Sjögren’s Syndrome Associated Dry Eye: Impact on Daily Living and Adherence to Therapy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Survey Design
2.2. Survey Population
2.3. Data Analysis
3. Results
3.1. Demographic Information
3.2. Dry Eye Symptoms Impacting Daily Activities
3.3. Emotional Well-Being and DED
3.4. Income Distribution
3.5. Private Insurance
3.6. Adherence to Treatment
3.7. Variables Influencing Missed Drops
3.8. Cost-Saving Strategies
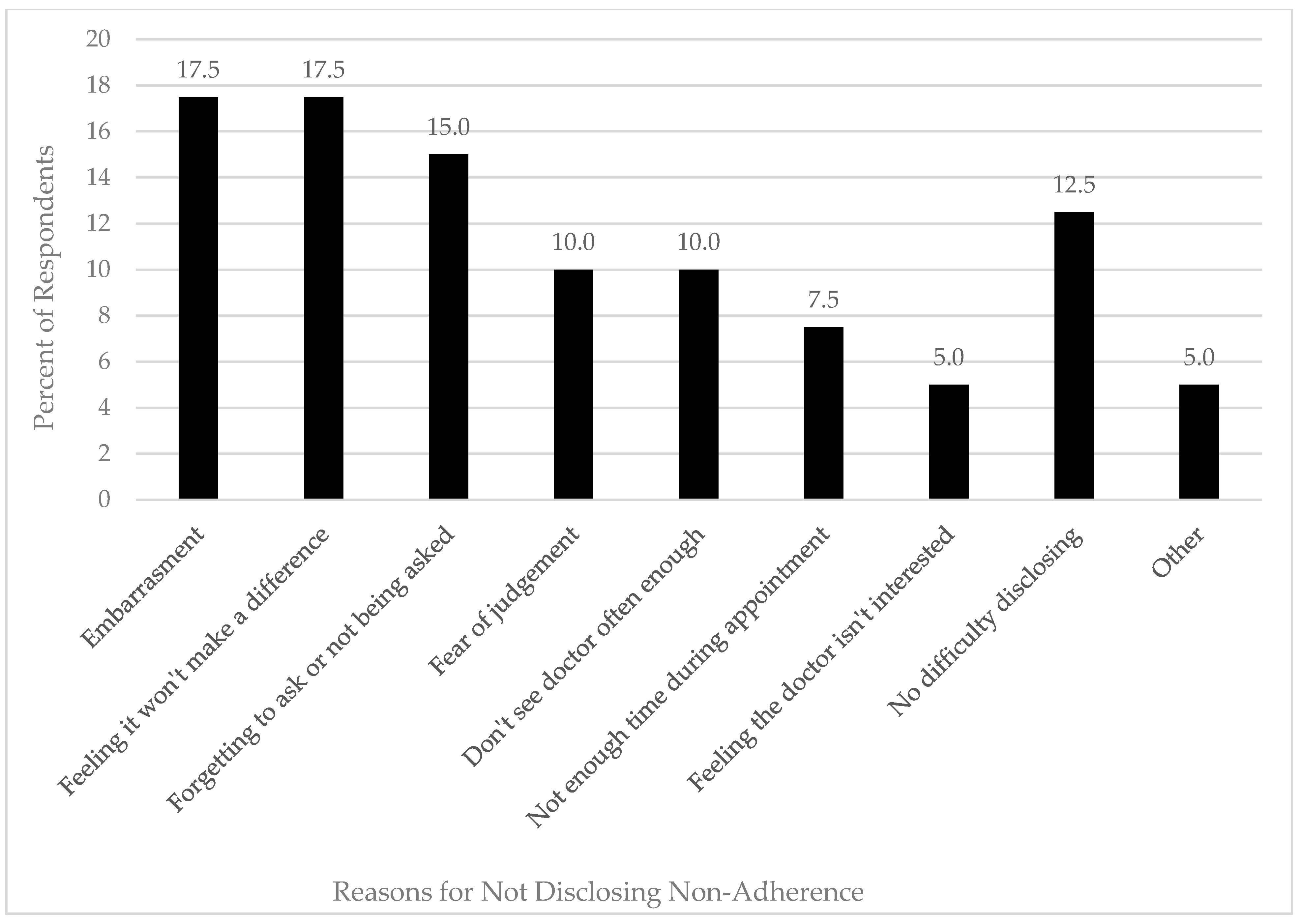
3.9. Disclosure of Non-Adherence
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Appendix A. Survey Questions
Patient Demographics
|
|
|
|
Employed Therapies, Cost, and Insurance
|
|
|
|
|
|
|
__________ |
|
| __________ |
|
Non-Adherence and Rationing Strategies
|
|
|
|
|
|
|
Nondisclosure and Patients Fears
|
|
|
|
|
Appendix B. Patient Open-Ended Response Examples—Response Are Presented Verbatim
| Q15: What are the reasons that you may not be using your dry eye medications and artificial tears as advised by your doctor? | Q16: In order to make your drops last longer, have you ever tried any of the listed techniques (select all that apply)? |
| “I have recently stopped Restasis after 2+ years. It burned my eyes so much I decided to give myself a break. My eyes are much better now without it (4 month).” | “Use Restasis vile twice” |
| “cost prevents me from using the drops on a regular basis and forces me to use them prn” | “I only use them when eyes are bothering me” |
| “I’m grateful for the job that I currently have & that my doctors give me a discount card ... or I’m not sure HOW I would pay for my eye drops that help me to actually see.” | “my ophthalmologist gives me a discount card to help me afford the eye drops” |
| “I drops pur gel in the bottle are difficult to squeeze, it takes a lot of strength to get a drop out.” | “I use a single serve of restasis for two days-once per day” |
| “very inconvenient because only one drugstore that can make perscription drops/must keep perscription drops refridgerated/can only get 2 weeks of drops at a time due to how its made” | “Worked more hours” |
| “I’m compliant for now, but cost may become an issue” |
References
- Qin, B.; Wang, J.; Yang, Z. Epidemiology of primary Sjögren’s syndrome: A Systematic Review and Meta-Analysis. Ann. Rheum. Dis. 2015, 74, 1983–1989. [Google Scholar] [CrossRef] [PubMed]
- Pflugfelder, S.; Huang, A.; Feuer, W.; Chuchovski, P.; Pereira, I.; Tseng, S.C. Conjunctival cytologic features of primary Sjögren’s syndrome. Opthalmology 1990, 97, 985–991. [Google Scholar] [CrossRef]
- Tsubota, K.; Toda, I.; Yagi, Y.; Ogawa, Y.; Ono, M.; Yoshino, K. Three different types of dry eye syndrome. Cornea 1994, 13, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Johnson, M.E. The association between symptoms of discomfort and signs in dry eye. Ocul. Surf. 2009, 7, 199–211. [Google Scholar] [CrossRef]
