Gender-Based Quantitative Analysis of the Grand Piano Sign in Mechanically Aligned Total Knee Arthroplasty in Asians
Abstract
1. Introduction
1.1. Background
1.2. Rationale
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Boldt, J.G.; Stiehl, J.B.; Hodler, J.; Zanetti, M.; Munzinger, U. Femoral component rotation and arthrofibrosis following mobile-bearing total knee arthroplasty. Int. Orthop. 2006, 30, 420–425. [Google Scholar] [CrossRef]
- Romero, J.; Stahelin, T.; Binkert, C.; Pfirrmann, C.; Hodler, J.; Kessler, O. The clinical consequences of flexion gap asymmetry in total knee arthroplasty. J. Arthroplast. 2007, 22, 235–240. [Google Scholar] [CrossRef]
- Anouchi, Y.S.; Whiteside, L.A.; Kaiser, A.D.; Milliano, M.T. The effects of axial rotational alignment of the femoral component on knee stability and patellar tracking in total knee arthroplasty demonstrated on autopsy specimens. Clin. Orthop. Relat. Res. 1993, 287, 170–177. [Google Scholar] [CrossRef]
- Whiteside, L.A.; Arima, J. The anteroposterior axis for femoral rotational alignment in valgus total knee arthroplasty. Clin. Orthop. Relat. Res. 1995, 321, 168–172. [Google Scholar] [CrossRef]
- Berger, R.A.; Crossett, L.S.; Jacobs, J.J.; Rubash, H.E. Malrotation causing patellofemoral complications after total knee arthroplasty. Clin. Orthop. Relat. Res. 1998, 356, 144–153. [Google Scholar] [CrossRef]
- Barrack, R.L.; Schrader, T.; Bertot, A.J.; Wolfe, M.W.; Myers, L. Component rotation and anterior knee pain after total knee arthroplasty. Clin. Orthop. Relat. Res. 2001, 392, 46–55. [Google Scholar] [CrossRef] [PubMed]
- Churchill, D.L.; Incavo, S.J.; Johnson, C.C.; Beynnon, B.D. The transepicondylar axis approximates the optimal flexion axis of the knee. Clin. Orthop. Relat. Res. 1998, 356, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Olcott, C.W.; Scott, R.D. A comparison of 4 intraoperative methods to determine femoral component rotation during total knee arthroplasty. J. Arthroplast. 2000, 15, 22–26. [Google Scholar] [CrossRef]
- Franceschini, V.; Nodzo, S.R.; Gonzalez Della Valle, A. Femoral Component Rotation in Total Knee Arthroplasty: A Comparison Between Transepicondylar Axis and Posterior Condylar Line Referencing. J. Arthroplast. 2016, 31, 2917–2921. [Google Scholar] [CrossRef] [PubMed]
- Stoeckl, B.; Nogler, M.; Krismer, M.; Beimel, C.; de la Barrera, J.L.; Kessler, O. Reliability of the transepicondylar axis as an anatomical landmark in total knee arthroplasty. J. Arthroplast. 2006, 21, 878–882. [Google Scholar] [CrossRef]
