Mechanical Complications in Adult Spine Deformity Surgery: Retrospective Evaluation of Incidence, Clinical Impact and Risk Factors in a Single-Center Large Series
Abstract
:1. Introduction
2. Materials and Methods
Statistical Analysis
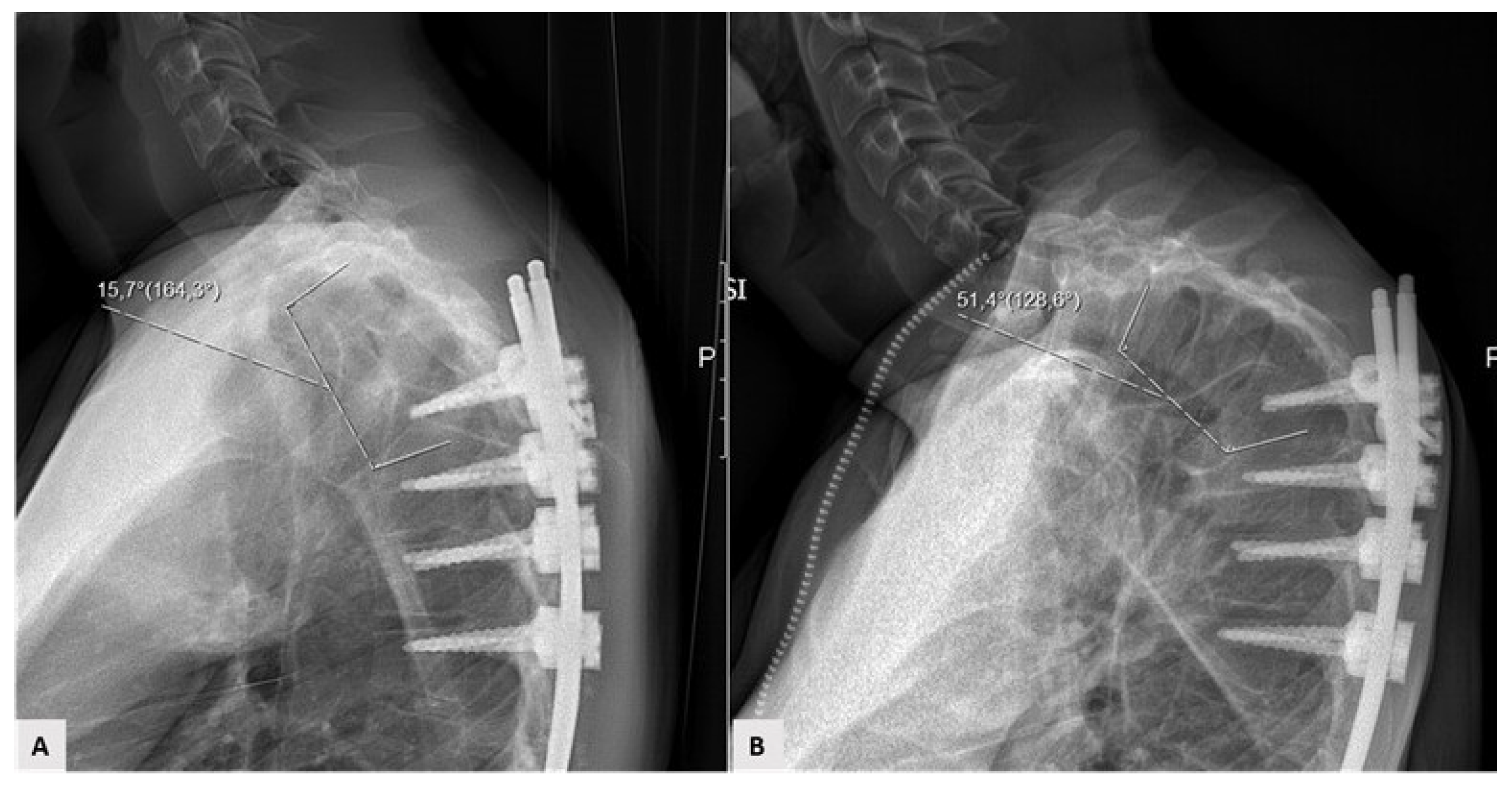
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schwab, F.; Ungar, B.; Blondel, B.; Buchowski, J.; Coe, J.; Deinlein, D.; DeWald, C.; Mehdian, H.; Shaffrey, C.; Tribus, C.; et al. Scoliosis Research Society-Schwab adult spine deformity classification. A validation study. Spine 2012, 37, 1077–1082. [Google Scholar] [CrossRef]
- Schwab, F.; Dubey, A.; Gamez, L.; El Fegoun, A.B.; Hwang, K.; Pagala, M.; Farcy, J.P. Adult scoliosis: Prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine 2005, 30, 1082–1085. [Google Scholar] [CrossRef] [PubMed]
- Lafage, V.; Schwab, F.; Patel, A.; Hawkinson, N.; Farcy, J.P. Pelvic tilt and truncal inclination: Two key radiographic parameters in the setting of adults with spinal deformity. Spine 2009, 34, e599–e606. [Google Scholar] [CrossRef] [PubMed]
- Bridwell, K.H.; Baldus, C.; Berven, S.; Edwards, C., 2nd; Glassman, S.; Hamill, C.; Horton, W.; Lenke, L.G.; Ondra, S.; Schwab, F.; et al. Changes in radiographic and clinical outcomes with primary treatment adult spine deformity surgeries from two years to three- to five-years follow up. Spine 2010, 35, 1849–1854. [Google Scholar] [CrossRef]
- Smith, J.S.; Lafage, V.; Shaffrey, C.I.; Schwab, F.; Lafage, R.; Hostin, R.; O’Brien, M.; Boachie-Adjei, O.; Akbarnia, B.A.; Mundis, G.M.; et al. Outcomes of operative and nonoperative treatment for adult spinal deformity: A prospective, multicenter, propensity-matched cohort assessment with minimum 2-years follow up. Neurosurgery 2016, 78, 851–861. [Google Scholar] [CrossRef]
- Smith, J.S.; Shaffrey, C.I.; Glassman, S.D.; Berven, S.H.; Schwab, F.J.; Hamill, C.L.; Horton, W.C.; Ondra, S.L.; Sansur, C.A.; Bridwell, K.H.; et al. Risk-benefit assessment of surgery for adult scoliosis: An analysis based on patient age. Spine 2011, 36, 817–824. [Google Scholar] [CrossRef]
- Ailon, T.; Smith, J.S.; Shaffrey, C.I.; Soroceanu, A.; Lafage, V.; Schwab, F.; Burton, D.; Hart, R.; Kim, H.J.; Gum, J.; et al. Patients with Adult Spinal Deformity with previous fusions have an equal chance of reaching substantial clinical benefit thresholds in Health-Related Quality of Life measures but do not reach the same absolute level of improvement. World Neurosurg. 2018, 116, e354–e361. [Google Scholar] [CrossRef] [PubMed]
