Clinical Features and Diagnosis of Cardiac Sarcoidosis
Abstract
:1. Introduction
Epidemiology
2. Clinical Features of Cardiac Sarcoidosis
3. Diagnosis of Cardiac Sarcoidosis
3.1. Patient Screening for Cardiac Involvement
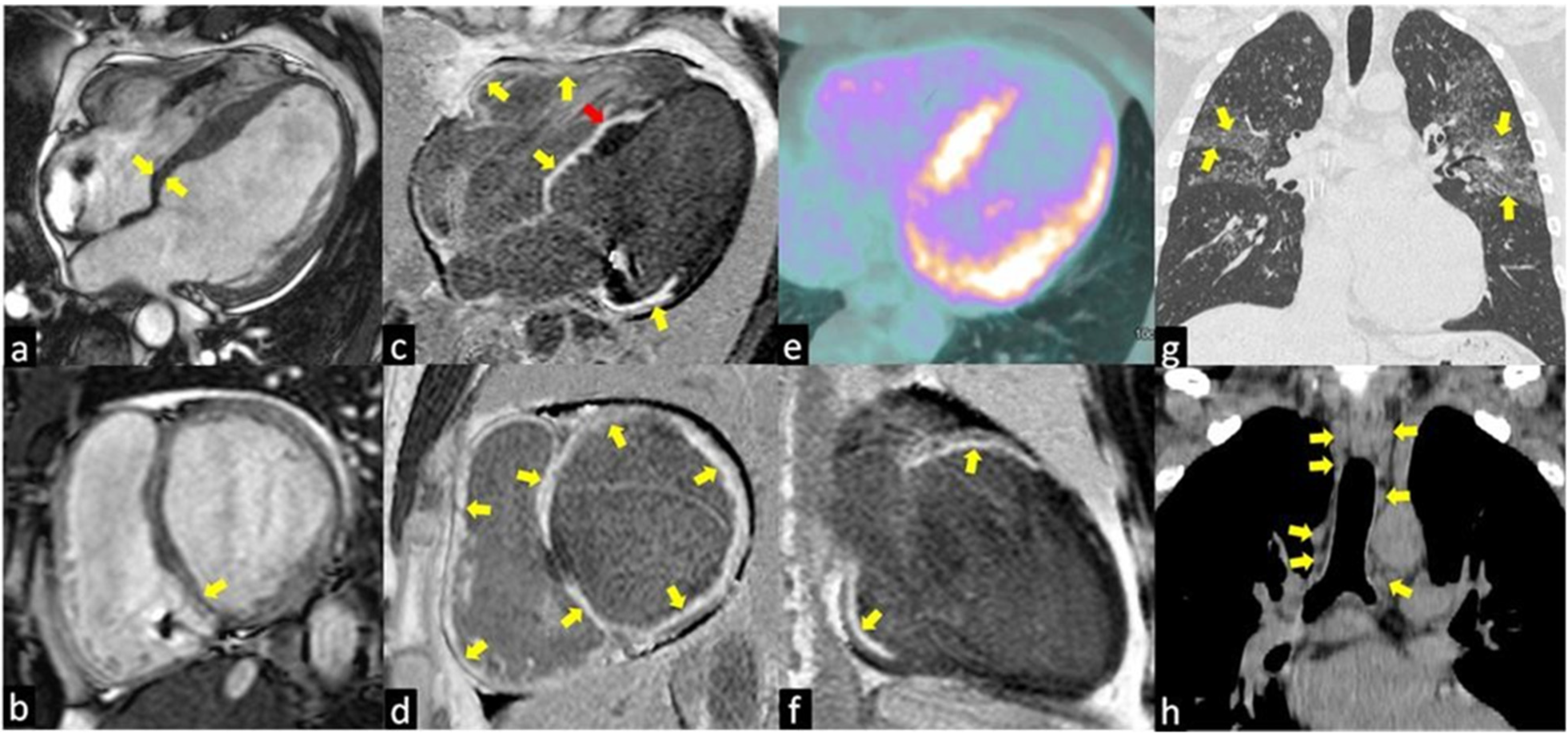
3.2. Cardiac MRI
4. 18F-FDG PET Study of Cardiac Sarcoidosis
4.1. Hybrid PET/CMR Imaging
4.2. Endomyocardial Biopsy
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Birnie, D.; Ha, A.C.; Gula, L.J.; Chakrabarti, S.; Beanlands, R.S.; Nery, P. Cardiac Sarcoidosis. Clin. Chest Med. 2015, 36, 657–668. [Google Scholar] [CrossRef]
- Tana, C.; Schiavone, C.; Cipollone, F.; Giamberardino, M.A. Management issues of sarcoidosis in the time of COVID. Chest 2021, 159, 1306–1307. [Google Scholar]
- Tchernev, G.; Cardoso, J.C.; Chokoeva, A.A.; Verma, S.B.; Tana, C.; Ananiev, J.; Gulubova, M.; Philipov, S.; Kanazawa, N.; Nenoff, P.; et al. The "mystery" of cutaneous sarcoidosis: Facts and controversies. Int. J. Immunopathol. Pharmacol. 2014, 27, 321–330. [Google Scholar] [CrossRef] [Green Version]
- Silverman, K.J.; Hutchins, G.M.; Bilkley, B.H. Cardiac sarcoidosis: A clinicopathologic study of 84 unselected patients with systemic sarcoidosis. Circulation 1978, 58, 1204–1211. [Google Scholar] [CrossRef] [Green Version]
- Tana, C.; Tchernev, G.; Chokoeva, A.A.; Wollina, U.; Lotti, T.; Fioranelli, M.; Roccia, M.G.; Maximov, G.K.; Silingardi, M. Pulmonary and abdominal sarcoidosis, the great imitators on imaging? J. Biol. Regul. Homeost. Agents 2016, 30, 45–48. [Google Scholar]
- Iannuzzi, M.C.; Rybicki, B.A.; Teirstein, A.S. Sarcoidosis. N. Engl. J. Med. 2007, 357, 2153–2165. [Google Scholar] [CrossRef] [PubMed]
- Tchernev, G.; Chokoeva, A.A.; Tana, M.; Tana, C. Transcriptional blood signatures of sarcoidosis, sarcoid-like reactions and tubercolosis and their diagnostic implications. Sarcoidosis Vasc. Diffus. Lung Dis. Off. J. WASOG 2016, 33, 5030. [Google Scholar]
- Tana, C.; Donatiello, I.; Coppola, M.G.; Ricci, F.; Maccarone, M.T.; Ciarambino, T.; Cipollone, F.; Giamberardino, M.A. CT Findings in Pulmonary and Abdominal Sarcoidosis. Implications for Diagnosis and Classification. J. Clin. Med. 2020, 9, 3028. [Google Scholar] [CrossRef]
- Tana, C.; Wegener, S.; Borys, E.; Pambuccian, S.; Tchernev, G.; Tana, M.; Giamberardino, M.A.; Silingardi, M. Challenges in the diagnosis and treatment of neurosarcoidosis. Ann. Med. 2015, 47, 1–16. [Google Scholar] [CrossRef] [Green Version]
- Tchernev, G.; Chokoeva, A.A.; Tana, C.; Patterson, J.W.; Wollina, U.; Lotti, T. Sarcoid sine sarcoidosis? A classificative, semantic and therapeutic dilemma. J. Boil. Regul. Homeost. Agents 2015, 29, 33–34. [Google Scholar]
