Non-Surgical Strategies for Assisting Closure of Pharyngocutaneous Fistula after Total Laryngectomy: A Systematic Review of the Literature
Abstract
:1. Introduction
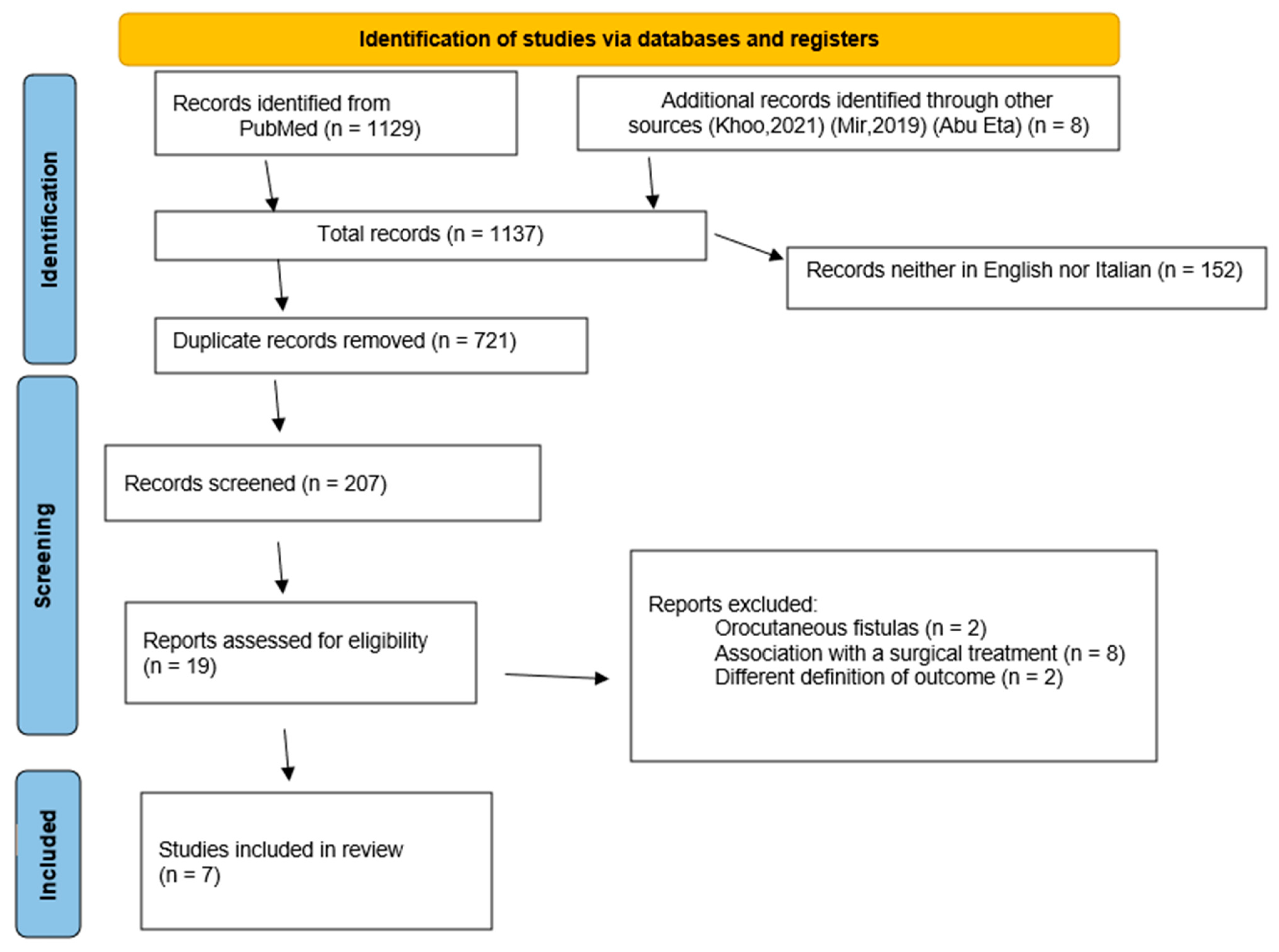
2. Materials and Methods
2.1. Literature Search
2.2. Data Collection
2.3. Definition of the Outcome and Statistical Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Paydarfar, J.A.; Birkmeyer, N.J. Complications in Head and Neck Surgery: A meta-analysis of postlaryngectomy pharyngocutaneous fistula. Arch. Otolaryngol. Head Neck Surg. 2006, 132, 67–72. [Google Scholar] [CrossRef] [Green Version]
- Cavalot, A.L.; Gervasio, C.F.; Nazionale, G.; Albera, R.; Bussi, M.; Staffieri, A.; Ferrero, V.; Cortesina, G. Pharyngocutaneous Fistula as a Complication of Total Laryngectomy: Review of the Literature and Analysis of Case Records. Otolaryngol. Neck Surg. 2000, 123, 587–592. [Google Scholar] [CrossRef] [PubMed]
- Kiong, K.L.; Tan, N.C.; Skanthakumar, T.; Teo, C.E.; Soo, K.C.; Tan, H.K.; Roche, E.; Yee, K.; Iyer, N.G. Salivary fistula: Blue dye testing as part of an algorithm for early diagnosis. Laryngoscope 2017, 2, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Friedman, M.; Venkatesan, T.K.; Yakovlev, A.; Lim, J.W.; Tanyeri, H.M.; Caldarelli, D.D. Early Detection and Treatment of Postoperative Pharyngocutaneous Fistula. Otolaryngol. Neck Surg. 1999, 121, 378–380. [Google Scholar] [CrossRef]
- Khoo, M.J.W.; Ooi, A.S.H. Management of postreconstructive head and neck salivary fistulae: A review of current practices. J. Plast. Reconstr. Aesthet. Surg. 2021, 74, 2120–2132. [Google Scholar] [CrossRef]
- Bomeli, S.R.; Desai, S.C.; Johnson, J.T.; Walvekar, R.R. Management of salivary flow in head and neck cancer patients—A systematic review. Oral Oncol. 2008, 44, 1000–1008. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [Green Version]
- Neovius, E.B.; Lind, M.G.; Lind, F.G. Hyperbaric oxygen therapy for wound complications after surgery in the irradiated head and neck: A review of the literature and a report of 15 consecutive patients. Head Neck 1997, 19, 315–322. [Google Scholar] [CrossRef]
- Abu Eta, R.; Eviatar, E.; Gavriel, H. Hyperbaric oxygen therapy as an alternative to surgery for non-healing pharyngocutaneous fistula. Eur. Arch. Oto-Rhino-Laryngol. 2016, 273, 3857–3861. [Google Scholar] [CrossRef]
- Andrews, B.T.; Smith, R.B.; Hoffman, H.T.; Funk, G.F. Orocutaneous and Pharyngocutaneous Fistula Closure Using a Vacuum-Assisted Closure System. Ann. Otol. Rhinol. Laryngol. 2008, 117, 298–302. [Google Scholar] [CrossRef] [PubMed]
