Long-Term Follow-Up of Inpatients with Failed Back Surgery Syndrome Who Received Integrative Korean Medicine Treatment: A Retrospective Analysis and Questionnaire Survey Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.1.1. Inclusion Criteria
2.1.2. Exclusion Criteria
2.2. Analysis of Medical Records
General Information
- Date and mode of onset (onset dates of current and initial symptoms, as well as reasons for symptom onset).
- Intervention(s) received between onset and admission (analgesic, steroid, etc.).
- Current disease history and information regarding spinal surgery (diagnosis of spinal disorder, spinal surgery, name of surgical procedure, and surgical site).
- Comorbidities (hypertension, diabetes, heart disease, liver disease, and other comorbidities).
- Social history (smoking, drinking, and occupation).
- Radiological findings (L-spine T2-weighted MRI or CT scans).
2.3. Treatment
2.4. Follow-Up Questionnaire Survey
2.5. Outcomes
2.5.1. Primary Outcome
- Numeric Rating Scale (NRS) [16]
2.5.2. Secondary Outcomes
- Oswestry Disability Index (ODI) [17]
- 5-Level EuroQol 5-Dimension (EQ-5D-5L) [19]
2.6. Statement of Ethics
2.7. Statistical Analysis
3. Results
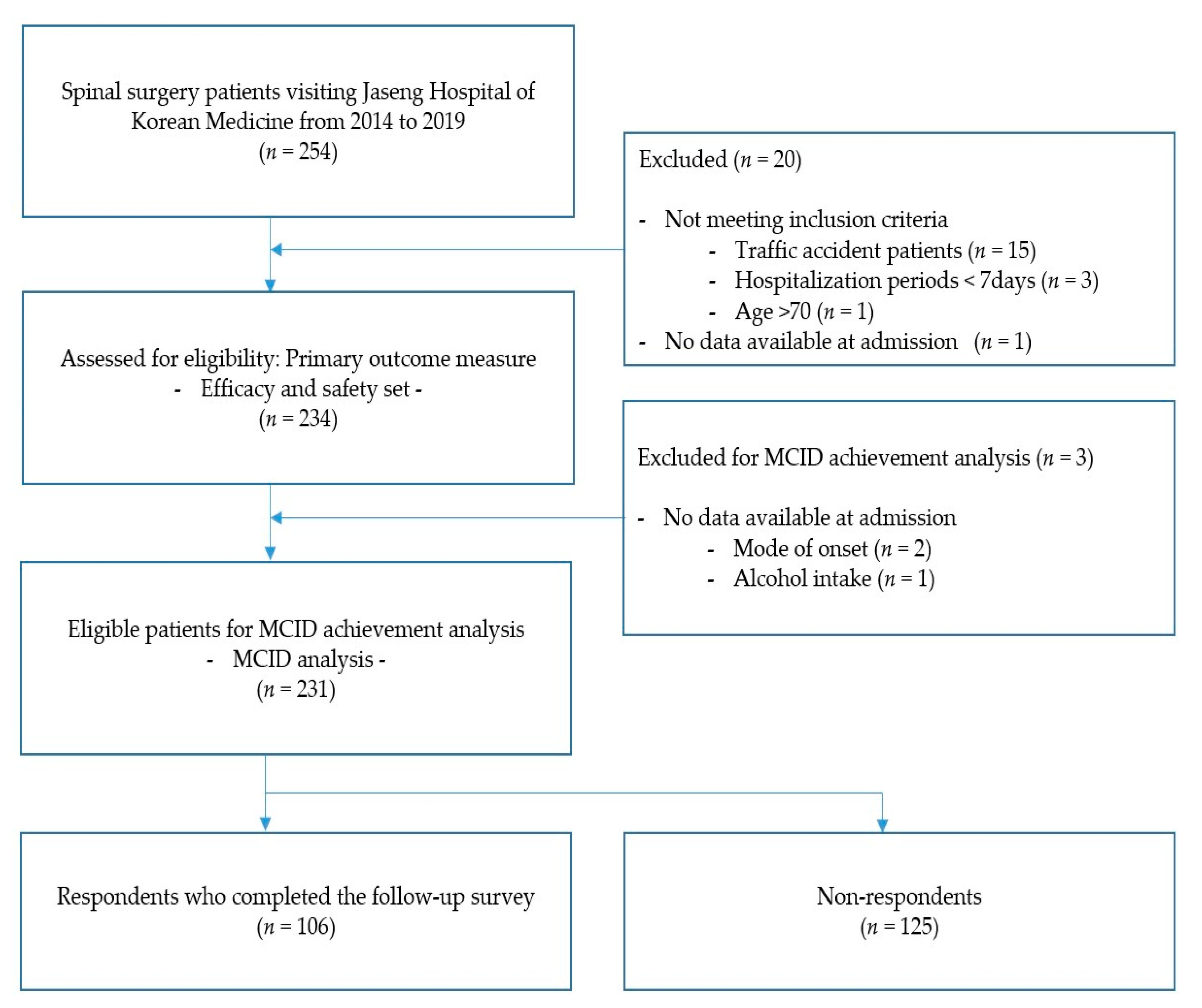
3.1. Study Flow
3.2. Baseline Characteristics
3.3. Post-Treatment Changes in the Values
3.4. MCID Analysis
3.5. Treatments
3.6. Follow-Up Survey
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rubin, D.I. Epidemiology and Risk Factors for Spine Pain. Neurol. Clin. 2007, 25, 353–371. [Google Scholar] [CrossRef]
- Daniell, J.R.; Osti, O.L. Failed Back Surgery Syndrome: A Review Article. Asian Spine J. 2018, 12, 372–379. [Google Scholar] [CrossRef] [PubMed]
- Baber, Z.; Erdek, M.A. Failed back surgery syndrome: Current perspectives. J. Pain Res. 2016, 9, 979–987. [Google Scholar] [CrossRef] [Green Version]
- Sivasubramaniam, V.; Patel, H.C.; Ozdemir, B.A.; Papadopoulos, M.C. Trends in hospital admissions and surgical procedures for degenerative lumbar spine disease in England: A 15-year time-series study. BMJ Open 2015, 5, e009011. [Google Scholar] [CrossRef] [Green Version]
- Chan, C.-W.; Peng, P. Failed Back Surgery Syndrome. Pain Med. 2011, 12, 577–606. [Google Scholar] [CrossRef] [Green Version]
- Follett, K.A.; Dirks, B.A. Etiology and evaluation of the failed back surgery syndrome. Neurosurg. Q. 1993, 3, 40. [Google Scholar]
- Merskey, H.E. Classification of Chronic Pain: Descriptions of Chronic Pain Syndromés and Definitions of Pain Terms. Pain 1986, 3, 226. [Google Scholar]
- Thomson, S.; Jacques, L. Demographic Characteristics of Patients with Severe Neuropathic Pain Secondary to Failed Back Surgery Syndrome. Pain Pract. 2009, 9, 206–215. [Google Scholar] [CrossRef] [PubMed]
- Sandroni, P.; Benrud-Larson, L.M.; McClelland, R.L.; Low, P.A. Complex regional pain syndrome type I: Incidence and prevalence in Olmsted county, a population-based study. Pain 2003, 103, 199–207. [Google Scholar] [CrossRef]
- Woolf, A.D.; Pfleger, B. Burden of major musculoskeletal conditions. Bull. World Health Organ. 2003, 81, 646–656. [Google Scholar]
- Thomson, S. Failed back surgery syndrome—Definition, epidemiology and demographics. Br. J. Pain 2013, 7, 56–59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ohnmeiss, D.D.; Rashbaum, R.F. Patient satisfaction with spinal cord stimulation for predominant complaints of chronic, intractable low back pain. Spine J. 2003, 1, 358–363. [Google Scholar] [CrossRef]
