Invasive Assessment of Coronary Microvascular Function
Abstract
:1. Introduction
2. Coronary Microvascular Dysfunction (CMD)
2.1. Phenotypes and Pathophysiological Mechanisms
2.2. Clinical Presentation
3. Coronary Flow Reserve (CFR)
4. Index of Microcirculatory Resistance (IMR)
5. Hyperemic Microvascular Resistance (HMR)
6. Other Hyperemic Methods of CMD Assessment
6.1. Minimal Microvascular Resistance (mMR)
6.2. Resistive Reserve Ratio (RRR)
7. Absolute Coronary Flow and Resistance
8. Clinical Utility of Microvascular Function Assessment and Future Perspectives
9. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Vancheri, F.; Longo, G.; Vancheri, S.; Henein, M. Coronary Microvascular Dysfunction. J. Clin. Med. 2020, 9, 2880. [Google Scholar] [CrossRef]
- Layland, J.; Nerlekar, N.; Palmer, S.; Berry, C.; Oldroyd, K. Invasive assessment of the coronary microcirculation in the catheter laboratory. Int. J. Cardiol. 2015, 199, 141–149. [Google Scholar] [CrossRef] [PubMed]
- Sorop, O.; Van Den Heuvel, M.; Van Ditzhuijzen, N.S.; De Beer, V.J.; Heinonen, I.; Van Duin, R.W.B.; Zhou, Z.; Koopmans, S.J.; Merkus, D.; Van Der Giessen, W.J.; et al. Coronary microvascular dysfunction after long-term diabetes and hypercholesterolemia. Am. J. Physiol. Heart Circ. Physiol. 2016, 311, 1339–1351. [Google Scholar] [CrossRef] [Green Version]
- Hubert, A.; Seitz, A.; Pereyra, V.M.; Bekeredjian, R.; Sechtem, U.; Ong, P. Coronary artery spasm: The interplay between endothelial dysfunction and vascular smooth muscle cell hyperreactivity. Eur. Cardiol. Rev. 2020, 15, e12. [Google Scholar] [CrossRef] [PubMed]
- Konst, R.E.; Damman, P.; Pellegrini, D.; Hartzema-Meijer, M.J.; van Uden, B.J.C.; Jansen, T.P.J.; Brandsma, J.; Vart, P.; Gehlmann, H.; Maas, A.H.E.M.; et al. Vasomotor dysfunction in patients with angina and nonobstructive coronary artery disease is dominated by vasospasm. Int. J. Cardiol. 2021, 333, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Montone, R.A.; Niccoli, G.; Fracassi, F.; Russo, M.; Gurgoglione, F.; Cammà, G.; Lanza, G.A.; Crea, F. Patients with acute myocardial infarction and non-obstructive coronary arteries: Safety and prognostic relevance of invasive coronary provocative tests. Eur. Heart J. 2018, 39, 91–98. [Google Scholar] [CrossRef]
- Ong, P.; Camici, P.G.; Beltrame, J.F.; Crea, F.; Shimokawa, H.; Sechtem, U.; Kaski, J.C.; Bairey Merz, C.N. International standardization of diagnostic criteria for microvascular angina. Int. J. Cardiol. 2018, 250, 16–20. [Google Scholar] [CrossRef] [PubMed]
- Pries, A.R.; Badimon, L.; Bugiardini, R.; Camici, P.G.; Dorobantu, M.; Duncker, D.J.; Escaned, J.; Koller, A.; Piek, J.J.; De Wit, C. Coronary vascular regulation, remodelling, and collateralization: Mechanisms and clinical implications on behalf of the working group on coronary pathophysiology and microcirculation. Eur. Heart J. 2015, 36, 3134–3146. [Google Scholar] [CrossRef] [Green Version]
- Piccirillo, F.; Carpenito, M.; Verolino, G.; Chello, C.; Nusca, A.; Lusini, M.; Spadaccio, C.; Nappi, F.; Di Sciascio, G.; Nenna, A. Changes of the coronary arteries and cardiac microvasculature with aging: Implications for translational research and clinical practice. Mech. Ageing Dev. 2019, 184, 111161. [Google Scholar] [CrossRef]
- Kunadian, V.; Chieffo, A.; Camici, P.G.; Berry, C.; Escaned, J.; Maas, A.H.E.M.; Prescott, E.; Karam, N.; Appelman, Y.; Fraccaro, C.; et al. An EAPCI expert consensus document on ischaemia with non-obstructive coronary arteries in collaboration with european society of cardiology working group on coronary pathophysiology & microcirculation endorsed by coronary vasomotor disorders international study group. EuroIntervention 2021, 16, 1049–1069. [Google Scholar] [CrossRef]