- Patel, M.R.; Cawley, P.J.; Heitner, J.F.; Klem, I.; Parker, M.A.; Jaroudi, W.A.; Meine, T.J.; White, J.B.; Elliott, M.D.; Kim, H.W.; et al. Detection of Myocardial Damage in Patients With Sarcoidosis. Circulation 2009, 120, 1969–1977. [Google Scholar] [CrossRef] [Green Version]
- Kandolin, R.; Lehtonen, J.; Airaksinen, J.; Vihinen, T.; Miettinen, H.; Ylitalo, K.; Kaikkonen, K.; Tuohinen, S.; Haataja, P.; Kerola, T.; et al. Cardiac sarcoidosis: Epidemiology, characteristics, and outcome over 25 years in a nationwide study. Circulation 2015, 131, 624–632. [Google Scholar] [CrossRef] [PubMed]
- Tezuka, D.; Terashima, M.; Kato, Y.; Toriihara, A.; Hirasawa, K.; Sasaoka, T.; Yoshikawa, S.; Maejima, Y.; Ashikaga, T.; Suzuki, J.-I.; et al. Clinical Characteristics of Definite or Suspected Isolated Cardiac Sarcoidosis: Application of Cardiac Magnetic Resonance Imaging and 18F-Fluoro-2-deoxyglucose Positron-Emission Tomography/Computerized Tomography. J. Card. Fail. 2015, 21, 313–322. [Google Scholar] [CrossRef]
- Okada, D.R.; Bravo, P.E.; Vita, T.; Agarwal, V.; Osborne, M.T.; Taqueti, V.R.; Skali, H.; Chareonthaitawee, P.; Dorbala, S.; Stewart, G.; et al. Isolated cardiac sarcoidosis: A focused review of an under-recognized entity. J. Nucl. Cardiol. 2018, 25, 1136–1146. [Google Scholar] [CrossRef] [PubMed]
- Sadek, M.M.; Yung, D.; Birnie, D.H.; Beanlands, R.S.; Nerdy, P.B. Corticosteroid therapy for cardiac sarcoidosis a systematic review. Can. J. Cardiol. 2013, 29, 1034–1041. [Google Scholar] [CrossRef]
- Roberts, W.C.; McAllister, H.A., Jr.; Ferrans, V.J. Sarcoidosis of the heart. A clinicopathologic study of 35 necropsy patients (group 1) and review of 78 previously described necropsy patients (group 11). Am. J. Med. 1977, 63, 86–108. [Google Scholar] [CrossRef]
- Patel, N.; Kalra, R.; Doshi, R.; Arora, H.; Bajaj, N.S.; Arora, G.; Arora, P. Hospitalization Rates, Prevalence of Cardiovascular Manifestations, and Outcomes Associated With Sarcoidosis in the United States. J. Am. Hear. Assoc. 2018, 7, e007844. [Google Scholar] [CrossRef] [Green Version]
- Terasaki, F.; Ukimura, A.; Tsukada, B.; Fujita, S.; Katashima, T.; Otsuka, K.; Otsuka, K.; Kanzaki, Y.; Shimomura, H.; Fujita, M.; et al. Enhanced Expression of Type 1 Helper T-Cell Cytokines in the Myocardium of Active Cardiac Sarcoidosis. Circ. J. 2008, 72, 1303–1307. [Google Scholar] [CrossRef] [Green Version]
- Ricci, F.; Mantini, C.; Grigoratos, C.; Bianco, F.; Bucciarelli, V.; Tana, C.; Mastrodicasa, D.; Caulo, M.; Aquaro, G.D.; Cotroneo, A.R.; et al. The Multi-modality Cardiac Imaging Approach to Cardiac Sarcoidosis. Curr. Med Imaging Formerly: Curr. Med Imaging Rev. 2018, 15, 10–20. [Google Scholar] [CrossRef]
