolly, M.; Gersch, I. A support group for parents of children on a waiting list for an assessment for autism spectrum disorder. Educ. Psychol. Pr. 2013, 29, 293–308. [Google Scholar] [CrossRef]
- Denman, K.; Smart, C.; Dallos, R.; Levett, P. How Families Make Sense of Their Child’s Behaviour When on an Autism Assessment and Diagnosis Waiting List. J. Autism Dev. Disord. 2016, 46, 3408–3423. [Google Scholar] [CrossRef] [PubMed]
- Gibbs, V.; Aldridge, F.; Sburlati, E.; Chandler, F.; Smith, K.; Cheng, L. Missed opportunities: An investigation of pathways to autism diagnosis in Australia. Res. Autism Spectr. Disord. 2019, 57, 55–62. [Google Scholar] [CrossRef]
- Rivard, M.; Morin, M.; Mercier, C.; Terroux, A.; Mello, C.; Lépine, A. Social Validity of a Training and Coaching Program for Parents of Children with Autism Spectrum Disorder on a Waiting List for Early Behavioral Intervention. J. Child Fam. Stud. 2017, 26, 877–887. [Google Scholar] [CrossRef]
- Hine, J.F.; Herrington, C.G.; Rothman, A.M.; Mace, R.L.; Patterson, B.L.; Carlson, K.L.; Warren, Z.E. Embedding Autism Spectrum Disorder Diagnosis Within the Medical Home: Decreasing Wait Times Through Streamlined Assessment. J. Autism Dev. Disord. 2018, 48, 2846–2853. [Google Scholar] [CrossRef] [PubMed]
- Warren, Z.; McPheeters, M.L.; Sathe, N.; Foss-Feig, J.H.; Glasser, A.; Veenstra-Vander Weele, J. A Systematic Review of Early Intensive Intervention for Autism Spectrum Disorders. Pediatrics 2011, 127, e1303–e1311. [Google Scholar] [CrossRef]
- Luyster, R.; Luyster, R.J.; Gotham, K.; Guthrie, W. Autism Diagnostic Observation Schedule, Second Edition: Toddler Module, 2nd ed.; Western Psychological Services: Cary, NC, USA, 2012. [Google Scholar]
- Pierce, K.; Gazestani, V.H.; Bacon, E.; Barnes, C.C.; Cha, D.; Nalabolu, S.; Lopez, L.; Moore, A.; Pence-Stophaeros, S.; Courchesne, E. Evaluation of the Diagnostic Stability of the Early Autism Spectrum Disorder Phenotype in the General Population Starting at 12 Months. JAMA Pediatr. 2019, 173, 578–587. [Google Scholar] [CrossRef]
- Jo, H.; Schieve, L.A.; Rice, C.E.; Yeargin-Allsopp, M.; Tian, L.H.; Blumberg, S.J.; Kogan, M.D.; Boyle, C.A. Age at Autism Spectrum Disorder (ASD) Diagnosis by Race, Ethnicity, and Primary Household Language Among Children with Special Health Care Needs, United States, 2009–2010. Matern. Child Health J. 2015, 19, 1687–1697. [Google Scholar] [CrossRef]
- Martinez, M.; Thomas, K.C.; Williams, C.S.; Christian, R.; Crais, E.; Pretzel, R.; Hooper, S.R. Family Experiences with the Diagnosis of Autism Spectrum Disorder: System Barriers and Facilitators of Efficient Diagnosis. J. Autism Dev. Disord. 2018, 48, 2368–2378. [Google Scholar] [CrossRef]
- Christensen, D.L.; Bilder, D.A.; Zahorodny, W.; Pettygrove, S.; Durkin, M.S.; Fitzgerald, R.T.; Rice, C.; Kurzius-Spencer, M.; Baio, J.; Yeargin-Allsopp, M. Prevalence and characteristics of autism spectrum disorder among 4-year-old children in the au-tism and developmental disabilities monitoring network. J. Dev. Behav. 2016, 37, 1–8. [Google Scholar] [CrossRef]
- Daniels, A.M.; Halladay, A.K.; Shih, A.; Elder, L.M.; Dawson, G. Approaches to Enhancing the Early Detection of Autism Spectrum Disorders: A Systematic Review of the Literature. J. Am. Acad. Child Adolesc. Psychiatry 2014, 53, 141–152. [Google Scholar] [CrossRef]
