Impact of the COVID-19 Pandemic on Urologic Oncology Surgery: Implications for Moving Forward
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Study Population and Outcome Measures
2.2. Statistical Analysis
3. Results
3.1. Study Cohort
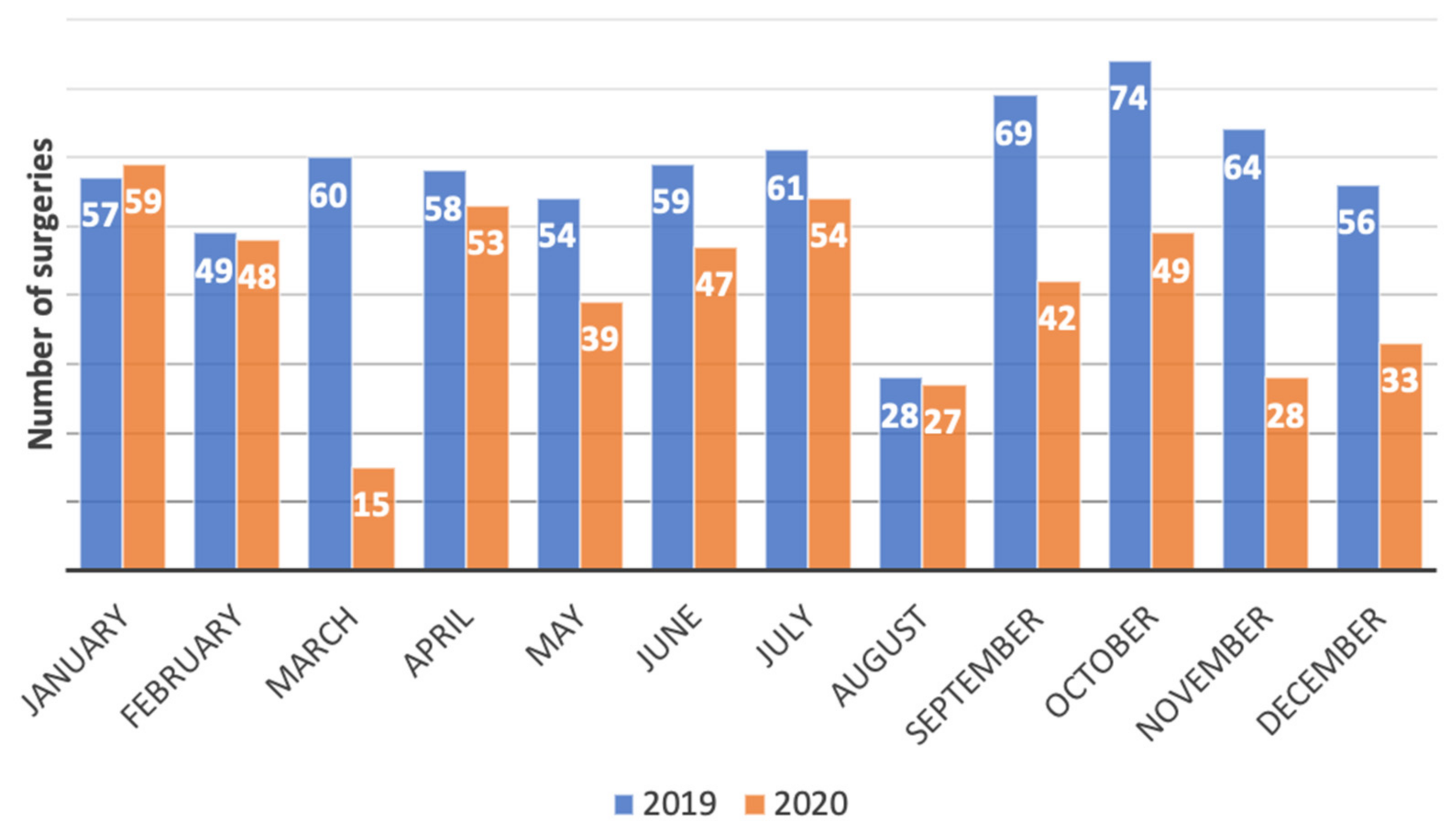
3.2. Number of Urologic Oncology Surgeries Performed
3.3. Waiting Time
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- COVIDSurg Collaborative. Elective surgery cancellations due to the COVID-19 pandemic: Global predictive modelling to inform surgical recovery plans. Br. J. Surg. 2020, 107, 1440–1449. [Google Scholar] [CrossRef]
- Wallis, C.J.D.; Catto, J.W.F.; Finelli, A.; Glaser, A.W.; Gore, J.L.; Loeb, S.; Morgan, T.M.; Morgans, A.K.; Mottet, N.; Neal, R.; et al. The Impact of the COVID-19 Pandemic on Genitourinary Cancer Care: Re-envisioning the Future. Eur. Urol. 2020, 78, 731–742. [Google Scholar] [CrossRef]
- Wang, J.; Vahid, S.; Eberg, M.; Milroy, S.; Milkovich, J.; Wright, F.C.; Hunter, A.; Kalladeen, R.; Zanchetta, C.; Wijeysundera, H.C.; et al. Clearing the surgical backlog caused by COVID-19 in Ontario: A time series modelling study. CMAJ 2020, 192, E1347–E1356. [Google Scholar] [CrossRef] [PubMed]
- Carenzo, L.; Costantini, E.; Greco, M.; Barra, F.L.; Rendiniello, V.; Mainetti, M.; Bui, R.; Zanella, A.; Grasselli, G.; Lagioia, M.; et al. Hospital surge capacity in a tertiary emergency referral centre during the COVID-19 outbreak in Italy. Anaesthesia 2020, 75, 928–934. [Google Scholar] [CrossRef]
- Remuzzi, A.; Remuzzi, G. COVID-19 and Italy: What next? Lancet 2020, 395, 1225–1228. [Google Scholar] [CrossRef]
- Livingston, E.; Bucher, K. Coronavirus Disease 2019 (COVID-19) in Italy. JAMA 2020, 323, 1335. [Google Scholar] [CrossRef] [Green Version]
- Motterle, G.; Morlacco, A.; Iafrate, M.; Bianco, M.; Federa, G.; Xhafka, O.; Zattoni, F.; Prayer-Galetti, T. The impact of COVID-19 pandemic on urological emergencies: A single-center experience. World J. Urol. 2021, 39, 1985–1989. [Google Scholar] [CrossRef] [PubMed]
- Naspro, R.; Da Pozzo, L.F. Urology in the time of corona. Nat. Rev. Urol. 2020, 17, 251–253. [Google Scholar] [CrossRef] [PubMed]
- Novara, G.; Bartoletti, R.; Crestani, A.; De Nunzio, C.; Durante, J.; Gregori, A.; Liguori, G.; Pavan, N.; Trombetta, C.; Simonato, A.; et al. Impact of the COVID-19 pandemic on urological practice in emergency departments in Italy. BJU Int. 2020, 126, 245–247. [Google Scholar] [CrossRef]