- Nery, P.B.; Beanlands, R.S.; Nair, G.M.; Green, M.; Yang, J.; McArdle, B.A.; Davis, D.; Ohira, H.; Gollob, M.H.; Leung, E.; et al. Atrioventricular Block as the Initial Manifestation of Cardiac Sarcoidosis in Middle-Aged Adults. J. Cardiovasc. Electrophysiol. 2014, 25, 875–881. [Google Scholar] [CrossRef]
- Kumar, S.; Barbhaiya, C.; Nagashima, K.; Choi, E.K.; Epstein, L.M.; John, R.M.; Maytin, M.; Albert, C.M.; Miller, A.L.; Koplan, B.A.; et al. Ventricular tachycardia in cardiac sarcoidosis: Characterization of ventricular substrate and outcomes of catheter ablation. Circ. Arrhythm. Electrophysiol. 2018, 8, 87–93. [Google Scholar] [CrossRef] [Green Version]
- Segawa, M.; Fukuda, K.; Nakano, M.; Kondo, M.; Satake, H.; Hirano, M.; Shimokawa, H. Time course and factors correlated with ventricular tachyarrhythmias after the introduction of steroid therapy in cardiac sarcoidosis. Circ. Arrhytm. Electrophysiol. 2016, 9, e003353. [Google Scholar]
- Yazaki, Y.; Isobe, M.; Hiroe, M.; Morimoto, S.-I.; Hiramitsu, S.; Nakano, T.; Izumi, T.; Sekiguchi, M. Prognostic determinants of long-term survival in Japanese patients with cardiac sarcoidosis treated with prednisone. Am. J. Cardiol. 2001, 88, 1006–1010. [Google Scholar] [CrossRef]
- Ytakaya, Y.; Kusano, K.; Nishii, N. Early and frequent defibrillator discharge in patients with cardiac sarcoidosis compared to patients with idiopathic dilated cardiomyopathy. Int. J. Cardiol. 2017, 240, 302–306. [Google Scholar]
- Ho, J.; Chilvers, R.; Thillai, M. Cardiac sarcoidosis - an expert review for the chest physician. Expert. Rev. Respir. Med. 2019, 13, 507–520. [Google Scholar] [CrossRef]
- Ekström, K.; Lehtonen, J.; Nordenswan, H.-K.; Mäyränpää, M.I.; Räisänen-Sokolowski, A.; Kandolin, R.; Simonen, P.; Pietilä-Effati, P.; Alatalo, A.; Utriainen, S.; et al. Sudden death in cardiac sarcoidosis: An analysis of nationwide clinical and cause-of-death registries. Eur. Hear. J. 2019, 40, 3121–3128. [Google Scholar] [CrossRef] [PubMed]
- Fleming, H.A. Sarcoidosis of the heart. Am. J. Med. 1978, 64, 915–916. [Google Scholar] [CrossRef]
- Viles-Gonzales, J.F.; Pastori, L.; Fisher, A. Supraventricular arrhythmias in patients with cardiac sarcoidosis: Prevalence, predictors and clinical implications. Chest 2013, 143, 1085–1090. [Google Scholar] [CrossRef] [PubMed]
- Cain, M.A.; Metzl, M.D.; Patel, A.R.; Addetia, K.; Spencer, K.T.; Sweiss, N.J.; Beshai, J.F. Cardiac Sarcoidosis Detected by Late Gadolinium Enhancement and Prevalence of Atrial Arrhythmias. Am. J. Cardiol. 2014, 113, 1556–1560. [Google Scholar] [CrossRef]
- Kandolin, R.; Lehtonen, J.; Airaksinen, J.K.; Vihinen, T.; Miettinen, H.; Kaikkonen, K.S.; Haataja, P.; Kerola, T.; Kupari, M. Usefulness of Cardiac Troponins as Markers of Early Treatment Response in Cardiac Sarcoidosis. Am. J. Cardiol. 2015, 116, 960–964. [Google Scholar] [CrossRef]