- Esler, A.N.; Bal, V.H.; Guthrie, W.; Wetherby, A.; Weismer, S.E.; Lord, C. The Autism Diagnostic Observation Schedule, Toddler Module: Standardized Severity Scores. J. Autism Dev. Disord. 2015, 45, 2704–2720. [Google Scholar] [CrossRef]
- Fountain, C.; King, M.D.; Bearman, P.S. Age of diagnosis for autism: Individual and community factors across 10 birth co horts. J. Epidemiol. Comm. Health 2011, 65, 503–510. [Google Scholar] [CrossRef]
- Hertz-Picciotto, I.; Delwiche. L. The rise in autism and the role of age at diagnosis. Epidemiology 2009, 20, 84–90. [Google Scholar] [CrossRef]
- Boyd, B.A.; McDonough, S.G.; Bodfish, J.W. Evidence-Based Behavioral Interventions for Repetitive Behaviors in Autism. J. Autism Dev. Disord. 2012, 42, 1236–1248. [Google Scholar] [CrossRef]
- Lin, C.E.; Koegel, R. Treatment for Higher-Order Restricted Repetitive Behaviors (H-RRB) in Children with Autism Spectrum Disorder. J. Autism Dev. Disord. 2018, 48, 3831–3845. [Google Scholar] [CrossRef]
- U.S. Food and Drug Administration. The Voice of the Patient: A Series of Reports from the U.S. Food and Drug Administration’s Patient-Focused Drug Development Initiative-Autism (Document No. 2017-04229); Center for Drug Evaluation and Research; U.S. Food and Drug Administration: Washington, DC, USA, 2017.
- Dawson, G.; Rogers, S.; Munson, J.; Smith, M.; Winter, J.; Greenson, J.; Donaldson, A.; Varley, J. Randomized, Controlled Trial of an Intervention for Toddlers with Autism: The Early Start Denver Model. Pediatrics 2009, 125, e17–e23. [Google Scholar] [CrossRef]
- Kaiser, A.P.; Roberts, M.Y. Parent-Implemented Enhanced Milieu Teaching with Preschool Children Who Have Intellectual Disabilities. J. Speech Lang. Hear. Res. 2013, 56, 295–309. [Google Scholar] [CrossRef]
- Kasari, C.; Freeman, S.; Paparella, T. Joint attention and symbolic play in young children with autism: A randomized controlled intervention study. J. Child Psychol. Psychiatry 2005, 47, 611–620. [Google Scholar] [CrossRef]
- Weitzman, E. More Than Words—The Hanen Program for Parents of Children with Autism Spectrum Disorder: A Teaching Model for Parent-implemented Language Intervention. Perspect. Lang. Learn. Educ. 2013, 20, 96–111. [Google Scholar] [CrossRef]
- Steinbrenner, J.R.; Hume, K.; Odom, S.L.; Morin, K.L.; Nowell, S.W.; Tomaszewski, B.; Szendrey, S.; McIntyre, N.S.; Yücesoy-Özkan, S.; Savage, M.N. Evidence-Based Practices for Children, Youth, and Young Adults with Autism; The University of North Carolina at Chapel Hill; Frank Porter Graham Child Development Institute; National Clearinghouse on Autism Evidence and Practice Review Team: Chapel Hill, NC, USA, 2020. [Google Scholar]
- Rispoli, M.; Camargo, S.; Machalicek, W.; Lang, R.; Sigafoos, J. Functional communication training in the treatment of problem behavior maintained by access to rituals. J. Appl. Behav. Anal. 2014, 47, 580–593. [Google Scholar] [CrossRef] [PubMed]
- Lang, R.; Koegel, L.K.; Ashbaugh, K.; Regester, A.; Ence, W.; Smith, W. Physical exercise and individuals with autism spectrum disorders: A systematic review. Res. Autism Spectr. Disord. 2010, 4, 565–576. [Google Scholar] [CrossRef]
- Piazza, C.C.; Adelinis, J.D.; Hanley, G.P.; Goh, H.-L.; Delia, M.D. An evaluation of the effects of matched stimuli on behaviors maintained by automatic reinforcement. J. Appl. Behav. Anal. 2000, 33, 13–27. [Google Scholar] [CrossRef] [PubMed]
- Erturk, B.; Machalicek, W.; Drew, C. Self-Injurious Behavior in Children with Developmental Disabilities: A Systematic Review of Behavioral Intervention Literature. Behav. Modif. 2017, 42, 498–542. [Google Scholar] [CrossRef]