- Daubs, M.D.; Lenke, L.G.; Cheh, G.; Stobbs, G.; Bridwell, K.H. Adult spinal deformity surgery: Complications and outcomes in patients over age 60. Spine 2007, 32, 2238–2244. [Google Scholar] [CrossRef] [PubMed]
- Yadla, S.; Maltenfort, M.G.; Ratliff, J.K.; Harrop, J.S. Adult scoliosis surgery outcomes: A systematic review. Neurosurg. Focus 2010, 28, E3. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.S.; Shaffrey, C.I.; Klineberg, E.; Lafage, V.; Schwab, F.; Lafage, R.; Kim, H.J.; Hostin, R.; Mundis, G.M., Jr.; Gupta, M.; et al. Complication rates associated with 3-column osteotomy in 82 adult spinal deformity patients: Retrospective review of a prospectively collected multicenter consecutive series with 2-year follow-up. J. Neurosurg. Spine 2017, 27, 444–457. [Google Scholar] [CrossRef] [Green Version]
- Yilgor, C.; Sogunmez, N.; Boissiere, L.; Yavuz, Y.; Obeid, I.; Kleinstück, F.; Pérez-Grueso, F.J.S.; Acaroglu, E.; Haddad, S.; Mannion, A.F.; et al. Global Alignment and Proportion (GAP) Score. Development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J. Bone Jt. Surg. Am. 2017, 99, 1661–1672. [Google Scholar] [CrossRef] [PubMed]
- Maruo, K.; Ha, Y.; Inoue, S.; Okada, E.; Hu, S.S.; Deviren, V.; Burch, S.; William, S.; Ames, C.P.; Mummaneni, P.V.; et al. Predictive factors for proximal junctional kyphosis in long fusion to the sacrum in adult spinal deformity. Spine 2013, 38, e1469–e1476. [Google Scholar] [CrossRef]
- Soroceanu, A.; Diebo, B.G.; Burton, D.; Smith, J.S.; Deviren, V.; Shaffrey, C.; Kim, H.J.; Mundis, G.; Ames, C.; Errico, T.; et al. Radiographical and implant-related complications in adult spinal deformity surgery: Incidence, patient risk factors, and impact on health-related quality of life. Spine 2015, 40, 1414–1421. [Google Scholar] [CrossRef]
- Nicholls, F.H.; Bae, J.; Theologis, A.A.; Eksi, M.S.; Ames, C.P.; Berven, S.H.; Burch, S.; Tay, B.K.; Deviren, V. Factors associated with development of and revision for proximal junctional kyphosis in 440 consecutive adult spinal deformity patients. Spine 2017, 42, 1693–1698. [Google Scholar] [CrossRef]