- Ungprasert, P.; Crowson, C.S.; Matteson, E.L. Risk of cardiovascular disease among patients with sarcoidosis: A population-based retrospective cohort study, 1976–2013. Eur. Respir. J. 2017, 49, 1601. [Google Scholar]
- Ward, E.V.; Nazarim Edelman, R.R. Coronary artery vasculitis as a presentation of cardiac sarcoidosis. Circulation 2012, 125, e344–e346. [Google Scholar] [CrossRef] [Green Version]
- Guideline for Diagnosis of Cardiac Sarcoidosis. Study Report on Diffuse Pulmonary Diseases; Ministry of Health, Labour and Welfare: Tokyo, Japan, 1993; pp. 23–24. [Google Scholar]
- Hulten, E.; Agarwal, V.; Cahill, M.; Cole, G.; Vita, T.; Parrish, S.; Bittencourt, M.S.; Murthy, V.L.; Kwong, R.; di Carli, M.F.; et al. Presence of late gadolinium enhancement by cardiac magnetic resonance among patients with suspected cardiac sarcoidosis is associated with adverse cardiovascular prognosis: A systematic review and meta-analysis. Circ. Cardiovasc. Imaging 2016, 9, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Smedema, J.-P.; Snoep, G.; van Kroonenburgh, M.P.; van Geuns, R.-J.; Dassen, W.R.; Gorgels, A.P.; Crijns, H.J. Evaluation of the Accuracy of Gadolinium-Enhanced Cardiovascular Magnetic Resonance in the Diagnosis of Cardiac Sarcoidosis. J. Am. Coll. Cardiol. 2005, 45, 1683–1690. [Google Scholar] [CrossRef] [Green Version]
- Hamzeh, N.Y.; Wamboldt, F.S.; Weinberger, H.D. Management of Cardiac Sarcoidosis in the United States: A Delphi Study. Chest 2012, 141, 154–162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tchernev, G.; Chokoeva, A.A.; Schiavone, C.D.; Erme, A.M.; Tana, C.; Darling, M.; Kaley, J.; Gianfaldoni, S.; Wollina, U.; Lotti, T.; et al. Sarcoidosis exclusion criteria: The “simple truth” for a complicated diagnosis. J. Biol. Regul. Homeost. Agents 2015, 29 (Suppl. 1), 5–9. [Google Scholar]
- Larson, S.R.; Pieper, J.A.; Hulten, E.A.; Ficaro, E.P.; Corbett, J.R.; Murthy, V.L.; Weinberg, R.L. Characterization of a highly effective preparation for suppression of myocardial glucose utilization. J. Nucl. Cardiol. 2020, 27, 849–861. [Google Scholar] [CrossRef] [PubMed]
- Birnie, D.H.; Sauer, W.H.; Bogun, F.; Cooper, J.M.; Culver, D.A.; Duvernoy, C.S.; Judson, M.A.; Kron, J.; Mehta, D.; Nielsen, J.C.; et al. HRS Expert Consensus Statement on the Diagnosis and Management of Arrhythmias Associated With Cardiac Sarcoidosis. Hear. Rhythm. 2014, 11, 1304–1323. [Google Scholar] [CrossRef] [PubMed]
- Gasperetti, A.; Rossi, V.A.; Chiodini, A.; Casella, M.; Costa, S.; Akdis, D.; Büchel, R.; Deliniere, A.; Pruvot, E.; Gruner, C.; et al. Differentiating hereditary arrhythmogenic right ventricular cardiomyopathy from cardiac sarcoidosis fulfilling 2010 ARVC Task Force Criteria. Heart Rhythm. 2021, 18, 231–238. [Google Scholar] [CrossRef]