- Oderda, M.; Roupret, M.; Marra, G.; Merseburger, A.S.; Oderda, G.; Falcone, M.; Ceruti, C.; Shariat, S.F.; Gontero, P. The Impact of COVID-19 Outbreak on Uro-oncological Practice Across Europe: Which Burden of Activity Are We Facing Ahead? Eur. Urol. 2020, 78, 124–126. [Google Scholar] [CrossRef]
- Puliatti, S.; Eissa, A.; Eissa, R.; Amato, M.; Mazzone, E.; Dell’Oglio, P.; Sighinolfi, M.C.; Zoeir, A.; Micali, S.; Bianchi, G.; et al. COVID-19 and urology: A comprehensive review of the literature. BJU Int. 2020, 125, E7–E14. [Google Scholar] [CrossRef] [PubMed]
- Dell’Oglio, P.; Cacciamani, G.E.; Muttin, F.; Mirabella, G.; Secco, S.; Roscigno, M.; Rovati, F.A.; Barbieri, M.; Naspro, R.; Peroni, A.; et al. Applicability of COVID-19 Pandemic Recommendations for Urology Practice: Data from Three Major Italian Hot Spots (BreBeMi). Eur. Urol. Open Sci. 2021, 26, 1–9. [Google Scholar] [CrossRef]
- Ribal, M.J.; Cornford, P.; Briganti, A.; Knoll, T.; Gravas, S.; Babjuk, M.; Harding, C.; Breda, A.; Bex, A.; Rassweiler, J.J.; et al. European Association of Urology Guidelines Office Rapid Reaction Group: An Organisation-wide Collaborative Effort to Adapt the European Association of Urology Guidelines Recommendations to the Coronavirus Disease 2019 Era. Eur. Urol. 2020, 78, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Amparore, D.; Campi, R.; Checcucci, E.; Sessa, F.; Pecoraro, A.; Minervini, A.; Fiori, C.; Ficarra, V.; Novara, G.; Serni, S.; et al. Forecasting the Future of Urology Practice: A Comprehensive Review of the Recommendations by International and European Associations on Priority Procedures During the COVID-19 Pandemic. Eur. Urol. Focus 2020, 6, 1032–1048. [Google Scholar] [CrossRef]
- Campi, R.; Amparore, D.; Capitanio, U.; Checcucci, E.; Salonia, A.; Fiori, C.; Minervini, A.; Briganti, A.; Carini, M.; Montorsi, F.; et al. Assessing the Burden of Nondeferrable Major Uro-oncologic Surgery to Guide Prioritisation Strategies During the COVID-19 Pandemic: Insights from Three Italian High-volume Referral Centres. Eur. Urol. 2020, 78, 11–15. [Google Scholar] [CrossRef] [PubMed]
- Katims, A.B.; Razdan, S.; Eilender, B.M.; Wiklund, P.; Tewari, A.K.; Kyprianou, N.; Badani, K.K.; Mehrazin, R. Urologic oncology practice during COVID-19 pandemic: A systematic review on what can be deferrable vs. nondeferrable. Urol. Oncol. 2020, 38, 783–792. [Google Scholar] [CrossRef] [PubMed]
- Maganty, A.; Yu, M.; Anyaeche, V.I.; Zhu, T.; Hay, J.M.; Davies, B.J.; Yabes, J.G.; Jacobs, B.L. Referral pattern for urologic malignancies before and during the COVID-19 pandemic. Urol. Oncol. 2021, 39, 268–276. [Google Scholar] [CrossRef]
