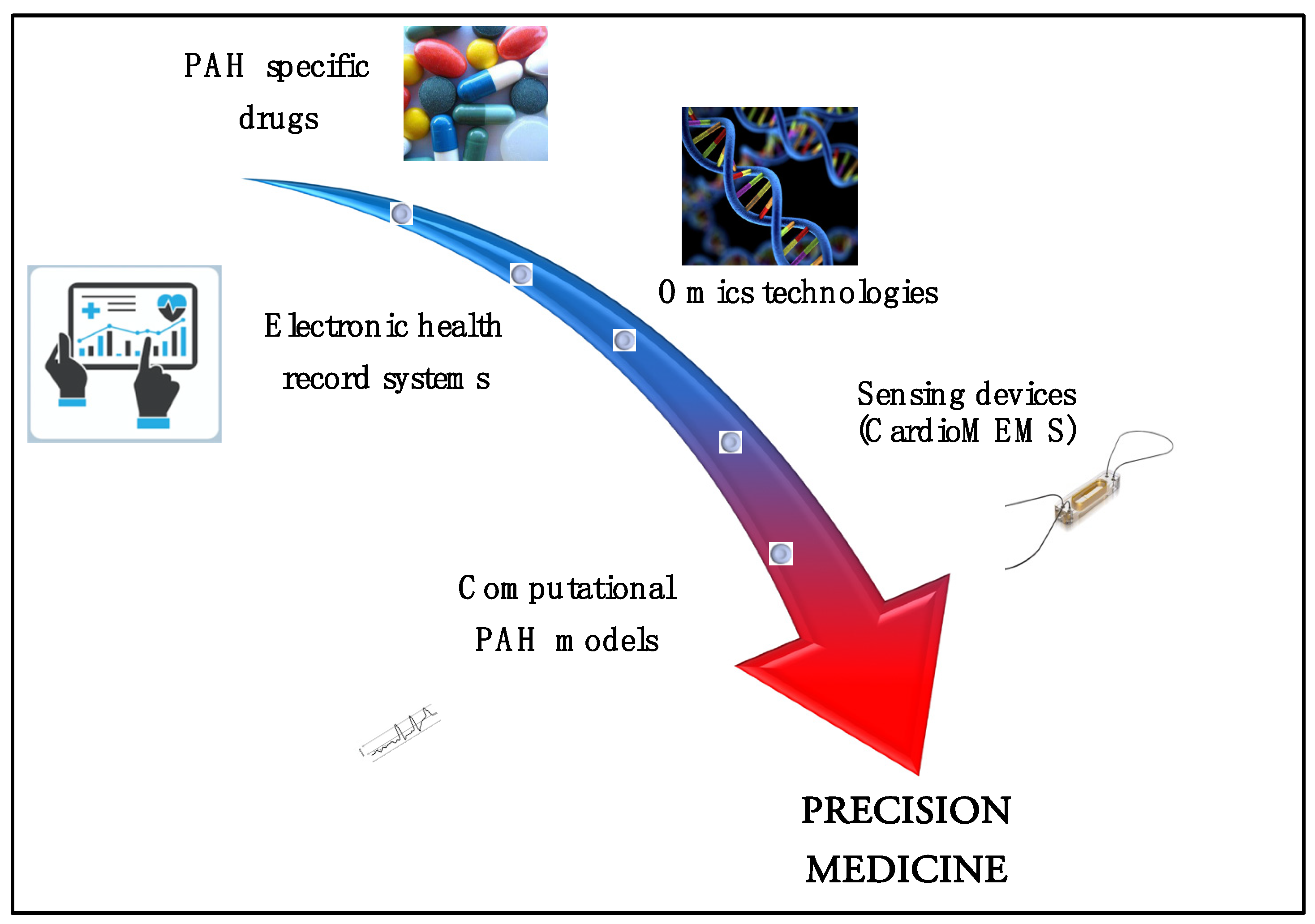
Computational Simulator Models and Invasive Hemodynamic Monitoring as Tools for Precision Medicine in Pulmonary Arterial Hypertension
Abstract
:1. Introduction
2. A Look at Omic Technologies in PAH
3. Ambulatory Implantable Hemodynamic Monitors: A New Source of Big Data
4. Novel Devices for Monitoring Pulmonary Arterial Hypertension Patients
5. The CardioMEMS System
6. Computational Cardiovascular Simulators
- -
- Supplementary modules for ventricular assist devices;
- -
- A supplementary module to reproduce the biventricular pacemaker behavior;
- -
- A supplementary module for the total artificial heart;
- -
- A supplementary module for intra-aortic balloon pumping;
- -
- A supplementary module for the thoracic artificial lung.