- Durand, V.M.; Carr, E.G. Functional communication training to reduce challenging behavior: Maintenance and application in a new setting. J. Appl. Behav. Anal. 1991, 24, 251–264. [Google Scholar] [CrossRef] [PubMed]
- Tucker, M.; Sigafoos, J.; Bushell, H. Use of noncontingent reinforcement in the treatment of challenging behavior: A review and clinical guide. Behav. Modif. 1998, 22, 498–542. [Google Scholar] [CrossRef] [PubMed]
- Sidener, T.M.; Carr, J.A.E.; Firth, A.M. Superimposition and withholding of edible consequences as treatment for automatically reinforced stereotypy. J. Appl. Behav. Anal. 2005, 38, 121–124. [Google Scholar] [CrossRef]
- Raulston, T.J.; Hansen, S.G.; Machalicek, W.; McIntyre, L.L.; Carnett, A. Interventions for Repetitive Behavior in Young Children with Autism: A Survey of Behavioral Practices. J. Autism Dev. Disord. 2019, 49, 3047–3059. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, K.N.; Ledford, J.R.; Barton, E.E. Using Visual Activity Schedules for Young Children with Challenging Behavior. J. Early Interv. 2017, 39, 339–358. [Google Scholar] [CrossRef]
- Dupere, S.; Macdonald, R.P.F.; Ahearn, W.H. Using video modeling with substitutable loops to teach varied play to children with autism. J. Appl. Behav. Anal. 2013, 46, 662–668. [Google Scholar] [CrossRef]
- Harrop, C.; Gulsrud, A.; Shih, W.; Hovsepyan, L.; Kasari, C. Characterizing caregiver responses to restricted and repetitive behaviors in toddlers with autism spectrum disorder. Autism 2015, 20, 330–342. [Google Scholar] [CrossRef]
- Fisher, W.A.; Groff, R.A.; Roane, H.S. History, philosophy, principles, and basic methods. In Handbook of Applied Behavior Analysis; Fisher, W.W., Piazza, C.C., Roane, H.S., Eds.; The Guilford Press: New York, NY, USA, 2011; pp. 3–13. [Google Scholar]
- Sam, A.; AFIRM Team. Modeling; National Professional Development Center on Autism Spectrum Dis-order, FPG Child Development Center, University of North Carolina: Chapel Hill, NC, USA, 2016; Available online: http://afirm.fpg.unc.edu/modeling (accessed on 1 May 2020).
- Dieringer, S.T.; Zoder-Martell, K.; Porretta, D.L.; Bricker, A.; Kabazie, J. Increasing physical activity in children with autism through music, prompting, and modeling. Psychol. Sch. 2017, 54, 421–432. [Google Scholar] [CrossRef]
- Hanley, G.P.; Tiger, J.H. Differential reinforcement procedures. In Handbook of Applied Behavior Analysis; Fisher, W.W., Piazza, C.C., Roane, H.S., Eds.; The Guilford Press: New York, NY, USA, 2011; pp. 229–249. [Google Scholar]
- Savage, M.N.; AFIRM Team. Differential Reinforcement; National Professional Development Center on Autism Spectrum Dis-order, FPG Child Development Center, University of North Carolina: Chapel Hill, NC, USA, 2017; Available online: http://afirm.fpg.unc.edu/differential-reinforcement (accessed on 1 May 2020).
- Stahmer, A.C.; Ingersoll, B.; Carter, C. Behavioral Approaches to Promoting Play. Autism 2003, 7, 401–413. [Google Scholar] [CrossRef]
- Tomaszewski, B.; Regan, T.; AFIRM Team. Response Interruption and Redirection; National Professional Development Center on Autism Spectrum Disorder, FPG Child Development Center, University of North Carolina: Chapel Hill, NC, USA, 2017; Available online: http://afirm.fpg.unc.edu/response-interruption-and-redirection (accessed on 1 May 2020).