- Yagi, M.; King, A.B.; Boachie-Adjei, O. Incidence, risk factors and natural course of proximal junctional kyphosis. Spine 2012, 37, 1479–1489. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.J.; Bridwell, K.H.; Lenke, L.G.; Glattes, C.R.; Rhim, S.; Cheh, G. Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: Minimum five-year follow-up. Spine 2008, 33, 2179–2184. [Google Scholar] [CrossRef] [PubMed]
- Hassanzadeh, H.; Gupta, S.; Jain, A.; El Dafrawy, M.H.; Skolasky, R.L.; Kebaish, K.M. Type of anchor at the proximal fusion level has a significant effect on the incidence of proximal junctional kyphosis and outcome in adults after long posterior spinal fusion. Spine Deform. 2013, 1, 299–305. [Google Scholar] [CrossRef] [PubMed]
- Scheer, J.K.; Osorio, J.A.; Smith, J.S.; Schwab, F.; Lafage, V.; Hart, R.A.; Bess, S.; Line, B.; Diebo, B.G.; Protopsaltis, T.S.; et al. Development of validated computer-based preoperative predictive model for proximal junction failure (PJF) or clinically significant PJK with 86% accuracy based on 510 ASD patients with 2-year follow-up. Spine 2016, 41, e1328–e1335. [Google Scholar] [CrossRef] [PubMed]
- Lau, D.; Osorio, J.A.; Deviren, V.; Ames, C.P. The relationship of older age and perioperative outcomes following thoracolumbar three-column osteotomy for adult spinal deformity: An analysis of 300 consecutive cases. J. Neurosurg. Spine 2018, 28, 593–606. [Google Scholar] [CrossRef]
- Maier, S.; Smith, J.S.; Schwab, F.F.J.; Obeid, I.; Mundis, G.M.; Klineberg, E.; Hostin, R.; Hart, R.A.; Burton, D.; Boachie-Adjei, O. Revision surgery after three-column osteotomy in 335 adult spinal deformity patients: Inter-center variability and risk factors. Spine 2014, 39, 881–885. [Google Scholar] [CrossRef] [Green Version]
- Schwab, F.J.; Blondel, B.; Bess, S.; Hostin, R.; Shaffrey, C.I.; Smith, J.S.; Boachie-Adjei, O.; Burton, D.C.; Akbarnia, B.A.; Mundis, G.M.; et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity. Spine 2013, 38, e803–e812. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Merrill, R.K.; Kim, J.S.; Leven, D.M.; Kim, J.H.; Cho, S.K. Multi-rod constructs can prevent rod breakage and pseudarthrosis at the lumbosacral junction in adult spinal deformity. Glob. Spine J. 2017, 7, 514–520. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.S.; Shaffrey, C.I.; Ames, C.P.; Demakakos, J.; Fu, K.M.; Keshavarzi, S.; Li, C.M.; Deviren, V.; Schwab, F.J.; Lafage, V.; et al. Assessment of symptomatic rod fracture after posterior instrumented fusion for adult spinal deformity. Neurosurgery 2012, 71, 862–868. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Complication Type | n | % |