- Wai Hung, C.L.; Wai Pan, Y.; Kwong Yuen, C.; Hon Bong, L.; Lei Sha, L.W.; Ho Man, S.W. Interobserver and intraobserver error in distal femur transepicondylar axis measurement with computed tomography. J. Arthroplast. 2009, 24, 96–100. [Google Scholar] [CrossRef]
- Yoshino, N.; Takai, S.; Ohtsuki, Y.; Hirasawa, Y. Computed tomography measurement of the surgical and clinical transepicondylar axis of the distal femur in osteoarthritic knees. J. Arthroplast. 2001, 16, 493–497. [Google Scholar] [CrossRef] [PubMed]
- Cui, W.Q.; Won, Y.Y.; Baek, M.H.; Kim, K.K.; Cho, J.H. Variations of the ’grand-piano sign’ during total knee replacement. A computer-simulation study. J. Bone Jt. Surg. Br. 2006, 88, 1441–1447. [Google Scholar] [CrossRef] [PubMed]
- Conley, S.; Rosenberg, A.; Crowninshield, R. The female knee: Anatomic variations. J. Am. Acad. Orthop. Surg. 2007, 15, S31–S36. [Google Scholar] [CrossRef] [PubMed]
- Yue, B.; Varadarajan, K.M.; Ai, S.; Tang, T.; Rubash, H.E.; Li, G. Gender differences in the knees of Chinese population. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 80–88. [Google Scholar] [CrossRef]
- Gillespie, R.J.; Levine, A.; Fitzgerald, S.J.; Kolaczko, J.; DeMaio, M.; Marcus, R.E.; Cooperman, D.R. Gender differences in the anatomy of the distal femur. J. Bone Jt. Surg. Br. 2011, 93, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Li, K.; Langdale, E.; Tashman, S.; Harner, C.; Zhang, X. Gender and condylar differences in distal femur morphometry clarified by automated computer analyses. J. Orthop. Res. 2012, 30, 686–692. [Google Scholar] [CrossRef]
- Lim, H.C.; Bae, J.H.; Yoon, J.Y.; Kim, S.J.; Kim, J.G.; Lee, J.M. Gender differences of the morphology of the distal femur and proximal tibia in a Korean population. Knee 2013, 20, 26–30. [Google Scholar] [CrossRef]
- Yang, B.; Yu, J.K.; Zheng, Z.Z.; Lu, Z.H.; Zhang, J.Y. Comparative study of sex differences in distal femur morphology in osteoarthritic knees in a Chinese population. PLoS ONE 2014, 9, e89394. [Google Scholar] [CrossRef]
- Li, K.; Cavaignac, E.; Xu, W.; Cheng, Q.; Telmon, N.; Huang, W. Morphometric evaluation of the knee in Chinese population reveals sexual dimorphism and age-related differences. Int. Orthop. 2018, 42, 2349–2356. [Google Scholar] [CrossRef]
