Cognitive–Behavioral Treatment of Obsessive–Compulsive Disorder: The Results of a Naturalistic Outcomes Study
Abstract
1. Introduction
- (a)
- a significant percentage of participants do not respond to treatment;
- (b)
- many participants are unwilling or do not tolerate ERP.
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Measure
2.4. Treatment
3. Results
3.1. Repeated-Measures ANOVA
3.2. Wilcoxon Signed-Rank Test
3.3. Reliable Change Index and Clinical Significance
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Phase | Contents of the Treatment | Mean Number of Psychotherapy Sessions |
|---|---|---|
| 1 | Reconstruction and sharing of the functioning scheme of patient’s disorder and specific symptomatology | 4 |
| 2 | Modulate beliefs that support the negative or threat evaluation of the critical event and that sustain the motivation: cognitive restructuring techniques | 5 |
| 3 | Accepting the risk (threat) to reduce investments in prevention: cognitive techniques to facilitate willingness to accept feared stimuli exposure and the progressive renunciation of compulsions | 8 |
| 4 | Exposure and response prevention (ERP) | 10 |
| 5 | Intervention to reduce OCD historical vulnerability | 5 |
- After analyzing the advantages and disadvantages of the obsessive activity, the therapist proposes that patients alternately sit in each of the two chairs.
- When sitting in the first chair, patients list all of the costs connected to the threat and, therefore, the benefits of prudence.
- When sitting in the second chair, patients must instead list all the costs of prevention and the benefits of an eventual reduction in the search for absolute certainty.
- At this point, the objective is to render explicit the internal dialectic by asking that the two positions be discussed constructively for the purpose of highlighting the costs of the two operations, namely ‘preventing’ and ‘accepting’ a threat of being responsible for future harm (or compromising the goal of being morally perfect). In this way, patients can, on the one hand, simultaneously and more accurately represent the benefits of acceptance and the costs of investment and, on the other hand, they prepare themselves to consider both sets of costs and benefits together.
References
- Kessler, R.C.; Chiu, W.T.; Demler, O.; Walters, E.E. Prevalence, Severity, and Comorbidity of 12-Month DSM-IV Disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 2005, 62, 617–627. [Google Scholar] [CrossRef] [PubMed]
- Ruscio, A.M.; Stein, D.; Chiu, W.T.; Kessler, R.C. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol. Psychiatry 2010, 15, 53–63. [Google Scholar] [CrossRef] [PubMed]
- Foa, E.B.; Franklin, M.E. Obsessive compulsive disorder. In Clinical Handbook of Psychological Disorders; Barlow, D.H., Ed.; Guilford Press: New York, NY, USA, 2001. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®); American Psychiatric Pub: Washington, DC, USA, 2013. [Google Scholar]
- Hollander, E.; Stein, D.J.; Fineberg, N.A.; Marteau, F.; Legault, M. Quality of Life Outcomes in Patients With Obsessive-Compulsive Disorder. J. Clin. Psychiatry 2010, 71, 784–792. [Google Scholar] [CrossRef] [PubMed]
- Hollander, E.; Doernberg, E.; Shavitt, R.; Waterman, R.J.; Soreni, N.; Veltman, D.J.; Sahakian, B.; Fineberg, N.A. The cost and impact of compulsivity: A research perspective. Eur. Neuropsychopharmacol. 2016, 26, 800–809. [Google Scholar] [CrossRef] [PubMed]
- Leonard, H.L.; Swedo, S.E.; Lenane, M.C.; Rettew, D.C.; Hamburger, S.D.; Bartko, J.J.; Rapoport, J.L. A 2- to 7-Year Follow-up Study of 54 Obsessive-Compulsive Children and Adolescents. Arch. Gen. Psychiatry 1993, 50, 429–439. [Google Scholar] [CrossRef] [PubMed]
- Skoog, G.; Skoog, I. A 40-Year Follow-up of Patients With Obsessive-compulsive Disorder. Arch. Gen. Psychiatry 1999, 56, 121–127. [Google Scholar] [CrossRef]
