Conservative Surgery in Endometrial Cancer
Abstract
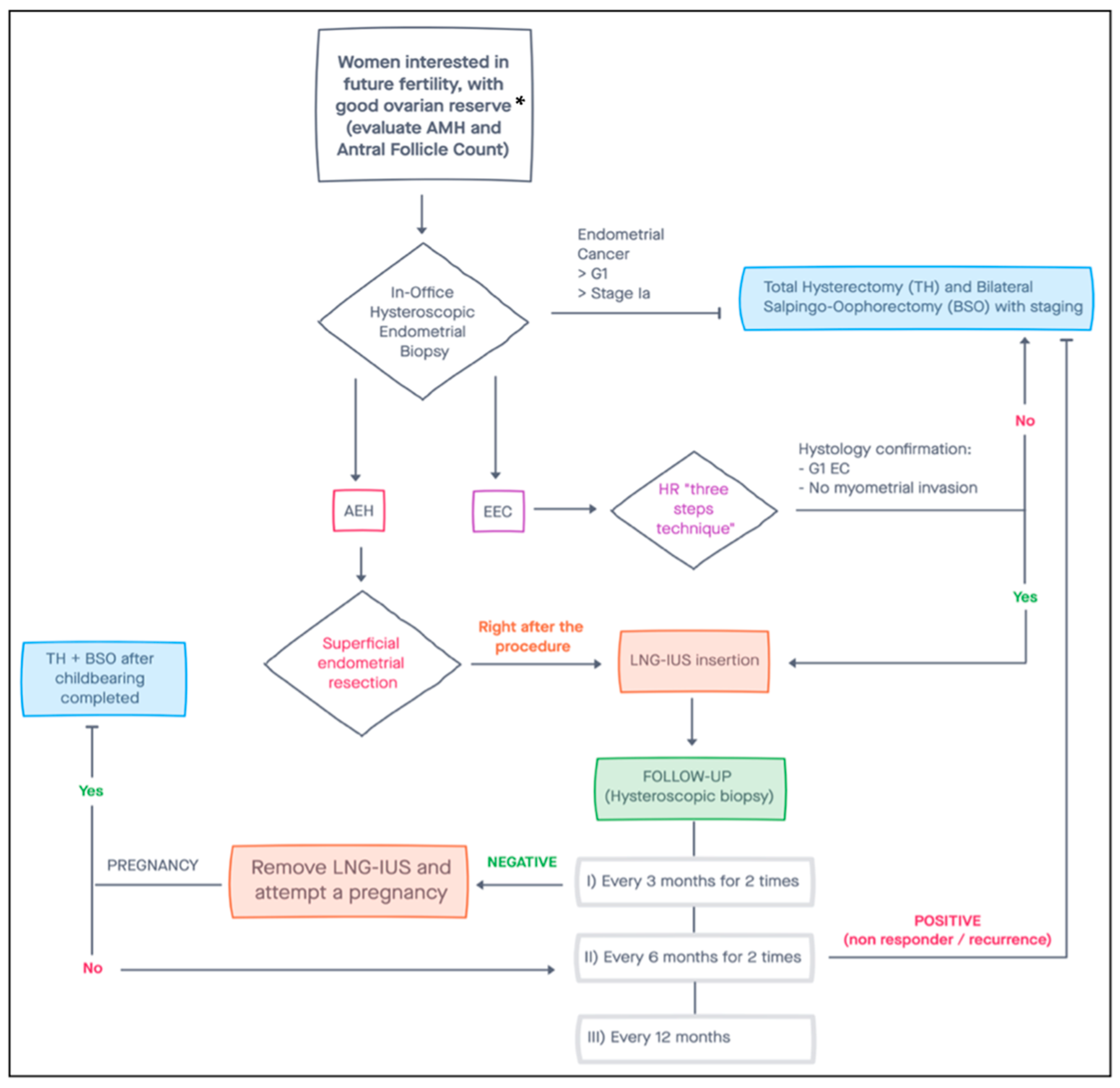
:1. Introduction
2. Objectives
- Risk factors for endometrial hyperplasia and cancer
- Screening and diagnosis
- Treatment
- Follow-up
- Oncological outcomes
- Reproductive outcomes
2.1. Risk Factors for Endometrial Hyperplasia and Cancer
2.2. Screening and Diagnosis
Imaging
2.3. Treatment
- The patient must be diagnosed with well-differentiated (Grade 1) endometrioid adenocarcinoma on D&C, confirmed by expert pathology review.