- Koller, A. Perspectives: Microvascular endothelial dysfunction and gender. Eur. Heart J. Suppl. 2014, 16, 30–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hinkel, R.; Hoewe, A.; Renner, S.; Ng, J.; Lee, S.; Klett, K.; Kaczmarek, V.; Moretti, A.; Laugwitz, K.L.; Skroblin, P.; et al. Diabetes Mellitus–Induced Microvascular Destabilization in the Myocardium. J. Am. Coll. Cardiol. 2017, 69, 131–143. [Google Scholar] [CrossRef] [PubMed]
- Triantafyllou, A.; Anyfanti, P.; Triantafyllou, G.; Zabulis, X.; Aslanidis, S.; Douma, S. Impaired metabolic profile is a predictor of capillary rarefaction in a population of hypertensive and normotensive individuals. J. Am. Soc. Hypertens. 2016, 10, 640–646. [Google Scholar] [CrossRef] [PubMed]
- Alonso, R.; Mata, P.; De Andres, R.; Villacastin, B.P.; Martínez-González, J.; Badimon, L. Sustained long-term improvement of arterial endothelial function in heterozygous familial hypercholesterolemia patients treated with simvastatin. Atherosclerosis 2001, 157, 423–429. [Google Scholar] [CrossRef]
- Hein, T.W.; Liao, J.C.; Kuo, L. oxLDL specifically impairs endothelium-dependent, NO-mediated dilation of coronary arterioles. Am. J. Physiol. Heart Circ. Physiol. 2000, 278, H175–H183. [Google Scholar] [CrossRef]
- Konst, R.E.; Guzik, T.J.; Kaski, J.C.; Maas, A.H.E.M.; Elias-Smale, S.E. The pathogenic role of coronary microvascular dysfunction in the setting of other cardiac or systemic conditions. Cardiovasc. Res. 2020, 116, 817–828. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Layland, J.; Carrick, D.; Lee, M.; Oldroyd, K.; Berry, C. Adenosine: Physiology, pharmacology, and clinical applications. JACC Cardiovasc. Interv. 2014, 7, 581–591. [Google Scholar] [CrossRef] [Green Version]
- Everaars, H.; de Waard, G.A.; Driessen, R.S.; Danad, I.; van de Ven, P.M.; Raijmakers, P.G.; Lammertsma, A.A.; van Rossum, A.C.; Knaapen, P.; van Royen, N. Doppler Flow Velocity and Thermodilution to Assess Coronary Flow Reserve: A Head-to-Head Comparison with [15O]H2O PET. JACC Cardiovasc. Interv. 2018, 11, 2044–2054. [Google Scholar] [CrossRef]
- Hozumi, T.; Yoshida, K.; Akasaka, T.; Asami, Y.; Ogata, Y.; Takagi, T.; Kaji, S.; Kawamoto, T.; Ueda, Y.; Morioka, S. Noninvasive assessment of coronary flow velocity and coronary flow velocity reserve in the left anterior descending coronary artery by Doppler echocardiography: Comparison with invasive technique. J. Am. Coll. Cardiol. 1998, 32, 1251–1259. [Google Scholar] [CrossRef] [Green Version]
- Hozumi, T.; Yoshida, K.; Ogata, Y.; Akasaka, T.; Asami, Y.; Takagi, T.; Morioka, S. Noninvasive assessment of significant left anterior descending coronary artery stenosis by coronary flow velocity reserve with transthoracic color doppler echocardiography. Circulation 1998, 97, 1557–1562. [Google Scholar] [CrossRef] [Green Version]
- Okura, H.; Fuyuki, H.; Kubo, T.; Iwata, K.; Taguchi, H.; Toda, I.; Yoshikawa, J. Noninvasive Diagnosis of Ischemic and Nonischemic Cardiomyopathy Using Coronary Flow Velocity Measurements of the Left Anterior Descending Coronary Artery by Transthoracic Doppler Echocardiography. J. Am. Soc. Echocardiogr. 2006, 19, 552–558. [Google Scholar] [CrossRef] [PubMed]
- Meimoun, P.; Tribouilloy, C. Non-invasive assessment of coronary flow and coronary flow reserve by transthoracic Doppler echocardiography: A magic tool for the real world. Eur. J. Echocardiogr. 2008, 9, 449–457. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fearon, W.F.; Farouque, H.M.O.; Balsam, L.B.; Cooke, D.T.; Robbins, R.C.; Fitzgerald, P.J.; Yeung, A.C.; Yock, P.G. Comparison of Coronary Thermodilution and Doppler Velocity for Assessing Coronary Flow Reserve. Circulation 2003, 108, 2198–2200. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barbato, E.; Aarnoudse, W.; Aengevaeren, W.R.; Werner, G.; Klauss, V.; Bojara, W.; Herzfeld, I.; Oldroyd, K.G.; Pijls, N.H.J.; De Bruyne, B. Validation of coronary flow reserve measurements by thermodilution in clinical practice. Eur. Heart J. 2004, 25, 219–223. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Bruyne, B.; Pijls, N.H.J.; Smith, L.; Wievegg, M.; Heyndrickx, G.R. Coronary Thermodilution to Assess Flow Reserve Experimental Validation. Circulation 2001, 104, 2003–2006. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pijls, N.H.J.; De Bruyne, B.; Smith, L.; Aarnoudse, W.; Barbato, E.; Bartunek, J.; Bech, G.J.W.; Van De Vosse, F. Coronary thermodilution to assess flow reserve: Validation in humans. Circulation 2002, 105, 2482–2486. [Google Scholar] [CrossRef]
- Lee, J.M.; Jung, J.H.; Hwang, D.; Park, J.; Fan, Y.; Na, S.H.; Doh, J.H.; Nam, C.W.; Shin, E.S.; Koo, B.K. Coronary Flow Reserve and Microcirculatory Resistance in Patients with Intermediate Coronary Stenosis. J. Am. Coll. Cardiol. 2016, 67, 1158–1169. [Google Scholar] [CrossRef] [PubMed]
- Usui, E.; Murai, T.; Kanaji, Y.; Hoshino, M.; Yamaguchi, M.; Hada, M.; Hamaya, R.; Kanno, Y.; Lee, T.; Yonetsu, T.; et al. Clinical significance of concordance or discordance between fractional flow reserve and coronary flow reserve for coronary physiological indices, microvascular resistance, and prognosis after elective percutaneous coronary intervention. EuroIntervention 2018, 14, 798–805. [Google Scholar] [CrossRef]
- AlBadri, A.; Bairey Merz, C.N.; Johnson, B.D.; Wei, J.; Mehta, P.K.; Cook-Wiens, G.; Reis, S.E.; Kelsey, S.F.; Bittner, V.; Sopko, G.; et al. Impact of Abnormal Coronary Reactivity on Long-Term Clinical Outcomes in Women. J. Am. Coll. Cardiol. 2019, 73, 684–693. [Google Scholar] [CrossRef]
- Van De Hoef, T.P.; Van Lavieren, M.A.; Damman, P.; Delewi, R.; Piek, M.A.; Chamuleau, S.A.J.; Voskuil, M.; Henriques, J.P.S.; Koch, K.T.; De Winter, R.J.; et al. Physiological basis and long-term clinical outcome of discordance between fractional flow reserve and coronary flow velocity reserve in coronary stenoses of intermediate severity. Circ. Cardiovasc. Interv. 2014, 7, 301–311. [Google Scholar] [CrossRef] [Green Version]
- Indorkar, R.; Kwong, R.Y.; Romano, S.; White, B.E.; Chia, R.C.; Trybula, M.; Evans, K.; Shenoy, C.; Farzaneh-Far, A. Global Coronary Flow Reserve Measured during Stress Cardiac Magnetic Resonance Imaging Is an Independent Predictor of Adverse Cardiovascular Events. JACC Cardiovasc. Imaging 2019, 12, 1686–1695. [Google Scholar] [CrossRef] [PubMed]
- Murthy, V.L.; Bateman, T.M.; Beanlands, R.S.; Berman, D.S.; Borges-Neto, S.; Chareonthaitawee, P.; Cerqueira, M.D.; deKemp, R.A.; DePuey, E.G.; Dilsizian, V.; et al. Clinical Quantification of Myocardial Blood Flow Using PET: Joint Position Paper of the SNMMI Cardiovascular Council and the ASNC. J. Nucl. Cardiol. 2018, 25, 269–297. [Google Scholar] [CrossRef] [Green Version]
- Murthy, V.L.; Naya, M.; Foster, C.R.; Hainer, J.; Gaber, M.; Di Carli, G.; Blankstein, R.; Dorbala, S.; Sitek, A.; Pencina, M.J.; et al. Improved cardiac risk assessment with noninvasive measures of coronary flow reserve. Circulation 2011, 124, 2215–2224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gibson, C.M.; Cannon, C.P.; Daley, W.L.; Dodge, J.T.; Alexander, B.; Marble, S.J.; McCabe, C.H.; Raymond, L.; Fortin, T.; Poole, W.K.; et al. TIMI frame count: A quantitative method of assessing coronary artery flow. Circulation 1996, 93, 879–888. [Google Scholar] [CrossRef] [PubMed]
- Ong, P.; Safdar, B.; Seitz, A.; Hubert, A.; Beltrame, J.F.; Prescott, E. Diagnosis of coronary microvascular dysfunction in the clinic. Cardiovasc. Res. 2020, 116, 841–855. [Google Scholar] [CrossRef] [PubMed]