- Choi, H.S.; Chi, E.H.; Kim, M.-R.; Jung, J.; Lee, J.; Shin, J.-S.; Ha, I.-H. Demographic Characteristics and Medical Service Use of Failed Back Surgery Syndrome Patients at an Integrated Treatment Hospital Focusing on Complementary and Alternative Medicine: A Retrospective Review of Electronic Medical Records. Evid. Based Complement. Altern. Med. 2014, 2014, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Shin, J.-S.; Lee, Y.J.; Kim, M.-R.; Choi, A.; Lee, J.-H.; Shin, K.-M.; Shin, B.-C.; Cho, J.-H.; Ha, I.-H. Long-Term Course of Failed Back Surgery Syndrome (FBSS) Patients Receiving Integrative Korean Medicine Treatment: A 1 Year Prospective Observational Multicenter Study. PLoS ONE 2017, 12, e0170972. [Google Scholar] [CrossRef] [Green Version]
- Stevens, L.; Duarte, H.; Park, J. Promising Implications for Integrative Medicine for Back Pain: A Profile of a Korean Hospital. J. Altern. Complement. Med. 2007, 13, 481–484. [Google Scholar] [CrossRef] [PubMed]
- Childs, J.D.; Piva, S.R.; Fritz, J.M. Responsiveness of the Numeric Pain Rating Scale in Patients with Low Back Pain. Spine 2005, 30, 1331–1334. [Google Scholar] [CrossRef] [PubMed]
- Fairbank, J.C.T.; Pynsent, P.B. The Oswestry Disability Index. Spine 2000, 25, 2940–2953. [Google Scholar] [CrossRef] [PubMed]
- Jeon, C.-H.; Kim, D.-J.; Kim, S.-K.; Lee, H.-M.; Park, H.-J.; Kim, N.-J. Validation in the Cross-Cultural Adaptation of the Korean Version of the Oswestry Disability Index. J. Korean Med. Sci. 2006, 21, 1092–1097. [Google Scholar] [CrossRef]
- Herdman, M.; Gudex, C.; Lloyd, A.; Janssen, M.; Kind, P.; Parkin, D.; Bonsel, G.; Badia, X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.-H.; Ahn, J.; Ock, M.; Shin, S.; Park, J.; Luo, N.; Jo, M.-W. The EQ-5D-5L valuation study in Korea. Qual. Life Res. 2016, 25, 1845–1852. [Google Scholar] [CrossRef]
- Lee, S. Validity and reliability evaluation for eq-5d in korea. Cheongju Korea Cent. Dis. Control Prev. 2011, 40, 59. [Google Scholar]
- Park, K.B.; Shin, J.-S.; Lee, J.; Lee, Y.J.; Kim, M.-R.; Lee, J.-H.; Shin, K.-M.; Shin, B.-C.; Cho, J.-H.; Ha, I.-H. Minimum Clinically Important Difference and Substantial Clinical Benefit in Pain, Functional, and Quality of Life Scales in Failed Back Surgery Syndrome Patients. Spine 2017, 42, E474–E481. [Google Scholar] [CrossRef] [PubMed]
- Scalone, L.; Zucco, F.; Lavano, A.; Costantini, A.; De Rose, M.; Poli, P.; Fortini, G.; DeMartini, L.; De Simone, E.; Menardo, V.; et al. Benefits in pain perception, ability function and health-related quality of life in patients with failed back surgery syndrome undergoing spinal cord stimulation in a clinical practice setting. Health Qual. Life Outcomes 2018, 16, 1–14. [Google Scholar] [CrossRef] [PubMed]
- North, R.; Shipley, J. Practice Parameters for the Use of Spinal Cord Stimulation in the Treatment of Chronic Neuropathic Pain. Pain Med. 2007, 8, S200–S275. [Google Scholar] [CrossRef] [Green Version]
- Kapural, L.; Peterson, E.; Provenzano, D.A.; Staats, P. Clinical Evidence for Spinal Cord Stimulation for Failed Back Surgery Syndrome (FBSS). Spine 2017, 42, S61–S66. [Google Scholar] [CrossRef]