- The disease must be limited to the endometrium on MRI (preferred) or TV ultrasound.
- There must be an absence of suspicious or metastatic disease on imaging.
- There must be no contraindications to medical treatment or pregnancy.
2.4. Follow-Up
2.5. Outcomes
2.5.1. Oncological Outcomes
2.5.2. Reproductive Outcomes
3. Discussion
3.1. Main Findings
3.2. Implication and Future Perspective
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Trojano, G.; Olivieri, C.; Tinelli, R.; Damiani, G.R.; Pellegrino, A.; Cicinelli, E. Conservative treatment in early-stage endometrial cancer: A review. Acta Biomed. 2019, 90, 405–410. [Google Scholar] [CrossRef]
- Casadio, P.; La Rosa, M.; Alletto, A.; Magnarelli, G.; Arena, A.; Fontana, E.; Fabbri, M.; Giovannico, K.; Virgilio, A.; Raimondo, D.; et al. Fertility Sparing Treatment of Endometrial Cancer with and without Initial Infiltration of Myometrium: A Single Center Experience. Cancers 2020, 12, 3571. [Google Scholar] [CrossRef] [PubMed]
- Gressel, G.M.; Parkash, V.; Pal, L. Management options and fertility-preserving therapy for premenopausal endometrial hyperplasia and early-stage endometrial cancer. Int. J. Gynaecol. Obstet. 2015, 131, 234–239. [Google Scholar] [CrossRef] [PubMed]
- Parslov, M.; Lidegaard, O.; Klintorp, S.; Pedersen, B.; Jønsson, L.; Eriksen, P.S.; Ottesen, B. Risk factors among young women with endometrial cancer: A Danish case-control study. Am. J. Obstet. Gynecol. 2000, 182, 23–29. [Google Scholar] [CrossRef] [Green Version]
- Gadducci, A.; Spirito, N.; Baroni, E.; Tana, R.; Genazzani, A.R. The fertility-sparing treatment in patients with endometrial atypical hyperplasia and early endometrial cancer: A debated therapeutic option. Gynecol. Endocrinol. 2009, 25, 683–691. [Google Scholar] [CrossRef] [PubMed]
- Soliman, P.T.; Oh, J.C.; Schmeler, K.M.; Sun, C.C.; Slomovitz, B.M.; Gershenson, D.M.; Burke, T.W.; Lu, K.H. Risk factors for young premenopausal women with endometrial cancer. Obstet. Gynecol. 2005, 105, 575–580. [Google Scholar] [CrossRef] [PubMed]
- Esposito, K.; Chiodini, P.; Capuano, A.; Bellastella, G.; Maiorino, M.I.; Giugliano, D. Metabolic syndrome and endometrial cancer: A meta-analysis. Endocrine 2014, 45, 28–36. [Google Scholar] [CrossRef]
- Viola, A.S.; Gouveia, D.; Andrade, L.; Aldrighi, J.M.; Viola, C.F.; Bahamondes, L. Prevalence of endometrial cancer and hyperplasia in non-symptomatic overweight and obese women. Aust. N. Z. J. Obstet. Gynaecol. 2008, 48, 207–213. [Google Scholar] [CrossRef]
- Zhang, Y.; Liu, H.; Yang, S.; Zhang, J.; Qian, L.; Chen, X. Overweight, obesity and endometrial cancer risk: Results from a systematic review and meta-analysis. Int. J. Biol. Markers 2014, 29, e21–e29. [Google Scholar] [CrossRef]
- Gallos, I.D.; Ganesan, R.; Gupta, J.K. Prediction of regression and relapse of endometrial hyperplasia with conservative therapy. Obstet. Gynecol. 2013, 121, 1165–1171. [Google Scholar] [CrossRef]
- World Cancer Research Fund; American Institute for Cancer Research. Food, Nutrition, Physical Activity, and the Prevention of Cancer: A Global Perspective; American Institute for Cancer Research: Washington, DC, USA, 2007. [Google Scholar]
