No Significant Bone Resorption after Open Treatment of Mandibular Condylar Head Fractures in the Medium-Term
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
- Displaced condylar head fracture type M or P according to Neff et al. [2], regardless of the degree of fragmentation (none, minor, major) and vertical apposition (complete, partial, or lost).
- Open reduction and internal fixation (ORIF) were performed using positional screws with or without additional mini-plate osteosynthesis.
- Complete patient documentation during follow-up of at least 6 months.
- Postoperative and follow-up cone beam computed tomography (CBCT) scans of appropriate quality allowing for 3D-segmentation.
- Fulfilled patient consent. Patients were excluded if they were lost to a follow-up.
2.2. Variables
2.2.1. Clinical Parameters and Outcome Measures
2.2.2. Surgical Procedure
2.3. Data Collection Methods
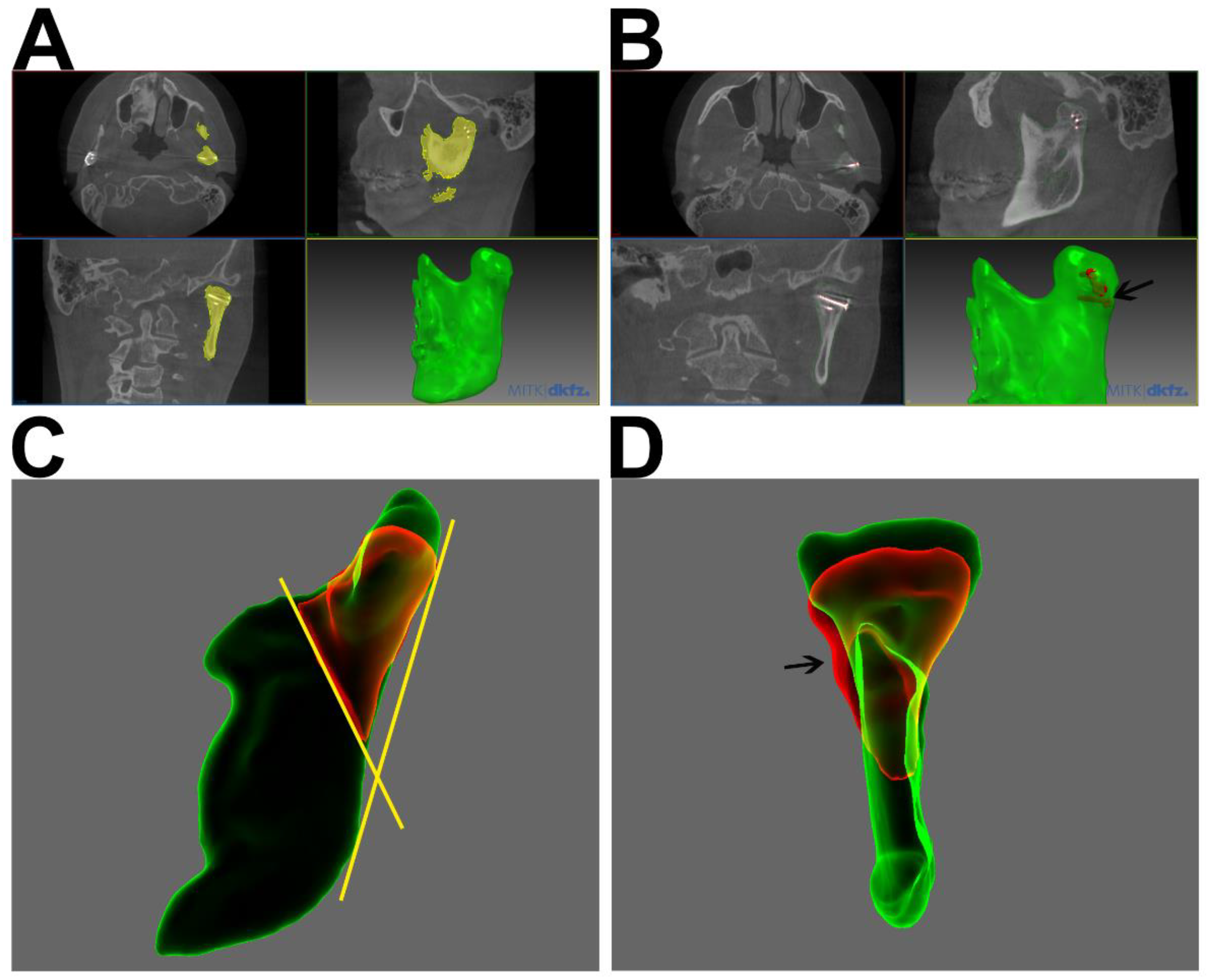
2.3.1. 3D Segmentation and Analysis
2.3.2. Data Analysis
3. Results
3.1. Demographics and Etiology
3.2. Fracture Topography and Classification
3.3. Clinical and Surgical Parameters
Morphological Alterations of the Condylar Head
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bormann, K.H.; Wild, S.; Gellrich, N.C.; Kokemüller, H.; Stühmer, C.; Schmelzeisen, R.; Schön, R. Five-Year Retrospective Study of Mandibular Fractures in Freiburg, Germany: Incidence, Etiology, Treatment and Complications. J. Oral Maxillofac. Surg. 2009, 67, 1251–1255. [Google Scholar] [CrossRef] [PubMed]
- Neff, A.; Cornelius, C.P.; Rasse, M.; Torre, D.; Audigé, L. The comprehensive AOCMF classification system: Condylar process fractures—Level 3 tutorial. Craniomaxillofac. Trauma Reconstr. 2014, 7, S44–S58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neff, A.; Chossegros, C.; Blanc, J.L.; Champsaur, P.; Cheynet, F.; Devauchelle, B.; Eckelt, U.; Ferri, J.; Gabrielli, M.F.R.; Guyot, L.; et al. Position paper from the IBRA Symposium on Surgery of the Head—International Symposium for Condylar Fracture Osteosynthesis, Marseille, France 2012. J. Cranio-Maxillofac. Surg. 2014, 42, 1234–1249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neff, A. Open reduction and internal fixation in temporomandibular joint traumatology: Current concepts and future perspectives. Stomatol. Dis. Sci. 2019, 3, 2. [Google Scholar] [CrossRef] [Green Version]
- Neuhaus, M.T.; Zeller, A.N.; Desch, L.; Dhawan, A.; Jehn, P.; Gellrich, N.-C.; Zimmerer, R. Endoscopically Assisted Treatment of Condylar Base and Neck Fractures: A Single Institution Analysis of Outcomes and Complications. J. Maxillofac. Oral Surg. 2021, 20, 665–673. [Google Scholar] [CrossRef] [PubMed]
- Neff, A.; Cornelius, C.-P.; Rasse, M.; Audigé, L. Kiefergelenkfortsatzfrakturen nach der AO-CMF-Trauma-KlassifikationCondylar process fractures according to the AO CMF trauma classification. Der. MKG-Chirurg. 2017, 10, 113–126. [Google Scholar] [CrossRef]
- Loukota, R.A.; Neff, A.; Rasse, M. Nomenclature/classification of fractures of the mandibular condylar head. Br. J. Oral Maxillofac. Surg. 2010, 48, 477–478. [Google Scholar] [CrossRef]