- Stewart, S.E.; Geller, D.A.; Jenike, M.; Pauls, D.; Shaw, D.; Mullin, B.; Faraone, S.V. Long-term outcome of pediatric obsessive-compulsive disorder: A meta-analysis and qualitative review of the literature. Acta Psychiatr. Scand. 2004, 110, 4–13. [Google Scholar] [CrossRef]
- Fineberg, N.A.; Dell’Osso, B.; Albert, U.; Maina, G.; Geller, D.; Carmi, L.; Sireau, N.; Walitza, S.; Grassi, G.; Pallanti, S.; et al. Early intervention for obsessive compulsive disorder: An expert consensus statement. Eur. Neuropsychopharmacol. 2019, 29, 549–565. [Google Scholar] [CrossRef]
- Franklin, M.E.; Foa, E.B. Treatment of Obsessive-Compulsive Disorder. Annu. Rev. Clin. Psychol. 2011, 7, 229–243. [Google Scholar] [CrossRef]
- National Institute for Health and Clinical Excellence. Obsessive Compulsive Disorder: Core Interventions in the Treatment of Obsessive-Compulsive Disorder and Body Dysmorphic Disorder; Clinical Guideline No. 31; National Institute for Health and Clinical Excellence: London, UK, 2005. [Google Scholar]
- Kozak, M.J.; Foa, E.B.; Clark, D.A. Mastery of Obsessive-Compulsive Disorder: A Cognitive-Behavioral Approach Therapist Guide. J. Cogn. Psychother. 2001, 15, 273–276. [Google Scholar] [CrossRef]
- Foa, E.B. Cognitive behavioral therapy of obsessive-compulsive disorder. Dialogues Clin. Neurosci. 2010, 12, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Olatunji, B.O.; Davis, M.L.; Powers, M.B.; Smits, J.A. Cognitive-behavioral therapy for obsessive-compulsive disorder: A meta-analysis of treatment outcome and moderators. J. Psychiatr. Res. 2013, 47, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Öst, L.-G.; Havnen, A.; Hansen, B.; Kvale, G. Cognitive behavioral treatments of obsessive–compulsive disorder. A systematic review and meta-analysis of studies published 1993–2014. Clin. Psychol. Rev. 2015, 40, 156–169. [Google Scholar] [CrossRef] [PubMed]
- Rosa-Alcazar, A.I.; Sánchez-Meca, J.; Gómez-Conesa, A.; Marín-Martínez, F. Psychological treatment of obsessive–compulsive disorder: A meta-analysis. Clin. Psychol. Rev. 2008, 28, 1310–1325. [Google Scholar] [CrossRef]
- Hunsley, J.; Elliott, K.; Therrien, Z. The efficacy and effectiveness of psychological treatments for mood, anxiety, and related disorders. Can. Psychol. 2014, 55, 161–176. [Google Scholar] [CrossRef]
- Franklin, M.E.; Foa, E.B. Cognitive-behavioral treatments for obsessive compulsive disorder. In A Guide to Treatments That Work; Nathan, P.E., Gorman, J.M., Eds.; Oxford University Press: Oxford, UK, 1998; pp. 339–357. [Google Scholar]
- Emmelkamp, P.M.; Foa, E.B. (Eds.) Failures are a change. In Failures in Behavior Therapy; Wiley: New York, NY, USA, 1983; pp. 1–9. [Google Scholar]
- Kozak, M.; Liebowitz, M.; Foa, E.B. Cognitive Behavior therapy and pharmacotherapy for obsessive–compulsive disorder: The NIMH-Sponsored collaborative study. In Obsessive–Compulsive Disorder; Goodman, W.K., Ed.; Erlbaum: Mahwah, NJ, USA, 2000; pp. 501–530. [Google Scholar]
- Abramowitz, J.S. The Psychological Treatment of Obsessive—Compulsive Disorder. Can. J. Psychiatry 2006, 51, 407–416. [Google Scholar] [CrossRef]
- Skapinakis, P.; Caldwell, D.; Hollingworth, W.; Bryden, P.; Fineberg, N.; Salkovskis, P.; Welton, N.; Baxter, H.; Kessler, D.; Churchill, R.; et al. A systematic review of the clinical effectiveness and cost-effectiveness of pharmacological and psychological interventions for the management of obsessive–compulsive disorder in children/adolescents and adults. Health Technol. Assess. 2016, 20, 1–392. [Google Scholar] [CrossRef]
- Reid, J.E.; Laws, K.R.; Drummond, L.; Vismara, M.; Grancini, B.; Mpavaenda, D.; Fineberg, N.A. Cognitive behavioural therapy with exposure and response prevention in the treatment of obsessive-compulsive disorder: A systematic review and meta-analysis of randomised controlled trials. Compr. Psychiatry 2021, 106, 152223. [Google Scholar] [CrossRef]
