Intraoperative 3D Comparison of Round and Anatomical Breast Implants: Dispelling a Myth
Abstract
:1. Introduction
2. Materials and Methods
2.1. General Procedure
2.2. Implant Selection, 3D Scan, and Measurements
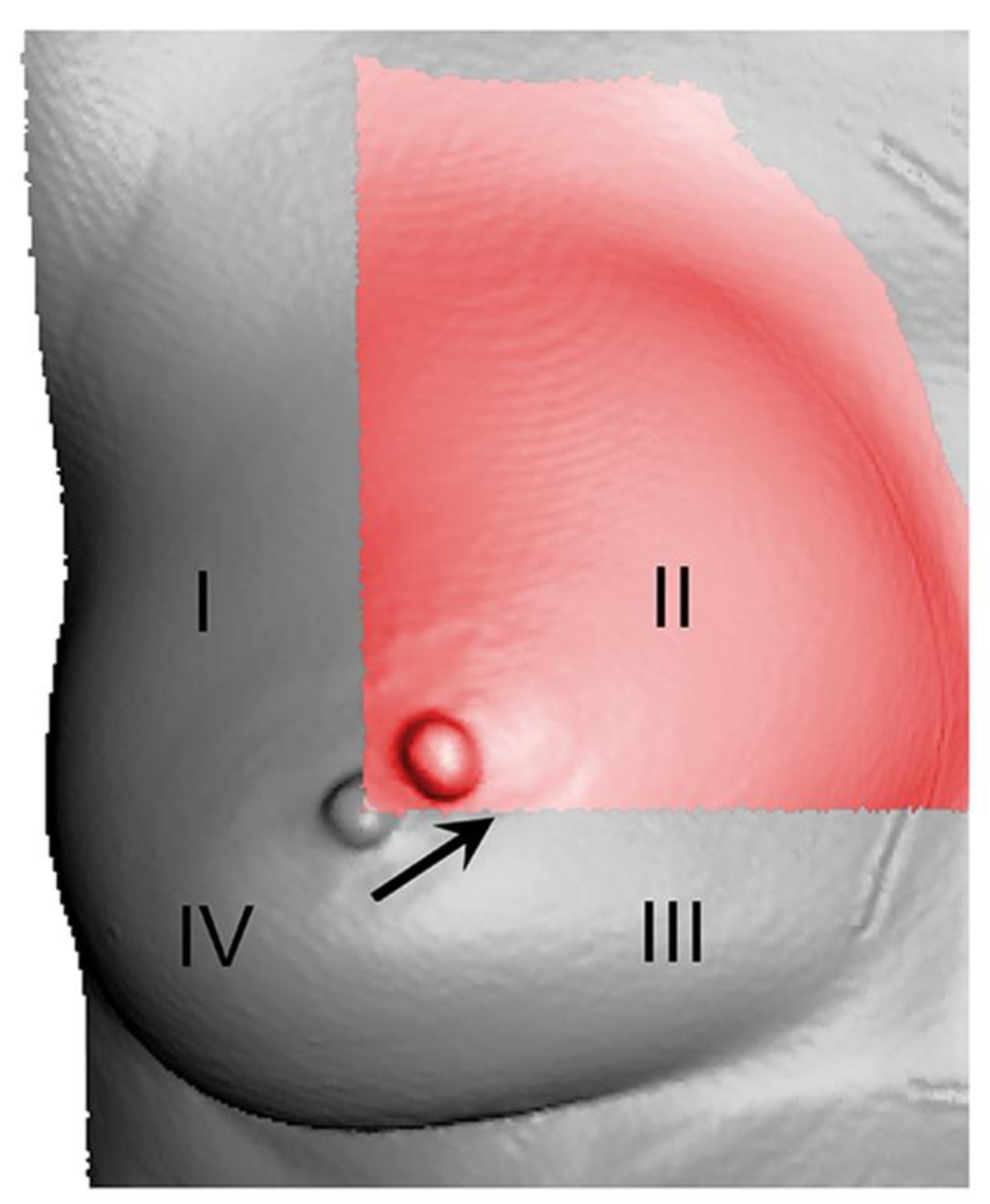
2.3. Topographic Shift (TS) over the Four Breast Quadrants
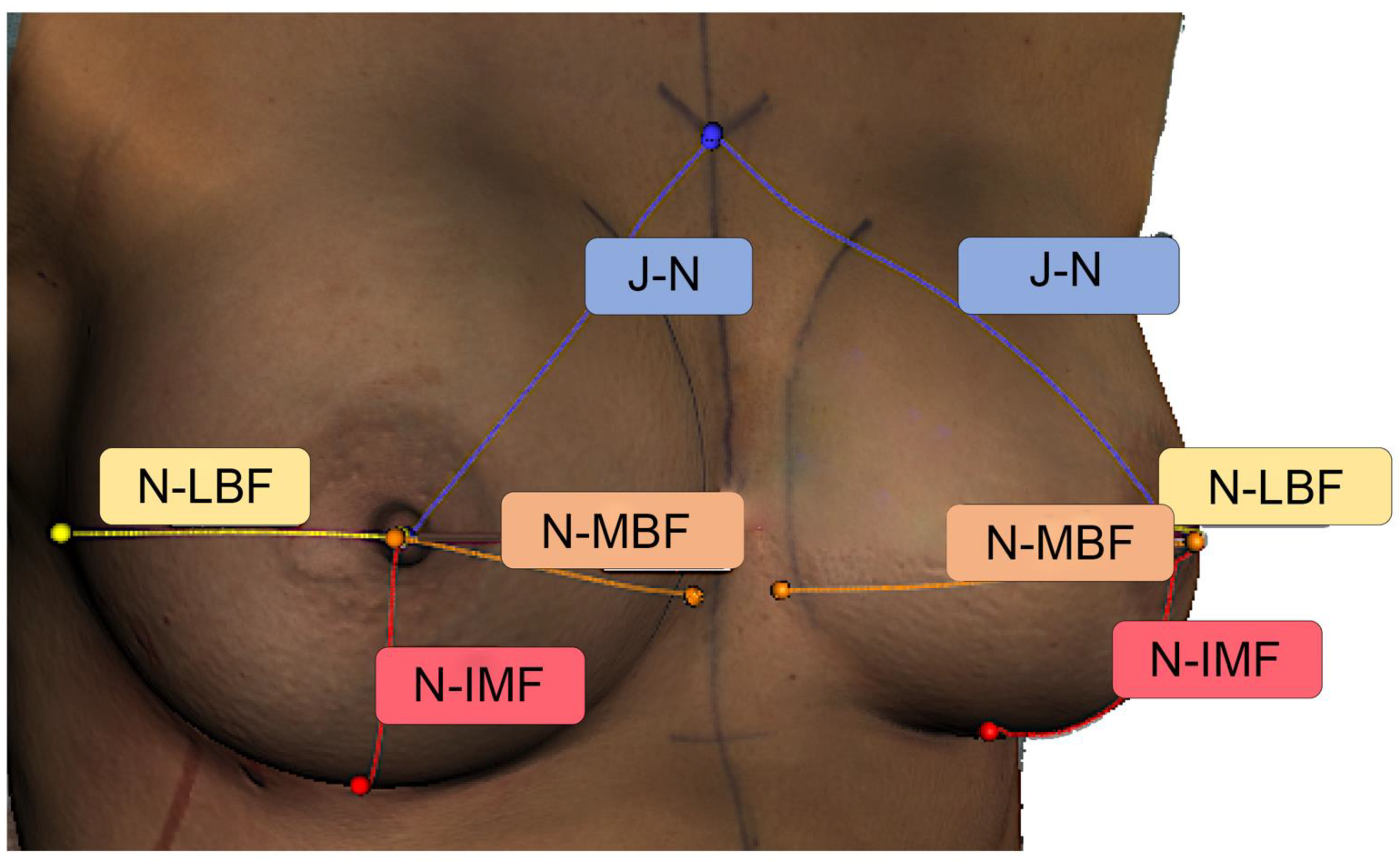
2.4. Inter-Landmark Distances
2.5. Position Change of the Nipple
2.6. Statistics
3. Results
3.1. Topographic Shift (TS) over the Four Breast Quadrants
3.1.1. Main Effect: Shape (Round vs. Anatomical)
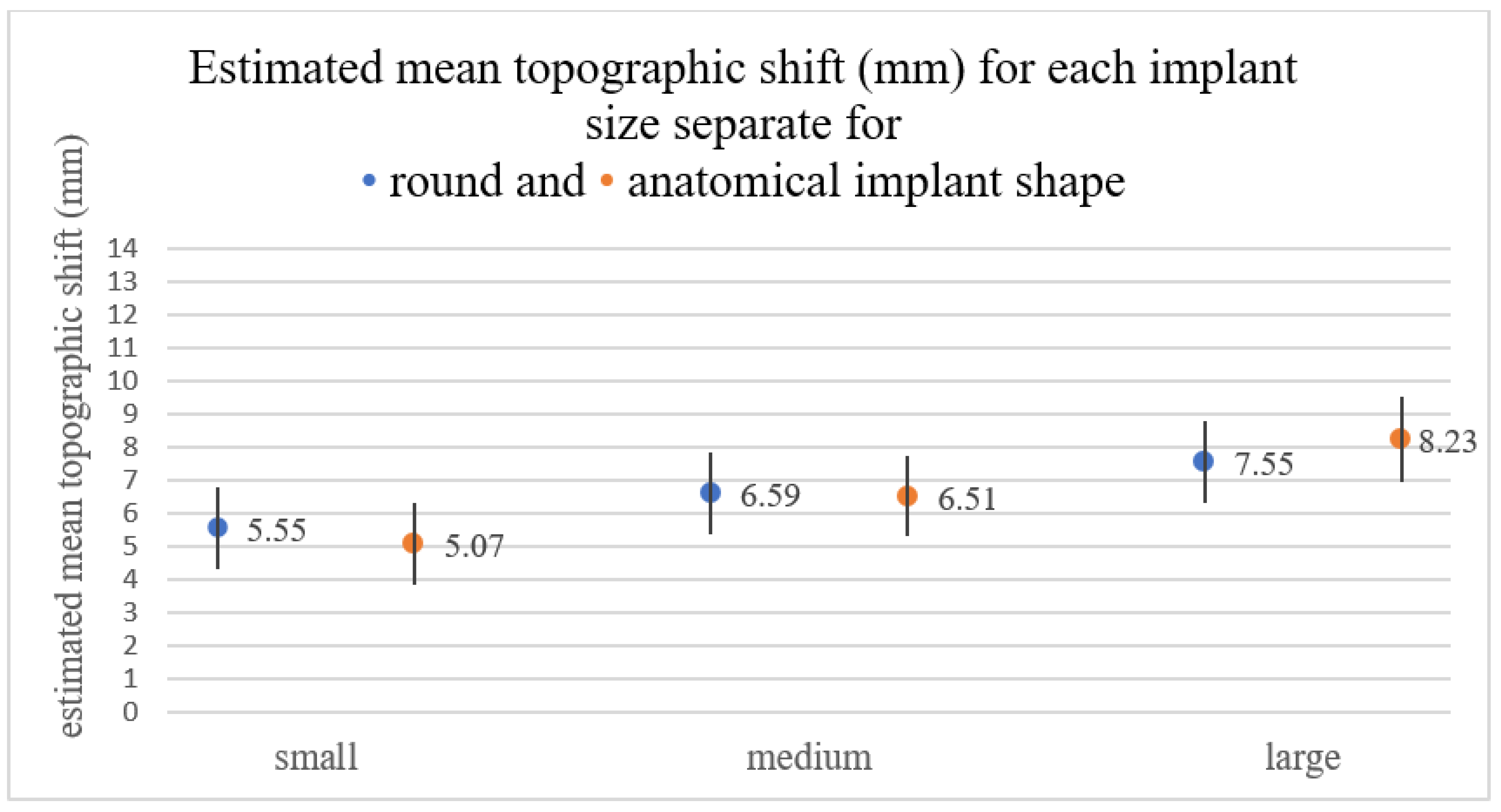
3.1.2. Main Effect: Size (Small vs. Medium vs. Large)
3.1.3. Main Effect: Quadrant (I vs. II vs. III vs. IV)
3.1.4. Interaction: Implant Size × Shape
3.1.5. Interaction: Implant Size × Quadrant
3.1.6. Interaction: Quadrant × Shape
3.2. Inter-Landmark Distances
3.3. Position Change of the Nipple
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Eder, M.; Schneider, A.; Feussner, H.; Zimmermann, A.; Höhnke, C.; Papadopulos, N.A.; Kovacs, L. Breast volume assessment based on 3D surface geometry: Verification of the method using MR imaging. Biomed. Tech. 2008, 53, 112–121. [Google Scholar] [CrossRef] [PubMed]
- Henseler, H.; Khambay, B.; Ju, X.; Ayoub, A.; Ray, A.K. Landmark-based statistical procrustes analysis in the examination of breast shape and symmetry. Handchir. Mikrochir. Plast. Chir. 2014, 46, 342–349. [Google Scholar]
- Kovacs, L.; Eder, M.; Hollweck, R.; Zimmermann, A.; Settles, M.; Schneider, A.; Endlich, M.; Mueller, A.; Schwenzer-Zimmerer, K.; Papadopulos, N.A.; et al. Comparison between breast volume measurement using 3D surface imaging and classical techniques. Breast 2007, 16, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Kovacs, L.; Eder, M.; Hollweck, R.; Zimmermann, A.; Settles, M.; Schneider, A.; Udosic, K.; Schwenzer-Zimmerer, K.; Papadopulos, N.; Biemer, E. New aspects of breast volume measurement using 3-dimensional surface imaging. Ann. Plast. Surg. 2006, 57, 602–610. [Google Scholar] [CrossRef]
- Kovacs, L.; Eder, M.; Zimmermann, A.; Müller, D.; Schuster, T.; Papadopulos, N.A.; Biemer, E.; Klöppel, M.; Machens, H.-G. Three-dimensional evaluation of breast augmentation and the influence of anatomic and round implants on operative breast shape changes. Aesthetic Plast. Surg. 2012, 36, 879–887. [Google Scholar] [CrossRef]
- Yip, J.M.; Mouratova, N.; Jeffery, R.M.; Veitch, D.E.; Woodman, R.J.; Dean, N.R. Accurate assessment of breast volume: A study comparing the volumetric gold standard (direct water displacement measurement of mastectomy specimen) with a 3D laser scanning technique. Ann. Plast. Surg. 2012, 68, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Cheng, F.; Cen, Y.; Liu, C.; Liu, R.; Pan, C.; Dai, S. Round versus Anatomical Implants in Primary Cosmetic Breast Augmentation: A Meta-Analysis and Systematic Review. Plast. Reconstr. Surg. 2019, 143, 711–721. [Google Scholar] [CrossRef] [PubMed]
- Friedman, T.; Davidovitch, N.; Scheflan, M. Comparative double blind clinical study on round versus shaped cohesive gel implants. Aesthet. Surg. J. 2006, 26, 530–536. [Google Scholar] [CrossRef] [Green Version]
- Hidalgo, D.A.; Weinstein, A.L. Intraoperative Comparison of Anatomical versus Round Implants in Breast Augmentation: A Randomized Controlled Trial. Plast. Reconstr. Surg. 2017, 139, 587–596. [Google Scholar] [CrossRef]