- Pontone, G.; Di Cesare, E.; Castelletti, S.; De Cobelli, F.; De Lazzari, M.; Esposito, A.; Focardi, M.; Di Renzi, P.; Indolfi, C.; Lanzillo, C.; et al. Appropriate use criteria for cardiovascular magnetic resonance imaging (CMR): SIC-SIRM position paper part 1 (ischemic and congenital heart diseases, cardio-oncology, cardiac masses and heart transplant). Radiol. Med. 2021, 126, 365–379. [Google Scholar] [CrossRef] [PubMed]
- Dubrey, S.W.; Grocott-Mason, R.; Mittal, T.K. Images in cardiology: Cardiac sarcoidosis with delayed enhanced MRI. Heart 2005, 91, 1185. [Google Scholar] [CrossRef] [Green Version]
- Dubrey, S.W.; Sharma, R.; Underwood, R.; Mittal, T. Cardiac sarcoidosis: Diagnosis and management. Postgrad. Med. J. 2015, 91, 384–394. [Google Scholar] [CrossRef]
- Tadamura, E.; Yamamuro, M.; Kubo, S.; Kanao, S.; Saga, T.; Harada, M.; Ohba, M.; Hosokawa, R.; Kimura, T.; Kita, T.; et al. Effectiveness of Delayed Enhanced MRI for Identification of Cardiac Sarcoidosis: Comparison with Radionuclide Imaging. Am. J. Roentgenol. 2005, 185, 110–115. [Google Scholar] [CrossRef]
- Greulich, S.; Deluigi, C.C.; Gloekler, S.; Wahl, A.; Zürn, C.; Kramer, U.; Nothnagel, D.; Bültel, H.; Schumm, J.; Grün, S.; et al. CMR Imaging Predicts Death and Other Adverse Events in Suspected Cardiac Sarcoidosis. JACC Cardiovasc. Imaging 2013, 6, 501–511. [Google Scholar] [CrossRef] [PubMed]
- Nagai, T.; Kohsaka, S.; Okuda, S.; Anzai, T.; Asano, K.; Fukuda, K. Incidence and Prognostic Significance of Myocardial Late Gadolinium Enhancement in Patients With Sarcoidosis Without Cardiac Manifestation. Chest 2014, 146, 1064–1072. [Google Scholar] [CrossRef]
- Sharma, S. Cardiac imaging in myocardial sarcoidosis and other cardiomyopathies. Curr. Opin. Pulm. Med. 2009, 15, 507–512. [Google Scholar] [CrossRef]
- Mantini, C.; Di Giammarco, G.; Pizzicannella, J.; Gallina, S.; Ricci, F.; D’Ugo, E.; Marchetti, M.; Cotroneo, A.R.; Ahmed, N.; Bucciarelli-Ducci, C.; et al. Grading of aortic stenosis severity: A head-to-head comparison between cardiac magnetic resonance imaging and echocardiography. Radiol. Med. 2018, 123, 643–654. [Google Scholar] [CrossRef] [Green Version]
- Ricci, F.; Aung, N.; Gallina, S.; Zemrak, F.; Fung, K.; Bisaccia, G.; Paiva, J.M.; Khanji, M.Y.; Mantini, C.; Palermi, S.; et al. Cardiovascular magnetic resonance reference values of mitral and tricuspid annular dimensions: The UK Biobank cohort. J. Cardiovasc. Magn. Reson. 