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ahn, A.C.; Tewari, M.; Poon, C.S.; Phillips, R.S. The limits of reductionism in medicine: Could systems biology offer an alternative? PLoS Med. 2006, 3, e208. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sitbon, O.; Galiè, N. Treat-to-target strategies in pulmonary arterial hypertension: The importance of using multiple goals. Eur. Respir. Rev. 2010, 19, 272–278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benza, R.L.; Park, M.H.; Keogh, A.; Girgis, R.E. Management of pulmonary arterial hypertension with a focus on combination therapies. J. Heart Lung Transpl. 2007, 26, 437–446. [Google Scholar] [CrossRef] [PubMed]
- Savale, L.; Guignabert, C.; Weatherald, J.; Humbert, M. Precision medicine and personalising therapy in pulmonary hypertension: Seeing the light from the dawn of a new era. Eur. Respir. Rev. 2018, 27, 180004. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Badagliacca, R.; Papa, S.; Matsubara, H.; Lang, I.M.; Poscia, R.; Manzi, G.; Vizza, C.D. The importance of right ventricular evaluation in risk assessment and therapeutic strategies: Raising the bar in pulmonary arterial hypertension. Int. J. Cardiol. 2020, 301, 183–189. [Google Scholar] [CrossRef]
- Morrell, N.W.; Aldred, M.A.; Chung, W.K.; Elliott, C.G.; Nichols, W.C.; Soubrier, F.; Trembath, R.C.; Loyd, J.E. Genetics and genomics of pulmonary arterial hypertension. Eur. Respir. J. 2019, 53, 1801899. [Google Scholar] [CrossRef] [Green Version]
- Oldham, W.M.; Hemnes, A.R.; Aldred, M.A.; Barnard, J.; Brittain, E.L.; Chan, S.Y.; Cheng, F.; Cho, M.H.; Desai, A.A.; Garcia, J.G.N.; et al. NHLBI-CMREF Workshop Report on Pulmonary Vascular Disease Classification: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2021, 77, 2040–2052. [Google Scholar] [CrossRef]
- Hemnes, A.R.; Beck, G.J.; Newman, J.H.; Abidov, A.; Aldred, M.A.; Barnard, J.; Berman Rosenzweig, E.; Borlaug, B.A.; Chung, W.K.; Comhair, S.A.; et al. PVDOMICS: A Multi-Center Study to Improve Understanding of Pulmonary Vascular Disease Through Phenomics. Circ. Res. 2017, 121, 1136–1139. [Google Scholar] [CrossRef]
- Hulsen, T.; Jamuar, S.S.; Moody, A.R.; Karnes, J.H.; Varga, O.; Hedensted, S.; Spreafico, R.; Hafler, D.A.; McKinney, E.F. From Big Data to Precision Medicine. Front. Med. 2019, 6, 34. [Google Scholar] [CrossRef] [Green Version]
- Leff, D.R.; Yang, G. Big data for precision medicine. Engineering 2015, 1, 277–279. [Google Scholar] [CrossRef] [Green Version]
- Badagliacca, R.; D’Alto, M.; Ghio, S.; Argiento, P.; Bellomo, V.; Brunetti, N.D.; Casu, G.; Confalonieri, M.; Corda, M.; Correale, M.; et al. Risk Reduction and Hemodynamics with Initial Combination Therapy in Pulmonary Arterial Hypertension. Am. J. Respir. Crit. Care Med. 2021, 203, 484–492. [Google Scholar] [CrossRef] [PubMed]
- D’Alto, M.; Badagliacca, R.; Lo Giudice, F.; Argiento, P.; Casu, G.; Corda, M.; Correale, M.; Ghio, S.; Greco, A.; Lattanzio, M.; et al. Hemodynamics and risk assessment 2 years after the initiation of upfront ambrisentan–tadalafil in pulmonary arterial hypertension. J. Heart Lung Transpl. 2020, 39, 1389–1397. [Google Scholar] [CrossRef] [PubMed]
- Badagliacca, R.; Raina, A.; Ghio, S.; D’Alto, M.; Confalonieri, M.; Correale, M.; Corda, M.; Paciocco, G.; Lombardi, C.; Mulè, M.; et al. Influence of various therapeutic strategies on right ventricular morphology, function and hemodynamics in pulmonary arterial hypertension. J. Heart Lung Transpl. 2018, 37, 365–375. [Google Scholar] [CrossRef] [PubMed]