- Backes, F.J.; Cohn, D.E. Lynch syndrome. Clin. Obstet. Gynecol. 2011, 54, 199–214. [Google Scholar] [CrossRef]
- Corzo, C.; Santillan, N.B.; Westin, S.N.; Ramirez, P.T. Updates on Conservative Management of Endometrial Cancer. J. Minim. Invasive Gynecol. 2018, 25, 308–313. [Google Scholar] [CrossRef]
- Staff, S.; Aaltonen, M.; Huhtala, H.; Pylvänäinen, K.; Mecklin, J.P.; Mäenpää, J. Endometrial cancer risk factors among Lynch syndrome women: A retrospective cohort study. Br. J. Cancer 2016, 115, 375–381. [Google Scholar] [CrossRef] [Green Version]
- Assikis, V.J.; Neven, P.; Jordan, V.C.; Vergote, I. A realistic clinical perspective of tamoxifen and endometrial carcinogenesis. Eur. J. Cancer 1996, 32, 1464–1476. [Google Scholar] [CrossRef]
- Kim, H.S.; Jeon, Y.T.; Kim, Y.B. The effect of adjuvant hormonal therapy on the endometrium and ovary of breast cancer patients. J. Gynecol. Oncol. 2008, 19, 256–260. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Cancer Institute. Endometrial Cancer Screening Physician Data Query (PDQ). 2015. Available online: www.cancer.gov/cancertopics/pdq/screening/endometrial/HealthProfessional/ (accessed on 22 November 2021).
- Colombo, N.; Creutzberg, C.; Amant, F.; Bosse, T.; González-Martín, A.; Ledermann, J.; Marth, C.; Nout, R.; Querleu, D.; Mirza, M.R.; et al. ESMO-ESGO-ESTRO Consensus Conference on Endometrial Cancer: Diagnosis, treatment and follow-up. Ann. Oncol. 2016, 27, 16–41, Erratum in Ann. Oncol. 2017, 28 (Suppl. 4), iv167–iv168. [Google Scholar] [CrossRef]
- Provenzale, D.; Gupta, S.; Ahnen, D.J.; Bray, T.; Cannon, J.A.; Cooper, G.; David, D.S.; Early, D.S.; Erwin, D.; Ford, J.M.; et al. Genetic/Familial High-Risk Assessment: Colorectal Version 1.2016, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Canc. Netw. 2016, 14, 1010–1030. [Google Scholar] [CrossRef] [PubMed]
- Pennant, M.E.; Mehta, R.; Moody, P.; Hackett, G.; Prentice, A.; Sharp, S.J.; Lakshman, R. Premenopausal abnormal uterine bleeding and risk of endometrial cancer. BJOG 2017, 124, 404–411. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sardo, A.D.S.; De Angelis, M.C.; Della Corte, L.; Carugno, J.; Zizolfi, B.; Guadagno, E.; Gencarelli, A.; Cecchi, E.; Simoncini, T.; Bifulco, G.; et al. Should endometrial biopsy under direct hysteroscopic visualization using the grasp technique become the new gold standard for the preoperative evaluation of the patient with endometrial cancer? Gynecol. Oncol. 2020, 158, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Rodolakis, A.; Biliatis, I.; Morice, P.; Reed, N.; Mangler, M.; Kesic, V.; Denschlag, D. European Society of Gynecological Oncology Task Force for Fertility Preservation: Clinical Recommendations for Fertility-Sparing Management in Young Endometrial Cancer Patients. Int. J. Gynecol. Cancer 2015, 25, 1258–1265. [Google Scholar] [CrossRef] [PubMed]