- Martinez, C.K.; Betz, A.M. Response interruption and redirection: Current research trends and clinical application. J. Appl. Behav. Anal. 2013, 46, 549–554. [Google Scholar] [CrossRef] [PubMed]
- McSwain, S.D.; Bernard, J.; Burke, B.L.; Cole, S.L.; Dharmar, M.; Hall-Barrow, J.; Herendeen, N.; Herendeen, P.; Krupinski, E.A.; Martin, A.; et al. American Telemedicine Association Operating Procedures for Pediatric Telehealth. Telemed. eHealth 2017, 23, 699–706. [Google Scholar] [CrossRef]
- Rispoli, M.; Machalicek, W. Advances in Telehealth and Behavioral Assessment and Intervention in Education: Introduction to the Special Issue. J. Behav. Educ. 2020, 29, 189–194. [Google Scholar] [CrossRef]
- Simacek, J.; Dimian, A.F.; McComas, J.J. Communication Intervention for Young Children with Severe Neurodevelopmental Disabilities Via Telehealth. J. Autism Dev. Disord. 2017, 47, 744–767. [Google Scholar] [CrossRef]
- Machalicek, W.; Lequia, J.; Pinkelman, S.; Knowles, C.; Raulston, T.; Davis, T.; Alresheed, F. Behavioral Telehealth Consultation with Families of Children with Autism Spectrum Disorder. Behav. Interv. 2016, 31, 223–250. [Google Scholar] [CrossRef]
- Rooks-Ellis, D.; Howorth, S.K.; Kunze, M.; Boulette, S.; Sulinski, E. Effects of a parent training using telehealth: Equity and access to early intervention for rural families. J. Child. Educ. Soc. 2020, 1, 141–166. [Google Scholar] [CrossRef]
- Unholz-Bowden, E.; McComas, J.J.; McMaster, K.L.; Girtler, S.N.; Kolb, R.L.; Shipchandler, A. Caregiver Training Via Telehealth on Behavioral Procedures: A Systematic Review. J. Behav. Educ. 2020, 29, 246–281. [Google Scholar] [CrossRef]
- Rodriguez, K.A. Maintaining Treatment Integrity in the Face of Crisis: A Treatment Selection Model for Transitioning Direct ABA Services to Telehealth. Behav. Anal. Pr. 2020, 13, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Vismara, L.A.; Young, G.S.; Rogers, S.J. Telehealth for Expanding the Reach of Early Autism Training to Parents. Autism Res. Treat. 2012, 2012, 121878. [Google Scholar] [CrossRef]
- McDuffie, A.; Oakes, A.; Machalicek, W.; Ma, M.; Bullar, L.; Nelson, S.; Abbeduto, L. Early language intervention using vid-eo-teleconferencing: A pilot study of young boys with Fragile-X syndrome and their mothers. Am. J. Speech Lang Pathol. 2016, 25, 46–66. [Google Scholar] [CrossRef]
- Boisvert, M.; Lang, R.; Andrianopoulos, M.; Boscardin, M.L. Telepractice in the assessment and treatment of individuals with autism spectrum disorders: A systematic review. Dev. Neurorehabilit. 2010, 13, 423–432. [Google Scholar] [CrossRef]
- Wacker, D.P.; Lee, J.F.; Dalmau, Y.C.P.; Kopelman, T.G.; Lindgren, S.D.; Kuhle, J.; Pelzel, K.E.; Dyson, S.; Schieltz, K.M.; Waldron, D.B. Conducting Functional Communication Training via Telehealth to Reduce the Problem Behavior of Young Children with Autism. J. Dev. Phys. Disabil. 2013, 25, 35–48. [Google Scholar] [CrossRef]
- Jang, J.; Dixon, D.; Tarbox, J.; Granpeesheh, D.; Kornack, J.; de Nocker, Y. Randomized controlled trial of an eLearning program for training family members of children with autism in the principles and procedures of applied behavior analysis. Res. Autism Spectr. Disord. 2012, 6, 852–856. [Google Scholar] [CrossRef]
- Fettig, A.; Ostrosky, M.M. Collaborating with parents in reducing children’s challenging behaviors: Linking functional assess-ment to intervention. Child Dev. Res. 2011, 2011, 835941. [Google Scholar] [CrossRef]
- Fettig, A.; Schultz, T.R.; Sreckovic, M.A. Effects of Coaching on the Implementation of Functional Assessment–Based Parent Intervention in Reducing Challenging Behaviors. J. Posit. Behav. Interv. 2015, 17, 170–180. [Google Scholar] [CrossRef]
- Ingersoll, B.; Wainer, A.L.; Berger, N.I.; Pickard, K.E. Comparison of self-directed and therapist-assisted telehealth par-ent-mediated intervention for children with ASD: A pilot RCT. J. Autism Dev. Dis. 2016, 46, 2284–2775. [Google Scholar] [CrossRef]
- Wolff, J.J.; Boyd, B.A.; Elison, J.T. A quantitative measure of restricted and repetitive behaviors for early childhood. J. Neurodev. Disord. 2016, 8, 27. [Google Scholar] [CrossRef]
- U.S. Census Bureau. Urban and Rural Classifications. 2019. Available online: https://www.census.gov/programs-surveys/geography/guidance/geo-areas/urban-rural.html (accessed on 1 May 2020).