- Cottraux, J.; Note, I.; Yao, S.N.; Lafont, S.; Note, B.; Mollard, E.; Bouvard, M.; Sauteraud, A.; Bourgeois, M.; Dartigues, J.-F. A Randomized Controlled Trial of Cognitive Therapy versus Intensive Behavior Therapy in Obsessive Compulsive Disorder. Psychother. Psychosom. 2001, 70, 288–297. [Google Scholar] [CrossRef]
- Kushner, M.G.; Kim, S.W.; Donahue, C.; Thuras, P.; Adson, D.; Kotlyar, M.; McCabe, J.; Peterson, J.; Foa, E.B. D-Cycloserine Augmented Exposure Therapy for Obsessive-Compulsive Disorder. Biol. Psychiatry 2007, 62, 835–838. [Google Scholar] [CrossRef]
- Leeuwerik, T.; Cavanagh, K.; Strauss, C. Patient adherence to cognitive behavioural therapy for obsessive-compulsive disorder: A systematic review and meta-analysis. J. Anxiety Disord. 2019, 68, 102135. [Google Scholar] [CrossRef] [PubMed]
- Ong, C.W.; Clyde, J.W.; Bluett, E.J.; Levin, M.E.; Twohig, M.P. Dropout rates in exposure with response prevention for obsessive-compulsive disorder: What do the data really say? J. Anxiety Disord. 2016, 40, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Swift, J.K.; Greenberg, R.P. A treatment by disorder meta-analysis of dropout from psychotherapy. J. Psychother. Integr. 2014, 24, 193–207. [Google Scholar] [CrossRef]
- Mancini, F.; Barcaccia, B.; Capo, R.; Gangemi, A.; Gragnani, A.; Perdighe, C.; Rainone, A.; Romano, G. Trattamento cognitivo-comportamentale nel Disturbo Ossessivo-Compulsivo:risultati di uno studio di esito naturalistico in aperto con follow-up a 6,12 e 24 mesi. Riv Psichiatr. 2006, 41, 99–106. [Google Scholar] [CrossRef]
- Mancini, F.; Gangemi, A. Cognitive Processes in Obsessive-Compulsive Disorder. In The Obsessive Mind: Understanding and Treating Obsessive-Compulsive Disorder; Mancini, F., Ed.; Routledge: New York, NY, USA, 2019; pp. 73–92. [Google Scholar]
- Zaccari, V.; Gragnani, A.; Pellegrini, V.; Caiazzo, T.; D’Arienzo, M.C.; Magno, A.; Femia, G.; Mancini, F. An Observational Study of OCD Patients Treated With Cognitive Behavioral Therapy during the COVID-19 Pandemic. Front. Psychiatry 2021, 12, 1822. [Google Scholar] [CrossRef]
- Jacobson, N.S.; Christensen, A. Studying the effectiveness of psychotherapy: How well can clinical trials do the job? Am. Psychol. 1996, 51, 1031–1039. [Google Scholar] [CrossRef]
- Franklin, M.E.; Abramowitz, J.S.; Kozak, M.J.; Levitt, J.T.; Foa, E.B. Effectiveness of exposure and ritual prevention for obsessive-compulsive disorder: Randomized compared with nonrandomized samples. J. Consult. Clin. Psychol. 2000, 68, 594–602. [Google Scholar] [CrossRef]
- Morris, S.B.; DeShon, R.P. Combining effect size estimates in meta-analysis with repeated measures and independent-groups designs. Psychol. Methods 2002, 7, 105–125. [Google Scholar] [CrossRef]
- Stewart, R.E.; Chambless, D.L. Cognitive–behavioral therapy for adult anxiety disorders in clinical practice: A meta-analysis of effectiveness studies. J. Consult. Clin. Psychol. 2009, 77, 595–606. [Google Scholar] [CrossRef]
- Hans, E.; Hiller, W. A meta-analysis of nonrandomized effectiveness studies on outpatient cognitive behavioral therapy for adult anxiety disorders. Clin. Psychol. Rev. 2013, 33, 954–964. [Google Scholar] [CrossRef]
- First, M.; Williams, J.; Karg, R.; Spitzer, R. Structured Clinical Interview for DSM-5 (SCID-5 for DSM-5); American Psychiatric Association: Arlington, VA, USA, 2017. [Google Scholar]
- Goodman, W.K.; Price, L.H.; Rasmussen, S.A.; Mazure, C.; Fleischmann, R.L.; Hill, C.L.; Heninger, G.R.; Charney, D.S. The Yale-Brown Obsessive Compulsive Scale. I. Development, Use, and Reliability. Arch. Gen. Psychiatry 1989, 46, 1006–1011. [Google Scholar] [CrossRef] [PubMed]