- Loaec, E.; Vaillant, P.-Y.; Bonne, L.; Marianowski, R. Negative-pressure wound therapy for the treatment of pharyngocutaneous fistula. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2014, 131, 351–355. [Google Scholar] [CrossRef] [Green Version]
- Teixeira, S.; Costa, J.; Bartosch, I.; Correia, B.; Álvaro, S. Management of Pharyngocutaneous Fistula with Negative-Pressure Wound Therapy. J. Craniofac. Surg. 2017, 28, e364–e367. [Google Scholar] [CrossRef]
- Marchese, M.R.; Almadori, G.; Giorgio, A.; Paludetti, G. Post-surgical role of botulinum toxin-A injection in patients with head and neck cancer: Personal experience. Acta Otorhinolaryngol. Ital. 2008, 28, 13–16. [Google Scholar]
- Guntinas-Lichius, O.; Eckel, H.E. Temporary Reduction of Salivation in Laryngectomy Patients with Pharyngocutaneous Fistulas by Botulinum Toxin A Injection. Laryngoscope 2002, 112, 187–189. [Google Scholar] [CrossRef]
- Busoni, M.; Deganello, A.; Gallo, O. Fistola faringocutanea dopo laringectomia totale: Analisi dei fattori di rischio, della prognosi e delle modalità di trattamento. Acta Otorhinolaryngol. Ital. 2015, 35, 400–405. [Google Scholar] [CrossRef] [PubMed]
- Sayles, M.; Grant, D.G. Preventing pharyngo-cutaneous fistula in total laryngectomy: A systematic review and meta-analysis. Laryngoscope 2014, 124, 1150–1163. [Google Scholar] [CrossRef]
- Nesemeier, R.; Dunlap, N.; McClave, S.A.; Tennant, P. Evidence-Based Support for Nutrition Therapy in Head and Neck Cancer. Curr. Surg. Rep. 2017, 5, 18. [Google Scholar] [CrossRef]
- Guimarães, A.V.; Aires, F.T.; Dedivitis, R.A.; Kulcsar, M.A.V.; Ramos, D.M.; Cernea, C.R.; Brandão, L.G. Efficacy of pectoralis major muscle flap for pharyngocutaneous fistula prevention in salvage total laryngectomy: A systematic review. Head Neck 2015, 38, E2317–E2321. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.; Karantanis, W.; Fadhil, M.; Dow, C.; Fuzi, J.; Robinson, R.; Jacobson, I. Meta-analysis on the rate of pharyngocutaneous fistula in early oral feeding in laryngectomy patients. Am. J. Otolaryngol. 2021, 42, 102748. [Google Scholar] [CrossRef] [PubMed]
- Le Flem, M.; Santini, L.; Boulze, C.; Alshukry, A.; Giovanni, A.; Dessi, P.; Fakhry, N. Early oral hydration protects against pharyngocutaneous fistula after total laryngectomy or total pharyngolaryngectomy. Head Neck 2020, 42, 1902–1906. [Google Scholar] [CrossRef]
- Crosetti, E.; Arrigoni, G.; Sprio, A.E.; Succo, G. “Fistula Zero” Project After Total Laryngectomy: The Candiolo Cancer Institute Experience. Front. Oncol. 2021, 11, 690703. [Google Scholar] [CrossRef]
- Morton, R.P.; Mehanna, H.; Hall, F.T.; McIvor, N.P. Prediction of pharyngocutaneous fistulas after laryngectomy. Otolaryngol. Neck Surg. 2007, 136, s46–s49. [Google Scholar] [CrossRef]