2021, 23, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Mantini, C.; Mastrodicasa, D.; Bianco, F.; Bucciarelli, V.; Scarano, M.; Mannetta, G.; Gabrielli, D.; Gallina, S.; Petersen, S.E.; Ricci, F.; et al. Prevalence and Clinical Relevance of Extracardiac Findings in Cardiovascular Magnetic Resonance Imaging. J. Thorac. Imaging 2019, 34, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Slart, R.H.; Glaudemans, A.W.; Lancellotti, P.; Hyafil, F.; Blankstein, R.; Schwartz, R.G.; Document Reading Group. A joint procedural position statement on imaging in cardiac sarcoidosis: From the Cardiovascular and Inflammation & Infection Committees of the European Association of Nuclear Medicine, the European Association of Cardiovascular Imaging, and the American Society of Nuclear Cardiology. J. Nucl. Cardiol. 2018, 25, 298–319. [Google Scholar] [PubMed] [Green Version]
- Tana, C. FDG-PET Imaging in Sarcoidosis. Curr. Med. Imaging Rev. 2019, 15, 2–3. [Google Scholar] [CrossRef]
- Pellegrino, D.; Bonab, A.A.; Dragotakes, S.C.; Pitman, J.T.; Mariani, G.; Carter, E.A. Inflammation and infection: Imaging properties of 18F-FDG-labeled white blood cells versus 18F-FDG. J. Nucl. Med. 2005, 46, 1522–1530. [Google Scholar]
- Osborne, M.T.; Hulten, E.A.; Murthy, V.L.; Skali, H.; Taqueti, V.R.; Dorbala, S.; DiCarli, M.F.; Blankstein, R. Patient preparation for cardiac fluorine-18 fluorodeoxyglucose positron emission tomography imaging of inflammation. J. Nucl. Cardiol. 2017, 24, 86–99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manabe, O.; Yoshinaga, K.; Ohira, H.; Masuda, A.; Sato, T.; Tsujino, I.; Yamada, A.; Oya-ma-Manabe, N.; Hirata, K.; Nishimura, M.; et al. The effects of 18-h fasting with low-carbohydrate diet preparation on suppressed physiological myocardial (18)F-fluorodeoxyglucose (FDG) uptake and possible minimal effects of unfractionated heparin use in patients with suspected cardiac involvement sarcoidosis. J. Nucl. Cardiol. 2016, 23, 244–252. [Google Scholar] [CrossRef] [Green Version]
- Christopoulos, G.; Jouni, H.; Acharya, G.A.; Blauwet, L.A.; Kapa, S.; Bois, J.; Chareonthaitawee, P.; Rodriguez-Porcel, M.G. Suppressing physiologic 18-fluorodeoxyglucose uptake in patients undergoing positron emission tomography for cardiac sarcoidosis: The effect of a structured patient preparation protocol. J. Nucl. Cardiol. 2019, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, R.; Trivieri, M.; Fayad, Z.A.; Ahmadi, A.; Narula, J.; Argulian, E. Advanced Imaging in Cardiac Sarcoidosis. J. Nucl. Med. 2019, 60, 892–898. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.-J.; Pak, K.; Kim, K. Diagnostic performance of F-18 FDG PET for detection of cardiac sarcoidosis: A systematic review and meta-analysis. J. Nucl. Cardiol. 2020, 27, 2103–2115. [Google Scholar] [CrossRef] [PubMed]
- Sgard, B.; Brillet, P.Y.; Bouvry, D.; Djelbani, S.; Nunes, H.; Meune, C. Valutazione della PET FDG combinata con MRI cardiaca per la diagnosi e il monitoraggio terapeutico della sarcoidosi cardiaca. Radiol. Clin. 2019, 74, 661–671. [Google Scholar] [CrossRef] [PubMed]