- Shire, S.Y.; Shih, W.; Chang, Y.-C.; Kasari, C. Short Play and Communication Evaluation: Teachers’ assessment of core social communication and play skills with young children with autism. Autism 2018, 22, 299–310. [Google Scholar] [CrossRef] [PubMed]
- Robins, D.; Fein, D.; Barton, M. Modified Checklist for Autism in Toddlers, Revised with Follow-Up (M-CHAT-R/F). 2009. Available online: https://www.m-chat.org/about.php (accessed on 1 May 2020).
- Rush, D.D.; Sheldan, M.L. The Early Childhood Coaching Handbook; Paul, H., Ed.; Brooks Publishing Co: Baltimore, MD, USA, 2011. [Google Scholar]
- Frey, J.R.; Kaiser, A.P. The Use of Play Expansions to Increase the Diversity and Complexity of Object Play in Young Children with Disabilities. Top. Early Child. Spéc. Educ. 2011, 31, 99–111. [Google Scholar] [CrossRef]
- Quigley, J.; Griffith, A.K.; Kates-McElrath, K. A Comparison of Modeling, Prompting, and a Multi-component Intervention for Teaching Play Skills to Children with Developmental Disabilities. Behav. Anal. Pr. 2018, 11, 315–326. [Google Scholar] [CrossRef]
- Sam, A.; AFIRM Team. Prompting; National Professional Development Center on Autism Spectrum Disorder, FPG Child Development Center, University of North Carolina: Chapel Hill, NC, USA, 2015; Available online: http://afirm.fpg.unc.edu/prompting (accessed on 1 May 2020).
- Francis, R.; Winchester, C.; Barton, E.E.; Ledford, J.R.; Velez, M. Using Progressive Time Delay to Increase Levels of Peer Imitation During Play with Preschoolers with Disabilities. Am. J. Intellect. Dev. Disabil. 2020, 125, 186–199. [Google Scholar] [CrossRef]
- Gast, D.L.; Lloyd, B.P.; Ledford, J.R. Multiple baseline and multiple probe designs. In Single Case Research Methodology: Applications in Special Education and Behavioral Sciences; Gast, D.L., Ledford, J.R., Eds.; Routledge: New York, NY, USA, 2014; pp. 252–296. [Google Scholar]
- Pustejovsky, J.E.; Swan, D.M. Single-Case Effect Size Calculator (Version 0.5) Web Application. 2018. Available online: https://jepusto.shinyapps.io/SCD-effect-sizes/ (accessed on 5 May 2020).
- Pustejovsky, J.E. Scdhlm: A Web-Based Calculator for between-Case Standardized Mean Differences (Version 0.3.1) Web Application. 2016. Available online: https://jepusto.shinyapps.io/scdhlm (accessed on 5 May 2020).
- Reimers, T.M.; Wacker, D.P. Acceptability of behavioral treatments for children: Analog and naturalistic evaluations by par-ents. School Psychol. Rev. 1992, 21, 628–643. [Google Scholar]
- Ulke-Kurkcuoglu, B. A comparison of least-to-most prompting and video modeling for teaching pretend play skills to children with autism spectrum disorder. Educ. Sci. Theory Pract. 2015, 15, 499–517. [Google Scholar]
- Nijhof, S.L.; Vinkers, C.H.; van Geelen, S.M.; Duijff, S.N.; Achterberg, E.M.; van der Net, J.; Veltkamp, R.C.; Grootenhuis, M.A.; van de Putte, E.M.; Hillegers, M.H.; et al. Healthy play, better coping: The importance of play for the development of children in health and disease. Neurosci. Biobehav. Rev. 2018, 95, 421–429. [Google Scholar] [CrossRef]
- Eisenhower, A.S.; Baker, B.L.; Blacher, J. Children’s delayed development and behavior problems: Impact on mothers’ perceived physical health across early childhood. Soc. Sci. Med. 2009, 68, 89–99. [Google Scholar] [CrossRef]
- Harrop, C.; McConachie, H.; Emsley, R.; Leadbitter, K.; Green, J. Restricted and repetitive behaviors in autism spectrum dis-orders and typical development: Cross-sectional and longitudinal comparisons. J. Autism Dev. Dis. 2014, 44, 1207–1219. [Google Scholar] [CrossRef]