- Hénin, M. Yale–Brown Obsessive–Compulsive Scale, In Disturbo Ossessivo-Compulsivo. Questionari e Interviste per la Valutazione Clinica; Sica, C., Ed.; Erickson: Trento, OH, USA, 2012. [Google Scholar]
- Melli, G.; Avallone, E.; Moulding, R.; Pinto, A.; Micheli, E.; Carraresi, C. Validation of the Italian version of the Yale–Brown Obsessive Compulsive Scale–Second Edition (Y-BOCS-II) in a clinical sample. Compr. Psychiatry 2015, 60, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Ellis, A. Reason and Emotion in Psychotherapy; Lyle Stuart: New York, NY, USA, 1962. [Google Scholar]
- Wells, A. Cognitive Therapy of Anxiety Disorders: A Practice Manual and Conceptual Guide; John Wiley and Sons: Honoken, NJ, USA, 1997; Volume 12. [Google Scholar] [CrossRef]
- Van Oppen, P.; Arntz, A. Cognitive Therapy for Obsessive-compulsive disorder. Behav. Res. Ther. 1994, 32, 79–87. [Google Scholar] [CrossRef]
- Vos, S.P.F.; Huibers, M.J.H.; Arntz, A. Experimental investigation of targeting responsibility versus danger in cognitive therapy of obsessive-compulsive disorder. Depress. Anxiety 2012, 29, 629–637. [Google Scholar] [CrossRef]
- Leahy, R.L. Cognitive Therapy Techniques: A Practitioner’s Guide; Guilford Press: New York, NY, USA, 2003. [Google Scholar]
- Abramowitz, J.S.; Whiteside, S.; Kalsy, S.A.; Tolin, D.F. Thought control strategies in obsessive-compulsive dis-order: A replication and extension’. Behav. Res. Ther. 2003, 41, 529–540. [Google Scholar] [CrossRef]
- Rachman, S.; de Silva, P. Abnormal and normal obsessions. Behav. Res. Ther. 1978, 16, 233–248. [Google Scholar] [CrossRef]
- Perdighe, C.; Gragnani, A.; Rainone, A. Accepting risk: Cognitive Techniques. In The Obsessive Mind: Understanding and Treating Obsessive-Compulsive Disorder; Mancini, F., Ed.; Routledge: New York, NY, USA, 2019; pp. 221–249. [Google Scholar]
- Perdighe, C.; Mancini, F. Dall’investimento alla rinuncia: Favorire l’accettazione in psicoterapia. Cogn. Clin. 2012, 9, 116–134. [Google Scholar]
- Gangemi, A.; Tenore, K.; Mancini, F. Two Reasoning Strategies in Patients With Psychological Illnesses. Front. Psychol. 2019, 10, 2335. [Google Scholar] [CrossRef]
- Salkovskis, P.; Westbrook, D.; Davis, J.; Jeavons, A.; Gledhill, A. Effects of neutralizing on intrusive thoughts: An experiment investigating the etiology of obsessive-compulsive disorder. Behav. Res. Ther. 1997, 35, 211–219. [Google Scholar] [CrossRef]
- Salkovskis, P.M.; Forrester, E.; Richards, C. Cognitive–behavioural approach to understanding obsessional thinking. Br. J. Psychiatry 1998, 173, 53–63. [Google Scholar] [CrossRef]
- Gragnani, A.; Buonanno, C.; Saettoni, M. Techniques of cognitive Restructuring. In The Obsessive Mind: Understanding and Treating Obsessive-Compulsive Disorder; Mancini, F., Ed.; Routledge: New York, NY, USA, 2019. [Google Scholar]
- Mancini, F.; Gragnani, A. L’esposizione con prevenzione della risposta come pratica dell’accettazione. Cognitivismo Clinico 2005, 2, 38–58. [Google Scholar]
- Mancini, F.; Gragnani, A. Gli Homework Nel Disturbo Ossessivo-Compulsivo. In Homework: Un’antologia di Prescrizioni Terapeutiche; Baldini, F., Ed.; McGraw-Hill: Milan, Italy, 2004; pp. 105–136. [Google Scholar]
- Pugh, M. Cognitive Behavioural Chairwork: Distinctive Features; Routledge: Oxon, UK, 2019. [Google Scholar]
- Gragnani, A.; Toro, B.; De Luca, L.; Cavagnoli, M.; Mancini, F. L’efficacia delle tecniche cognitive nella riattribuzione della stima della probabilità. Psicoter. Cogn. Comport. 2003, 9, 91–108. [Google Scholar]
- Foa, E.B.; Yadin, E.; Lichner, T.K. Exposure and Response (Ritual) Prevention for Obsessive Compulsive Disorder; Oxford University Press: Oxford, UK, 2012. [Google Scholar] [CrossRef]