- Lotter, L.; Brébant, V.; Eigenberger, A.; Hartmann, R.; Mueller, K.; Baringer, M.; Prantl, L.; Schiltz, D. “Topographic Shift”: A new digital approach to evaluating topographic changes of the female breast. Arch. Gynecol. Obstet. 2020, 303, 515–520. [Google Scholar] [CrossRef] [PubMed]
- Eder, M.; Waldenfels, F.v.; Sichtermann, M.; Schuster, T.; Papadopulos, N.A.; Machens, H.G.; Biemer, E.; Kovacs, L. Three-dimensional evaluation of breast contour and volume changes following subpectoral augmentation mammaplasty over 6 months. J. Plast. Reconstr. Aesthet. Surg. 2011, 64, 1152–1160. [Google Scholar] [CrossRef] [PubMed]
- Eder, M.; Waldenfels, F.v.; Swobodnik, A.; Klöppel, M.; Pape, A.K.; Schuster, T.; Raith, S.; Kitzler, E.; Papadopulos, N.A.; Machens, H.-G.; et al. Objective breast symmetry evaluation using 3-D surface imaging. Breast 2012, 21, 152–158. [Google Scholar] [CrossRef]
- Koban, K.C.; Titze, V.; Etzel, L.; Frank, K.; Schenck, T.; Giunta, R. Quantitative volumetric analysis of the lower extremity: Validation against established tape measurement and water displacement. Handchir. Mikrochir. Plast. Chir. 2018, 50, 393–399. [Google Scholar]
- Roostaeian, J.; Adams, W.P., Jr. Three-Dimensional Imaging for Breast Augmentation: Is This Technology Providing Accurate Simulations? Aesthet. Surg. J. 2014, 34, 857–875. [Google Scholar] [CrossRef] [Green Version]
- Göpper, M.W.; Neubauer, J.; Kalash, Z.; Stark, G.B.; Simunovic, F. Improved accuracy of breast volume calculation from 3D surface imaging data using statistical shape models. PLoS ONE 2020, 15, e0233586. [Google Scholar] [CrossRef]
- Brown, T.P.; Ringrose, C.; Hyland, R.E.; Cole, A.A.; Brotherston, T.M. A method of assessing female breast morphometry and its clinical application. Br. J. Plast. Surg. 1999, 52, 355–359. [Google Scholar] [CrossRef]