|---|---|---|
| Proximal junctional kyphosis | 5 | 33.3 |
| Proximal junctional failure | 4 | 26.7 |
| Distal junctional failure | 2 | 13.3 |
| Rod breakage | 3 | 20 |
| Screws loosening | 1 | 6.7 |
| Early (<6 months) | 5 | 33.3 |
| Delayed (>6 months) | 10 | 66.7 |
| Revision | 8 | 53.3 |
| All Patients | Group A | Group B | p | |
|---|---|---|---|---|
| VAS pre | 7.4 | 7.3 [2.1] | 7.8 [1.3] | =0.38 |
| VAS post | 3.2 | 2.7 [2.2] | 5.5 [1.8] | <0.01 |
| p | <0.01 | <0.01 | =0.03 | |
| ODI pre | 44.6 | 44.2 [14.5] | 46.3 [11.5] | 0.6 |
| ODI post | 19.5 | 15.5 [13.7] | 39.7 [10.2] | <0.01 |
| p | <0.01 | <0.01 | =0.17 | |
| ∆VAS | 4.2 | 4.6 [2.1] | 2.3 [1.8] | =0.01 |
| ∆ODI | 25.1 | 28.7 [15.9] | 6.6 [11.5] | <0.01 |
| All Patients | Group A | Group B | p | |
|---|---|---|---|---|
| Patients, n | 102 | 87 | 15 | - |
| Age, y | 55.7 | 54.8 (10.9) | 61.2 (11.1) | 0.04 |
| F/M | 91/11 | 76/11 | 15/0 | 0.14 |
| Height, cm | 162.1 | 162.3 (7.4) | 161.2 (7.6) | 0.62 |
| Weight, Kg | 64.5 | 64.7 (10.1) | 63.1 (8.8) | 0.53 |
| BMI | 24.5 | 24.6 (3.4) | 24.3 (3.8) | 0.8 |
| Follow-up, m | 40.9 | 41.2 (18) | 39.6 (18.5) | 0.75 |
| Instrumented vertebrae, n | 10.1 | 9.8 (2.9) | 11.2 (3.2) | 0.1 |
| Iliac extension, n | 7 (6.8) | 4 (4.6) | 3 (20) | 0.02 |
| UIV at T1–T5, n | 41(40.2) | 32 (36.8) | 9 (60) | 0.09 |
| Cage application, n | 35 (34.3) | 32 (36.8) | 3 (20) | 0.2 |
| Combined Approach, n | 27 (26.5) | 26 (29.8) | 1 (6.7) | 0.06 |
| All Patients | Group A | Group B | p | |
|---|---|---|---|---|
| Coronal Cobb, ° | 42.9 | 43.3 [18.5] | 41.1 [21.6] | 0.67 |
| SVA, mm | 39.2 | 38.4 [30.6] | 42.3 [37.2] | 0.68 |
| LL, ° | −41.5 | −42.3 [17.5] | −37.9 [17.7] | 0.38 |
| SS, ° | 30.1 | 30.7 [10.7] | 26.5 [13] | 0.17 |
| PT, ° | 21.1 | 20.6 [9.9] | 23.7 [11.5] | 0.27 |
| PI, ° | 51.4 | 51.5 [10.5] | 50.9 [12.9] | 0.87 |
| PI-LL, ° | 9.8 | 9.2 [16.6] | 13.1 [17.4] | 0.41 |
| GT, ° | 22.8 | 21.8 [13.8] | 27.8 [14.9] | 0.12 |
| TK, ° | 33.3 | 32.3 [14.1] | 38.8 [14.1] | 0.11 |
| Postoperative radiographic parameters; mean [standard deviation] | ||||
| Coronal Cobb, ° | 19 | 19.5 [13.3] | 16.4 [12.8] | 0.41 |
| SVA, mm | 27.2 | 25.6 [21.6] | 35.6 [25.9] | 0.11 |
| LL, ° | −44.8 | −46.2 [13.2] | −37.9 [12.6] | 0.02 |
| SS, ° | 30 | 31.2 [9.9] | 24.1 [9.7] | 0.01 |
| PT, ° | 20.8 | 19.8 [8.7] | 26.3 [8.5] | 0.009 |