- Luppino, O.I.; Pontillo, M. Exposure with Response Prevention as a Practice of Acceptance. In The Obsessive Mind: Understanding and Treating Obsessive-Compulsive Disorder; Mancini, F., Ed.; Routledge: New York, NY, USA, 2019; pp. 250–274. [Google Scholar]
- Mancini, F.; Gangemi, A. Fear of guilt from behaving irresponsibly in obsessive? compulsive disorder. J. Behav. Ther. Exp. Psychiatry 2004, 35, 109–120. [Google Scholar] [CrossRef]
- Chiang, B.; Purdon, C.; Radomsky, A.S. Development and initial validation of the Fear of Guilt Scale for obsessive-compulsive disorder (OCD). J. Obs. Compuls. Relat. Disord. 2016, 11, 63–73. [Google Scholar] [CrossRef]
- Salkovskis, P. Obsessional-compulsive problems: A cognitive-behavioural analysis. Behav. Res. Ther. 1985, 23, 571–583. [Google Scholar] [CrossRef]
- Rachman, S. Obsessions, responsibility and guilt. Behav. Res. Ther. 1993, 31, 149–154. [Google Scholar] [CrossRef]
- Rachman, S. A cognitive theory of compulsive checking. Behav. Res. Ther. 2002, 40, 625–639. [Google Scholar] [CrossRef]
- Rachman, S. Fear of Contamination: Assessment and Treatment; Oxford University Press Inc.: New York, NY, USA, 2006. [Google Scholar]
- Salkovskis, P.M.; Forrester, E. Responsibility. In Cognitive Approaches to Obsessions and Compulsions; Frost, R.O., Steketee, G., Eds.; Elsevier Science: Oxford, UK, 2002. [Google Scholar]
- Mancini, F.; Gangemi, A. Fear of deontological guilt and fear of contamination in obsessive compulsive patient. Psicoter. Cogn. Comport. 2011, 17, 395–404. [Google Scholar]
- Tenore, K.; Gragnani, A. Intervention on Historical Vulnerability. In The Obsessive Mind: Understanding and Treating Obsessive-Compulsive Disorder; Mancini, F., Ed.; Routledge: New York, NY, USA, 2019; pp. 310–322. [Google Scholar]
- Basile, B.; De Sanctis, B.; Fadda, S.; Luppino, O.I.; Perdighe, C.; Saliani, A.M.; Mancini, F. Early life experiences in ocd and other disorders: A retrospective observational study using imagery with rescripting. Clin. Neuropsychiatry 2018, 15, 299–305. [Google Scholar]
- Luppino, O.I.; Tenore, K.; Mancini, F.; Basile, B. A Theoretical Integration of Schema Therapy and Cognitive Therapy in OCD Treatment: Goals and Beliefs of the Obsessive Mind (Part I). Psychology 2018, 9, 2261–2277. [Google Scholar] [CrossRef][Green Version]
- Tenore, K.; Basile, B.; Mancini, F.; Luppino, O.I.L. A theoretical integration of Schema Therapy and Cognitive Therapy in OCD treatment: Conceptualization and rationale (Part II). Psychology 2018, 9, 2278–2295. [Google Scholar] [CrossRef][Green Version]
- Veale, D.; Page, N.; Woodward, E.; Salkovskis, P. Imagery Rescripting for Obsessive Compulsive Disorder: A single case experimental design in 12 cases. J. Behav. Ther. Exp. Psychiatry 2015, 49, 230–236. [Google Scholar] [CrossRef] [PubMed]
- Tenore, K.; Basile, B.; Cosentino, T.; De Sanctis, B.; Fadda, S.; Femia, G.; Gragnani, A.; Luppino, O.I.; Pellegrini, V.; Perdighe, C.; et al. Imagery Rescripting on Guilt-Inducing Memories in OCD: A Single Case Series Study. Front. Psychiatry 2020, 11, 543806. [Google Scholar] [CrossRef] [PubMed]
- Gragnani, A.; Tenore, K. Preventing relapses and concluding therapy. In The Obsessive Mind: Understanding and Treating Obsessive-Compulsive Disorder; Mancini, F., Ed.; Routledge: New York, NY, USA, 2019; pp. 180–200. [Google Scholar]
- Lakens, D. Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Front. Psychol. 2013, 4, 863. [Google Scholar] [CrossRef]
- Fritz, C.O.; Morris, P.E.; Richler, J.J. Effect size estimates: Current use, calculations, and interpretation. J. Exp. Psychol. Gen. 2012, 141, 2–18. [Google Scholar] [CrossRef]
- Jacobson, N.S.; Truax, P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. J. Consult. Clin. Psychol. 1991, 59, 12–19. [Google Scholar] [CrossRef]
- Lemon, J.; Lemon, M.J. Package ‘clinsig’. 2016. Available online: https://CRAN.R-project.org/package=clinsig (accessed on 29 December 2021).