- Rosenzweig, B.; Bex, A.; Dotan, Z.A.; Frydenberg, M.; Klotz, L.; Lotan, Y.; Schulman, C.C.; Tsaur, I.; Ramon, J. Trends in urologic oncology clinical practice and medical education under COVID-19 pandemic: An international survey of senior clinical and academic urologists. Urol. Oncol. 2020, 38, 929.e921–929.e910. [Google Scholar] [CrossRef]
- Shinder, B.M.; Patel, H.V.; Sterling, J.; Tabakin, A.L.; Kim, I.Y.; Jang, T.L.; Singer, E.A. Urologic oncology surgery during COVID-19: A rapid review of current triage guidance documents. Urol. Oncol. Semin. Orig. Investig. 2020, 38, 609–614. [Google Scholar] [CrossRef]
- Stensland, K.D.; Morgan, T.M.; Moinzadeh, A.; Lee, C.T.; Briganti, A.; Catto, J.W.F.; Canes, D. Considerations in the Triage of Urologic Surgeries During the COVID-19 Pandemic. Eur. Urol. 2020, 77, 663–666. [Google Scholar] [CrossRef]
- Tachibana, I.; Ferguson, E.L.; Mahenthiran, A.; Natarajan, J.P.; Masterson, T.A.; Bahler, C.D.; Sundaram, C.P. Delaying Cancer Cases in Urology during COVID-19: Review of the Literature. J. Urol. 2020, 204, 926–933. [Google Scholar] [CrossRef]
- Tayeh, G.A.; Khalil, N.; Alkassis, M.; Aoun, F.; Waked, C.; Nemr, E. Urothelial carcinoma in COVID-19: Lessons from a pandemic and their impact on clinical practice. Future Oncol. 2021, 17, 4233–4235. [Google Scholar] [CrossRef]
- Tulchiner, G.; Staudacher, N.; Fritz, J.; Radmayr, C.; Culig, Z.; Horninger, W.; Pichler, R. The “COVID-19 Pandemic Gap” and Its Influence on Oncologic Outcomes of Bladder Cancer. Cancers 2021, 13, 1758. [Google Scholar] [CrossRef] [PubMed]
- Macdonald, N.; Clements, C.; Sobti, A.; Rossiter, D.; Unnithan, A.; Bosanquet, N. Tackling the elective case backlog generated by Covid-19: The scale of the problem and solutions. J. Public Health 2020, 42, 712–716. [Google Scholar] [CrossRef]
- Uimonen, M.; Kuitunen, I.; Paloneva, J.; Launonen, A.P.; Ponkilainen, V.; Mattila, V.M. The impact of the COVID-19 pandemic on waiting times for elective surgery patients: A multicenter study. PLoS ONE 2021, 16, e0253875. [Google Scholar] [CrossRef] [PubMed]
- Uimonen, M.; Kuitunen, I.; Seikkula, H.; Mattila, V.M.; Ponkilainen, V. Healthcare lockdown resulted in a treatment backlog in elective urological surgery during COVID-19. BJU Int. 2021, 128, 33–35. [Google Scholar] [CrossRef]
- Oderda, M.; Calleris, G.; Falcone, M.; Fasolis, G.; Muto, G.; Oderda, G.; Porpiglia, F.; Volpe, A.; Bertetto, O.; Gontero, P. How uro-oncology has been affected by COVID-19 emergency? Data from Piedmont/Valle d’Aosta Oncological Network, Italy. Urol. J. 2021, 88, 3–8. [Google Scholar] [CrossRef]