- Bulstrode, N.; Bellamy, E.; Shrotria, S. Breast volume assessment: Comparing five different techniques. Breast 2001, 10, 117–123. [Google Scholar] [CrossRef]
- Hamas, R. The comparative dimensions of round and anatomical saline-filled breast implants. Aesthet. Surg. J. 2000, 20, 281–290. [Google Scholar] [CrossRef] [Green Version]
- Al-Ajam, Y.; Marsh, D.J.; Mohan, A.T.; Hamilton, S. Assessing the augmented breast: A blinded study comparing round and anatomical form-stable implants. Aesthet. Surg. J. 2015, 35, 273–278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adams, W.P., Jr.; Mallucci, P. Breast augmentation. Plast. Reconstr. Surg. 2012, 130, 597e–611e. [Google Scholar] [CrossRef] [PubMed]
- Cordeiro, P.G.; McGuire, P.; Murphy, D.K. Natrelle 410 Extra-Full Projection Silicone Breast Implants: 2-Year Results from Two Prospective Studies. Plast. Reconstr. Surg. 2015, 136, 638–646. [Google Scholar] [CrossRef] [Green Version]
- HedÈn, P.; Montemurro, P.; Adams, W.P.; Germann, G.; Scheflan, M.; Maxwell, G.P. Anatomical and Round Breast Implants: How to Select and Indications for Use. Plast. Reconstr. Surg. 2015, 136, 263–272. [Google Scholar] [CrossRef]
- Westreich, M. Anthropomorphic breast measurement: Protocol and results in 50 women with aesthetically perfect breasts and clinical application. Plast. Reconstr. Surg. 1997, 100, 468–479. [Google Scholar] [CrossRef]
- Xi, W.; Perdanasari, A.T.; Ong, Y.; Han, S.; Min, P.; Su, W.; Feng, S.; Pacchioni, L.; Zhang, Y.X.; Lazzeri, D. Objective breast volume, shape and surface area assessment: A systematic review of breast measurement methods. Aesthetic Plast. Surg. 2014, 38, 1116–1130. [Google Scholar] [CrossRef] [PubMed]
