Hyperuricemia as a Marker of Reduced Left Ventricular Ejection Fraction in Patients with Atrial Fibrillation: Results of the POL-AF Registry Study
Abstract
:1. Introduction
2. Materials and Methods
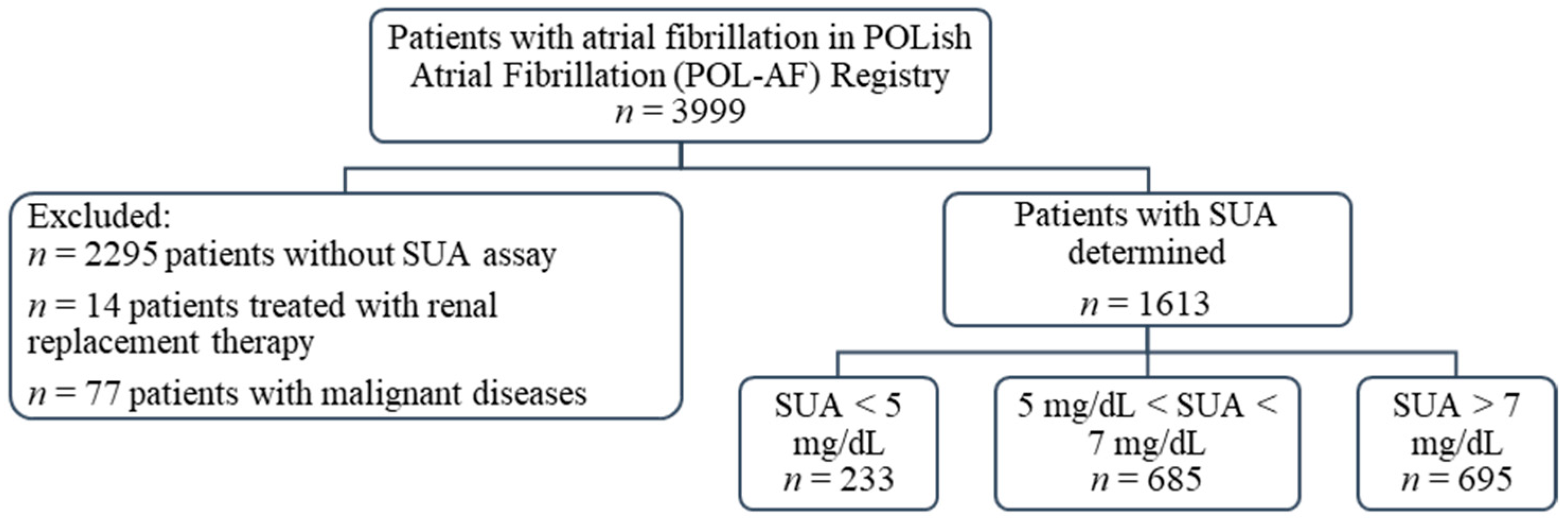
2.1. Study Design and Participants
2.2. Statistical Analysis
3. Results
3.1. General Characteristics
3.2. Uric Acid
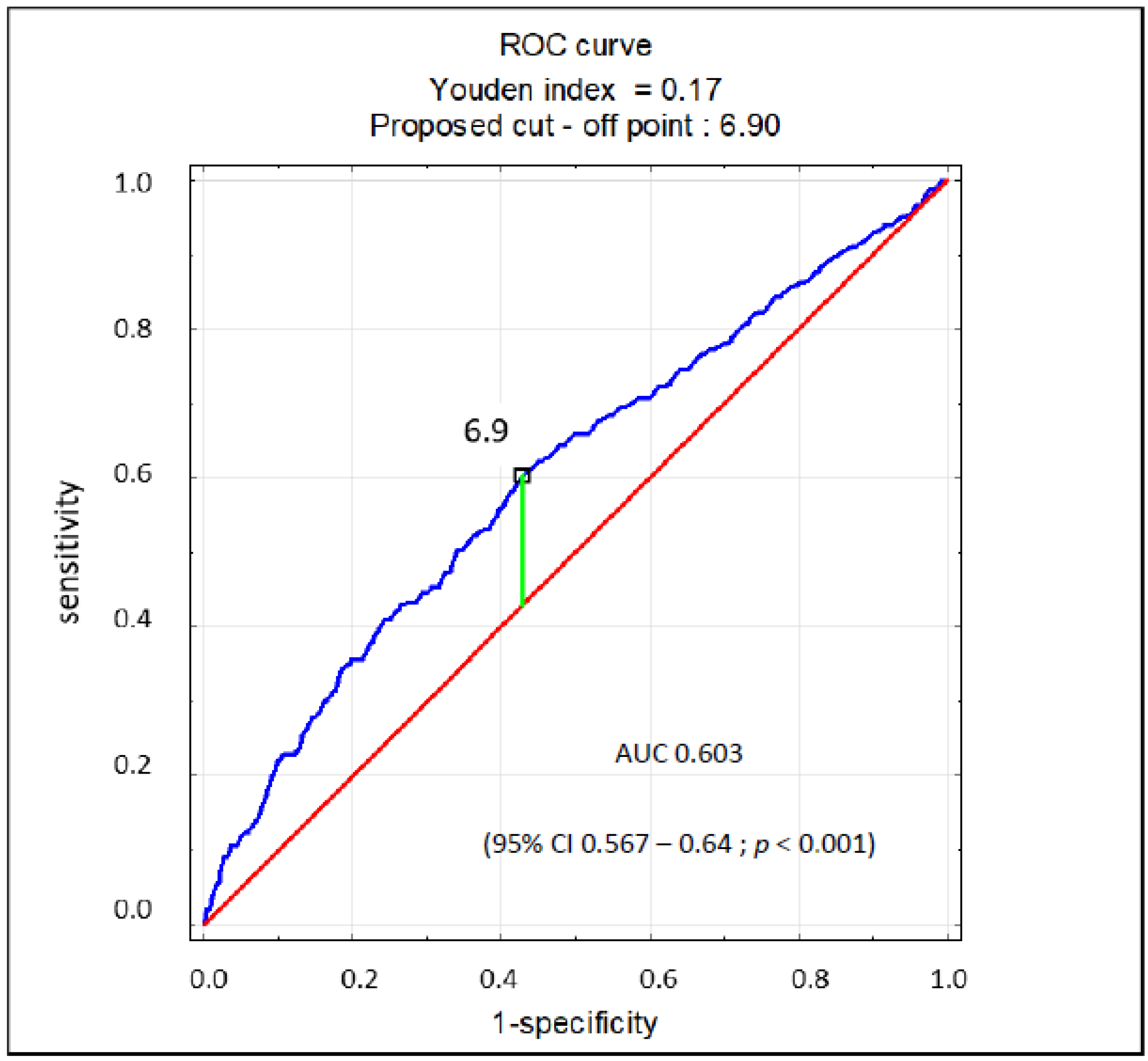
3.3. Markers of Lowered Ejection Fraction of the Left Ventricle
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Khanna, D.; FitzGerland, J.D.; Khanna, P.P.; Bae, S.; Singh, M.; Neogi, T.; Pillinger, M.H.; Merill, J.; Lee, S.; Prakash, S.; et al. 2012 American College of Rheumatology Guidelines for Management of Gout Part 1: Systematic Non-pharmacologic nd Pharmacologic Therapeutic Approaches to Hyperuricemia. Arthritis Care Res. 2012, 64, 1431–1446. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khanna, D.; Khanna, P.P.; FitzGerland, J.D.; Singh, M.; Bae, S.; Neogi, T.; Pillinger, M.H.; Merill, J.; Lee, S.; Prakash, S.; et al. 2012 American College of Rheumatology Guidelines for Management of Gout. Part 2: Therapy and Anti-inflammatory Prophylaxis of Acute Gouty Arthritis. Arthritis Care Res. 2012, 64, 1447–1461. [Google Scholar] [CrossRef]
- Richette, P.; Doherty, M.; Pascual, E.; Barskova, V.; Becce, F.; Castañeda-Sanabria, J.; Coyfish, M.; Guillo, S.; Jansen, T.L.; Janssens, H.; et al. 2016 updated EULAR evidence-based recommendations for the management of gout. Ann. Rheum. Dis. 2017, 76, 29–42. [Google Scholar] [CrossRef]
- Borghi, C.; Tykarski, A.; Widecka, K.; Filipiak, K.J.; Domienik-Karłowicz, J.; Kostka-Jeziorny, K.; Varga, A.; Jaguszewski, M.; Narkiewicz, K.; Mancia, G. Expert consensus for the diagnosis and treatment of patient with hyperuricemia and high cardiovascular risk. Cardiol. J. 2018, 25, 545–563. [Google Scholar] [CrossRef]
- Borghi, C.; Domienik-Karłowicz, J.; Tykarski, A.; Widecka, K.; Filipiak, K.J.; Jaguszewski, M.J.; Narkiewicz, K.; Mancia, G. Expert consensus for the diagnosis and treatment of patient with hyperuricemia and high cardiovascular risk: 2021 update. Cardiol. J. 2021, 28, 1–14. [Google Scholar] [CrossRef]