- Vonk Noordegraaf, A.; Chin, K.M.; Haddad, F.; Hassoun, P.M.; Hemnes, A.R.; Hopkins, S.R.; Kawut, S.M.; Langleben, D.; Lumens, J.; Naeije, R. Pathophysiology of the right ventricle and of the pulmonary circulation in pulmonary hypertension: An update. Eur. Respir. J. 2019, 53, 1801900. [Google Scholar] [CrossRef]
- Badagliacca, R.; Poscia, R.; Pezzuto, B.; Papa, S.; Pesce, F.; Manzi, G.; Giannetta, E.; Raineri, C.; Schina, M.; Sciomer, S.; et al. Right ventricular concentric hypertrophy and clinical worsening in idiopathic pulmonary arterial hypertension. J. Heart Lung Transpl. 2016, 35, 1321–1329. [Google Scholar] [CrossRef] [PubMed]
- Badagliacca, R.; Poscia, R.; Pezzuto, B.; Nocioni, M.; Mezzapesa, M.; Francone, M.; Giannetta, E.; Papa, S.; Gambardella, C.; Sciomer, S.; et al. Right ventricular remodeling in idiopathic pulmonary arterial hypertension: Adaptive versus maladaptive morphology. J. Heart Lung Transpl. 2015, 34, 395–403. [Google Scholar] [CrossRef]
- Naeije, R.; Vanderpool, R.; Peacock, A.; Badagliacca, R. The Right Heart-Pulmonary Circulation Unit: Physiopathology. Heart Fail. Clin. 2018, 14, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Badagliacca, R.; Rischard, F.; Papa, S.; Kubba, S.; Vanderpool, R.; Yuan, J.X.; Garcia, J.G.; Airhart, S.; Poscia, R.; Pezzuto, B.; et al. Clinical implications of idiopathic pulmonary arterial hypertension phenotypes defined by cluster analysis. J. Heart Lung Transpl. 2020, 39, 310–320. [Google Scholar] [CrossRef] [Green Version]
- Badagliacca, R.; Poscia, R.; Pezzuto, B.; Papa, S.; Reali, M.; Pesce, F.; Manzi, G.; Gianfrilli, D.; Ciciarello, F.; Sciomer, S.; et al. Prognostic relevance of right heart reverse remodeling in idiopathic pulmonary arterial hypertension. J. Heart Lung Transpl. 2017. [Google Scholar] [CrossRef]
- Sciomer, S.; Badagliacca, R.; Fedele, F. Pulmonary hypertension: Echocardiographic assessment. Ital. Heart J. 2005, 6, 840–845. [Google Scholar]
- Miotti, C.; Papa, S.; Manzi, G.; Scoccia, G.; Luongo, F.; Toto, F.; Malerba, C.; Cedrone, N.; Sciomer, S.; Ciciarello, F.; et al. The Growing Role of Echocardiography in Pulmonary Arterial Hypertension Risk Stratification: The Missing Piece. J. Clin. Med. 2021, 10, 619. [Google Scholar] [CrossRef] [PubMed]
- Raina, A.; Benza, R.L. Ambulatory Hemodynamic Monitoring in the Management of Pulmonary Arterial Hypertension. Adv. Pulm. Hypertens 2014, 13, 81–85. [Google Scholar] [CrossRef] [Green Version]
- Abraham, W.T.; Stevenson, L.W.; Bourge, R.C.; Lindenfeld, J.A.; Bauman, J.G.; Adamson, P.B.; CHAMPION Trial Study Group. Sustained efficacy of pulmonary artery pressure to guide adjustment of chronic heart failure therapy: Complete follow-up results from the CHAMPION randomised trial. Lancet 2016, 387, 453–461. [Google Scholar] [CrossRef]
- Givertz, M.M.; Stevenson, L.W.; Costanzo, M.R.; Bourge, R.C.; Bauman, J.G.; Ginn, G.; Abraham, W.T.; CHAMPION Trial Investigators. Pulmonary Artery Pressure-Guided Management of Patients With Heart Failure and Reduced Ejection Fraction. J. Am. Coll. Cardiol. 2017, 70, 1875–1886. [Google Scholar] [CrossRef] [PubMed]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; González-Juanatey, J.R.; Harjola, V.P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2016, 37, 2129–2200. [Google Scholar] [CrossRef] [PubMed]
- Benza, R.L.; Doyle, M.; Lasorda, D.; Parikh, K.S.; Correa-Jaque, P.; Badie, N.; Ginn, G.; Airhart, S.; Franco, V.; Kanwar, M.K.; et al. Monitoring Pulmonary Arterial Hypertension Using an Implantable Hemodynamic Sensor. Chest 2019, 156, 1176–1186. [Google Scholar] [CrossRef]