- Rubi, C.G.; Lozano, J.A.; PÈrez-Espadero, A.; Leache, M.E. Comparing Round and Anatomically Shaped Implants in Augmentation Mammaplasty: The Experts’ Ability to Differentiate the Type of Implant. Plast. Reconstr. Surg. 2017, 139, 60–64. [Google Scholar] [CrossRef]
- Adams, W.P.; Small, K.H. The Process of Breast Augmentation with Special Focus on Patient Education, Patient Selection and Implant Selection. Clin. Plast. Surg. 2015, 42, 413–426. [Google Scholar] [CrossRef] [PubMed]
- Vorstenbosch, J.; Islur, A. Correlation of Prediction and Actual Outcome of Three-Dimensional Simulation in Breast Augmentation Using a Cloud-Based Program. Aesthetic Plast. Surg. 2017, 41, 481. [Google Scholar] [CrossRef]
- Longo, B.; Farcomeni, A.; Ferri, G.; Campanale, A.; Sorotos, M.; Santanelli, F. The BREAST-V: A unifying predictive formula for volume assessment in small, medium, and large breasts. Plast. Reconstr. Surg. 2013, 132, 1e–7e. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, M.J.; Cardoso, J.; Amaral, N.; Azevedo, I.; Barreau, L.; Bernardo, M.; Christie, D.; Costa, S.; Fitzal, F.; Fougo, J.L.; et al. Turning subjective into objective: The BCCT.core software for evaluation of cosmetic results in breast cancer conservative treatment. Breast 2007, 16, 456–461. [Google Scholar] [CrossRef]




| Patient No. | Age (Years) | Weight (kg) | BMI (kg/m2) | Regnault’s Degree of Ptosis |
|---|---|---|---|---|
| 1 | 24 | 59 | 22 | 0 |
| 2 | 23 | 76 | 25 | 0 |
| 3 | 31 | 75 | 26 | 2 |
| 4 | 49 | 58 | 22 | 1 |
| 5 | 22 | 68 | 24 | 0 |
| 6 | 47 | 60 | 22 | 1 |
| 7 | 27 | 54 | 22 | 2 |
| 8 | 46 | 65 | 25 | 0 |
| 9 | 33 | 60 | 19 | 1 |
| 10 | 32 | 69 | 20 | 0 |
| Median (range) | 32 (22–49) | 63 (54–76) | 22 (19–26) | 0.5 (0–2) |