- Norvik, J.V.; Storhaug, H.M.; Ytrehus, K.; Jenssen, T.G.; Zykova, S.N.; Eriksen, B.O.; Solbu, M.D. Overweight modifies the longitudinal association between uric acid and some components of the metabolic syndrome: The Tromsø Study. BMC Cardiovasc. Disord. 2016, 16, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shirasawa, T.; Ochiai, H.; Yoshimoto, T.; Nagahama, S.; Watanabe, A.; Yoshida, R.; Kokaze, A. Cross-sectional study of associations between normal body weight with central obesity and hyperuricemia in Japan. BMC Endocr. Disord. 2020, 20, 2. [Google Scholar] [CrossRef] [Green Version]
- Bombelli, M.; Ronchi, I.; Volpe, M.; Facchetti, R.; Carugo, S.; Dell’oro, R.; Cuspidi, C.; Grassi, G.; Mancia, G. Prognostic value of serum uric acid: New-onset in and out-of-office hypertension and long-term mortality. J. Hypertens. 2014, 32, 1237–1244. [Google Scholar] [CrossRef]
- Grayson, P.C.; Kim, S.Y.; LaValley, M.; Choi, H.K. Hyperuricemia and incident hypertension: A systematic review and meta-analysis. Arthritis Care Res. 2011, 63, 102–110. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.Y.; Guevara, J.P.; Kim, K.M.; Choi, H.K.; Heitjan, D.F.; Albert, D.A. Hyperuricemia and risk of stroke: A systematic review and meta-analysis. Arthritis Rheum. 2009, 61, 885–892. [Google Scholar] [CrossRef] [Green Version]
- Zhong, C.; Zhong, X.; Xu, T.; Xu, T.; Zhang, Y. Sex-Specific relationship between serum uric acid and risk of stroke: A dose-response me-ta-analysis of prospective studies. J. Am. Heart Assoc. 2017, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ndrepepa, G.; Braun, S.; Haase, H.-U.; Schulz, S.; Ranftl, S.; Hadamitzky, M.; Mehilli, J.; Schömig, A.; Kastrati, A. Prognostic Value of Uric Acid in Patients With Acute Coronary Syndromes. Am. J. Cardiol. 2012, 109, 1260–1265. [Google Scholar] [CrossRef] [PubMed]
- Ilundain-González, A.I.; Gimeno-Orna, J.A.; Sáenz-Abad, D.; Pons-Dolset, J.; Hoyo, J.C.-D.; Lahoza-Pérez, M.D.C. Impact of uric acid levels on the risk of long-term cardiovascular mortality in patients with type 2 diabetes mellitus. Endocrinol. Diabetes Nutr. 2018, 65, 335–341. [Google Scholar] [CrossRef]
- Manolis, A.J. Serum uric acid and atrial fibrillation. Curr. Med. Res. Opin. 2017, 33, 21–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ono, K. How Is Uric Acid Related to Atrial Fibrillation? Circ. J. 2019, 83, 705–706. [Google Scholar] [CrossRef] [PubMed]