- Kumar, K.; Taylor, R.S.; Jacques, L.; Eldabe, S.; Meglio, M.; Molet, J.; Thomson, S.; O’Callaghan, J.; Eisenberg, E.; Milbouw, G.; et al. Spinal cord stimulation versus conventional medical management for neuropathic pain: A multicentre randomised controlled trial in patients with failed back surgery syndrome. Pain 2007, 132, 179–188. [Google Scholar] [CrossRef]
- Kim, K.; Jeong, Y.; Youn, Y.; Choi, J.; Kim, J.; Chung, W.; Kim, T.-H. Nonoperative Korean Medicine Combination Therapy for Lumbar Spinal Stenosis: A Retrospective Case-Series Study. Evid. Based Complement. Altern. Med. 2015, 2015, 1–5. [Google Scholar] [CrossRef] [Green Version]
- Shin, J.-S.; Lee, J.; Lee, Y.J.; Kim, M.-R.; Ahn, Y.-J.; Park, K.B.; Shin, B.-C.; Lee, M.S.; Ha, I.-H. Long-term course of alternative and integrative therapy for lumbar disc herniation and risk factors for surgery: A prospective observational 5-year follow-up study. Spine 2016, 41, E955–E963. [Google Scholar] [CrossRef]
- Rigoard, P.; Basu, S.; Desai, M.; Taylor, R.; Annemans, L.; Tan, Y.; Johnson, M.J.; Abeele, C.V.D.; North, R.; PROMISE Study Group. Multicolumn spinal cord stimulation for predominant back pain in failed back surgery syndrome patients: A multicenter randomized controlled trial. Pain 2019, 160, 1410–1420. [Google Scholar] [CrossRef]
- Benyamin, R.; Galan, V.; Hatheway, J.; Kim, P.; Choi, D.; Falowski, S.; Calodney, A.; Sweet, J.; Yu, C.; Kapural, L.; et al. Options: A Prospective, Open-Label Study of High-Dose Spinal Cord Stimulation in Patients with Chronic Back and Leg Pain. Pain Physician 2020, 23, 87–98. [Google Scholar] [CrossRef]
- Lee, J.; Kim, J.; Shin, J.-S.; Lee, Y.J.; Kim, M.-R.; Jeong, S.-Y.; Choi, Y.-J.; Yoon, T.K.; Moon, B.-H.; Yoo, S.-B.; et al. Long-Term Course to Lumbar Disc Resorption Patients and Predictive Factors Associated with Disc Resorption. Evid. Based Complement. Altern. Med. 2017, 2017, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.-S.; Lee, J.; Kim, M.-R.; Jung, J.; Shin, B.-C.; Lee, M.S.; Ha, I.-H. The short-term effect of integrated complementary and alternative medicine treatment in inpatients diagnosed with lumbar intervertebral disc herniation: A prospective observational study. J. Altern. Complement. Med. 2016, 22, 533–543. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.-H.; Lee, Y.J.; Shin, J.-S.; Lee, J.; Jeong, H.; Kim, M.-R.; Park, S.-M.; Go, U.; Kim, S.-M.; Kim, J.-Y.; et al. The Long-Term Course of Outcomes for Lumbar Intervertebral Disc Herniation following Integrated Complementary and Alternative Medicine Inpatient Treatment: A Prospective Observational Study. Evid. Based Complement. Altern. Med. 2017, 2017, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, J.J.; Shin, J.-S.; Choi, Y.; Youn, Y.; Lee, S.; Kwon, S.-R.; Lee, H.; Kang, M.-H.; Ha, I.-H.; Shin, I. Integrative package for low back pain with leg pain in Korea: A prospective cohort study. Complement. Ther. Med. 2010, 18, 78–86. [Google Scholar] [CrossRef]
- Lin, X.-J.; Chen, C.-Y. Advances on study of treatment of lumbar disk herniation by Chinese medicinal herbs. China J. Chin. Mater. Med. 2007, 32, 186–191. [Google Scholar]
- Chung, H.-J.; Lee, H.-S.; Shin, J.-S.; Lee, S.-H.; Park, B.-M.; Youn, Y.-S.; Lee, S.K. Modulation of acute and chronic inflammatory processes by a traditional medicine preparation GCSB-5 both in vitro and in vivo animal models. J. Ethnopharmacol. 2010, 130, 450–459. [Google Scholar] [CrossRef]