- Johnson, N.P.; Kirkeeide, R.L.; Gould, K.L. Is discordance of coronary flow reserve and fractional flow reserve due to methodology or clinically relevant coronary pathophysiology? JACC Cardiovasc. Imaging 2012, 5, 193–202. [Google Scholar] [CrossRef] [Green Version]
- Ahn, S.G.; Suh, J.; Hung, O.Y.; Lee, H.S.; Bouchi, Y.H.; Zeng, W.; Gandhi, R.; Eshtehardi, P.; Gogas, B.D.; Samady, H. Discordance between Fractional Flow Reserve and Coronary Flow Reserve: Insights from Intracoronary Imaging and Physiological Assessment. JACC Cardiovasc. Interv. 2017, 10, 999–1007. [Google Scholar] [CrossRef]
- Stegehuis, V.E.; Wijntjens, G.W.M.; van de Hoef, T.P.; Casadonte, L.; Kirkeeide, R.L.; Siebes, M.; Spaan, J.A.E.; Gould, K.L.; Johnson, N.P.; Piek, J.J. Distal Evaluation of Functional performance with Intravascular sensors to assess the Narrowing Effect—Combined pressure and Doppler FLOW velocity measurements (DEFINE-FLOW) trial: Rationale and trial design. Am. Heart J. 2020, 222, 139–146. [Google Scholar] [CrossRef]
- Fearon, W.F.; Balsam, L.B.; Farouque, H.M.O.; Robbins, R.C.; Fitzgerald, P.J.; Yock, P.G.; Yeung, A.C. Novel index for invasively assessing the coronary microcirculation. Circulation 2003, 107, 3129–3132. [Google Scholar] [CrossRef]
- Fearon, W.F.; Kobayashi, Y. Invasive Assessment of the Coronary Microvasculature: The Index of Microcirculatory Resistance. Circ. Cardiovasc. Interv. 2017, 10, e005361. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, Y.; Fearon, W.F. Invasive coronary microcirculation assessment—Current status of index of microcirculatory resistance. Circ. J. 2014, 78, 1021–1028. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fearon, W.F.; Aarnoudse, W.; Pijls, N.H.J.; De Bruyne, B.; Balsam, L.B.; Cooke, D.T.; Robbins, R.C.; Fitzgerald, P.J.; Yeung, A.C.; Yock, P.G. Microvascular resistance is not influenced by epicardial coronary artery stenosis severity: Experimental validation. Circulation 2004, 109, 2269–2272. [Google Scholar] [CrossRef] [PubMed]
- Yong, A.S.C.; Ho, M.; Shah, M.G.; Ng, M.K.C.; Fearon, W.F. Coronary microcirculatory resistance is independent of epicardial stenosis. Circ. Cardiovasc. Interv. 2012, 5, 103–108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Layland, J.; MacIsaac, A.I.; Burns, A.T.; Somaratne, J.B.; Leitl, G.; Whitbourn, R.J.; Wilson, A.M. When collateral supply is accounted for epicardial stenosis does not increase microvascular resistance. Circ. Cardiovasc. Interv. 2012, 5, 97–102. [Google Scholar] [CrossRef] [Green Version]
- Nolte, F.; Van De Hoef, T.P.; Meuwissen, M.; Voskuil, M.; Chamuleau, S.A.J.; Henriques, J.P.S.; Verberne, H.J.; Van Eck-Smit, B.L.F.; Koch, K.T.; De Winter, R.J.; et al. Increased hyperaemic coronary microvascular resistance adds to the presence of myocardial ischaemia. EuroIntervention 2014, 9, 1423–1431. [Google Scholar] [CrossRef] [PubMed]
- Waard, G.A.; Fahrni, G.; De Wit, D.; Kitabata, H.; Williams, R.; Patel, N.; Teunissen, P.F.; Van De Ven, P.M.; Umman, S.; Knaapen, P.; et al. Hyperaemic microvascular resistance predicts clinical outcome and microvascular injury after myocardial infarction. Heart 2018, 104, 127–134. [Google Scholar] [CrossRef]
- Sheikh, A.R.; Zeitz, C.J.; Rajendran, S.; Di Fiore, D.P.; Tavella, R.; Beltrame, J.F. Clinical and coronary haemodynamic determinants of recurrent chest pain in patients without obstructive coronary artery disease—A pilot study. Int. J. Cardiol. 2018, 267, 16–21. [Google Scholar] [CrossRef]
- Williams, R.P.; de Waard, G.A.; De Silva, K.; Lumley, M.; Asrress, K.; Arri, S.; Ellis, H.; Mir, A.; Clapp, B.; Chiribiri, A.; et al. Doppler Versus Thermodilution-Derived Coronary Microvascular Resistance to Predict Coronary Microvascular Dysfunction in Patients with Acute Myocardial Infarction or Stable Angina Pectoris. Am. J. Cardiol. 2018, 121, 1–8. [Google Scholar] [CrossRef] [Green Version]