- Tamariz, L.; Agarwal, S.; Soliman, E.Z.; Chamberlain, A.M.; Prineas, R.; Folsom, A.R.; Ambrose, M.; Alonso, A. Association of Serum Uric Acid With Incident Atrial Fibrillation (from the Atherosclerosis Risk in Communities [ARIC] Study). Am. J. Cardiol. 2011, 108, 1272–1276. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, C.H.; Huang, D.S.; Shen, D.; Zhang, L.W.; Ma, Y.J.; Wang, Y.M.; Sun, H.Y. Association Between Serum Uric Acid Levels and Atrial Fibrillation Risk. Cell. Physiol. Biochem. 2016, 38, 1589–1595. [Google Scholar] [CrossRef]
- Xu, X.; Du, N.; Wang, R.; Wang, Y.; Cai, S. Hyperuricemia is independently associated with increased risk of atrial fibrillation: A meta-analysis of cohort studies. Int. J. Cardiol. 2015, 184, 699–702. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Zheng, R.; Li, H.; Guo, J. Serum uric acid and incident atrial fibrillation: A systematic review and dose–response meta-analysis. Clin. Exp. Pharmacol. Physiol. 2020, 47, 1774–1782. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.; Huang, B.; Li, Y.; Huang, Y.; Li, J.; Yao, H.; Jing, X.; Chen, J.; Wang, J. Uric acid and risk of heart failure: A systematic review and meta-analysis. Eur. J. Heart Fail. 2013, 16, 15–24. [Google Scholar] [CrossRef] [PubMed]
- Huang, G.; Qin, J.; Deng, X.; Luo, G.; Yu, D.; Zhang, M.; Zhou, S.; Wang, L. Prognostic value of serum uric acid in patients with acute heart failure: A meta-analysis. Medicine 2019, 98, e14525. [Google Scholar] [CrossRef] [PubMed]
- Kanbay, M.; Afsar, B.; Siriopol, D.; Dincer, N.; Erden, N.; Yilmaz, O.; Sag, A.A.; Kuwabara, M.; Cherney, D.; Rossignol, P.; et al. Effect of Uric Acid-Lowering Agents on Cardiovascular Outcome in Patients With Heart Failure: A Systematic Review and Meta-Analysis of Clinical Studies. Angiology 2020, 71, 315–323. [Google Scholar] [CrossRef] [PubMed]
- Seferovic, P.M.; Ponikowski, P.; Anker, S.D.; Bauersachs, J.; Chioncel, O.; Cleland, J.G.; De Boer, R.A.; Drexel, H.; Ben Gal, T.; Hill, L.; et al. Clinical practice update on heart failure 2019: Pharmacotherapy, procedures, devices and patient management. An expert consensus meeting report of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 2019, 21, 1169–1186. [Google Scholar] [CrossRef] [PubMed]