- De Zinis, L.O.R.; Ferrari, L.; Tomenzoli, D.; Premoli, G.; Parrinello, G.; Nicolai, P. Postlaryngectomy pharyngocutaneous fistula: Incidence, predisposing factors, and therapy. Head Neck 1999, 21, 131–138. [Google Scholar] [CrossRef]
- Mäkitie, A.A.; Irish, J.; Gullane, P.J. Pharyngocutaneous fistula. Curr. Opin. Otolaryngol. Head Neck Surg. 2003, 11, 78–84. [Google Scholar] [CrossRef]
- Powitzky, R.; Vasan, N.; Krempl, G.; Medina, J. Carotid Blowout in Patients with Head and Neck Cancer. Ann. Otol. Rhinol. Laryngol. 2010, 119, 476–484. [Google Scholar] [CrossRef] [PubMed]
- Davies, J.C.; Hugh, S.; Rich, J.T.; de Almeida, J.R.; Gullane, P.J.; Orsini, M.; Eskander, A.; Monteiro, E.; Mimica, X.; McGill, M.; et al. Association of Pharyngocutaneous Fistula with Cancer Outcomes in Patients After Laryngectomy. JAMA Otolaryngol. Neck Surg. 2021, 47, 1027–1034. [Google Scholar] [CrossRef] [PubMed]
- Tandara, A.A.; Mustoe, T.A. Oxygen in Wound Healing—More than a Nutrient. World J. Surg. 2004, 28, 294–300. [Google Scholar] [CrossRef]
- Tibbles, P.M.; Edelsberg, J.S. Hyperbaric-Oxygen Therapy. N. Engl. J. Med. 1996, 334, 1642–1648. [Google Scholar] [CrossRef]
- Wang, C.; Schwaitzberg, S.; Berliner, E.; Zarin, D.A.; Lau, J. Hyperbaric Oxygen for Treating Wounds. Arch. Surg. 2003, 138, 272–279. [Google Scholar] [CrossRef] [Green Version]
- Marx, R.E.; Ehler, W.J.; Tayapongsak, P.; Pierce, L.W. Relationship of oxygen dose to angiogenesis induction in irradiated tissue. Am. J. Surg. 1990, 160, 519–524. [Google Scholar] [CrossRef]
- Moen, I.; Stuhr, L.E.B. Hyperbaric oxygen therapy and cancer—A review. Target. Oncol. 2012, 7, 233–242. [Google Scholar] [CrossRef] [Green Version]
- Mir, A.; Guys, N.; Bs, K.A.; Svider, P.F.; Rayess, H.; Zuliani, G.; Raza, S.N.; Lin, H. Negative Pressure Wound Therapy in the Head and Neck: An Evidence-Based Approach. Laryngoscope 2019, 129, 671–683. [Google Scholar] [CrossRef] [PubMed]
- Rosenthal, E.L.; Blackwell, K.E.; McGrew, B.; Carroll, W.R.; Peters, G.E. Use of negative pressure dressings in head and neck reconstruction. Head Neck 2005, 27, 970–975. [Google Scholar] [CrossRef] [PubMed]
- Inatomi, Y.; Kadota, H.; Yoshida, S.; Kamizono, K.; Shimamoto, R.; Fukushima, S.; Miyashita, K.; Matsuo, M.; Yasumatsu, R.; Tanaka, S.; et al. Utility of negative-pressure wound therapy for orocutaneous and pharyngocutaneous fistula following head and neck surgery. Head Neck 2020, 42, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Asher, S.A.; White, H.N.; Illing, E.A.; Carroll, W.R.; Magnuson, J.S.; Rosenthal, E.L. Intraluminal Negative Pressure Wound Therapy for Optimizing Pharyngeal Reconstruction. JAMA Otolaryngol. Neck Surg. 2014, 140, 143–149. [Google Scholar] [CrossRef] [Green Version]