- Falcone, F.; Laurelli, G.; Losito, S.; Di Napoli, M.; Granata, V.; Greggi, S. Fertility preserving treatment with hysteroscopic resection followed by progestin therapy in young women with early endometrial cancer. J. Gynecol. Oncol. 2017, 28, e2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Auclair, M.H.; Yong, P.J.; Salvador, S.; Thurston, J.; Colgan, T.T.J.; Sebastianelli, A. Guideline No. 392-Classification and Management of Endometrial Hyperplasia. J. Obstet. Gynaecol. Can. 2019, 41, 1789–1800, Erratum in J. Obstet. Gynaecol. Can. 2020, 42, 1287. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goldstein, S.R. Modern evaluation of the endometrium. Obstet. Gynecol. 2010, 116, 168–176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bettocchi, S.; Ceci, O.; Vicino, M.; Marello, F.; Impedovo, L.; Selvaggi, L. Diagnostic inadequacy of dilatation and curettage. Fertil. Steril. 2001, 75, 803–805. [Google Scholar] [CrossRef]
- Ramshaw, N.; Narayansingh, G. The implications of hysteroscopy in the updated guidelines on heavy menstrual bleeding from the UK National Institute for Health and Care Excellence (NICE). Case Rep. Women’s Health 2019, 22, e00117. [Google Scholar] [CrossRef] [PubMed]
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines); Uterine Neoplasms; Version 3.2021; National Comprehensive Cancer Network: Plymouth, PA, USA, 2021. [Google Scholar]
- Manfredi, R.; Mirk, P.; Maresca, G.; Margariti, P.A.; Testa, A.; Zannoni, G.F.; Giordano, D.; Scambia, G.; Marano, P. Local-regional staging of endometrial carcinoma: Role of MR imaging in surgical planning. Radiology 2004, 231, 372–378. [Google Scholar] [CrossRef] [Green Version]
- Savelli, L.; Ceccarini, M.; Ludovisi, M.; Fruscella, E.; De Iaco, P.A.; Salizzoni, E.; Mabrouk, M.; Manfredi, R.; Testa, A.C.; Ferrandina, G. Preoperative local staging of endometrial cancer: Transvaginal sonography vs. magnetic resonance imaging. Ultrasound Obstet. Gynecol. 2008, 31, 560–566. [Google Scholar] [CrossRef]
- Eriksson, L.S.; Lindqvist, P.G.; Flöter Rådestad, A.; Dueholm, M.; Fischerova, D.; Franchi, D.; Jokubkiene, L.; Leone, F.P.; Savelli, L.; Sladkevicius, P.; et al. Transvaginal ultrasound assessment of myometrial and cervical stromal invasion in women with endometrial cancer: Interobserver reproducibility among ultrasound experts and gynecologists. Ultrasound Obstet. Gynecol. 2015, 45, 476–482. [Google Scholar] [CrossRef] [Green Version]
- McKenzie, N.D.; Kennard, J.A.; Ahmad, S. Fertility preserving options for gynecologic malignancies: A review of current understanding and future directions. Crit. Rev. Oncol. Hematol. 2018, 132, 116–124. [Google Scholar] [CrossRef]
- Coakley, K.; Wolford, J.; Tewari, K.S. Fertility preserving treatment for gynecologic malignancies: A review of recent literature. Curr. Opin. Obstet. Gynecol. 2020, 32, 51–56. [Google Scholar] [CrossRef]
- Ramirez, P.T.; Frumovitz, M.; Bodurka, D.C.; Sun, C.C.; Levenback, C. Hormonal therapy for the management of grade 1 endometrial adenocarcinoma: A literature review. Gynecol. Oncol. 2004, 95, 133–138. [Google Scholar] [CrossRef]
- Mazzon, I.; Corrado, G.; Masciullo, V.; Morricone, D.; Ferrandina, G.; Scambia, G. Conservative surgical management of stage 1A endometrial carcinoma for fertility preservation. Fertil. Steril. 2010, 93, 1286–1289. [Google Scholar] [CrossRef]