- Chase, P.J.; Davis, P.G.; Bensimhon, D.R. The Obesity Paradox in Chronic Heart Failure: What Does It Mean? Curr. Heart Fail. Rep. 2014, 11, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Maharani, N.; Kuwabara, M.; Hisatome, I. Hyperuricemia and Atrial Fibrillation. Int. Heart J. 2016, 57, 395–399. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Corry, D.B.; Eslami, P.; Yamamoto, K.; Nyby, M.D.; Makino, H.; Tuck, M.L. Uric acid stimulates vascular smooth muscle cell pro-liferation and oxidative stress via the vascular renin-angiotensin system. J. Hypertens. 2008, 26, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Kumrić, M.; Borovac, J.; Kurir, T.; Božić, J. Clinical Implications of Uric Acid in Heart Failure: A Comprehensive Review. Life 2021, 11, 53. [Google Scholar] [CrossRef] [PubMed]
| Demographics | Number (%) or Mean (±SD) | ||
| Women | 705 (44) | ||
| Age (years) | 71.98 (±11.61) | ||
| BMI (kg/m2) | 29.35 (±5.60) | ||
| SUA < 5 mg/dL | 233 (14) | ||
| SUA > 7 mg/dL | 695 (43) | ||
| High cardiovascular risk * | 1362 (84) | ||
| Comorbidities | Number (%) | ||
| Arterial hypertension | 1343 (83) | ||
| Heart failure | 1087 (67) | ||
| HFrEF (EF < 40%) | 300 (19) | ||
| Diabetes | 539 (33) | ||
| History of stroke | 190 (12) | ||
| History of TIA | 95 (6) | ||
| CAD | 806 (50) | ||
| Post CABG | 121 (7.5) | ||
| Post PCI | 365 (23) | ||
| History of MI | 355 (22) | ||
| PAD | 232 (14) | ||
| CKD (MDRD < 60) | 812 (50) | ||
| Laboratory Results (unit) | Mean | Standard Deviation | |
| HGB (g/dL) | 13.25 | 1.88 | |
| GFR (mL/min/1.73 m2) | 62.24 | 22.12 | |
| ALT (U/L) | 31.05 | 52.03 | |
| AST (U/L) | 33.48 | 50.10 | |
| SUA (mg/dL) | 6.88 | 1.93 | |
| TC (mg/dL) | 167.47 | 52.40 | |
| LDL (mg/dL) | 97.93 | 43.67 | |
| HDL (mg/dL) | 47.60 | 22.12 | |
| TG (mg/dL) | 124.88 | 61.75 | |
| EF (%) | 48.84 | 13.34 | |
| Parameter (Unit) | SUA > 7 (n = 695) | SUA < 5 (n = 233) | p Value | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Age (years) | 71.94 | 11.85 | 72.23 | 11.05 | 0.733 |
| BMI (kg/m2) | 28.90 | 5.54 | 29.73 | 5.36 | 0.078 |
| Creatinine (mg/dL) | 1.28 | 0.43 | 1.14 | 0.62 | <0.001 |
| GFR (mL/min/1.73 m2) | 57.88 | 20.33 | 69.11 | 24.20 | <0.001 |
| UA (mg/dL) | 8.59 | 1.45 | 4.37 | 1.04 | <0.001 |
| TC (mg/dL) | 165.61 | 54.37 | 154.79 | 47.75 | 0.008 |
| LDL (mg/dL) | 97.01 | 45.28 | 90.59 | 40.73 | 0.060 |
| HDL (mg/dL) | 46.01 | 24.04 | 46.78 | 13.45 | 0.649 |
| TG (mg/dL) | 129.75 | 66.21 | 100.88 | 46.81 | <0.001 |
| EF (%) | 46.83 | 14.47 | 50.17 | 11.49 | 0.003 |
| EF ranges | n (%) | n (%) | p value | ||
| EF < 40% | 168 (24) | 31 (13) | <0.001 | ||
| EF ≥ 50% | 325 (47) | 132 (57) | 0.001 | ||