- de Waard, G.A.; Nijjer, S.S.; van Lavieren, M.A.; van der Hoeven, N.W.; Petraco, R.; van de Hoef, T.P.; Echavarria-Pinto, M.; Sen, S.; van de Ven, P.M.; Knaapen, P.; et al. Invasive minimal Microvascular Resistance is a New Index to Assess Microcirculatory Function Independent of Obstructive Coronary Artery Disease. J. Am. Heart Assoc. 2016, 5, e004482. [Google Scholar] [CrossRef] [Green Version]
- Maznyczka, A.M.; Oldroyd, K.G.; Greenwood, J.P.; McCartney, P.J.; Cotton, J.; Lindsay, M.; McEntegart, M.; Rocchiccioli, J.P.; Good, R.; Robertson, K.; et al. Comparative Significance of Invasive Measures of Microvascular Injury in Acute Myocardial Infarction. Circ. Cardiovasc. Interv. 2020, 13, e008505. [Google Scholar] [CrossRef]
- Lee, S.H.; Lee, J.M.; Park, J.; Choi, K.H.; Hwang, D.; Doh, J.H.; Nam, C.W.; Shin, E.S.; Hoshino, M.; Murai, T.; et al. Prognostic implications of resistive reserve ratio in patients with coronary artery disease. J. Am. Heart Assoc. 2020, 9, e015846. [Google Scholar] [CrossRef]
- Candreva, A.; Gallinoro, E.; van’t Veer, M.; Sonck, J.; Collet, C.; Di Gioia, G.; Kodeboina, M.; Mizukami, T.; Nagumo, S.; Keulards, D.; et al. Basics of Coronary Thermodilution. JACC Cardiovasc. Interv. 2021, 14, 595–605. [Google Scholar] [CrossRef] [PubMed]
- Xaplanteris, P.; Fournier, S.; Keulards, D.C.J.; Adjedj, J.; Ciccarelli, G.; Milkas, A.; Pellicano, M.; Van’t Veer, M.; Barbato, E.; Pijls, N.H.J.; et al. Catheter-based measurements of absolute coronary blood flow and microvascular resistance feasibility, safety, and reproducibility in humans. Circ. Cardiovasc. Interv. 2018, 11, e006194. [Google Scholar] [CrossRef] [PubMed]
- Fournier, S.; Keulards, D.C.J.; van‘t Veer, M.; Colaiori, I.; Di Gioia, G.; Zimmermann, F.M.; Mizukami, T.; Nagumo, S.; Kodeboina, M.; El Farissi, M.; et al. Normal values of thermodilution-derived absolute coronary blood flow and microvascular resistance in humans. EuroIntervention 2021, 17, e309–e316. [Google Scholar] [CrossRef] [PubMed]
- De Bruyne, B.; Adjedj, J.; Xaplanteris, P.; Ferrara, A.; Mo, Y.; Penicka, M.; Floré, V.; Pellicano, M.; Toth, G.; Barbato, E.; et al. Saline-Induced Coronary Hyperemia. Circ. Cardiovasc. Interv. 2017, 10, e004719. [Google Scholar] [CrossRef] [PubMed]
- Gallinoro, E.; Candreva, A.; Colaiori, I.; Kodeboina, M.; Fournier, S.; Nelis, O.; Di Gioia, G.; Sonck, J.; van‘t Veer, M.; Pijls, N.H.J.; et al. Thermodilution-Derived Volumetric Resting Coronary Blood Flow Measurement in Humans. EuroIntervention 2021, 17, e672–e679. [Google Scholar] [CrossRef]
- Everaars, H.; De Waard, G.A.; Schumacher, S.P.; Zimmermann, F.M.; Bom, M.J.; Van De Ven, P.M.; Raijmakers, P.G.; Lammertsma, A.A.; Götte, M.J.; Van Rossum, A.C.; et al. Continuous thermodilution to assess absolute flow and microvascular resistance: Validation in humans using [15O]H2O positron emission tomography. Eur. Heart J. 2019, 40, 2350–2359. [Google Scholar] [CrossRef]
- De Bruyne, B.; Pijls, N.H.J.; Gallinoro, E.; Candreva, A.; Fournier, S.; Keulards, D.C.J.; Sonck, J.; van‘t Veer, M.; Barbato, E.; Bartunek, J.; et al. Microvascular Resistance Reserve for Assessment of Coronary Microvascular Function. J. Am. Coll. Cardiol. 2021, 78, 1541–1549. [Google Scholar] [CrossRef]
- Konst, R.E.; Elias-Smale, S.E.; Pellegrini, D.; Hartzema-Meijer, M.; van Uden, B.J.C.; Jansen, T.P.J.; Vart, P.; Gehlmann, H.; Maas, A.H.E.M.; van Royen, N.; et al. Absolute Coronary Blood Flow Measured by Continuous Thermodilution in Patients with Ischemia and Nonobstructive Disease. J. Am. Coll. Cardiol. 2021, 77, 728–741. [Google Scholar] [CrossRef]