- Manabe, O.; Ohira, H.; Hirata, K.; Hayashi, S.; Naya, M.; Tsujino, I.; Aikawa, T.; Koyanagawa, K.; Oyama-Manabe, N.; Tomiyama, Y.; et al. Use of 18F-FDG PET/CT texture analysis to diagnose cardiac sarcoidosis. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 1240–1247. [Google Scholar] [CrossRef]
- Youssef, G.; Leung, E.; Mylonas, I.; Nery, P.; Williams, K.; Wisenberg, G.; Gulenchyn, K.Y.; Dekemp, R.A.; DaSilva, J.; Birnie, D.; et al. The Use of 18F-FDG PET in the Diagnosis of Cardiac Sarcoidosis: A Systematic Review and Metaanalysis Including the Ontario Experience. J. Nucl. Med. 2012, 53, 241–248. [Google Scholar] [CrossRef] [Green Version]
- Manabe, O.; Koyanagawa, K.; Hirata, K.; Oyama-Manabe, N.; Ohira, H.; Aikawa, T.; Fu-ruya, S.; Naya, M.; Tsujino, I.; Tomiyama, Y.; et al. Prognostic Value of 18F-FDG PET Using Texture Analysis in Cardiac Sarcoidosis. JACC Cardiovasc. Im-aging 2020, 13, 1096–1097. [Google Scholar] [CrossRef]
- Furuya, S.; Manabe, O.; Ohira, H.; Hirata, K.; Aikawa, T.; Naya, M.; Tsujino, I.; Koyanaga-wa, K.; Anzai, T.; Oyama-Manabe, N.; et al. Which is the proper reference tissue for measuring the change in FDG PET metabolic volume of cardiac sarcoidosis before and after steroid therapy? EJNMMI Res. 2018, 8, 94. [Google Scholar] [CrossRef]
- Kim, R.J.; Fieno, D.S.; Parrish, T.B.; Harris, K.; Chen, E.-L.; Simonetti, O.; Bundy, J.; Finn, J.P.; Klocke, F.J.; Judd, R.M. Relationship of MRI Delayed Contrast Enhancement to Irreversible Injury, Infarct Age, and Contractile Function. Circlation 1999, 100, 1992–2002. [Google Scholar] [CrossRef] [Green Version]
- Bogaert, J.; Taylor, A.M.; Van Kerkhove, F.; Dymarkowski, S. Use of Inversion Recovery Contrast-Enhanced MRI for Cardiac Imaging:Spectrum of Applications. Am. J. Roentgenol. 2004, 182, 609–615. [Google Scholar] [CrossRef] [Green Version]
- Farber, G.; Boczar, K.; Wiefels, C.; Zelt, J.; Guler, E.C.; DeKemp, R.A. The Future of Cardiac Molecular Imaging. Semin. Nucl. Med. 2020, 50, 367–385. [Google Scholar] [CrossRef] [PubMed]
- Furuya, S.; Naya, M.; Manabe, O.; Hirata, K.; Ohira, H.; Aikawa, T.; Koyanagawa, K.; Magota, K.; Tsujino, I.; Anzai, T.; et al. 18F-FMISO PET/CT detects hypoxic lesions of cardiac and extra-cardiac involvement in patients with sarcoidosis. J. Nucl. Cardiol. 2019. [Google Scholar] [CrossRef] [PubMed]
- Vita, T.; Okada, D.R.; Veillet-Chowdhury, M.; Bravo, P.E.; Mullins, E.; Hulten, E.; Agrawal, M.; Madan, R.; Taqueti, V.R.; Steigner, M.; et al. Complementary Value of Cardiac Magnetic Resonance Imaging and Positron Emission Tomography/Computed Tomography in the Assessment of Cardiac Sarcoidosis. Circ. Cardiovasc. Imaging 2018, 11, e007030. [Google Scholar] [CrossRef] [PubMed]