- Johnston, J.; Mariano, F.; Vokes, D. Negative pressure dressing around the airway. N. Z. Med. J. 2013, 126, 24045317. [Google Scholar]
- Yang, Y.-H.; Jeng, S.-F.; Hsieh, C.-H.; Feng, G.-M.; Chen, C.C. Vacuum-assisted closure for complicated wounds in head and neck region after reconstruction. J. Plast. Reconstr. Aesthet. Surg. 2013, 66, e209–e216. [Google Scholar] [CrossRef]
- Steinbichler, T.B.; Wolfram, D.; Runge, A.; Hartl, R.; Dejaco, D.; Rauchenwald, T.; Pototschnig, C.; Riechelmann, H.; Schartinger, V.H. Modified vacuum-assisted closure (EndoVAC) therapy for treatment of pharyngocutaneous fistula: A case series and a review of the literature. Head Neck 2021, 43, 2377–2384. [Google Scholar] [CrossRef]
- Waldie, K. Pain associated with negative pressure wound therapy. Br. J. Nurs. 2013, 22, S15–S21. [Google Scholar] [CrossRef] [PubMed]
- Reiter, M.; Harréus, U. Vacuum assisted closure in the management of wound healing disorders in the head and neck: A retrospective analysis of 23 cases. Am. J. Otolaryngol. 2013, 34, 411–415. [Google Scholar] [CrossRef] [PubMed]
- Braakenburg, A.; Obdeijn, M.C.; Feitz, R.; Van Rooij, I.A.L.M.; Van Griethuysen, A.J.; Klinkenbijl, J.H.G. The Clinical Efficacy and Cost Effectiveness of the Vacuum-Assisted Closure Technique in the Management of Acute and Chronic Wounds: A Randomized Controlled Trial. Plast. Reconstr. Surg. 2006, 118, 390–397. [Google Scholar] [CrossRef] [PubMed]
- Shehee, L.; O’Rourke, A.; Garand, K.L. The Role of Radiation Therapy and Botulinum Toxin Injections in the Management of Sialorrhea in Patients with Amyotrophic Lateral Sclerosis: A Systematic Review. J. Clin. Neuromuscul. Dis. 2020, 21, 205–221. [Google Scholar] [CrossRef]
- Ruiz-Roca, J.A.; Pons-Fuster, E.; Lopez-Jornet, P. Effectiveness of the Botulinum Toxin for Treating Sialorrhea in Patients with Parkinson’s Disease: A Systematic Review. J. Clin. Med. 2019, 8, 317. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ng, L.; Khan, F.; Young, C.A.; Galea, M. Symptomatic treatments for amyotrophic lateral sclerosis/motor neuron disease. Cochrane Database Syst. Rev. 2017, 2017, CD011776. [Google Scholar] [CrossRef]
- Walshe, M.; Smith, M.; Pennington, L. Interventions for drooling in children with cerebral palsy. Cochrane Database Syst. Rev. 2012, 11, CD008624. [Google Scholar] [CrossRef] [Green Version]
- Corradino, B.; Di Lorenzo, S.; Mossuto, C.; Costa, R.P.; Moschella, F. Botulinum toxin in preparation of oral cavity for microsurgical reconstruction. Acta Oto-Laryngol. 2010, 130, 156–160. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.; Lee, Y.; Park, H.; Lee, J.W.; Cha, W. Intraoperative botulinum toxin injection for superficial partial parotidectomy: A prospective pilot study. Clin. Otolaryngol. 2021, 46, 998–1004. [Google Scholar] [CrossRef]