- Kim, T.-H.; Yoon, S.-J.; Lee, W.-C.; Kim, J.-K.; Shin, J.; Lee, S.; Lee, S.-M. Protective effect of GCSB-5, an herbal preparation, against peripheral nerve injury in rats. J. Ethnopharmacol. 2011, 136, 297–304. [Google Scholar] [CrossRef]
- Weinstein, J.N.; Lurie, J.D.; Tosteson, T.D.; Hanscom, B.; Tosteson, A.N.; Blood, E.A.; Birkmeyer, N.J.; Hilibrand, A.S.; Herkowitz, H.; Cammisa, F.P.; et al. Surgical versus Nonsurgical Treatment for Lumbar Degenerative Spondylolisthesis. N. Engl. J. Med. 2007, 356, 2257–2270. [Google Scholar] [CrossRef] [Green Version]
- Schulte, T.L.; Ringel, F.; Quante, M.; Eicker, S.O.; Muche-Borowski, C.; Kothe, R. Surgery for adult spondylolisthesis: A systematic review of the evidence. Eur. Spine J. 2015, 25, 2359–2367. [Google Scholar] [CrossRef]
- Luna, S.P.L.; Angeli, A.L.; Ferreira, C.L.; Lettry, V.; Scognamillo-Szabó, M. Comparison of Pharmacopuncture, Aquapuncture and Acepromazine for Sedation of Horses. Evid. Based Complement. Altern. Med. 2008, 5, 267–272. [Google Scholar] [CrossRef] [Green Version]
- Park, J.; Lee, H.; Shin, B.-C.; Lee, M.S.; Kim, B.; Kim, J.-I. Pharmacopuncture in Korea: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Evid. Based Complement. Altern. Med. 2016, 2016, 1–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cheon, S.; Zhang, X.; Lee, I.-S.; Cho, S.-H.; Chae, Y.; Lee, H. Pharmacopuncture for Cancer Care: A Systematic Review. Evid. Based Complement. Altern. Med. 2014, 2014, 1–14. [Google Scholar] [CrossRef] [Green Version]
- Kim, M.; Han, C.-H. Pharmacopuncture for stroke survivors: A systematic review of randomized controlled trials in South Korea. Complement. Ther. Clin. Pract. 2020, 40, 101179. [Google Scholar] [CrossRef]
- Yoon, J.; Jeon, J.-H.; Lee, Y.-W.; Cho, C.-K.; Kwon, K.-R.; Shin, J.-E.; Sagar, S.; Wong, R.; Yoo, H.-S. Sweet Bee Venom Pharmacopuncture for Chemotherapy-Induced Peripheral Neuropathy. J. Acupunct. Meridian Stud. 2012, 5, 156–165. [Google Scholar] [CrossRef]
- Shen, F.-Y.; Lee, M.S.; Jung, S.-K. Effectiveness of Pharmacopuncture for Asthma: A Systematic Review and Meta-Analysis. Evid. Based Complement. Altern. Med. 2011, 2011, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, J.-H.; Chung, H.-J.; Lee, I.-H.; Lee, J.-W.; Kim, E.-J.; Kim, M.-J. Study on Single-dose Intramuscular Toxicity of Shinbaro Pharmacopuncture in Sprague-Dawley (SD) Rats and Beagle Dogs. J. Korean Med. Rehabilit. 2015, 25, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.H.; Ha, I.H.; Kim, M.R.; Kim, M.J.; Lee, J.W.; Lee, I.H.; Chung, H.J.; Kim, E.J. Multiple-dose intramuscular toxicity study of shinbaro pharmacopuncture in sprague-dawley rats over a 4-week period. Acupuncture 2015, 32, 77–89. [Google Scholar] [CrossRef]
- Moon, T.-W.; Choi, T.-Y.; Park, T.-Y.; Lee, M.S. Chuna therapy for musculoskeletal pain: A systematic review of randomized clinical trials in Korean literature. Chin. J. Integr. Med. 2012, 19, 228–232. [Google Scholar] [CrossRef] [PubMed]
- Vickers, A.J.; Cronin, A.M.; Maschino, A.C.; Lewith, G.; MacPherson, H.; Foster, N.E.; Sherman, K.J.; Witt, C.M.; Linde, K.; Acupuncture Trialists’ Collaboration. Acupuncture for chronic pain: Individual patient data meta-analysis. Arch. Intern. Med. 2012, 172, 1444–1453. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.-S.; Ha, I.-H.; Lee, J.; Choi, Y.; Kim, M.-R.; Park, B.-Y.; Shin, B.-C.; Lee, M.S. Effects of motion style acupuncture treatment in acute low back pain patients with severe disability: A multicenter, randomized, controlled, comparative effectiveness trial. Pain 2013, 154, 1030–1037. [Google Scholar] [CrossRef] [Green Version]