- Mian, B.M.; Siddiqui, S.; Ahmad, A.E. Management of urologic cancers during the pandemic and potential impact of treatment deferrals on outcomes. Urol. Oncol. 2021, 39, 258–267. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Rojo, E.; Manfredi, C.; Santos-Perez-de-la-Blanca, R.; Tejido-Sanchez, A.; Garcia-Gomez, B.; Aliaga-Benitez, M.; Romero-Otero, J.; Rodriguez-Antolin, A. Impact of COVID-19 outbreak on urology surgical waiting lists and waiting lists prioritization strategies in the Post-COVID-19 era. Actas Urol. Esp. 2021, 45, 207–214. [Google Scholar] [CrossRef]
- Torzilli, G.; Vigano, L.; Galvanin, J.; Castoro, C.; Quagliuolo, V.; Spinelli, A.; Zerbi, A.; Donadon, M.; Montorsi, M.; COVID-SURGE-ITA Group. A Snapshot of Elective Oncological Surgery in Italy during COVID-19 Emergency: Pearls, Pitfalls, and Perspectives. Ann. Surg. 2020, 272, e112–e117. [Google Scholar] [CrossRef]
- Alkatout, I.; Biebl, M.; Momenimovahed, Z.; Giovannucci, E.; Hadavandsiri, F.; Salehiniya, H.; Allahqoli, L. Has COVID-19 Affected Cancer Screening Programs? A Systematic Review. Front Oncol. 2021, 11, 675038. [Google Scholar] [CrossRef]
- Morris, E.J.A.; Goldacre, R.; Spata, E.; Mafham, M.; Finan, P.J.; Shelton, J.; Richards, M.; Spencer, K.; Emberson, J.; Hollings, S.; et al. Impact of the COVID-19 pandemic on the detection and management of colorectal cancer in England: A population-based study. Lancet Gastroenterol. Hepatol. 2021, 6, 199–208. [Google Scholar] [CrossRef]
- Sud, A.; Jones, M.E.; Broggio, J.; Loveday, C.; Torr, B.; Garrett, A.; Nicol, D.L.; Jhanji, S.; Boyce, S.A.; Gronthoud, F.; et al. Collateral damage: The impact on outcomes from cancer surgery of the COVID-19 pandemic. Ann. Oncol. 2020, 31, 1065–1074. [Google Scholar] [CrossRef]
- Sud, A.; Torr, B.; Jones, M.E.; Broggio, J.; Scott, S.; Loveday, C.; Garrett, A.; Gronthoud, F.; Nicol, D.L.; Jhanji, S.; et al. Effect of delays in the 2-week-wait cancer referral pathway during the COVID-19 pandemic on cancer survival in the UK: A modelling study. Lancet Oncol. 2020, 21, 1035–1044. [Google Scholar] [CrossRef]
- Ficarra, V.; Novara, G.; Abrate, A.; Bartoletti, R.; Crestani, A.; De Nunzio, C.; Giannarini, G.; Gregori, A.; Liguori, G.; Mirone, V.; et al. Urology practice during the COVID-19 pandemic. Minerva Urol. Nefrol. 2020, 72, 369–375. [Google Scholar] [CrossRef] [PubMed]