- Corradino, B.; Di Lorenzo, S.; Moschella, F.; Bartolo, C.; Sara, D.L.; Francesco, M. Botulinum Toxin A for Oral Cavity Cancer Patients: In Microsurgical Patients BTX Injections in Major Salivary Glands Temporarily Reduce Salivary Production and the Risk of Local Complications Related to Saliva Stagnation. Toxins 2012, 4, 956–961. [Google Scholar] [CrossRef]
- Lewis, D.W.; Fontana, C.; Mehallick, L.K.; Everett, Y. Transdermal Scopolamine for Reduction Of Drooling In Developmentally Delayed Children. Dev. Med. Child Neurol. 2008, 36, 484–486. [Google Scholar] [CrossRef]
- Talmi, Y.P.; Zohar, Y.; Finkelstein, Y.; Laurian, N. Reduction of Salivary Flow with Scopoderm Tts. Ann. Otol. Rhinol. Laryngol. 1988, 97, 128–130. [Google Scholar] [CrossRef]
- Reid, S.M.; Westbury, C.; Guzys, A.T.; Reddihough, D.S. Anticholinergic medications for reducing drooling in children with developmental disability. Dev. Med. Child Neurol. 2020, 62, 346–353. [Google Scholar] [CrossRef] [PubMed]
- Varley, L.P.; Denieffe, S.; O’Gorman, C.; Murphy, A.; Gooney, M. A systematic review of noninvasive and invasive sialorrhoea management. J. Clin. Nurs. 2019, 28, 4190–4206. [Google Scholar] [CrossRef]
- Mantsopoulos, K.; Goncalves, M.; Iro, H. Transdermal scopolamine for the prevention of a salivary fistula after parotidectomy. Br. J. Oral Maxillofac. Surg. 2018, 56, 212–215. [Google Scholar] [CrossRef] [PubMed]
- Send, T.; Bertlich, M.; Eichhorn, K.W.; Bootz, F.; Jakob, M. Management and Follow-up Results of Salivary Fistulas Treated with Botulinum Toxin. Laryngoscope 2019, 129, 403–408. [Google Scholar] [CrossRef]
- Dessy, L.; Mazzocchi, M.; Monarca, C.; Onesti, M.; Scuderi, N. Combined transdermal scopolamine and botulinum toxin A to treat a parotid fistula after a face-lift in a patient with siliconomas. Int. J. Oral Maxillofac. Surg. 2007, 36, 949–952. [Google Scholar] [CrossRef]
- Suzuki, S.; Aihara, R.; Ooki, T.; Matsumura, N.; Wada, W.; Mogi, A.; Hosouchi, Y.; Nishida, Y.; Sakai, M.; Sohda, M.; et al. Successful treatment of enterocutaneous fistula after esophagectomy with scopolamine ointment and negative pressure wound therapy: A case report. Surg. Case Rep. 2020, 6, 177. [Google Scholar] [CrossRef]
- Wang, M.; Xun, Y.; Wang, K.; Lu, L.; Yu, A.; Guan, B.; Yu, C. Risk factors of pharyngocutaneous fistula after total laryngectomy: A systematic review and meta-analysis. Eur. Arch. Oto-Rhino-Laryngol. 2020, 277, 585–599. [Google Scholar] [CrossRef]