- Cho, Y.; Kim, C.; Heo, K.; Lee, M.S.; Ha, I.; Son, D.W.; Choi, B.K.; Song, G.; Shin, B. Acupuncture for Acute Postoperative Pain after Back Surgery: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Pain Pract. 2015, 15, 279–291. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Mean ± SD or Median (%) | |
|---|---|
| Age | |
| Mean ± SD | 54.9 ± 11.5 |
| 20≤, <30 | 3 (1.3) |
| 30≤, <40 | 27 (11.5) |
| 40≤, <50 | 49 (20.9) |
| 50≤, <60 | 54 (23.1) |
| 60≤, <70 | 89 (38.0) |
| 70≤ | 12 (5.1) |
| Sex | |
| Male | 93 (39.7) |
| Female | 141 (60.3) |
| Length of hospital stay | |
| Mean ± SD (day) | 28.1 ± 17.1 |
| Median (IQR) | 23.5 (14.3–38) |
| Type of spinal surgery 1 | |
| Laminectomy | 219 (93.6) |
| Discectomy | 71 (30.3) |
| Spinal fusion | 31 (13.2) |
| Vertebroplasty | 12 (5.1) |
| Artificial disc replacement | 2 (0.9) |
| Operated disc levels1 | |
| L1–2 | 9 (3.8) |
| L2–3 | 13 (5.6) |
| L3–4 | 36 (15.9) |
| L4–5 | 157 (67.1) |
| L5-S1 | 84 (35.9) |
| Duration from pain recurrence until admission | |
| Mean ± SD (day) | 205.4 ± 484.2 |
| Median (IQR) | 39 (7–147.3) |
| Mode of pain recurrence | |
| No specific cause | 150 (64.1) |
| Overwork/Over exercise | 42 (17.9) |
| Trauma/Fall | 33 (14.1) |
| Other | 7 (3.0) |
| Unknown | 2 (0.9) |
| Analgesics † | |
| Mean ± SD | 3.6 ± 10.5 |
| Median (IQR) | 0 (0,1,2,3) |
| Steroid injections † | |
| Mean ± SD | 0.9 ± 3.5 |
| Median (IQR) | 0 (0,1) |
| Radiological findings of MRI/CT scans 1 | |
| Herniation of the nucleus pulposus | 129 (55.1) |
| Protrusion | 77 (32.9) |
| Extrusion | 77 (32.9) |
| Sequestration | 0 (0.0) |
| Spinal stenosis | 67 (28.6) |
| Central canal | 42 (17.9) |
| Foraminal | 42 (17.9) |
| Spondylolisthesis | 17 (7.3) |
| Vertebral fracture | 11 (4.7) |
| Other | 2 (0.9) |
| Comorbidity 1 | |
| Hypertension | 37 (15.8) |
| Diabetes mellitus | 22 (9.4) |
| Cardiovascular disease | 44 (18.8) |
| Thyroid-related comorbidity | 10 (4.3) |
| Liver-related comorbidity | 4 (1.7) |
| Other | 63 (26.9) |
| Smoking | |
| Yes | 44 (18.8) |
| No | 190 (81.2) |
| Alcohol intake | |
| Yes | 44 (18.8) |
| No | 189 (80.8) |
| Unknown | 1 (0.4) |
| Occupation | |
| Unemployed ‡ | 133 (56.8) |
| Office work § | 63 (26.9) |
| Service or retail industry 11 | 22 (9.4) |
| Manual labor †† | 15 (6.4) |
| Unknown | 1 (0.4) |
| Outcome | Outcome | Value | Difference | p-Value | |
|---|---|---|---|---|---|
| NRS | LBP | Admission | 5.77 ± 1.38 | — | |
| Discharge | 3.15 ± 1.49 | −2.62 (−2.82, −2.41) | <0.001 | ||
| Leg pain | Admission | 4.40 ± 2.76 | — | ||
| Discharge | 2.52 ± 1.99 | −1.88 (−2.08, −1.68) | <0.001 | ||
| ODI | Admission | 50.55 ± 16.53 | — | ||
| Discharge | 33.19 ± 15.93 | −17.35 (−19.62, −15.09) | <0.001 | ||
| Follow-up | 27.39 ± 16.97 | −23.50 (−26.39, −20.61) | <0.001 | ||
| EQ-5D | Admission | 0.54 ± 0.22 | — | ||
| Discharge | 0.74 ± 0.13 | 0.20 (0.17, 0.22) | <0.001 | ||
| Follow-up | 0.74 ± 0.17 | 0.20 (0.17, 0.24) | <0.001 | ||
| Discharge (n = 231) | Follow-Up (n = 106) | |||||||
|---|---|---|---|---|---|---|---|---|