- Heldwein, F.L.; Loeb, S.; Wroclawski, M.L.; Sridhar, A.N.; Carneiro, A.; Lima, F.S.; Teoh, J.Y. A Systematic Review on Guidelines and Recommendations for Urology Standard of Care During the COVID-19 Pandemic. Eur. Urol. Focus 2020, 6, 1070–1085. [Google Scholar] [CrossRef] [PubMed]
- Chan, V.W.; Tan, W.S.; Asif, A.; Ng, A.; Gbolahan, O.; Dinneen, E.; To, W.; Kadhim, H.; Premchand, M.; Burton, O.; et al. Effects of Delayed Radical Prostatectomy and Active Surveillance on Localised Prostate Cancer—A Systematic Review and Meta-Analysis. Cancers 2021, 13, 3274. [Google Scholar] [CrossRef] [PubMed]
- Virseda Rodríguez, A.J.; Marcos Asensio, S.; Herrero Polo, M.; Hernández Sanchez, T.; Sanz Ruiz, A.; García, F.; Vesga, F.; Gutiérrez, E.; Serrano, J.M.; Calleja, J.; et al. The impact of time from biopsy to radical prostatectomy on Gleason score undergrading and other related factors. Actas Urol. Esp. 2020, 44, 187–195. [Google Scholar] [CrossRef] [PubMed]
- Culpan, M.; Keser, F.; Acar, H.C.; Otunctemur, A.; Kucuk, E.V.; Erdem, S.; Ozer, M.; Sen, U.T.; Degirmenci, E.; Ergul, R.; et al. Impact of delay in cystoscopic surveillance on recurrence and progression rates in patients with non-muscle-invasive bladder cancer during the COVID-19 pandemic. Int. J. Clin. Pract. 2021, 75, e14490. [Google Scholar] [CrossRef]
- Amparore, D.; Checcucci, E.; Serni, S.; Minervini, A.; Gacci, M.; Esperto, F.; Fiori, C.; Porpiglia, F.; Campi, R. Urology Residency Training at the Time of COVID-19 in Italy: 1 Year after the Beginning. Eur. Urol. Open Sci. 2021, 31, 37–40. [Google Scholar] [CrossRef]
- Amparore, D.; Claps, F.; Cacciamani, G.E.; Esperto, F.; Fiori, C.; Liguori, G.; Serni, S.; Trombetta, C.; Carini, M.; Porpiglia, F.; et al. Impact of the COVID-19 pandemic on urology residency training in Italy. Minerva Urol. Nefrol. 2020, 72, 505–509. [Google Scholar] [CrossRef] [PubMed]
- Boehm, K.; Ziewers, S.; Brandt, M.P.; Sparwasser, P.; Haack, M.; Willems, F.; Thomas, A.; Dotzauer, R.; Höfner, T.; Tsaur, I.; et al. Telemedicine Online Visits in Urology During the COVID-19 Pandemic-Potential, Risk Factors, and Patients’ Perspective. Eur. Urol. 2020, 78, 16–20. [Google Scholar] [CrossRef]
- Novara, G.; Checcucci, E.; Crestani, A.; Abrate, A.; Esperto, F.; Pavan, N.; De Nunzio, C.; Galfano, A.; Giannarini, G.; Gregori, A.; et al. Telehealth in Urology: A Systematic Review of the Literature. How Much Can Telemedicine Be Useful during and after the COVID-19 Pandemic? Eur. Urol. 2020, 78, 786–811. [Google Scholar] [CrossRef] [PubMed]