- Rachman, S. A cognitive theory of obsessions. Behav. Res. Ther. 1997, 31, 793–802. [Google Scholar] [CrossRef]
- Mancini, F.; D’Olimpio, F.; D’Ercole, S. Responsibility attitude, obsession and compulsion: Further support in a non-clinical sample. Clin. Psychol. Psychother. 2001, 8, 274–281. [Google Scholar] [CrossRef]
- Mancini, F. Il Disturbo Ossessivo-Compulsivo. In Il Manuale di Terapia Cognitiva; Bollati Boringhieri: Torino, Italy, 2005. [Google Scholar]
- Mancini, F.; Gangemi, A.; Perdighe, C.; Marini, C. Not just right experience: Is it influenced by feelings of guilt? J. Behav. Ther. Exp. Psychiatry 2008, 39, 162–176. [Google Scholar] [CrossRef]
- Summerfeldt, L.J.; Kloosterman, P.H.; Antony, M.M.; Swinson, R.P. Examining an obsessive-compulsive core dimensions model: Structural validity of harm avoidance and incompleteness. J. Obs. Compuls. Relat. Disord. 2014, 3, 83–94. [Google Scholar] [CrossRef]
- Zaccari, V.; Rogier, G.; Pulsinelli, D.; Mancini, F.; D’Olimpio, F. Explaining Interaction of Guilt and Obses-sive-Compulsive Symptoms In Not Just Right Experiences. Clin. Neuropsychiatry 2022, 19, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Hayes, S.C.; Strosahl, K.D.; Wilson, K.G. Acceptance and commitment therapy. In The Process and Practice of Mindful Change, 2nd ed.; The Guilford Press: New York, NY, USA, 2012. [Google Scholar]
- Kabat-Zinn, J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness; Dell Publishing: New York, NY, USA, 1990. [Google Scholar]
- Barcaccia, B. Accepting Events: Topicality of Seneca’s Stoic Proposal. Ph.D. Thesis, Roma Tre University, Rome, Italy, 2007. (In Italian). [Google Scholar]
- Barcaccia, B. Accepting Limitations of Life: Leading Our Patients through a Painful but Healing Path; Invited Lecture Conducted from Ludwig-Maximilians-University, Munich Department Psychologie: Munich, Germany, 2008. [Google Scholar]