| MCID 1 of LBP NRS | MCID 2 of LBP NRS | MCID of ODI | MCID of EQ-5D | MCID of ODI | MCID of EQ-5D | Reoperation | ||
| Case (%) | 96 (41.6) | 109 (47.2) | 146 (63.2) | 101 (43.7) | 79 (74.5) | 45 (42.5) | 13 (12.3) | |
| Age | 20≤, <40 | — | — | — | — | — | — | — |
| 40≤, <60 | 0.60 (0.23, 1.53) | 0.61 (0.20, 1.84) | 0.69 (0.24, 2.03) | 2.38 (0.43, 13.2) | 3.64 (0.57, 23.23) | 3.11 (0.20, 49.16) | 0.30 (0.03, 3.07) | |
| 60≤ | 0.67 (0.24, 1.91) | 0.86 (0.25, 2.96) | 0.62 (0.19, 2.01) | 4.61 (0.74, 28.88) | 2.17 (0.23, 20.54) | 6.50 (0.26, 160.73) | 0.66 (0.06, 7.45) | |
| Sex | Female | 0.72 (0.34, 1.49) | 0.6 (0.25, 1.44) | 0.79 (0.35, 1.79) | 1.21 (0.40, 3.66) | 0.48 (0.07, 3.42) | 0.39 (0.04, 3.59) | 1.76 (0.16, 19.39) |
| Onset | <1 month | — | — | — | — | — | — | — |
| 1≤, <6 months | 1.36 (0.68, 2.72) | 1.04 (0.48, 2.24) | 1.05 (0.51, 2.17) | 1.38 (0.44, 4.34) | 0.19 (0.03, 1.05) | 0.10 (0.01, 0.82) | 8.41 (1.05, 67.57) | |
| 6 months < | 0.89 (0.37, 2.13) | 0.76 (0.29, 2.00) | 1.02 (0.41, 2.49) | 0.84 (0.22, 3.28) | 0.22 (0.03, 1.76) | 0.07 (0.01, 0.75) | 3.99 (0.32, 50.13) | |
| Mode of Onset | Overwork/Over exercise | 1.65 (0.74, 3.68) | 1.33 (0.52, 3.38) | 0.62 (0.26, 1.47) | 1.92 (0.51, 7.13) | 1.52 (0.19, 12.03) | 2.18 (0.21, 22.65) | 1.09 (0.07, 16.21) |
| Trauma/Fall | 2.00 (0.85, 4.71) | 2.01 (0.74, 5.42) | 0.99 (0.39, 2.49) | 1.09 (0.25, 4.69) | 1.40 (0.20, 9.65) | 0.55 (0.05, 5.59) | 6.42 (0.92, 44.9) | |
| Surgery type | Laminectomy | 1.48 (0.48, 4.57) | 1.49 (0.42, 5.33) | 3.20 (1.02, 10.06) | 7.71 (1.13, 52.37) | 0.48 (0.05, 4.84) | 0.35 (0.02, 5.33) | 1.09 (0.08, 15.53) |
| Spinal fusion | 2.01 (0.76, 5.28) | 3.13 (1.03, 9.51) | 0.59 (0.23, 1.54) | 0.31 (0.07, 1.40) | 0.18 (0.03, 1.12) | 0.37 (0.02, 8.20) | 2.61 (0.38, 17.81) | |
| Discectomy | 2.03 (1.07, 3.85) | 1.73 (0.84, 3.56) | 0.75 (0.36, 1.54) | 1.30 (0.46, 3.72) | 1.54 (0.30, 8.02) | 2.58 (0.38, 17.68) | 1.05 (0.17, 6.35) | |
| Operated disc level | L4-5 | 0.85 (0.43, 1.67) | 1.30 (0.61, 2.77) | 0.95 (0.46, 1.96) | 0.70 (0.25, 1.95) | 1.02 (0.23, 4.60) | 0.11 (0.01, 0.95) | 4.96 (0.66, 37.14) |
| Radiological findings | HNP | 2.29 (1.18, 4.47) | 2.97 (1.38, 6.39) | 1.47 (0.73, 2.94) | 1.34 (0.47, 3.82) | 1.80 (0.36, 8.96) | 1.22 (0.21, 6.98) | 0.26 (0.04, 1.85) |
| Stenosis central canal | 1.41 (0.71, 2.82) | 1.78 (0.81, 3.90) | 1.07 (0.52, 2.20) | 0.41 (0.14, 1.23) | 2.82 (0.57, 13.82) | 2.03 (0.20, 21.10) | 0.80 (0.14, 4.58) | |
| Spondylolisthesis | 0.63 (0.18, 2.18) | 0.27 (0.06, 1.16) | 0.29 (0.08, 0.99) | 0.04 (0, 0.37) | 1.33 (0.11, 15.51) | 9.51 (0.33, 278.24) | 3.73 (0.29, 48.21) | |
| Comorbidity | Hypertension | 0.59 (0.25, 1.40) | 0.73 (0.27, 2.00) | 0.70 (0.29, 1.67) | 0.45 (0.12, 1.72) | 0.45 (0.08, 2.59) | 0.75 (0.08, 6.99) | 3.91 (0.44, 35.12) |
| Diabetes mellitus | 1.19 (0.42, 3.41) | 0.46 (0.13, 1.67) | 0.38 (0.13, 1.17) | 0.12 (0.02, 0.72) | 0.13 (0.01, 1.41) | 0.34 (0.01, 17.81) | 0.15 (0.01, 2.63) | |
| Social history | Smoking | 0.27 (0.11, 0.69) | 0.15 (0.05, 0.46) | 0.52 (0.19, 1.40) | 0.47 (0.11, 2.02) | 1.43 (0.12, 16.53) | 1.82 (0.10, 33.60) | 2.02 (0.13, 30.51) |
| Alcohol intake | 1.08 (0.47, 2.47) | 1.46 (0.55, 3.84) | 1.31 (0.55, 3.13) | 1.60 (0.45, 5.74) | 3.64 (0.40, 33.28) | 5.27 (0.49, 57.31) | 1.01 (0.10, 10.13) | |