- Rodler, S.; Apfelbeck, M.; Schulz, G.B.; Ivanova, T.; Buchner, A.; Staehler, M.; Heinemann, V.; Stief, C.; Casuscelli, J. Telehealth in Uro-oncology Beyond the Pandemic: Toll or Lifesaver? Eur. Urol. Focus 2020, 6, 1097–1103. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez Socarrás, M.; Loeb, S.; Teoh, J.Y.; Ribal, M.J.; Bloemberg, J.; Catto, J.; N’Dow, J.; Van Poppel, H.; Gómez Rivas, J. Telemedicine and Smart Working: Recommendations of the European Association of Urology. Eur. Urol. 2020, 78, 812–819. [Google Scholar] [CrossRef]
- Westhofen, T.; Magistro, G.; Lennartz, S.; Casuscelli, J.; Stief, C.; Rodler, S. Confronting hidden COVID-19 burden: A telemedical solution for elective urological outpatient clinics. Infection 2020, 48, 935–939. [Google Scholar] [CrossRef] [PubMed]

| 2019 (n = 720) | 2020 (n = 528) | p-Value | |
|---|---|---|---|
| Sex | 0.012 | ||
| Male | 619 (86%) | 426 (81%) | |
| Female | 101 (14%) | 102 (19%) | |
| Age (years) | 69 ± 10 | 69 ± 11 | 0.1396 |
| Nationality | 0.667 | ||
| Italian | 696 (97%) | 508 (96%) | |
| Others | 24 (3%) | 20 (4%) | |
| Type of hospital admission | 0.094 | ||
| Elective | 689 (96%) | 494 (94%) | |
| Emergency | 31 (4%) | 34 (6%) | |
| Length of hospital stay (days) | 4 (IQR 3–5) | 3 (IQR 3–6) | 0.8274 |
| Indication for surgery | <0.0001 | ||
| Kidney tumor | 97 (13%) | 89 (17%) | |
| UTUC (including renal pelvis) | 9 (1%) | 19 (3%) | |
| Bladder tumor | 350 (49%) | 295 (56%) | |
| Prostate tumor | 264 (37%) | 125 (24%) | |
| Type of procedure | <0.0001 | ||
| Partial nephrectomy | 75 (10%) | 62 (12%) | |
| Radical nephrectomy/nephroureterectomy | 31 (4%) | 46 (9%) | |
| TURBT | 318 (44%) | 258 (49%) | |
| Radical cystectomy | 32 (5%) | 37 (7%) | |
| Radical prostatectomy | 264 (37%) | 125 (23%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guerrieri, R.; Rovati, L.; Dell’Oglio, P.; Galfano, A.; Ragazzoni, L.; Aseni, P. Impact of the COVID-19 Pandemic on Urologic Oncology Surgery: Implications for Moving Forward. J. Clin. Med. 2022, 11, 171. https://doi.org/10.3390/jcm11010171
Guerrieri R, Rovati L, Dell’Oglio P, Galfano A, Ragazzoni L, Aseni P. Impact of the COVID-19 Pandemic on Urologic Oncology Surgery: Implications for Moving Forward. Journal of Clinical Medicine. 2022; 11(1):171. https://doi.org/10.3390/jcm11010171
Chicago/Turabian StyleGuerrieri, Rossella, Lucrezia Rovati, Paolo Dell’Oglio, Antonio Galfano, Luca Ragazzoni, and Paolo Aseni. 2022. "Impact of the COVID-19 Pandemic on Urologic Oncology Surgery: Implications for Moving Forward" Journal of Clinical Medicine 11, no. 1: 171. https://doi.org/10.3390/jcm11010171