- Mancini, F.; Carlo, E. La mente non accettante. Cogn. Clin. 2017, 14, 222–237. [Google Scholar]
- Carlo, E.; Brasini, M.; Giacomantonio, M.; Mancini, F. Accettazione, Amor fati e Ordine naturale: Una prospettiva cognitivista. Cogn. Clin. 2021, 18, 67–86. [Google Scholar] [CrossRef]
- Romano, G.; Trincas, R. Constructing a Diagrammatic Model for Understanding the Disorder. In The Obsessive Mind: Understanding and Treating Obsessive-Compulsive Disorder; Mancini, F., Ed.; Routledge: New York, NY, USA, 2019; p. 173. [Google Scholar]

| Variables | Frequency | Percentage |
|---|---|---|
| Gender | ||
| Male | 25 | 58.1 |
| Female | 18 | 41.9 |
| Nationality | ||
| Italian | 42 | 97.7 |
| Other | 1 | 2.3 |
| Medications | ||
| Yes | 17 | 39.5 |
| No | 26 | 60.5 |
| Mean | SD | |
| Age | 32.70 | 8.91 |
| Disorder Duration in Months | 93.42 | 100.14 |
| Comorbidity 1 | Frequency | Percentage |
| APD | 2 | 4.7 |
| BD-II | 1 | 2.3 |
| BIP 2 | 1 | 2.3 |
| BN | 1 | 2.3 |
| BPD | 3 | 7.0 |
| BPD (Tr) | 2 | 4.7 |
| DEP | 7 | 16.3 |
| DPD (Tr) | 3 | 7.0 |
| IAD | 1 | 2.3 |
| NPD | 1 | 2.3 |
| NPD (Tr) | 4 | 9.3 |
| OCPD (Tr) | 2 | 4.7 |
| PAN | 4 | 9.3 |
| PPD | 1 | 2.3 |
| PPD (Tr) | 1 | 2.3 |
| SAD | 1 | 2.3 |
| NONE | 8 | 18.6 |
| Comorbidity 2 | Frequency | Percentage |
| BPD | 1 | 2.3 |
| DEP | 2 | 4.7 |
| DPD | 1 | 2.3 |
| NPD (Tr) | 1 | 2.3 |
| NPD and DEP | 1 | 2.3 |
| OCPD | 2 | 4.7 |
| PPD | 1 | 2.3 |
| PPD (Tr) | 3 | 7.0 |
| SAD | 3 | 7.0 |
| UPD | 3 | 7.0 |
| NONE | 25 | 58.1 |
| OCD Subtype 1 | Frequency | Percentage |
| AS | 2 | 4.7% |
| C and W | 9 | 20.9% |
| CH | 14 | 32.6% |
| U | 17 | 39.5% |
| Washer | 1 | 2.3% |
| OCD Subtype 2 | Frequency | Percentage |
| C and W | 5 | 11.6% |
| CH | 10 | 23.3% |
| U | 6 | 14.0% |
| None | 22 | 51.2% |
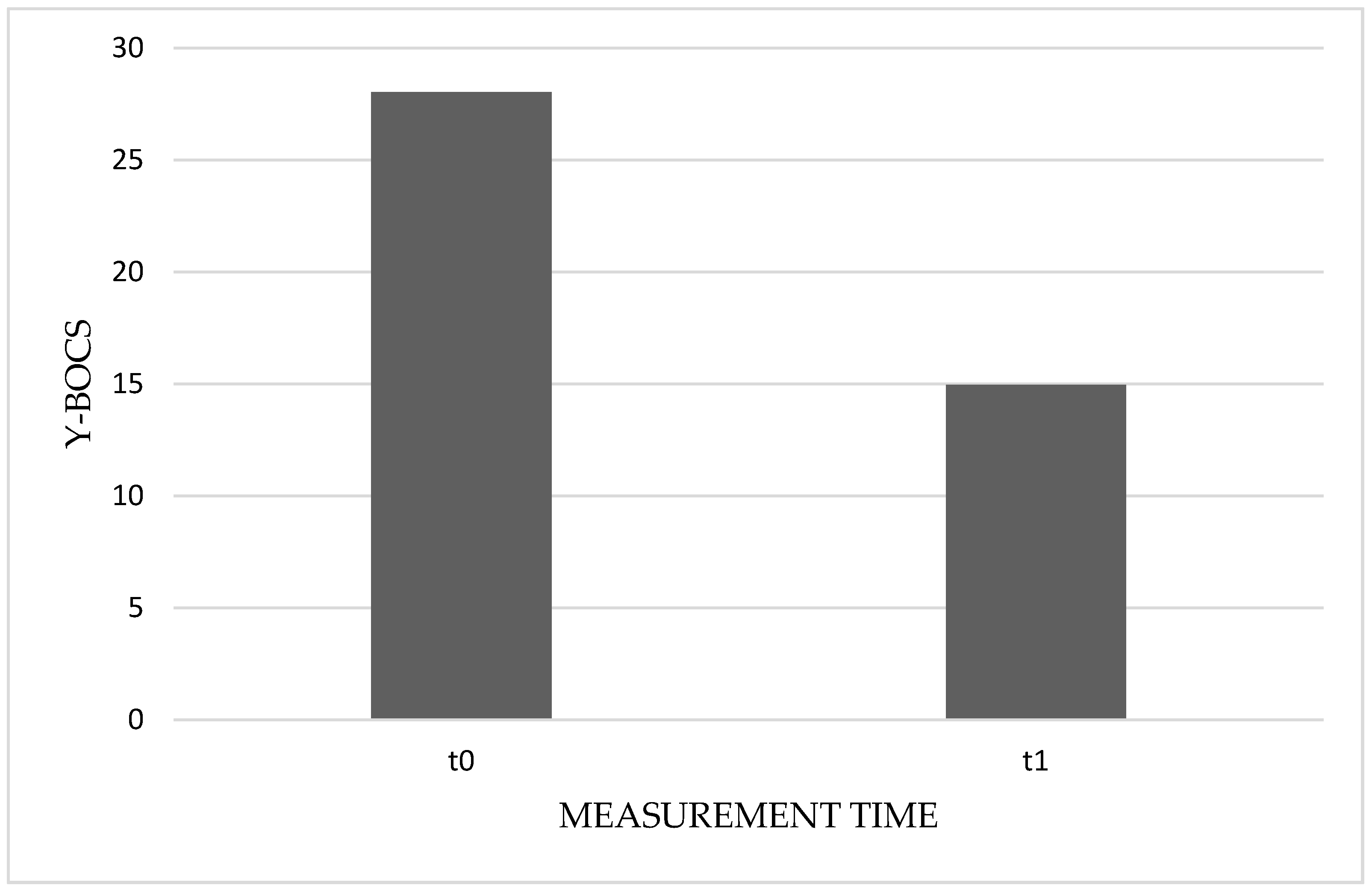
| Measures | Time | Mean | SD | Median | IQR |
|---|---|---|---|---|---|
| Y–BOCS | t0 | 28.03 | 5.30 | 28.00 | 8 |