| EF 40–50% | 91 (13) | 29 (12) | 0.874 | ||
| No ECHO | 111 (16) | 41 (18) | 0.561 | ||
| Medications | n (%) | n (%) | p value | ||
| Beta-blockers | 198 (85) | 609 (88) | 0.384 | ||
| ACE-I | 134 (57,5) | 417 (60) | 0.608 | ||
| Sartans | 41 (18) | 151 (22) | 0.190 | ||
| Aldosteron antagonists | 79 (34) | 325 (47) | <0.001 | ||
| Other diuretics | 135 (56) | 518 (74,5) | <0.001 | ||
| Digoxin | 24 (10) | 68 (10) | 0.790 | ||
| A Correlations for the Whole Study Group | ||||||||
| Correlation index (r) | SUA | Age | Cr | GFR | LDL | HDL | TG | EF |
| SUA (mg/dL) | 1.00 | −0.03 | 0.23 | −0.24 | −0.04 | −0.10 | 0.06 | −0.19 |
| Age (years) | −0.03 | 1.00 | −0.04 | −0.14 | −0.04 | 0.00 | 0.03 | −0.01 |
| Cr (mg/dL) | 0.23 | −0.04 | 1.00 | −0.75 | −0.06 | −0.09 | 0.02 | −0.20 |
| GFR (mL/min/1.73 m2) | −0.24 | −0.14 | −0.75 | 1.00 | 0.03 | 0.05 | −0.05 | 0.17 |
| LDL (mg/dL) | −0.04 | −0.04 | −0.06 | 0.03 | 1.00 | 0.08 | 0.38 | 0.10 |
| HDL (mg/dL) | −0.10 | 0.00 | −0.09 | 0.05 | 0.08 | 1.00 | 0.00 | 0.11 |
| TG (mg/dL) | 0.06 | 0.03 | 0.02 | −0.05 | 0.38 | 0.00 | 1.00 | 0.08 |
| EF (%) | −0.19 | −0.01 | −0.20 | 0.17 | 0.10 | 0.11 | 0.08 | 1.00 |
| B Correlations for UA < 5 | ||||||||
| Correlation index (r) | SUA | Age | Cr | GFR | LDL | HDL | TG | EF |
| SUA (mg/dL) | 1.00 | 0.00 | 0.09 | −0.04 | −0.05 | −0.17 | −0.03 | −0.01 |
| Age (years) | 0.00 | 1.00 | −0.02 | −0.06 | −0.08 | 0.13 | 0.00 | 0.13 |
| Cr (mg/dL) | 0.09 | −0.02 | 1.00 | −0.08 | −0.06 | −0.11 | 0.15 | −0.26 |
| GFR (mL/min/1.73 m2) | −0.04 | −0.06 | −0.08 | 1.00 | 0.01 | 0.08 | −0.09 | 0.04 |
| LDL (mg/dL) | −0.05 | −0.08 | −0.06 | 0.01 | 1.00 | 0.14 | 0.29 | −0.02 |
| HDL (mg/dL) | −0.17 | 0.13 | −0.11 | 0.08 | 0.14 | 1.00 | −0.14 | 0.12 |
| TG (mg/dL) | −0.03 | 0.00 | 0.15 | −0.09 | 0.29 | −0.14 | 1.00 | −0.10 |
| EF (%) | −0.01 | 0.13 | −0.26 | 0.04 | −0.02 | 0.12 | −0.10 | 1.00 |
| C Correlations for UA > 7 | ||||||||
| Correlation index (r) | SUA | Age | Cr | GFR | LDL | HDL | TG | EF |
| SUA (mg/dl) | 1.00 | −0.03 | 0.20 | −0.12 | −0.14 | −0.15 | −0.06 | −0.18 |
| Age (years) | −0.03 | 1.00 | −0.03 | −0.17 | −0.06 | 0.00 | 0.01 | −0.03 |
| Cr (mg/dL) | 0.20 | −0.03 | 1.00 | −0.78 | −0.16 | −0.07 | 0.00 | −0.20 |
| GFR (mL/min/1.73 m2) | −0.12 | −0.17 | −0.78 | 1.00 | 0.15 | 0.02 | −0.01 | 0.17 |
| LDL (mg/dL) | −0.14 | −0.06 | −0.16 | 0.15 | 1.00 | 0.10 | 0.39 | 0.15 |