- De Lazzari, C.; Genuini, I.; Pisanelli, D.M.; D’Ambrosi, A.; Fedele, F. Interactive simulator for e-Learning environments: A teaching software for health care professionals. Biomed. Eng. Online 2014, 13, 172. [Google Scholar] [CrossRef] [Green Version]
- Larrabide, I.; Blanco, P.J.; Urquiza, S.A.; Dari, E.A.; Vénere, M.J.; e Silva, N.D.; Feijóo, R.A. HeMoLab—Hemodynamics Modelling Laboratory: An application for modelling the human cardiovascular system. Comput. Biol. Med. 2012, 42, 993–1004. [Google Scholar] [CrossRef]
- Fresiello, L.; Ferrari, G.; Di Molfetta, A.; Zieliński, K.; Tzallas, A.; Jacobs, S.; Darowski, M.; Kozarski, M.; Meyns, B.; Katertsidis, N.S.; et al. A cardiovascular simulator tailored for training and clinical uses. J. Biomed. Inform. 2015, 57, 100–112. [Google Scholar] [CrossRef] [Green Version]
- Arts, T.; Delhaas, T.; Bovendeerd, P.; Verbeek, X.; Prinzen, F.W. Adaptation to mechanical load determines shape and properties of heart and circulation: The circadapt model. Am. J. Physiol. Heart Circ. Physiol. 2005, 288, H1943–H1954. [Google Scholar] [CrossRef]
- De Lazzari, C.; Quatember, B.; Recheis, W.; Mayr, M.; Demertzis, S.; Allasia, G.; De Rossi, A.; Cavoretto, R.; Venturino, E.; Genuini, I. Lung assist devices influence cardio-energetic parameters: Numerical simulation study. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2015, 2015, 4515–4519. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Capoccia, M.; Marconi, S.; Singh, S.A.; Pisanelli, D.M.; De Lazzari, C. Simulation as a preoperative planning approach in advanced heart failure patients. A retrospective clinical analysis. Biomed. Eng. Online 2018, 17, 52. [Google Scholar] [CrossRef] [PubMed]
- Gaudenzi, F.; Avolio, A.P. Lumped parameter model of cardiovascular-respiratory interaction. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2013, 2013, 473–476. [Google Scholar] [CrossRef] [PubMed]
- Marconi, S.; De Lazzari, C. In silico study of airway/lung mechanics in normal human breathing. Math. Comput. Simul. 2020, 177, 603–624. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manzi, G.; Miotti, C.; Mariani, M.V.; Papa, S.; Luongo, F.; Scoccia, G.; De Lazzari, B.; De Lazzari, C.; Benza, R.L.; Fedele, F.; et al. Computational Simulator Models and Invasive Hemodynamic Monitoring as Tools for Precision Medicine in Pulmonary Arterial Hypertension. J. Clin. Med. 2022, 11, 82. https://doi.org/10.3390/jcm11010082
Manzi G, Miotti C, Mariani MV, Papa S, Luongo F, Scoccia G, De Lazzari B, De Lazzari C, Benza RL, Fedele F, et al. Computational Simulator Models and Invasive Hemodynamic Monitoring as Tools for Precision Medicine in Pulmonary Arterial Hypertension. Journal of Clinical Medicine. 2022; 11(1):82. https://doi.org/10.3390/jcm11010082
Chicago/Turabian StyleManzi, Giovanna, Cristiano Miotti, Marco Valerio Mariani, Silvia Papa, Federico Luongo, Gianmarco Scoccia, Beatrice De Lazzari, Claudio De Lazzari, Raymond L. Benza, Francesco Fedele, and et al. 2022. "Computational Simulator Models and Invasive Hemodynamic Monitoring as Tools for Precision Medicine in Pulmonary Arterial Hypertension" Journal of Clinical Medicine 11, no. 1: 82. https://doi.org/10.3390/jcm11010082
APA StyleManzi, G., Miotti, C., Mariani, M. V., Papa, S., Luongo, F., Scoccia, G., De Lazzari, B., De Lazzari, C., Benza, R. L., Fedele, F., Vizza, C. D., & Badagliacca, R. (2022). Computational Simulator Models and Invasive Hemodynamic Monitoring as Tools for Precision Medicine in Pulmonary Arterial Hypertension. Journal of Clinical Medicine, 11(1), 82. https://doi.org/10.3390/jcm11010082