| t1 | 14.95 | 6.58 | 15.50 | 9 | |
| OBS | t0 | 14.65 | 2.45 | 14.50 | 4 |
| t1 | 8.13 | 3.84 | 8.50 | 5 | |
| COM | t0 | 13.38 | 3.50 | 14.00 | 4 |
| t1 | 6.83 | 3.79 | 7.00 | 5 |
| Measures | Negative Ranks | Positive Ranks | Ties | Total | z | p |
|---|---|---|---|---|---|---|
| Y–BOCS | 40 | 0 | 0 | 40 | −5.51 | <0.001 |
| OBS | 39 | 1 | 0 | 40 | −5.49 | <0.001 |
| COM | 39 | 0 | 1 | 40 | −5.45 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gragnani, A.; Zaccari, V.; Femia, G.; Pellegrini, V.; Tenore, K.; Fadda, S.; Luppino, O.I.; Basile, B.; Cosentino, T.; Perdighe, C.; et al. Cognitive–Behavioral Treatment of Obsessive–Compulsive Disorder: The Results of a Naturalistic Outcomes Study. J. Clin. Med. 2022, 11, 2762. https://doi.org/10.3390/jcm11102762
Gragnani A, Zaccari V, Femia G, Pellegrini V, Tenore K, Fadda S, Luppino OI, Basile B, Cosentino T, Perdighe C, et al. Cognitive–Behavioral Treatment of Obsessive–Compulsive Disorder: The Results of a Naturalistic Outcomes Study. Journal of Clinical Medicine. 2022; 11(10):2762. https://doi.org/10.3390/jcm11102762
Chicago/Turabian StyleGragnani, Andrea, Vittoria Zaccari, Giuseppe Femia, Valerio Pellegrini, Katia Tenore, Stefania Fadda, Olga Ines Luppino, Barbara Basile, Teresa Cosentino, Claudia Perdighe, and et al. 2022. "Cognitive–Behavioral Treatment of Obsessive–Compulsive Disorder: The Results of a Naturalistic Outcomes Study" Journal of Clinical Medicine 11, no. 10: 2762. https://doi.org/10.3390/jcm11102762
APA StyleGragnani, A., Zaccari, V., Femia, G., Pellegrini, V., Tenore, K., Fadda, S., Luppino, O. I., Basile, B., Cosentino, T., Perdighe, C., Romano, G., Saliani, A. M., & Mancini, F. (2022). Cognitive–Behavioral Treatment of Obsessive–Compulsive Disorder: The Results of a Naturalistic Outcomes Study. Journal of Clinical Medicine, 11(10), 2762. https://doi.org/10.3390/jcm11102762