| PI, ° | 51.4 | 51.6 [10.7] | 50.8 [13.3] | 0.81 |
| PI−LL, ° | 6.6 | 5.4 [11.9] | 12.9 [12.8] | 0.03 |
| GT, ° | 22.9 | 21.7 [10.3] | 29 [12.1] | 0.17 |
| TK, ° | 36.7 | 35.7 [10.9] | 41.8 [10.1] | 0.05 |
| GAP Score 0–2 | GAP Score 3–6 | GS ≥ 7 | ||
|---|---|---|---|---|
| Patients, n | 38 | 28 | 36 | |
| Complications, n | 3 (7.9%) | 4 (14.2%) | 8 (22.2%) | |
| All patients | Group A | Group B | p | |
| GAP Score, mean [SD] | 4.7 | 4.3 [3.5] | 6.9 [4.1] | 0.01 |
| Patient | Age at Intervention (Years) | Gender | BMI | Complication Type | GAP Score | UIV | Instrumented Vertebrae, n |
|---|---|---|---|---|---|---|---|
| 1 | 60 | F | 33.3 | Rod Breakage | 6 | T10 | 7 |
| 2 | 51 | F | 20.8 | Screws Loosening | 4 | T10 | 7 |
| 3 | 63 | F | 22.7 | DJF | 10 | T5 | 13 |
| 4 | 62 | F | 23.5 | DJF | 5 | T11 | 7 |
| 5 | 41 | F | 27.9 | Rod Breakage | 12 | T5 | 13 |
| 6 | 61 | F | 23 | Rod Breakage | 6 | T11 | 8 |
| 7 | 60 | F | 23 | PJF | 2 | T8 | 9 |
| 8 | 62 | F | 22.3 | PJK | 8 | T4 | 13 |
| 9 | 72 | F | 26.7 | PJK | 7 | T11 | 8 |
| 10 | 68 | F | 21.5 | PJK | 7 | T4 | 15 |
| 11 | 35 | F | 19.8 | PJF | 0 | T4 | 11 |
| 12 | 73 | F | 30.9 | PJF | 13 | T4 | 15 |
| 13 | 75 | F | 25.4 | PJF | 13 | T4 | 15 |
| 14 | 66 | F | 21.4 | PJK | 9 | T4 | 15 |
| 15 | 55 | F | 23.1 | PJK | 1 | T5 | 12 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barone, G.; Giudici, F.; Martinelli, N.; Ravier, D.; Muzzi, S.; Minoia, L.; Zagra, A.; Scaramuzzo, L. Mechanical Complications in Adult Spine Deformity Surgery: Retrospective Evaluation of Incidence, Clinical Impact and Risk Factors in a Single-Center Large Series. J. Clin. Med. 2021, 10, 1811. https://doi.org/10.3390/jcm10091811
Barone G, Giudici F, Martinelli N, Ravier D, Muzzi S, Minoia L, Zagra A, Scaramuzzo L. Mechanical Complications in Adult Spine Deformity Surgery: Retrospective Evaluation of Incidence, Clinical Impact and Risk Factors in a Single-Center Large Series. Journal of Clinical Medicine. 2021; 10(9):1811. https://doi.org/10.3390/jcm10091811
Chicago/Turabian StyleBarone, Giuseppe, Fabrizio Giudici, Nicolò Martinelli, Domenico Ravier, Stefano Muzzi, Leone Minoia, Antonino Zagra, and Laura Scaramuzzo. 2021. "Mechanical Complications in Adult Spine Deformity Surgery: Retrospective Evaluation of Incidence, Clinical Impact and Risk Factors in a Single-Center Large Series" Journal of Clinical Medicine 10, no. 9: 1811. https://doi.org/10.3390/jcm10091811