- Koh, Y.G.; Nam, J.H.; Chung, H.S.; Kim, H.J.; Chun, H.J.; Kang, K.T. Gender differences in morphology exist in posterior condylar offsets of the knee in Korean population. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1628–1634. [Google Scholar] [CrossRef] [PubMed]
- Koh, Y.G.; Nam, J.H.; Chung, H.S.; Lee, H.Y.; Kim, H.J.; Kim, H.J.; Kang, K.T. Gender-related morphological differences in sulcus angle and condylar height for the femoral trochlea using magnetic resonance imaging. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 3560–3566. [Google Scholar] [CrossRef] [PubMed]
- Nunley, R.M.; Ellison, B.S.; Zhu, J.; Ruh, E.L.; Howell, S.M.; Barrack, R.L. Do patient-specific guides improve coronal alignment in total knee arthroplasty? Clin. Orthop. Relat. Res. 2012, 470, 895–902. [Google Scholar] [CrossRef] [PubMed]
- Brooks, P. Seven cuts to the perfect total knee. Orthopedics 2009, 32, e1000642. [Google Scholar] [CrossRef] [PubMed]
- Ko, J.H.; Han, C.D.; Shin, K.H.; Nguku, L.; Yang, I.H.; Lee, W.S.; Kim, K.I.; Park, K.K. Femur bowing could be a risk factor for implant flexion in conventional total knee arthroplasty and notching in navigated total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 2476–2482. [Google Scholar] [CrossRef]
- Kim, J.T.; Han, J.; Shen, Q.H.; Moon, S.W.; Won, Y.Y. Morphological patterns of anterior femoral condylar resection in kinematically and mechanically aligned total knee arthroplasty. J. Arthroplast. 2018, 33, 2506–2511. [Google Scholar] [CrossRef]
- Ohmori, T.; Kabata, T.; Kajino, Y.; Taga, T.; Hasegawa, K.; Inoue, D.; Yamamoto, T.; Takagi, T.; Yoshitani, J.; Ueno, T.; et al. The accuracy of the “projected surgical transepicondylar axis” relative to the “true surgical transepicondylar axis” in total knee arthroplasty. Knee 2017, 24, 1428–1434. [Google Scholar] [CrossRef]
- Cohen, D.A.; Gursel, A.C.; Low, A.K. How coronal alignment affects distal femoral anatomy: An MRI-based comparison of varus and valgus knees. J. Orthop. Surg. Res. 2019, 14, 92. [Google Scholar] [CrossRef] [PubMed]
- Dimitriou, D.; Zou, D.; Wang, Z.; Helmy, N.; Tsai, T.Y. Anterior cruciate ligament bundle insertions vary between ACL-rupture and non-injured knees. Knee Surg. Sports Traumatol. Arthrosc. 2020, 29, 1164–1172. [Google Scholar] [CrossRef] [PubMed]
- Hoshino, Y.; Kuroda, R.; Nishizawa, Y.; Nakano, N.; Nagai, K.; Araki, D.; Oka, S.; Kawaguchi, S.; Nagamune, K.; Kurosaka, M. Stress distribution is deviated around the aperture of the femoral tunnel in the anatomic anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 1145–1151. [Google Scholar] [CrossRef]