- Miljanović., B.; Dana, R.; Sullivan, D.A.; Schaumberg, D.A. Impact of Dry Eye Syndrome on Vision-Related Quality of Life. Am. J. Ophthalmol. 2007, 143, 409–415. [Google Scholar] [CrossRef] [Green Version]
- Ahmed, F.; Burt, J.; Rowland, M. Measuring patient experience: Concepts and Methods. Patient Patient-Cent. Outcomes Res. 2014, 7, 235–241. [Google Scholar] [CrossRef] [Green Version]
- McDonald, M.; Patel, D.; Keith, M.; Snedecor, S. Economic and Humanistic Burden of Dry Eye Disease in Europe, North America, and Asia: A Systematic Literature Review. Ocul. Surf. 2016, 14, 144–167. [Google Scholar] [CrossRef] [Green Version]
- Lendrem, D.; Mitchell, S.; McMeekin, P.; Bowman, S.; Price, E.; Pease, C.; Emery, P.; Andrews, J.; Lanyon, P.; Hunter, J.; et al. Health-related utility values of patients with primary Sjögren’s syndrome and its predictors. Ann. Rheum. Dis. 2014, 73, 1362–1368. [Google Scholar] [CrossRef]
- Sjogren’s Society of Canada. 2012. Available online: http://sjogrenscanada.org/ (accessed on 1 August 2020).
- Craig, J.P.; Nichols, K.K.; Akpek, E.K.; Caffery, B.; Dua, H.S.; Joo, C.K.; Liu, Z.; Nelson, J.D.; Nichols, J.J.; Tsubota, K.; et al. TFOS DEWS II Definition and Classification Report. Ocul. Surf. 2017, 15, 276–283. [Google Scholar] [CrossRef]
- Au, N.; Mather, R.; To, A.; Malvankar-Mehta, M. Sleep outcomes associated with dry eye disease: A Systematic Review and Meta-Analysis. Can. J. Opthalmol. 2019, 54, 180–189. [Google Scholar] [CrossRef]
- Saldanha, I.; Bunya, V.; McCoy, S.; Makara, M.; Baer, A.; Akpek, E. Ocular Manifestations and Burden Related to Sjögren’s Syndrome: Results of a Patient Survey. Am. J. Ophthalmol. 2020, 219, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Bury, M. Chronic illness as biographical disruption. Sociol. Health Illn. 1982, 4, 167–182. [Google Scholar] [CrossRef] [PubMed]
- Mirzaei, M.; Aspin, C.; Essue, B.; Jeon, Y.; Dugdale, P.; Usherwood, T.; Leeder, S. A patient-centred approach to health service delivery: Improving Health Outcomes for People with Chronic Illness. BMC Health Serv. Res. 2013, 13, 251. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rahimi, A.R.; Spertus, J.A.; Reid, K.J.; Bernheim, S.M.; Krumholz, H.M. Financial Barriers to Health Care and Outcomes After Acute Myocardial Infarction. JAMA 2007, 297, 1063–1072. [Google Scholar] [CrossRef] [Green Version]
- Zeber, J.E.; Miller, A.L.; Copeland, L.A.; McCarthy, J.F.; Zivin, K.; Valenstein, M.; Greenwald, D.; Kilbourne, A.M. Medication adherence, ethnicity, and the influence of multiple psychosocial and financial barriers. Adm. Policy Ment. Health Ment. Health Serv. Res. 2011, 38, 86–95. [Google Scholar] [CrossRef]
- Statistics Canada. Household Income in Canada: Key Results from the 2016 Census; Statistics Canada: Ottawa, ON, Canada, 2017.