- Hanley, G.P.; Tiger, J.H.; Ingvarsson, E.T.; Cammilleri, A.P. Influencing preschoolers’ free-play activity preferences: An evaluation of satiation and embedded reinforcement. J. Appl. Behav. Anal. 2009, 42, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Silbaugh, B.C.; Murray, C.; Kelly, M.P.; Healy, O. A Systematic Synthesis of Lag Schedule Research in Individuals with Autism and Other Populations. Rev. J. Autism Dev. Disord. 2021, 8, 92–107. [Google Scholar] [CrossRef]
- Galizio, A.; Higbee, T.S.; Odum, A.L. Choice for reinforced behavioral variability in children with autism spectrum disorder. J. Exp. Anal. Behav. 2020, 113, 495–514. [Google Scholar] [CrossRef] [PubMed]
- Radley, K.C.; Dart, E.H.; Helbig, K.A.; Schrieber, S.R. An Additive Analysis of Lag Schedules of Reinforcement and Rules on Novel Responses of Individuals with Autism Spectrum Disorder. J. Dev. Phys. Disabil. 2018, 32, 395–408. [Google Scholar] [CrossRef]
- Eyberg, S.M.; Boggs, S.R.; Algina, J. Parent-child interaction therapy: A psychosocial model for the treatment of young children with conduct problem behavior and their families. Psychopharmacol. Bull. 1995, 31, 83–91. [Google Scholar]
- Solomon, M.; Ono, M.; Timmer, S.; Goodlin-Jones, B. The effectiveness of parent-child interaction therapy for families of children on the autism spectrum. J. Autism Dev. Disord. 2008, 38, 1767–1776. [Google Scholar] [CrossRef]
- Guthrie, W.; Wallis, K.; Bennett, A.; Brooks, E.; Dudley, J.; Gerdes, M.; Pandey, J.; Levy, S.E.; Schultz, R.T.; Miller, J.S. Accuracy of Autism Screening in a Large Pediatric Network. Pediatrics 2019, 144, e20183963. [Google Scholar] [CrossRef]
- Dahiya, A.V.; McDonnell, C.; DeLucia, E.; Scarpa, A. A systematic review of remote telehealth assessments for early signs of autism spectrum disorder: Video and mobile applications. Pr. Innov. 2020, 5, 150–164. [Google Scholar] [CrossRef]
- Hyman, S.L.; Levy, S.E.; Myers, S.M. AAP Council on Children with Disabilities Section on Developmental and Behavioral Pediatrics. Identification, evaluation, and management of children with autism spectrum disorder. Pediatrics 2020, 145, e20193447. [Google Scholar] [CrossRef]
- Thabtah, F. An accessible and efficient autism screening method for behavioural data and predictive analyses. Health Inform. J. 2018, 25, 1739–1755. [Google Scholar] [CrossRef]
- Barbaro, J.; Yaari, M. Study protocol for an evaluation of ASDetect—A Mobile application for the early detection of autism. BMC Pediatrics 2020, 20, 21. [Google Scholar] [CrossRef]
- Smith, C.J.; Rozga, A.; Matthews, N.; Oberleitner, R.; Nazneen, N.; Abowd, G. Investigating the accuracy of a novel telehealth diagnostic approach for autism spectrum disorder. Psychol. Assess. 2017, 29, 245–252. [Google Scholar] [CrossRef]
- Barbaro, J.; Dissanayake, C. Prospective Identification of Autism Spectrum Disorders in Infancy and Toddlerhood Using Developmental Surveillance: The Social Attention and Communication Study. J. Dev. Behav. Pediatr. 2010, 31, 376–385. [Google Scholar] [CrossRef]
- Wetherby, A.M.; Guthrie, W.; Woods, J.; Schatschneider, C.; Holland, R.D.; Morgan, L.; Lord, C. Parent-Implemented Social Intervention for Toddlers with Autism: An RCT. Pediatrics 2014, 134, 1084–1093. [Google Scholar] [CrossRef]
- Harrop, C. Evidence-based, parent-mediated interventions for young children with autism spectrum disorder: The case of restricted and repetitive behaviors. Autism 2015, 19, 662–672. [Google Scholar] [CrossRef]
- Zwaigenbaum, L.; Bauman, M.L.; Choueiri, R.; Kasari, C.; Carter, A.S.; Granpeesheh, D.; Mailloux, Z.; Roley, S.S.; Wagner, S.; Fein, D.; et al. Early Intervention for Children with Autism Spectrum Disorder Under 3 Years of Age: Recommendations for Practice and Research. Pediatrics 2015, 136 (Suppl. S1), S60–S81. [Google Scholar] [CrossRef]