| SI 1 | SI 2 | SI 3 | SI 4 | SI 5 | SI 6 | ||
|---|---|---|---|---|---|---|---|
| 1 | 165.0 | 170.0 | 210.0 | 210.0 | 250.0 | - | |
| 2 | 295.0 | 290.0 | 400.0 | 390.0 | 505.0 | 495.0 | |
| 3 | 320.0 | 320.0 | 400.0 | 395.0 | 485.0 | 480.0 | |
| 4 | 165.0 | 165.0 | 220.0 | 220.0 | 275.0 | 275.0 | |
| Patient, No. | 5 | 235.0 | 235.0 | 320.0 | 320.0 | 400.0 | 395.0 |
| 6 | 165.0 | 165.0 | 220.0 | 220.0 | - | - | |
| 7 | - | - | 220.0 | 220.0 | 275.0 | 275.0 | |
| 8 | 185.0 | 185.0 | 255.0 | 255.0 | 315.0 | 315.0 | |
| 9 | 215.0 | 210.0 | 285.0 | 280.0 | 360.0 | 350.0 | |
| 10 | 235.0 | 235.0 | 320.0 | 320.0 | 400.0 | 395.0 | |
| N valid (missing) | 9 (1) | 9 (1) | 10 (0) | 10 (0) | 9 (1) | 8 (2) | |
| Mean (cc) | 220.0 | 219.4 | 285.0 | 283.0 | 362.8 | 372.5 | |
| SD (cc) | 57.4 | 56.1 | 73.1 | 70.5 | 92.4 | 84.9 | |
| Minimum (cc) | 165.0 | 165.0 | 210.0 | 210.0 | 250.0 | 275.0 | |
| Maximum (cc) | 320.0 | 320.0 | 400.0 | 395.0 | 505.0 | 495.0 |
| 95% CI | |||||
|---|---|---|---|---|---|
| Estimated Mean (mm) | Lower Limit (mm) | Upper Limit (mm) | p Value | ||
| Shape | Round | 6.56 | 5.47 | 7.66 | 0.90 |
| Anatomical | 6.60 | 5.51 | 7.70 | ||
| Size | Small | 5.31 | 4.17 | 6.45 | |
| Medium | 6.55 | 5.43 | 7.67 | <0.001 | |
| Large | 7.89 | 6.74 | 9.03 | <0.001 | |
| Quadrant | I | 8.08 | 6.91 | 9.25 | |
| II | 9.16 | 7.99 | 10.33 | <0.014 | |
| III | 6.96 | 5.79 | 8.13 | <0.011 | |
| IV | 2.14 | 0.97 | 3.30 | <0.001 | |
| Nipple—Jugulum (mm) | Nipple—IMF (mm) | Nipple—Medial Breast Fold (mm) | Nipple—Lateral Breast Fold (mm) | |
|---|---|---|---|---|
| Native | 188.3 ± 13.7 | 64.7 ± 10.0 | 87.2 ± 11.7 | 97.7 ± 8.8 |
| SI 1 | 188.9 ± 12.3 | 85.8 ± 6.9 | 106.8 ± 7.0 | 116.5 ± 9.7 |