- Wicks, E.C.; Menezes, L.J.; Barnes, A.; Mohiddin, S.A.; Sekhri, N.; Porter, J.C.; Booth, H.L.; Garrett, E.; Patel, R.S.; Pavlou, M.; et al. Diagnostic accuracy and prognostic value of simultaneous hybrid 18F-fluorodeoxyglucose positron emission tomography/magnetic resonance imaging in cardiac sarcoidosis. Eur. Hear. J.—Cardiovasc. Imaging 2018, 19, 757–767. [Google Scholar] [CrossRef] [PubMed]
- Togo, R.; Hirata, K.; Manabe, O.; Ohira, H.; Tsujino, I.; Magota, K.; Ogawa, T.; Haseyama, M.; Shiga, T. Cardiac sarcoidosis classification with deep convolutional neural net-work-based features using polar maps. Comput. Biol. Med. 2019, 104, 81–86. [Google Scholar] [CrossRef] [Green Version]
- Nappi, C.; El Fakhri, G. State of the Art in Cardiac Hybrid Technology: PET/MR. Curr. Cardiovasc. Imaging Rep. 2013, 6, 338–345. [Google Scholar] [CrossRef] [Green Version]
- Dubrey, S.W.; Falk, R.H. Diagnosis and Management of Cardiac Sarcoidosis. Prog. Cardiovasc. Dis. 2010, 52, 336–346. [Google Scholar] [CrossRef] [PubMed]
- Chapelon-Abric, C. Cardiac sarcoidosis. Curr. Opin. Pulm. Med. 2013, 19, 493–502. [Google Scholar] [CrossRef] [PubMed]
- Tana, C.; Mantini, C.; Cipollone, F.; Giamberardino, M.A. Chest Imaging of Patients with Sarcoidosis and SARS-CoV-2 Infection. Current Evidence and Clinical. Diagnostics 2021, 11, 183. [Google Scholar] [CrossRef]
- Tana, C.; Schiavone, C.; Ticinesi, A.; Ricci, F.; Giamberardino, M.A.; Cipollone, F.; Silingardi, M.; Meschi, T.; Dietrich, C.F. Ultrasound imaging of abdominal sarcoidosis: State of the art. World J. Clin. Cases 2019, 7, 809–818. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tana, C.; Mantini, C.; Donatiello, I.; Mucci, L.; Tana, M.; Ricci, F.; Cipollone, F.; Giamberardino, M.A. Clinical Features and Diagnosis of Cardiac Sarcoidosis. J. Clin. Med. 2021, 10, 1941. https://doi.org/10.3390/jcm10091941
Tana C, Mantini C, Donatiello I, Mucci L, Tana M, Ricci F, Cipollone F, Giamberardino MA. Clinical Features and Diagnosis of Cardiac Sarcoidosis. Journal of Clinical Medicine. 2021; 10(9):1941. https://doi.org/10.3390/jcm10091941
Chicago/Turabian StyleTana, Claudio, Cesare Mantini, Iginio Donatiello, Luciano Mucci, Marco Tana, Fabrizio Ricci, Francesco Cipollone, and Maria Adele Giamberardino. 2021. "Clinical Features and Diagnosis of Cardiac Sarcoidosis" Journal of Clinical Medicine 10, no. 9: 1941. https://doi.org/10.3390/jcm10091941
APA StyleTana, C., Mantini, C., Donatiello, I., Mucci, L., Tana, M., Ricci, F., Cipollone, F., & Giamberardino, M. A. (2021). Clinical Features and Diagnosis of Cardiac Sarcoidosis. Journal of Clinical Medicine, 10(9), 1941. https://doi.org/10.3390/jcm10091941