- Concin, N.; Matias-Guiu, X.; Vergote, I.; Cibula, D.; Raza Mirza, M.; Marnitz, S.; Ledermann, J.; Bosse, T.; Chargari, C.; Fagotti, A.; et al. ESGO/ESTRO/ESP guidelines for the management of patients with endometrial carcinoma. Int. J. Gynecol. Cancer 2020, 31, 12–39. [Google Scholar] [CrossRef]
- Giampaolino, P.; Di Spiezio Sardo, A.; Mollo, A.; Raffone, A.; Travaglino, A.; Boccellino, A.; Zizolfi, B.; Insabato, L.; Zullo, F.; De Placido, G.; et al. Hysteroscopic Endometrial Focal Resection followed by Levonorgestrel Intrauterine Device Insertion as a Fertility-Sparing Treatment of Atypical Endometrial Hyperplasia and Early Endometrial Cancer: A Retrospective Study. J. Minim. Invasive Gynecol. 2019, 26, 648–656. [Google Scholar] [CrossRef]
- Masciullo, V.; Trivellizzi, N.; Zannoni, G.; Catena, U.; Moroni, R.; Fanfani, F.; Scambia, G. Prognostic impact of hysteroscopic resection of endometrial atypical hyperplasia-endometrioid intraepithelial neoplasia and early-stage cancer in combination with megestrol acetate. Am. J. Obstet. Gynecol. 2021, 224, 408–410. [Google Scholar] [CrossRef] [PubMed]
- Mazzon, I.; Corrado, G.; Morricone, D.; Scambia, G. Reproductive preservation for treatment of stage IA endometrial cancer in a young woman: Hysteroscopic resection. Int. J. Gynecol. Cancer 2005, 15, 974–978. [Google Scholar] [CrossRef]
- De Rijk, S.R.; Steenbergen, M.E.; Nieboer, T.E.; Coppus, S.F. Atypical Endometrial Polyps and Concurrent Endometrial Cancer: A Systematic Review. Obstet. Gynecol. 2016, 128, 519–525. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, I.; Tibosch, R.; Geomini, P.; Coppus, S.; Bongers, M.Y.; van Hanegem, N. Atypical endometrial polyps and the incidence of endometrial cancer: A retrospective cohort study. BJOG 2020, 127, 994–999. [Google Scholar] [CrossRef]
- Obermair, A.; Baxter, E.; Brennan, D.J.; McAlpine, J.N.; Muellerer, J.J.; Amant, F.; van Gent, M.D.J.M.; Coleman, R.L.; Westin, S.N.; Yates, M.S.; et al. Fertility-sparing treatment in early endometrial cancer: Current state and future strategies. Obstet. Gynecol. Sci. 2020, 63, 417–431. [Google Scholar] [CrossRef] [PubMed]
- Koskas, M.; Uzan, J.; Luton, D.; Rouzier, R.; Daraï, E. Prognostic factors of oncologic and reproductive outcomes in fertility-sparing management of endometrial atypical hyperplasia and adenocarcinoma: Systematic review and meta-analysis. Fertil. Steril. 2014, 101, 785–794. [Google Scholar] [CrossRef]
- Gallos, I.D.; Yap, J.; Rajkhowa, M.; Luesley, D.M.; Coomarasamy, A.; Gupta, J.K. Regression, relapse, and live birth rates with fertility-sparing therapy for endometrial cancer and atypical complex endometrial hyperplasia: A systematic review and metaanalysis. Am. J. Obstet. Gynecol. 2012, 207, 266.e1–266.e12. [Google Scholar] [CrossRef]
- Eskander, R.N.; Randall, L.M.; Berman, M.L.; Tewari, K.S.; Disaia, P.J.; Bristow, R.E. Fertility preserving options in patients with gynecologic malignancies. Am. J. Obstet. Gynecol. 2011, 205, 103–110. [Google Scholar] [CrossRef] [Green Version]
- Wei, J.; Zhang, W.; Feng, L.; Gao, W. Comparison of fertility-sparing treatments in patients with early endometrial cancer and atypical complex hyperplasia: A meta-analysis and systematic review. Medicine 2017, 96, e8034. [Google Scholar] [CrossRef] [PubMed]