- Pijls, N.H.J.; de Vos, A.M.J.; Keulards, D.C.J. Measurement of Absolute Coronary Blood Flow and Microvascular Resistance: A New Window to Coronary Microcirculation. J. Am. Coll. Cardiol. 2021, 77, 742–744. [Google Scholar] [CrossRef]
- Kogame, N.; Ono, M.; Kawashima, H.; Tomaniak, M.; Hara, H.; Leipsic, J.; Andreini, D.; Collet, C.; Patel, M.R.; Tu, S.; et al. The Impact of Coronary Physiology on Contemporary Clinical Decision Making. JACC Cardiovasc. Interv. 2020, 13, 1617–1638. [Google Scholar] [CrossRef]
- Ford, T.J.; Stanley, B.; Good, R.; Rocchiccioli, P.; McEntegart, M.; Watkins, S.; Eteiba, H.; Shaukat, A.; Lindsay, M.; Robertson, K.; et al. Stratified Medical Therapy Using Invasive Coronary Function Testing in Angina: The CorMicA Trial. J. Am. Coll. Cardiol. 2018, 72, 2841–2855. [Google Scholar] [CrossRef]
- Ford, T.J.; Stanley, B.; Sidik, N.; Good, R.; Rocchiccioli, P.; McEntegart, M.; Watkins, S.; Eteiba, H.; Shaukat, A.; Lindsay, M.; et al. 1-Year Outcomes of Angina Management Guided by Invasive Coronary Function Testing (CorMicA). JACC Cardiovasc. Interv. 2020, 13, 33–45. [Google Scholar] [CrossRef] [PubMed]
- Ng, M.K.C.; Yong, A.S.C.; Ho, M.; Shah, M.G.; Chawantanpipat, C.; O’Connell, R.; Keech, A.; Kritharides, L.; Fearon, W.F. The Index of Microcirculatory Resistance Predicts Myocardial Infarction Related to Percutaneous Coronary Intervention. Circ. Cardiovasc. Interv. 2012, 5, 515–522. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Layland, J.J.; Whitbourn, R.J.; Burns, A.T.; Somaratne, J.; Leitl, G.; MacIsaac, A.I.; Wilson, A. The index of microvascular resistance identifies patients with periprocedural myocardial infarction in elective percutaneous coronary intervention. Heart 2012, 98, 1492–1497. [Google Scholar] [CrossRef] [PubMed]
- Mangiacapra, F.; Bressi, E.; Gioia, G.D.; Pellicano, M.; Serafino, L.D.; Peace, A.J.; Bartunek, J.; Morisco, C.; Wijns, W.; Bruyne, B.D.; et al. Coronary microcirculation and peri-procedural myocardial injury during elective percutaneous coronary intervention. Int. J. Cardiol. 2020, 306, 42–46. [Google Scholar] [CrossRef] [PubMed]
- Mangiacapra, F.; Barbato, E. Microvascular impairment associated with percutaneous coronary revascularization: The quest for protective microcirculatory strategies. Int. J. Cardiol. 2020, 308, 9. [Google Scholar] [CrossRef] [PubMed]
- Fearon, W.F.; Low, A.F.; Yong, A.S.; McGeoch, R.; Berry, C.; Shah, M.G.; Ho, M.Y.; Kim, H.-S.; Loh, J.P.; Oldroyd, K.G. Prognostic Value of the Index of Microcirculatory Resistance Measured after Primary Percutaneous Coronary Intervention. Circulation 2013, 127, 2436–2441. [Google Scholar] [CrossRef] [Green Version]
- Mangiacapra, F.; Bartunek, J.; Bijnens, N.; Peace, A.J.; Dierickx, K.; Bailleul, E.; Serafino, L.D.; Pyxaras, S.A.; Fraeyman, A.; Meeus, P.; et al. Periprocedural variations of platelet reactivity during elective percutaneous coronary intervention. J. Thromb. Haemost. 2012, 10, 2452–2461. [Google Scholar] [CrossRef]
- Mangiacapra, F.; Cavallari, I.; Ricottini, E.; Pellicano, M.; Barbato, E.; Sciascio, G.D. High platelet reactivity and periprocedural myocardial infarction in patients undergoing percutaneous coronary intervention: A significant association beyond definitions. Int. J. Cardiol. 2015, 190, 124–125. [Google Scholar] [CrossRef]
- Niccoli, G.; Scalone, G.; Lerman, A.; Crea, F. Coronary microvascular obstruction in acute myocardial infarction. Eur. Heart J. 2016, 37, 1024–1033. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Niccoli, G.; Burzotta, F.; Galiuto, L.; Crea, F. Myocardial No-Reflow in Humans. J. Am. Coll. Cardiol. 2009, 54, 281–292. [Google Scholar] [CrossRef] [PubMed]