| HDL (mg/dL) | −0.15 | 0.00 | −0.07 | 0.02 | 0.10 | 1.00 | 0.01 | 0.11 |
| TG (mg/dL) | −0.06 | 0.01 | 0.00 | −0.01 | 0.39 | 0.01 | 1.00 | 0.15 |
| EF (%) | −0.18 | −0.03 | −0.20 | 0.17 | 0.15 | 0.11 | 0.15 | 1.00 |
| OR | 95% CI | p Value | |
|---|---|---|---|
| SUA < 5 mg/dL | 0.966 | 0.624–1.496 | 0.877 |
| SUA > 7 mg/dL | 1.741 | 1.319–2.298 | <0.001 |
| GFR < 60 mL/min/1.73 m2 | 1.939 | 1.459–2.578 | <0.001 |
| AH | 1.155 | 0.812–1.641 | 0.423 |
| DM | 0.952 | 0.720–1.260 | 0.731 |
| History of MI | 1.071 | 0.780–1.471 | 0.671 |
| Female sex | 0.735 | 0.556–0.971 | 0.030 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wełnicki, M.; Gorczyca, I.; Wójcik, W.; Jelonek, O.; Maciorowska, M.; Uziębło-Życzkowska, B.; Wójcik, M.; Błaszczyk, R.; Rajtar-Salwa, R.; Tokarek, T.; et al. Hyperuricemia as a Marker of Reduced Left Ventricular Ejection Fraction in Patients with Atrial Fibrillation: Results of the POL-AF Registry Study. J. Clin. Med. 2021, 10, 1829. https://doi.org/10.3390/jcm10091829
Wełnicki M, Gorczyca I, Wójcik W, Jelonek O, Maciorowska M, Uziębło-Życzkowska B, Wójcik M, Błaszczyk R, Rajtar-Salwa R, Tokarek T, et al. Hyperuricemia as a Marker of Reduced Left Ventricular Ejection Fraction in Patients with Atrial Fibrillation: Results of the POL-AF Registry Study. Journal of Clinical Medicine. 2021; 10(9):1829. https://doi.org/10.3390/jcm10091829
Chicago/Turabian StyleWełnicki, Marcin, Iwona Gorczyca, Wiktor Wójcik, Olga Jelonek, Małgorzata Maciorowska, Beata Uziębło-Życzkowska, Maciej Wójcik, Robert Błaszczyk, Renata Rajtar-Salwa, Tomasz Tokarek, and et al. 2021. "Hyperuricemia as a Marker of Reduced Left Ventricular Ejection Fraction in Patients with Atrial Fibrillation: Results of the POL-AF Registry Study" Journal of Clinical Medicine 10, no. 9: 1829. https://doi.org/10.3390/jcm10091829
APA StyleWełnicki, M., Gorczyca, I., Wójcik, W., Jelonek, O., Maciorowska, M., Uziębło-Życzkowska, B., Wójcik, M., Błaszczyk, R., Rajtar-Salwa, R., Tokarek, T., Bil, J., Wojewódzki, M., Szpotowicz, A., Krzciuk, M., Gawałko, M., Kapłon-Cieślicka, A., Tomaszuk-Kazberuk, A., Szyszkowska, A., Bednarski, J., ... Mamcarz, A. (2021). Hyperuricemia as a Marker of Reduced Left Ventricular Ejection Fraction in Patients with Atrial Fibrillation: Results of the POL-AF Registry Study. Journal of Clinical Medicine, 10(9), 1829. https://doi.org/10.3390/jcm10091829