| SI 2 | 189.5 ± 12.9 | 84.8 ± 6.8 | 107.5 ± 6.8 | 115.5 ± 8.4 |
| SI 3 | 188.9 ± 12.7 | 90.5 ± 9.4 | 111.5 ± 6.4 | 121.3 ± 10.5 |
| SI 4 | 188.0 ± 12.6 | 91.2 ± 9.2 | 111.5 ± 5.7 | 121.0 ± 10.8 |
| SI 5 | 190.5 ± 13.9 | 99.1 ± 12.6 | 115.3 ± 6.4 | 131.1 ± 12.5 |
| SI 6 | 187.4 ± 13.9 | 101.9 ± 11.6 | 116.3 ± 5.4 | 131.0 ± 11.3 |
| Anatomical, No. | Total | ||||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | |||
| Round, No. | Q1 | 2 | 1 | 0 | 3 |
| Q2 | 2 | 46 | 1 | 49 | |
| Q3 | 1 | 1 | 0 | 2 | |
| Total | 5 | 48 | 1 | 54 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lotter, L.; Zucal, I.; Brébant, V.; Heine, N.; Hartmann, R.; Mueller, K.; Prantl, L.; Schiltz, D. Intraoperative 3D Comparison of Round and Anatomical Breast Implants: Dispelling a Myth. J. Clin. Med. 2022, 11, 149. https://doi.org/10.3390/jcm11010149
Lotter L, Zucal I, Brébant V, Heine N, Hartmann R, Mueller K, Prantl L, Schiltz D. Intraoperative 3D Comparison of Round and Anatomical Breast Implants: Dispelling a Myth. Journal of Clinical Medicine. 2022; 11(1):149. https://doi.org/10.3390/jcm11010149
Chicago/Turabian StyleLotter, Luisa, Isabel Zucal, Vanessa Brébant, Norbert Heine, Robin Hartmann, Karolina Mueller, Lukas Prantl, and Daniel Schiltz. 2022. "Intraoperative 3D Comparison of Round and Anatomical Breast Implants: Dispelling a Myth" Journal of Clinical Medicine 11, no. 1: 149. https://doi.org/10.3390/jcm11010149
APA StyleLotter, L., Zucal, I., Brébant, V., Heine, N., Hartmann, R., Mueller, K., Prantl, L., & Schiltz, D. (2022). Intraoperative 3D Comparison of Round and Anatomical Breast Implants: Dispelling a Myth. Journal of Clinical Medicine, 11(1), 149. https://doi.org/10.3390/jcm11010149