- Hamirani, Y.S.; Wong, A.; Kramer, C.M.; Salerno, M. Effect of microvascular obstruction and intramyocardial hemorrhage by CMR on LV remodeling and outcomes after myocardial infarction: A systematic review and meta-analysis. JACC Cardiovasc. Imaging 2014, 7, 940–952. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mangiacapra, F.; Peace, A.J.; Di Serafino, L.; Pyxaras, S.A.; Bartunek, J.; Wyffels, E.; Heyndrickx, G.R.; Wijns, W.; De Bruyne, B.; Barbato, E. Intracoronary enalaprilat to reduce microvascular damage during percutaneous coronary intervention (ProMicro) study. J. Am. Coll. Cardiol. 2013, 61, 615–621. [Google Scholar] [CrossRef] [Green Version]
- Sato, T.; Sasaki, N.; O’Rourke, B.; Marbán, E. Nicorandil, a potent cardioprotective agent, acts by opening mitochondrial ATP-dependent potassium channels. J. Am. Coll. Cardiol. 2000, 35, 514–518. [Google Scholar] [CrossRef]
- Ishii, H.; Ichimiya, S.; Kanashiro, M.; Amano, T.; Imai, K.; Murohara, T.; Matsubara, T. Impact of a Single Intravenous Administration of Nicorandil Before Reperfusion in Patients with ST-Segment–Elevation Myocardial Infarction. Circulation 2005, 112, 1284–1288. [Google Scholar] [CrossRef] [Green Version]
- Su, Q.; Li, L.; Liu, Y. Short-term Effect of Verapamil on Coronary No-Reflow Associated With Percutaneous Coronary Intervention in Patients with Acute Coronary Syndrome: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Clin. Cardiol. 2013, 36, E11. [Google Scholar] [CrossRef]
- Werner, G.S.; Lang, K.; Kuehnert, H.; Figulla, H.R. Intracoronary verapamil for reversal of no-reflow during coronary angioplasty for acute myocardial infarction. Catheter. Cardiovasc. Interv. 2002, 57, 444–451. [Google Scholar] [CrossRef]
- Mangiacapra, F.; Patti, G.; Barbato, E.; Peace, A.J.; Ricottini, E.; Vizzi, V.; Gatto, L.; D’ambrosio, A.; De Bruyne, B.; Wijns, W.; et al. A Therapeutic Window for Platelet Reactivity for Patients Undergoing Elective Percutaneous Coronary Intervention: Results of the ARMYDA-PROVE (Antiplatelet therapy for Reduction of MYocardial Damage during Angioplasty–Platelet Reactivity for Outcome Validation Effort) Study. JACC Cardiovasc. Interv. 2012, 5, 281–289. [Google Scholar] [CrossRef] [Green Version]
- Hamilos, M.; Muller, O.; Ntalianis, A.; Trana, C.; Bartunek, J.; Sarno, G.; Mangiacapra, F.; Dierickx, K.; Meeus, P.; Cuisset, T.; et al. Relationship between peripheral arterial reactive hyperemia and residual platelet reactivity after 600 mg clopidogrel. J. Thromb. Thrombolysis 2011, 32, 64–71. [Google Scholar] [CrossRef] [Green Version]
- Mangiacapra, F.; Di Gioia, G.; Pellicano, M.; Di Serafino, L.; Bressi, E.; Peace, A.J.; Bartunek, J.; Wijns, W.; De Bruyne, B.; Barbato, E. Effects of Prasugrel Versus Clopidogrel on Coronary Microvascular Function in Patients Undergoing Elective PCI. J. Am. Coll. Cardiol. 2016, 68, 235–237. [Google Scholar] [CrossRef]
- Mangiacapra, F.; Pellicano, M.; Serafino, L.D.; Bressi, E.; Peace, A.J.; Gioia, G.D.; Morisco, C.; Bartunek, J.; Wijns, W.; Bruyne, B.D.; et al. Platelet reactivity and coronary microvascular impairment after percutaneous revascularization in stable patients receiving clopidogrel or prasugrel. Atherosclerosis 2018, 278, 23–28. [Google Scholar] [CrossRef]
- Mehilli, J.; Baquet, M.; Hochholzer, W.; Mayer, K.; Tesche, C.; Aradi, D.; Xu, Y.; Thienel, M.; Gschwendtner, S.; Zadrozny, M.; et al. Randomized Comparison of Intensified and Standard P2Y12-Receptor-Inhibition before Elective Percutaneous Coronary Intervention. Circ. Cardiovasc. Interv. 2020, 13, e008649. [Google Scholar] [CrossRef]
- Silvain, J.; Lattuca, B.; Beygui, F.; Rangé, G.; Motovska, Z.; Dillinger, J.-G.; Boueri, Z.; Brunel, P.; Lhermusier, T.; Pouillot, C.; et al. Ticagrelor versus clopidogrel in elective percutaneous coronary intervention (ALPHEUS): A randomised, open-label, phase 3b trial. Lancet 2020, 396, 1737–1744. [Google Scholar] [CrossRef]