- Sam, A.M.; Cox, A.W.; Savage, M.N.; Waters, V.; Odom, S.L. Disseminating Information on Evidence-Based Practices for Children and Youth with Autism Spectrum Disorder: AFIRM. J. Autism Dev. Disord. 2019, 50, 1931–1940. [Google Scholar] [CrossRef]
- Myerson, J.; Hale, S. Practical implications of the matching law. J. Appl. Behav. Anal. 1984, 17, 367–380. [Google Scholar] [CrossRef]
- Leonard, H.; Dixon, G.; Whitehouse, A.J.; Bourke, J.; Alberti, K.; Nassar, N.; Bower, C.G.; Lasson, E.J. Unpacking the complex nature of the autism epidemic. Res. Autism Spectr. Disord. 2010, 4, 548–554. [Google Scholar] [CrossRef]
- Bishop, S.L.; Richler, J.; Cani, A.C.; Lord, C.; Floyd, F. Predictors of perceived negative impact in mothers of children with autism spectrum disorder. Am. J. Ment. Retard. 2007, 112, 450–461. [Google Scholar] [CrossRef]
| Child Name (Dyad #) | Age in Months | Sex | Race | Alternative Diagnosis | Focus Behaviors |
|---|---|---|---|---|---|
| Jax (dyad 1) | 21 | M | White | Developmental Delay | 1, 2, 3, 4, 5 |
| Maude (dyad 2) | 33 | F | White | Developmental Delay | 4, 5, 7 |
| Daisy (dyad 3) | 30 | F | White | Hydrocephalus Epilepsy Hearing Impairment Developmental Delay Motor Impairment (Clubfoot) | 2, 5, 8 |
| Lucia (dyad 4) | 35 | F | Hispanic/Latinx | Developmental Delay | 1, 6 |
| Derek (dyad 5) | 35 | M | Indigenous North America/Alaskan Native | None | 1, 2, 3, 4, 5 |
| Allie (dyad 6) | 31 | F | Hispanic/Latinx | Developmental Delay | 1, 3, 4, 5, 9 |
| Parent Name (Dyad #) | Age in Years | Race | Marital Status | Qualifying Category |
|---|---|---|---|---|
| Bree (dyad 1) | 25 | White | Single | UR, US |
| Vicki (dyad 2) | 30 | White | Single | US |
| Liz (dyad 3) | 25 | White | Single | R, UR, US |
| Gigi (dyad 4) | 43 | Hispanic/Latinx | Married | US |
| Kay (dyad 5) | 42 | Indigenous North America/Alaskan Native | Married | UR, US |
| Maria (dyad 6) | 42 | Hispanic/Latinx | Married | US |
| Intervention Component | Component Description |
|---|---|
| Check-in & Rapport Building | Discuss how the parent and child are doing, specifics of the intervention, and areas of focus. Further descriptions of intervention strategies were discussed based on individual needs of the dyad. |
| Dyad Interaction(no coaching) | Parent and child interact with one another in play using areas of focus discussed during check-in. The researcher did not coach or correct here. Data collection occurred here. |
| Parent Coaching | The parent and researcher discuss the child’s behavior and parent responses. The researcher asked parent to practice some strategies with feedback. The researcher presented new information and reviewed past discussions as necessary. Parents were encouraged to practice strategies between meetings as necessary to reach fidelity. |
| Feedback | The researcher provided the parent with feedback on specific strengths and focus areas for additional practice between intervention sessions. The parent was provided with video recording of the intervention session to watch asynchronously for further learning opportunities. |
| Plan and Closing | The researcher and parent discussed the practice plan and goals for the upcoming week, confirming time and day for the next session. |
| Component | Description |
|---|---|
| Joint Planning | Agreement on what actions to take during a session Understanding what caregiver will practice between visits Discussion of interactions between coach and caregiver and caregiver and child |
| Observation | Coach’s observation of caregiver, child, and self Caregiver’s observation of coach, child, and self |