- Gallos, I.D.; Shehmar, M.; Thangaratinam, S.; Papapostolou, T.K.; Coomarasamy, A.; Gupta, J.K. Oral progestogens vs levonorgestrel-releasing intrauterine system for endometrial hyperplasia: A systematic review and metaanalysis. Am. J. Obstet. Gynecol. 2010, 203, 547.e1–547.e10. [Google Scholar] [CrossRef] [PubMed]
- Fan, Z.; Li, H.; Hu, R.; Liu, Y.; Liu, X.; Gu, L. Fertility-Preserving Treatment in Young Women With Grade 1 Presumed Stage IA Endometrial Adenocarcinoma: A Meta-Analysis. Int. J. Gynecol. Cancer 2018, 28, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Travaglino, A.; Raffone, A.; Saccone, G.; Insabato, L.; Mollo, A.; De Placido, G.; Zullo, F. Immunohistochemical predictive markers of response to conservative treatment of endometrial hyperplasia and early endometrial cancer: A systematic review. Acta Obstet. Gynecol. Scand. 2019, 98, 1086–1099. [Google Scholar] [CrossRef]
- The Cancer Genome Atlas Research Network; Schultz, N.; Cherniack, A.D.; Akbani, R.; Liu, Y.; Shen, H.; Robertson, A.G.; Pashtan, I.; Shen, R.; Benz, C.C.; et al. Integrated genomic characterization of endometrial carcinoma. Nature 2013, 497, 67–73, Erratum in Nature 2013, 500, 242. [Google Scholar] [CrossRef]
- Kommoss, S.; McConechy, M.K.; Kommoss, F.; Leung, S.; Bunz, A.; Magrill, J.; Britton, H.; Kommoss, F.; Grevenkamp, F.; Karnezis, A.; et al. Final validation of the ProMisE molecular classifier for endometrial carcinoma in a large population-based case series. Ann. Oncol. 2018, 29, 1180–1188. [Google Scholar] [CrossRef]
- Talhouk, A.; Hoang, L.N.; McConechy, M.K.; Nakonechny, Q.; Leo, J.; Cheng, A.; Leung, S.; Yang, W.; Lum, A.; Köbel, M.; et al. Molecular classification of endometrial carcinoma on diagnostic specimens is highly concordant with final hysterectomy: Earlier prognostic information to guide treatment. Gynecol. Oncol. 2016, 143, 46–53. [Google Scholar] [CrossRef] [Green Version]
- Falcone, F.; Normanno, N.; Losito, N.S.; Scognamiglio, G.; Abate, R.E.; Chicchinelli, N.; Casella, G.; Laurelli, G.; Scaffa, C.; Greggi, S. Application of the Proactive Molecular Risk Classifier for Endometrial Cancer (ProMisE) to patients conservatively treated: Outcomes from an institutional series. Eur. J. Obstet. Gynecol. Reprod. Biol. 2019, 240, 220–225. [Google Scholar] [CrossRef] [PubMed]
- Raffone, A.; Catena, U.; Travaglino, A.; Masciullo, V.; Spadola, S.; Della Corte, L.; Piermattei, A.; Insabato, L.; Zannoni, G.F.; Scambia, G.; et al. Mismatch repair-deficiency specifically predicts recurrence of atypical endometrial hyperplasia and early endometrial carcinoma after conservative treatment: A multi-center study. Gynecol. Oncol. 2021, 161, 795–801. [Google Scholar] [CrossRef]
- Casadio, P.; Guasina, F.; Paradisi, R.; Leggieri, C.; Caprara, G.; Seracchioli, R. Fertility-Sparing Treatment of Endometrial Cancer with Initial Infiltration of Myometrium by Resectoscopic Surgery: A Pilot Study. Oncologist 2018, 23, 478–480. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Falcone, F.; Leone Roberti Maggiore, U.; Di Donato, V.; Perrone, A.M.; Frigerio, L.; Bifulco, G.; Polterauer, S.; Casadio, P.; Cormio, G.; Masciullo, V.; et al. Fertility-sparing treatment for intramucous, moderately differentiated, endometrioid endometrial cancer: A Gynecologic Cancer Inter-Group (GCIG) study. J. Gynecol. Oncol. 2020, 31, e74. [Google Scholar] [CrossRef]