| NRS at admission | LBP | 1.45 (1.10, 1.90) | 3.43 (2.26, 5.22) | 1.05 (0.80, 1.37) | 0.80 (0.53, 1.20) | 1.06 (0.55, 2.08) | 2.51 (1.07, 5.90) | 0.63 (0.32, 1.28) |
| Leg pain | 0.97 (0.87, 1.09) | 0.88 (0.76, 1.01) | 0.93 (0.81, 1.05) | 0.86 (0.70, 1.05) | 0.87 (0.64, 1.18) | 0.84 (0.59, 1.18) | 1.25 (0.85, 1.83) | |
| ODI at admission | 1.01 (0.98, 1.03) | 1.00 (0.97, 1.03) | 1.06 (1.03, 1.09) | 0.99 (0.95, 1.04) | 1.16 (1.07, 1.27) | 0.85 (0.75, 0.96) | 0.97 (0.90, 1.05) | |
| EQ-5D at admission | 1.00 (0.98, 1.02) | 1.00 (0.98, 1.02) | 0.99 (0.97, 1.01) | 0.82 (0.77, 0.87) | 1.03 (0.98, 1.08) | 0.78 (0.69, 0.88) | 0.99 (0.94, 1.04) | |
| AUC | 0.73 (0.66, 0.80) | 0.84 (0.79, 0.89) | 0.78 (0.72, 0.84) | 0.95 (0.93, 0.98) | 0.89 (0.81, 0.97) | 0.97 (0.94, 1.00) | 0.84 (0.76, 0.93) | |
| Mean ± SD or Median (%) | |
|---|---|
| Duration from the onset to spinal surgery | |
| Mean ± SD (weeks) | 57.9 ± 109.5 |
| Median (IQR) | 8 (2–52) |
| ≤1 week | 21 (19.8) |
| <1 week, <1 month | 12 (11.3) |
| ≤1 month, <2 months | 17 (16.0) |
| ≤2 months, <6 months | 17 (16.0) |
| ≤6 months, <1 year | 3 (2.8) |
| ≤1 year, <2 years | 11 (10.4) |
| ≤2 years | 23 (21.7) |
| Unknown | 2 (1.9) |
| Duration from the first spinal surgery until pain recurrence | |
| Mean ± SD (month) | 40.0 ± 69.1 |
| Median (IQR) | 12 (1–48) |
| Continuation | 17 (16.0) |
| ≤1 month | 16 (15.1) |
| <1 month, <1 year | 11 (10.4) |
| ≤1 year, <3 years | 23 (21.7) |
| ≤3 years, <5 years | 15 (14.2) |
| ≤5 years, <10 years | 12 (11.3) |
| ≤10 years | 12 (11.3) |
| Duration from discharge until follow-up survey | |
| Mean ± SD (months) | 34.54 ± 14.47 |
| Median (IQR) | 34.95 (22.35–46.85) |
| Number of spinal surgeries | 1.3 ± 0.5 |
| Reasons for spinal surgery 1 | |
| No resistance due to significant pain | 65 (61.3) |
| Expectation of a significant pain reduction | 47 (44.3) |
| Compelled by the doctor | 25 (23.6) |
| Few sequelae | 10 (9.4) |
| No information regarding other treatments | 9 (8.5) |
| Low cost burden | 7 (6.6) |
| Easy rehabilitation | 6 (5.7) |
| Recommended by the people around | 2 (1.9) |
| Other | 3 (2.8) |
| Satisfactory reason with spinal surgery 1 | |
| Significant pain reduction | 46 (43.4) |
| Fast pain reduction | 25 (23.6) |
| A short treatment period | 12 (11.3) |
| Low cost burden | 12 (11.3) |
| Few sequelae | 11 (10.4) |
| Sufficient information regarding the surgery | 6 (5.7) |
| Easy rehabilitation | 3 (2.8) |
| Other | 2 (1.9) |
| Unsatisfactory reason for spinal surgery 1 | |
| No pain reduction | 44 (41.5) |
| Sequela | 39 (36.8) |
| Frequent pain recurrence | 39 (36.8) |
| Anxiety | 9 (8.5) |
| No functional recovery | 8 (7.5) |
| Painful treatment | 5 (4.7) |
| Cost burden | 5 (4.7) |
| Insufficient information regarding the surgery | 5 (4.7) |
| Other | 1 (0.9) |
| Recurrence at operated disc level | |
| Same level | 66 (62.3) |
| Contiguous level | 31 (29.2) |
| Different level | 5 (4.7) |
| Unknown | 4 (3.8) |
| Recommendation for reoperation † | |
| Yes | 40 (37.7) |
| No | 66 (62.3) |
| Reoperation † | |
| Yes | 16 (40.0) |
| No | 24 (60.0) |
| Mean ± SD or Median (%) | |
|---|---|
| PGIC for Korean medicine treatment | |
| Very much improved | 21 (19.8) |
| Much improved | 43 (40.6) |
| Minimally improved | 37 (34.9) |
| No change | 5 (4.7) |
| Minimally worse | 0 (0) |
| Much worse | 0 (0) |
| Very much worse | 0 (0) |