- Krych, A.J.; Johnson, N.R.; Mohan, R.; Dahm, D.L.; Levy, B.A.; Stuart, M.J. Partial meniscectomy provides no benefit for symptomatic degenerative medial meniscus posterior root tears. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 1117–1122. [Google Scholar] [CrossRef]
- Poilvache, P.L.; Insall, J.N.; Scuderi, G.R.; Font-Rodriguez, D.E. Rotational landmarks and sizing of the distal femur in total knee arthroplasty. Clin. Orthop. Relat. Res. 1996, 331, 35–46. [Google Scholar] [CrossRef] [PubMed]
- Kang, K.T.; Koh, Y.G.; Son, J.; Kwon, O.R.; Park, K.K. Flexed femoral component improves kinematics and biomechanical effect in posterior stabilized total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1174–1181. [Google Scholar] [CrossRef] [PubMed]
- Jang, E.S.; Connors-Ehlert, R.; LiArno, S.; Geller, J.A.; Cooper, H.J.; Shah, R.P. Accuracy of reference axes for femoral component rotation in total knee arthroplasty: Computed tomography-based study of 2,128 femora. J. Bone Jt. Surg. Am. 2019, 101, e125. [Google Scholar] [CrossRef]
- Gurava Reddy, A.V.; Mathur, R.K.; Mugalur, A.; Eachempati, K.K.; Reddy, A. Reference axes for optimal femoral rotational alignment in varus osteoarthritic Indian knees—A CT based study. J. Clin. Orthop. Trauma 2016, 7, 215–219. [Google Scholar] [CrossRef] [PubMed]

| Parameter | All Patients (n = 267) | Women (n = 202) | Men (n = 65) | p-Value |
|---|---|---|---|---|
| Mean ± SD (range) | Mean ± SD (range) | Mean ± SD (range) | ||
| Age | 70.9 ± 6.5 (54, 85) | 71.3 ± 6.6 (58, 85) | 69.9 ± 6.1 (58, 85) | n.s |
| BMI | 23.2 ± 3.9 (15.9, 39.7) | 23.0 ± 4.1 (16.6, 39.7) | 23.5 ± 3.5 (15.9, 33.2) | n.s |
| Varus/Valgus | 251/16 | 190/12 | 61/4 | NA |
| Parameter | All Patients (n = 267) | Women (n = 202) | Men (n = 65) | p-Value |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | ||
| sTEA | 0.63 ± 0.11 | 0.65 ± 0.11 | 0.58 ± 0.08 | <0.001 |
| WSL | 0.60 ± 0.11 | 0.61 ± 0.12 | 0.58 ± 0.09 | <0.05 |
| FEA | 0.70 ± 0.14 | 0.70 ± 0.14 | 0.70 ± 0.14 | 0.86 |
| Rotational References | p-Value (ANOVA) | Comparison | |||
|---|---|---|---|---|---|
| sTEA | WSL | FEA | |||
| All subjects | 0.63 ± 0.11 | 0.60 ± 0.11 | 0.70 ± 0.14 | <0.001 | FEA > sTEA = WSL |
| Female | 0.65 ± 0.10 | 0.61 ± 0.12 | 0.70 ± 0.14 | <0.001 | FEA > sTEA > WSL |