- Deganello, A.; Gallo, O.; De Cesare, J.M.; Ninu, M.B.; Gitti, G.; Campora, L.D.; Radici, M.; Campora, E.D. Supracricoid partial laryngectomy as salvage surgery for radiation therapy failure. Head Neck 2008, 30, 1064–1071. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alam, D.S.; Vivek, P.P.; Kmiecik, J. Comparison of voice outcomes after radial forearm free flap reconstruction versus primary closure after laryngectomy. Otolaryngol. Neck Surg. 2008, 139, 240–244. [Google Scholar] [CrossRef] [PubMed]
- Patel, U.A.; Keni, S.P. Pectoralis Myofascial Flap during Salvage Laryngectomy Prevents Pharyngocutaneous Fistula. Otolaryngol. Neck Surg. 2009, 141, 190–195. [Google Scholar] [CrossRef]
- Higgins, K.M.; Ashford, B.; Erovic, B.; Yoo, J.; Enepekides, D.J. Temporoparietal fascia free flap for pharyngeal coverage after salvage total laryngectomy. Laryngoscope 2011, 122, 523–527. [Google Scholar] [CrossRef] [PubMed]
- Frisch, T. Versatility of the facial artery myomucosal island flap in neopharyngeal reconstruction. Head Neck 2016, 39, E29–E33. [Google Scholar] [CrossRef] [PubMed]
- Microvascular Committee of the American Academy of Otolaryngology-Head & Neck Surgery. Salvage laryngectomy and laryngopharyngectomy: Multicenter review of outcomes associated with a reconstructive approach. Head Neck. 2019, 41, 16–29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steffen, A.; Hasselbacher, K.; Heinrichs, S.; Wollenberg, B. Botulinum toxin for salivary disorders in the treatment of head and neck cancer. Anticancer Res. 2014, 34, 6627–6632. [Google Scholar]
| Reference (Year, Country) | Study Type (Period) | N° of Cases (Sex) | Mean Age | Tumor Site | cTNM/ pTNM | Type of Surgery | Previous RT (Number of Patients) | Previous Surgical Treatment for Fistula Healing | Comorbidities | Time for Fistula Presentation (Days after Surgery) | Mean Time for Fistula Healing (Days) | Success Rate (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Neovius et al. (1997, Sweden) [8] | Retrospective (1993–1995) | 2 (2M/0F) | 58.5 | Laryngeal | T2-3 N0 M0 | NA | 2 | NA | NA | NA | 45 | 50% |
| R. Abu Eta et al. (2016, Israel) [9] | Retrospective (2008–2013) | 8 (8M/0F) | 63 | Glottic-supraglottic | T3-4 N0-2b M0 | 8 total laryngectomy + 6 PMF | 8 | 0 | 1 DMII 1 HNT 2 IHD 2 Dyslipidemia | 12.75 | 41.5 | 87.5% |
| Reference (Year, Country) | Study Type (Period) | N° of Cases (Sex) | Mean Age | Tumor Site | cTNM/ pTNM | Type of Surgery | Previous RT (Number of Patients) | Previous Surgical Treatments for Fistula Healing | Comorbidities | Time for Fistula Presentation (Days after Surgery) | Mean Time for Fistula Healing (Days) | Success Rate (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Andrews et al. (2008, USA) [10] | Case series (NA) | 1 (1M/0F) | 75 | larynx | T3-N0-M1 | Salvage + radial forearm reconstruction | 1 | 0 | NA | NA (dehiscence soon after the surgery) | 28 | 100% |