- Khan, M.A.; Jawad Hashim, M.; Mustafa, H.; Yousif Baniyas, M.; Khalid Buti Mohamad Al Suwaidi, S.; AlKatheeri, R.; Mohamed Khalfan Alblooshi, F.; Eisa Ali Hassan Almatrooshi, M.; Eisa Hazeem Alzaabi, M.; Saif Al Darmaki, R.; et al. Global Epidemiology of Ischemic Heart Disease: Results from the Global Burden of Disease Study. J. Thromb. Thrombolysis 2020, 12, e9349. [Google Scholar] [CrossRef] [PubMed]
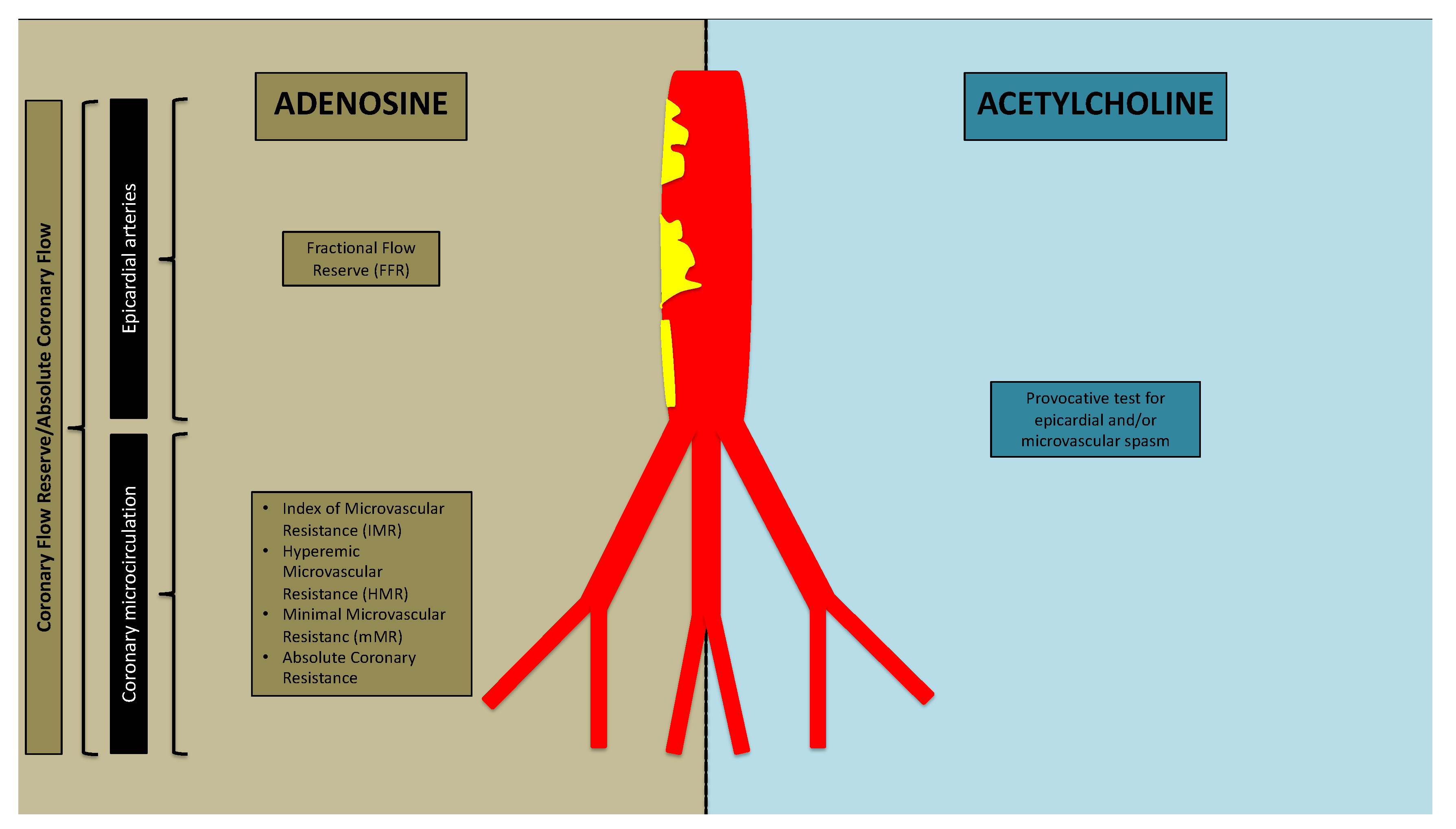
| Pathophysiologic Mechanisms | Hemodynamic Profiles | |
|---|---|---|
| Coronary Microvascular Dysfunction Structural remodeling | Adenosine test CFR < 2.0 IMR ≥ 25 HMR > 1.9/HMR > 2.5 | Acetylcholine test No ischemic symptoms and ECG changes No or <90% coronary diameter reduction |
| Coronary Microvascular Dysfunction Microvascular spasm | CFR < 2.0 IMR < 25 HMR ≤ 1.9/HMR ≤ 2.5 | Ischemic symptoms and ECG changes No or <90% coronary diameter reduction |
| Coronary Microvascular Dysfunction Structural remodeling and microvascular spasm | CFR < 2.0 IMR ≥ 25 HMR > 1.9/HMR > 2.5 | Ischemic symptoms and ECG changes No or <90% coronary diameter reduction |
| Coronary Epicardial Vasospasm | CFR < 2.0 IMR < 25 HMR ≤ 1.9/HMR ≤ 2.5 | Ischemic symptoms and ECG changes coronary diameter reduction ≥ 90% |
| Coronary Microvascular Dysfunction and Epicardial Vasospasm | CFR < 2.0 IMR ≥ 25 HMR > 1.9/HMR > 2.5 | Ischemic symptoms and ECG changes coronary diameter reduction ≥ 90% |
| Microvascular Angina (MVA) | Vasospastic Angina (VSA) |
|---|---|
|
|
| Index | Principle | Equation | Advantages | Disadvantages |
|---|---|---|---|---|
| Coronary Flow Reserve (CFR) | Thermodilution | -Feasible -Safe -Reproducible | -Requires hyperemia -Operator-dependent | |
| Doppler | ||||
| Index of Microcirculatory Resistance (IMR) | Thermodilution | Pd × Tmn[hyper] | -Feasible -Safe -Reproducible | -Requires hyperemia -Operator-dependent -May overestimate true microvascular resistance with critical epicardial CAD |
| Hyperemic Microvascular Resistance (HMR) | Doppler | -Feasible -Safe -Reproducible | -Requires hyperemia -May overestimate true microvascular resistance with critical epicardial CAD | |
| Minimal Microvascular Resistance (mMR) | Doppler | -Feasible -Safe -Reproducible -Good correlation with true microvascular resistance, irrespective of any epicardial CAD | ||
| Resistive Reserve Ratio (RRR) | Thermodilution | -Measure of vasodilation capacity of coronary microcirculation | -Requires hyperemia -Operator-dependent | |
| Absolute Coronary Flow and Resistance | Continuous thermodilution | -Safe -Reproducible -Operator-independent -Pharmacological-hyperemia not required | -Standardized reference values not available | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mangiacapra, F.; Viscusi, M.M.; Verolino, G.; Paolucci, L.; Nusca, A.; Melfi, R.; Ussia, G.P.; Grigioni, F. Invasive Assessment of Coronary Microvascular Function. J. Clin. Med. 2022, 11, 228. https://doi.org/10.3390/jcm11010228
Mangiacapra F, Viscusi MM, Verolino G, Paolucci L, Nusca A, Melfi R, Ussia GP, Grigioni F. Invasive Assessment of Coronary Microvascular Function. Journal of Clinical Medicine. 2022; 11(1):228. https://doi.org/10.3390/jcm11010228
Chicago/Turabian StyleMangiacapra, Fabio, Michele Mattia Viscusi, Giuseppe Verolino, Luca Paolucci, Annunziata Nusca, Rosetta Melfi, Gian Paolo Ussia, and Francesco Grigioni. 2022. "Invasive Assessment of Coronary Microvascular Function" Journal of Clinical Medicine 11, no. 1: 228. https://doi.org/10.3390/jcm11010228
APA StyleMangiacapra, F., Viscusi, M. M., Verolino, G., Paolucci, L., Nusca, A., Melfi, R., Ussia, G. P., & Grigioni, F. (2022). Invasive Assessment of Coronary Microvascular Function. Journal of Clinical Medicine, 11(1), 228. https://doi.org/10.3390/jcm11010228