- Winfield, A.J.; Jessiman, D.; Williams, A.; Esakowitz, L. A study of the causes of non-compliance by patients prescribed eyedrops. Br. J. Ophthalmol. 1990, 74, 477–480. [Google Scholar] [CrossRef] [Green Version]
- Tatham, A.J.; Sarodia, U.; Gatrad, F.; Awan, A. Eye drop instillation technique in patients with glaucoma. Eye 2013, 27, 1293–1298. [Google Scholar] [CrossRef] [Green Version]
- Uchino, M.; Yokoi, N.; Shimazaki, J.; Hori, Y.; Tsubota, K. Adherence to Eye Drops Usage in Dry Eye Patients and Reasons for Non-Compliance: A Web-Based Survey. J. Clin. Med. 2022, 11, 367. [Google Scholar] [CrossRef]
- Balkrishnan, R. Predictors of medication adherence in the elderly. Clin. Ther. 1998, 20, 764–771. [Google Scholar] [CrossRef]
- Yap, A.F.; Thirumoorthy, T.; Kwan, Y.H. Medication adherence in the elderly. J. Clin. Gerontol. Geriatr. 2016, 7, 64–67. [Google Scholar] [CrossRef] [Green Version]
- Claxton, A.J.; Cramer, J.; Pierce, C. A systematic review of the associations between dose regimens and medication compliance. Clin. Ther. 2001, 23, 1296–1310. [Google Scholar] [CrossRef]
- Col, N.; Fanale, J.E.; Kronholm, P. The role of medication noncompliance and adverse drug reactions in hospitalizations of the elderly. Arch. Intern. Med. 1990, 150, 841–845. [Google Scholar] [CrossRef] [PubMed]



| Total Respondents Analyzed | 244 |
|---|---|
| Gender (%) | |
| Male | 59 (24.2%) |
| Female | 183 (75.0%) |
| Non-binary/Third gender | 1 (0.4%) |
| Prefer not to disclose | 1 (0.4%) |
| Age | |
| Mean (SD) | 59.9 (12.4) |
| Median (IQR 1–3) | 61 (53–68) |
| Years since Sjögren’s Diagnosis | |
| Mean (SD) | 9.6 (8.6) |
| Median (IQR1–3) | 8 (3–13) |
| Diagnosis By (%) *: | |
| Ophthalmologist | 58 (23.8%) |
| Rheumatologist | 171 (70.1%) |
| Family Physician | 54 (22.1%) |
| Dentist | 30 (12.3%) |
| Private Medical Insurance | 137 (56.1%) |
| Coverage prescription eye drops | 87 (35.7%) |
| Coverage non-prescription eye drops | 7 (2.9%) |
| Income Distribution (CAD) | |
| <$39,000 | (27.5%) |
| $40,000–$69,999 | (23.8%) |
| $70,000–$99,999 | (16.8%) |
| >$100,000 | (18.9%) |
| Prefer not to disclose | (13.5%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Michaelov, E.; McKenna, C.; Ibrahim, P.; Nayeni, M.; Dang, A.; Mather, R. Sjögren’s Syndrome Associated Dry Eye: Impact on Daily Living and Adherence to Therapy. J. Clin. Med. 2022, 11, 2809. https://doi.org/10.3390/jcm11102809
Michaelov E, McKenna C, Ibrahim P, Nayeni M, Dang A, Mather R. Sjögren’s Syndrome Associated Dry Eye: Impact on Daily Living and Adherence to Therapy. Journal of Clinical Medicine. 2022; 11(10):2809. https://doi.org/10.3390/jcm11102809
Chicago/Turabian StyleMichaelov, Evan, Caroline McKenna, Pierre Ibrahim, Manav Nayeni, Arpit Dang, and Rookaya Mather. 2022. "Sjögren’s Syndrome Associated Dry Eye: Impact on Daily Living and Adherence to Therapy" Journal of Clinical Medicine 11, no. 10: 2809. https://doi.org/10.3390/jcm11102809