| Satisfaction degree of Korean medicine treatment 1 | 7.97 ± 1.98 |
| Korean medicine treatment with highest satisfaction degree † | |
| Pharmacopuncture | 68 (64.2) |
| Chuna manual therapy | 40 (37.7) |
| Acupuncture | 34 (32.1) |
| Herbal medicine | 28 (26.4) |
| Korean physical therapy | 20 (18.9) |
| Cupping | 7 (6.6) |
| Other | 17 (16.0) |
| Satisfactory reason with Korean medicine † | |
| Significant pain reduction | 37 (34.9) |
| Functional recovery | 29 (27.4) |
| Fast pain reduction | 27 (25.5) |
| Not painful treatment | 27 (25.5) |
| Sufficient information regarding treatments | 27 (25.5) |
| Low recurrence | 14 (13.2) |
| Diverse treatment | 11 (10.4) |
| Low cost burden | 0 (0) |
| Other | 7 (6.5) |
| Unsatisfactory reason with Korean medicine † | |
| Cost burden | 27 (25.5) |
| Prolonged treatment period | 16 (15.1) |
| Frequent pain recurrence | 8 (7.5) |
| No pain reduction | 6 (5.7) |
| Insufficient information regarding treatments | 1 (9) |
| Unnecessarily high number of treatment types | 0 (0) |
| Painful treatment | 0 (0) |
| Other | 6 (5.7) |
| Reoperation after taking Korean medicine treatment | |
| Yes | 13 (12.3) |
| No | 93 (87.7) |
| Number of reoperations after taking Korean medicine treatment | 1.5 ± 1.4 |
| Present treatment within 3 months | |
| Yes | 45 (42.5) |
| No | 61 (57.5) |
| Type of present treatment † | |
| Acupuncture | 19 (17.9) |
| Pharmacopuncture | 15 (14.2) |
| Chuna manual therapy | 11 (10.4) |
| Herbal medicine | 10 (9.4) |
| Cupping | 6 (5.7) |
| Manual therapy | 13 (12.3) |
| Physical therapy (ESWT, TENS, ICT) | 10 (9.4) |
| Steroid injection | 8 (7.5) |
| Medication | 8 (7.5) |
| Therapeutic exercise | 5 (4.7) |
| Other | 1 (0.9) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, J.-H.; Choi, K.-E.; Kim, S.-G.; Chu, H.-Y.; Lee, S.-W.; Kim, T.-J.; Cho, H.-W.; Kim, S.D.; Park, K.S.; Lee, Y.J.; et al. Long-Term Follow-Up of Inpatients with Failed Back Surgery Syndrome Who Received Integrative Korean Medicine Treatment: A Retrospective Analysis and Questionnaire Survey Study. J. Clin. Med. 2021, 10, 1703. https://doi.org/10.3390/jcm10081703
Park J-H, Choi K-E, Kim S-G, Chu H-Y, Lee S-W, Kim T-J, Cho H-W, Kim SD, Park KS, Lee YJ, et al. Long-Term Follow-Up of Inpatients with Failed Back Surgery Syndrome Who Received Integrative Korean Medicine Treatment: A Retrospective Analysis and Questionnaire Survey Study. Journal of Clinical Medicine. 2021; 10(8):1703. https://doi.org/10.3390/jcm10081703
Chicago/Turabian StylePark, Ju-Hun, Kang-Eah Choi, Sang-Gyun Kim, Hui-Yeong Chu, Sang-Woon Lee, Tae-Ju Kim, Hyun-Woo Cho, Sang Don Kim, Kyoung Sun Park, Yoon Jae Lee, and et al. 2021. "Long-Term Follow-Up of Inpatients with Failed Back Surgery Syndrome Who Received Integrative Korean Medicine Treatment: A Retrospective Analysis and Questionnaire Survey Study" Journal of Clinical Medicine 10, no. 8: 1703. https://doi.org/10.3390/jcm10081703
APA StylePark, J.-H., Choi, K.-E., Kim, S.-G., Chu, H.-Y., Lee, S.-W., Kim, T.-J., Cho, H.-W., Kim, S. D., Park, K. S., Lee, Y. J., Lee, J. H., & Ha, I.-H. (2021). Long-Term Follow-Up of Inpatients with Failed Back Surgery Syndrome Who Received Integrative Korean Medicine Treatment: A Retrospective Analysis and Questionnaire Survey Study. Journal of Clinical Medicine, 10(8), 1703. https://doi.org/10.3390/jcm10081703