| Practice | Practice skills and adjust strategy use Give feedback about practice Model, discuss, or prompt through intervention strategies |
| Reflection | Reflect and analyze actions and observations Reflect on skills needed for use in the next intervention |
| Feedback | Discuss strategies and implementation with improvements Refine skill expectations and goals |
| Child Behavior M (Range) | Parent Strategy Use M (Range) | Parent Treatment Fidelity | Intervention Procedural Fidelity | |||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Intervention | Overall | Baseline | Intervention | Overall | M (Range) | M (Range) | |
| Dyad 2 | 87% (83–90%) | 95% (80–100%) | 92% | 98% (95–100%) | 85% (65–95%) | 89% | 99% (98–100%) | 91% (82–100%) |
| Dyad 3 | 91% (89–92%) | 88% (81–100%) | 89% | 98% (95–100%) | 98% (95–100%) | 98% | 95% (88–100%) | 95% (91–100%) |
| Dyad 4 | 90% (86–94%) | 95% (84–100%) | 94% | 98% (95–100%) | 88% (70–100%) | 91% | 93% (87–97%) | 98% (91–100%) |
| Dyad 5 | 90% (85–100%) | 87% (78–100%) | 88% | 97% (90–100%) | 90% (75–100%) | 93% | 99% (96–100%) | 98% (91–100%) |
| Dyad 6 | 88% (79–100%) | 94% (82–100%) | 92% | 97% (90–100%) | 86% (75–95%) | 89% | 98% (95–100%) | 96% (91–100%) |
| Parent | |||||
|---|---|---|---|---|---|
| Descriptions | Vicki | Liz | Gigi | Kay | Maria |
| Strategy Sequence Use | |||||
| Model 1 sequence | 81 | 89 | 113 | 155 | 46 |
| Model 2 sequence | 7 | 8 | 7 | 3 | 7 |
| Prompt sequence | 27 | 9 | 8 | 6 | 29 |
| RIRD sequence | 0 | 0 | 1 | 0 | 0 |
| Missed Sequence Step | |||||
| DRA | 10 | 29 | 12 | 11 | 9 |
| Model in Model 2 sequence | 0 | 2 | 4 | 0 | 2 |
| Prompt in Prompt sequence | 3 | 1 | 2 | 0 | 2 |
| Participant | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Non-Experimental Measure | Bree/Jax Dyad 1 | Vicki/Maude Dyad 2 | Liz/Daisy Dyad 3 | Gigi/Lucia Dyad 4 | Kay/Derek Dyad 5 | Maria/Allie Dyad 6 | ||||||
| Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | |
| Assessments | ||||||||||||
| RBS-EC | 2.6 | --- | 1.9 | 0.6 | 2.2 | 2.2 | 0.4 | 0.4 | 1.9 | 1.6 | 1.5 | 2.2 |
| Scale I | 2.6 | --- | 2.8 | 1.1 | 2.6 | 2.0 | 0.4 | 0.7 | 1.6 | 1.7 | 3.0 | 2.8 |
| Scale II | 2.7 | --- | 0.3 | 0.1 | 2.0 | 1.8 | 0.9 | 0.8 | 2.9 | 2.2 | 1.0 | 2.0 |
| Scale III | 2.9 | --- | 3.3 | 0.9 | 2.9 | 2.3 | 0.1 | 0.0 | 2.1 | 2.0 | 2.0 | 3.9 |
| Scale IV | 2.1 | --- | 1.3 | 0.1 | 1.6 | 2.3 | 0.0 | 0.0 | 0.6 | 0.3 | 0.0 | 0.0 |
| M-CHAT- R/F | 4 | --- | 11 | 6 | 7 | 12 | 7 | 6 | 12 | 8 | 6 | 5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kunze, M.G.; Machalicek, W.; Wei, Q.; St. Joseph, S. Coaching via Telehealth: Caregiver-Mediated Interventions for Young Children on the Waitlist for an Autism Diagnosis Using Single-Case Design. J. Clin. Med. 2021, 10, 1654. https://doi.org/10.3390/jcm10081654
Kunze MG, Machalicek W, Wei Q, St. Joseph S. Coaching via Telehealth: Caregiver-Mediated Interventions for Young Children on the Waitlist for an Autism Diagnosis Using Single-Case Design. Journal of Clinical Medicine. 2021; 10(8):1654. https://doi.org/10.3390/jcm10081654
Chicago/Turabian StyleKunze, Megan G., Wendy Machalicek, Qi Wei, and Stephanie St. Joseph. 2021. "Coaching via Telehealth: Caregiver-Mediated Interventions for Young Children on the Waitlist for an Autism Diagnosis Using Single-Case Design" Journal of Clinical Medicine 10, no. 8: 1654. https://doi.org/10.3390/jcm10081654
APA StyleKunze, M. G., Machalicek, W., Wei, Q., & St. Joseph, S. (2021). Coaching via Telehealth: Caregiver-Mediated Interventions for Young Children on the Waitlist for an Autism Diagnosis Using Single-Case Design. Journal of Clinical Medicine, 10(8), 1654. https://doi.org/10.3390/jcm10081654