| Male | 0.58 ± 0.08 | 0.58 ± 0.09 | 0.70 ± 0.14 | <0.001 | FEA > sTEA = WSL |
| Parameter | All Patients (n = 267) | Women (n = 202) | Men (n = 65) | p-Value |
|---|---|---|---|---|
| Mean ± SD (range) | Mean ± SD (range) | Mean ± SD (range) | ||
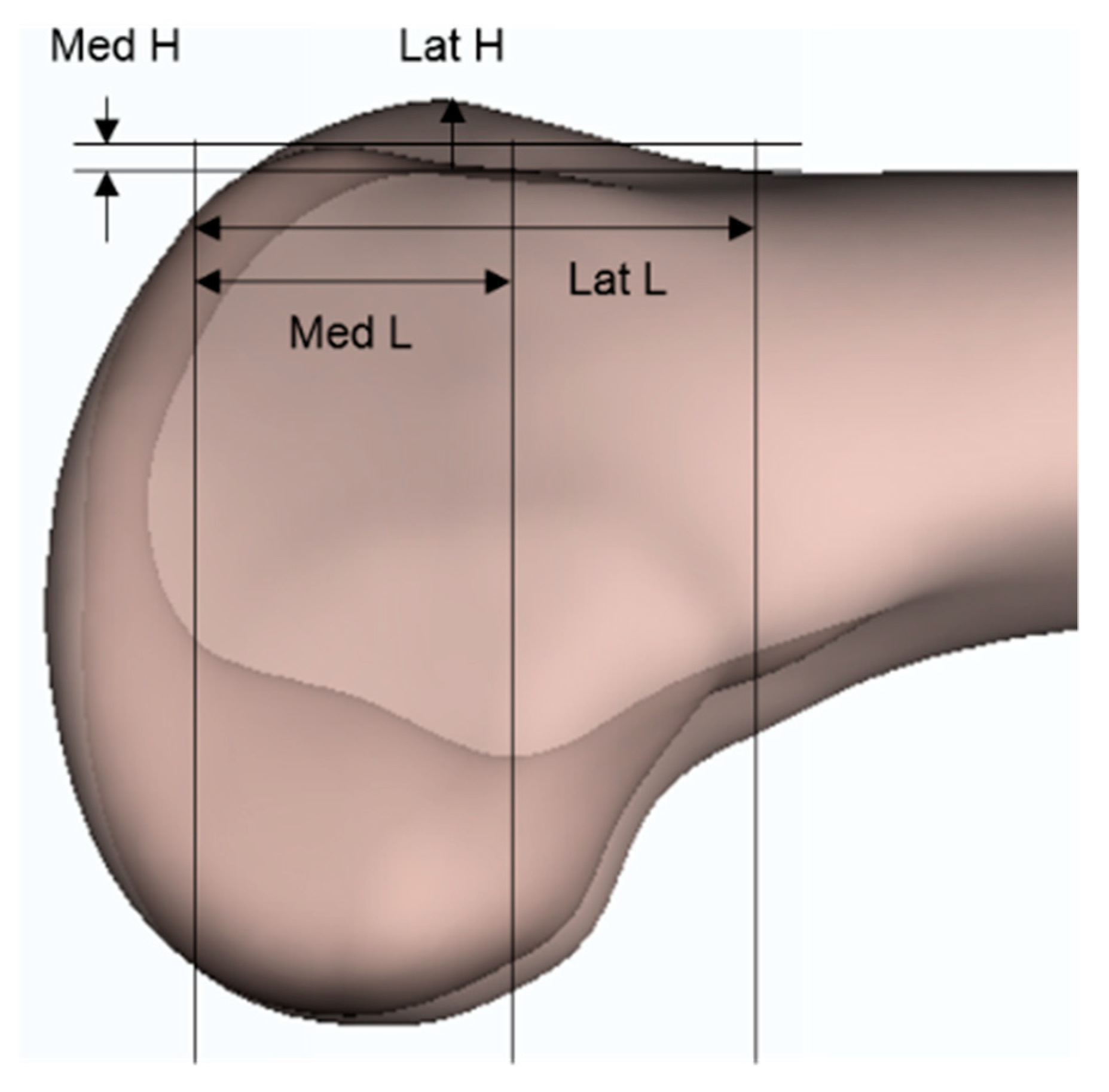
| ML (mm) | 75.6 ± 5.9 (65.4,91.3) | 72.9 ± 3.1 (65.4,83.3) | 84 ± 4.2 (68.8,91.3) | <0.001 |
| M′L′ (mm) | 46.9 ± 4.3 (38.2,66.5) | 45.6 ± 3.2 (38.2,56.3) | 51.1 ± 4.7 (43.1,66.5) | <0.001 |
| M′L′/ML (%) | 62.1 ± 3.9 (53.5,77.4) | 62.5 ± 3.6 (53.5,77.4) | 60.8 ± 4.5 (53.7,75.6) | <0.01 |
| LD | 5.3 ± 1.7 (−1.9,11.7) | 5.1 ± 1.6 (1.3,9.9) | 5.9 ± 2 (−1.9,11.7) | <0.01 |
| LD/ML (%) | 7.0 ± 2.1 (−2.1,13.2) | 7.0 ± 2 (1.8,13.2) | 7.0 ± 2.2 (−2.1,12.8) | 0.93 |
| Double peak type/Single peak type | 151/115 | 119/83 | 32/33 | 0.196 |
| Study | Population | Men | Women | ||||
|---|---|---|---|---|---|---|---|
| Lateral | Medial | Ratio (M/L) | Lateral | Medial | Ratio (M/L) | ||
| Koh et al. [22] 1 | Korean | 8.3 | 6.7 | 0.81 | 6.7 | 6.1 | 0.91 |
| Yang et al. [19] 2 | Chinese | 8.2 | 3.1 | 0.38 | 7.4 | 3.6 | 0.49 |
| Poilvache et al. [32] 1 | Western | 13.74 | 10.63 | 0.77 | 12.26 | 8.96 | 0.73 |
| Zimmer® [33] 3 | Western | 10.9 | 6.4 | 0.59 | 10.1 | 5.1 | 0.50 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cho, B.-W.; Nam, J.-H.; Koh, Y.-G.; Min, J.-H.; Park, K.-K.; Kang, K.-T. Gender-Based Quantitative Analysis of the Grand Piano Sign in Mechanically Aligned Total Knee Arthroplasty in Asians. J. Clin. Med. 2021, 10, 1969. https://doi.org/10.3390/jcm10091969
Cho B-W, Nam J-H, Koh Y-G, Min J-H, Park K-K, Kang K-T. Gender-Based Quantitative Analysis of the Grand Piano Sign in Mechanically Aligned Total Knee Arthroplasty in Asians. Journal of Clinical Medicine. 2021; 10(9):1969. https://doi.org/10.3390/jcm10091969
Chicago/Turabian StyleCho, Byung-Woo, Ji-Hoon Nam, Yong-Gon Koh, Ji-Hwan Min, Kwan-Kyu Park, and Kyoung-Tak Kang. 2021. "Gender-Based Quantitative Analysis of the Grand Piano Sign in Mechanically Aligned Total Knee Arthroplasty in Asians" Journal of Clinical Medicine 10, no. 9: 1969. https://doi.org/10.3390/jcm10091969
APA StyleCho, B.-W., Nam, J.-H., Koh, Y.-G., Min, J.-H., Park, K.-K., & Kang, K.-T. (2021). Gender-Based Quantitative Analysis of the Grand Piano Sign in Mechanically Aligned Total Knee Arthroplasty in Asians. Journal of Clinical Medicine, 10(9), 1969. https://doi.org/10.3390/jcm10091969