| Loaec et al. (France, 2014) [11] | Case series (2011–2013) | 5 (5M/0F) | 67.4 | Larynx-oropharynx | T3-4 N0-2 M0 | 1 total laryngectomy; 1 total circular pharyngolaryngectomy + RFFF; 2 partial laryngectomies, 1 transmandibular oropharyngectomy | 0 | 1 reoperation for Hematoma + debridement (NPWT for the recurrence of fistula) 1 RFFF | 1 COPD | 7.6 | 17.8 | 100% |
| Teixeira et al. (2017, Portugal) [12] | Case series (NA) | 2 (1M, 1F) | 64 | Pyriform sinus | pT3N0M0 | 2 total laryngectomies (+1 RFFF) | 1 | 1 PMF | 1DMII+, HNT obesity, splenectomy nephrectomy in the context of polyarteritis nodosa | NA | 22 | 100% |
| Reference (Year, Country) | Study Type (Period) | N° of Cases (Sex) | Mean Age | Tumor Site | cTNM/ pTNM | Type of Surgery | Previous RT (Number of Patients) | Surgical Treatment for Fistula Healing | Comorbidities | Time for Fistula Presentation (Days after Surgery) | Mean Time for Fistula Healing (Days) | Success Rate (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Marchese et al. (2008, Italy) [13] | Case series (2004–2006) | 6 (6M/0F) | 62.5 | Larynx-hypopharynx | NA | NA | 1 | 0 | NA | 7 | 6.7 | 100% |
| Guntinas-Lichius et al. (2002, Germany) [14] | Case series (NA) | 3 (3M/0F) | 58 | Larynx-oropharynx | rpT4 N2a-b M0 | 2 Laryngectomy + neck dissection; 1 Median mandibulotomy, tumor resection, radial forearm flap, neck dissection | 1 | 1 PMF (failed) | NA | 9.6 | 23.3 | 100% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Locatello, L.G.; Licci, G.; Maggiore, G.; Gallo, O. Non-Surgical Strategies for Assisting Closure of Pharyngocutaneous Fistula after Total Laryngectomy: A Systematic Review of the Literature. J. Clin. Med. 2022, 11, 100. https://doi.org/10.3390/jcm11010100
Locatello LG, Licci G, Maggiore G, Gallo O. Non-Surgical Strategies for Assisting Closure of Pharyngocutaneous Fistula after Total Laryngectomy: A Systematic Review of the Literature. Journal of Clinical Medicine. 2022; 11(1):100. https://doi.org/10.3390/jcm11010100
Chicago/Turabian StyleLocatello, Luca Giovanni, Giuseppe Licci, Giandomenico Maggiore, and Oreste Gallo. 2022. "Non-Surgical Strategies for Assisting Closure of Pharyngocutaneous Fistula after Total Laryngectomy: A Systematic Review of the Literature" Journal of Clinical Medicine 11, no. 1: 100. https://doi.org/10.3390/jcm11010100
APA StyleLocatello, L. G., Licci, G., Maggiore, G., & Gallo, O. (2022). Non-Surgical Strategies for Assisting Closure of Pharyngocutaneous Fistula after Total Laryngectomy: A Systematic Review of the Literature. Journal of Clinical Medicine, 11(1), 100. https://doi.org/10.3390/jcm11010100