- Hwang, J.Y.; Kim, D.H.; Bae, H.S.; Kim, M.L.; Jung, Y.W.; Yun, B.S.; Seong, S.J.; Shin, E.; Kim, M.K. Combined Oral Medroxyprogesterone/Levonorgestrel-Intrauterine System Treatment for Women with Grade 2 Stage IA Endometrial Cancer. Int. J. Gynecol. Cancer 2017, 27, 738–742. [Google Scholar] [CrossRef]
- Zuckerman, B.; Lavie, O.; Neuman, M.; Rabinowitz, R.; Ben-Chetrit, A.; Voss, E.; Rosenmann, E.; Beller, U. Endometrial carcinoma Stage I-Grade II. Conservative treatment followed by a healthy twin pregnancy. Int. J. Gynecol. Cancer 1998, 8, 172–174. [Google Scholar] [CrossRef]
- Koskas, M.; Yazbeck, C.; Walker, F.; Clouqueur, E.; Agostini, A.; Ruat, S.; Lucot, J.P.; Lambaudie, E.; Luton, D.; Madelenat, P. Fertility-sparing management of grade 2 and 3 endometrial adenocarcinomas. Anticancer Res. 2011, 31, 3047–3049. [Google Scholar]
- Park, J.Y.; Kim, D.Y.; Kim, T.J.; Kim, J.W.; Kim, J.H.; Kim, Y.M.; Kim, Y.T.; Bae, D.S.; Nam, J.H. Hormonal therapy for women with stage IA endometrial cancer of all grades. Obstet. Gynecol. 2013, 122, 7–14. [Google Scholar] [CrossRef]
- Kim, M.K.; Seong, S.J.; Kim, Y.S.; Song, T.; Kim, M.L.; Yoon, B.S.; Jun, H.S.; Lee, Y.H. Combined medroxyprogesterone acetate/levonorgestrel-intrauterine system treatment in young women with early-stage endometrial cancer. Am. J. Obstet. Gynecol. 2013, 209, 358.e1–358.e4. [Google Scholar] [CrossRef] [PubMed]
| First Author and Year | N. of Patient | Histology | Type of Treatment | Complete Response Rate | Recurrence Rate | Pregnancy Rate | Live Birth Rate |
|---|---|---|---|---|---|---|---|
| Ramirez 2004 | 81 | EEC | OP | 76% | 24% | N.A. | N.A. |
| Gallos 2012 | 559 | 408 EEC 151 AEH | N.A. | 76.2% 85.6% | 40.6% 26% | N.A. N.A. | 28% 26.3% |
| Falcone 2017 | 28 | EEC | HR + OP/HR + LNG-IUS | 96.3% | 7.7% | 93.3% 1 | 86.6% 1 |
| Fan 2017 | 619 | EEC | HR + OP OP LNG-IUS | 95.3% 76.3% 72.9% | 14.1% 30.7% 11% | 47.8% 52.1% 56% | N.A N.A. N.A. |
| Wei 2017 | 1038 | EEC/AEH | OP LNG-IUS OP + LNG-IUS | 71% 76% 87% | 20% 9% N.A. | 34% 18% 40% | 20% 14% 35% |
| Giampaolino 2018 | 69 | 14 EEC 55 AEH | HR + LNG-IUS | 78.6% 92.7% | 18.2% 3.9% | 0% 26.3% 1 | 0% 26.3% 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gallo, A.; Catena, U.; Saccone, G.; Di Spiezio Sardo, A. Conservative Surgery in Endometrial Cancer. J. Clin. Med. 2022, 11, 183. https://doi.org/10.3390/jcm11010183
Gallo A, Catena U, Saccone G, Di Spiezio Sardo A. Conservative Surgery in Endometrial Cancer. Journal of Clinical Medicine. 2022; 11(1):183. https://doi.org/10.3390/jcm11010183
Chicago/Turabian StyleGallo, Alessandra, Ursula Catena, Gabriele Saccone, and Attilio Di Spiezio Sardo. 2022. "Conservative Surgery in Endometrial Cancer" Journal of Clinical Medicine 11, no. 1: 183. https://doi.org/10.3390/jcm11010183
APA StyleGallo, A., Catena, U., Saccone, G., & Di Spiezio Sardo, A. (2022). Conservative Surgery in Endometrial Cancer. Journal of Clinical Medicine, 11(1), 183. https://doi.org/10.3390/jcm11010183