- Yao, S.; Zhou, J.; Li, Z. Contrast analysis of open reduction and internal fixation and non-surgical treatment of condylar fracture: A meta-analysis. J. Craniofac. Surg. 2014, 25, 2077–2080. [Google Scholar] [CrossRef]
- Chen, C.T.; Feng, C.H.; Tsay, P.K.; Lai, J.-P.; Chen, Y.-R. Functional outcomes following surgical treatment of bilateral mandibular condylar fractures. Int. J. Oral Maxillofac. Surg. 2011, 40, 38–44. [Google Scholar] [CrossRef]
- Smets, L.M.H.; Van Damme, P.A.; Stoelinga, P.J.W. Non-surgical treatment of condylar fractures in adults: A retrospective analysis. J. Cranio-Maxillofac. Surg. 2003, 31, 162–167. [Google Scholar] [CrossRef]
- Nussbaum, M.L.; Laskin, D.M.; Best, A.M. Closed Versus Open Reduction of Mandibular Condylar Fractures in Adults: A Meta-Analysis. J. Oral Maxillofac. Surg. 2008, 66, 1087–1092. [Google Scholar] [CrossRef] [PubMed]
- Ren, R.; Dai, J.; Zhi, Y.; Xi, F.; Shi, J. Comparison of temporomandibular joint function and morphology after surgical and non-surgical treatment in adult condylar head fractures. J. Cranio-Maxillofac. Surg. 2020, 48, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Ho, S.Y.-C.; Liao, H.-T.; Chen, C.-H.; Chen, Y.-C.; Chen, Y.-R.; Chen, C.-T. The radiographic and functional outcome of bilateral mandibular condylar head fractures: A comparison between open and closed treatment. Ann. Plast. Surg. 2015, 74, S93–S98. [Google Scholar] [PubMed]
- Kolk, A.; Neff, A. Long-term results of ORIF of condylar head fractures of the mandible: A prospective 5-year follow-up study of small-fragment positional-screw osteosynthesis (SFPSO). J. Cranio-Maxillofac. Surg. 2015, 43, 452–461. [Google Scholar] [CrossRef]
- Johner, J.P.; Essig, H.; Neff, A.; Wagner, M.E.; Blumer, M.; Gander, T. Volumetric Evaluated Bone Resorption After Open Reduction and Internal Fixation of Condylar Head Fractures of the Mandible. J. Oral Maxillofac. Surg. 2021, 79, 1902–1913. [Google Scholar] [CrossRef]
- Schneider, M.; Erasmus, F.; Gerlach, K.L.; Kuhlisch, E.; Loukota, R.A.; Rasse, M.; Schubert, J.; Terheyden, H.; Eckelt, U. Open Reduction and Internal Fixation Versus Closed Treatment and Mandibulomaxillary Fixation of Fractures of the Mandibular Condylar Process: A Randomized, Prospective, Multicenter Study With Special Evaluation of Fracture Level. J. Oral Maxillofac. Surg. 2008, 66, 2537–2544. [Google Scholar] [CrossRef]
- Xin, P.; Jiang, B.; Dai, J.; Hu, G.; Wang, X.; Xu, B.; Shen, S.G. Finite element analysis of type B condylar head fractures and osteosynthesis using two positional screws. J Cranio-Maxillofac. Surg. 2014, 42, 482–488. [Google Scholar] [CrossRef]
- Xie, S.T.; Singhal, D.; Chen, C.T.; Chen, Y.-R. Functional and radiologic outcome of open reduction and internal fixation of condylar head and neck fractures using miniplate or microplate system. Ann. Plast. Surg. 2013, 71 (Suppl. 1), S61–S66. [Google Scholar] [CrossRef]
- Smolka, W.; Cornelius, C.P.; Lechler, C. Resorption behaviour of the articular surface dome and functional outcome after open reduction and internal fixation of mandibular condylar head fractures using small-fragment positional screws. J. Cranio-Maxillofac. Surg. 2018, 46, 1953–1959. [Google Scholar] [CrossRef]
- Skroch, L.; Fischer, I.; Meisgeier, A.; Kozolka, F.; Apitzsch, J.; Neff, A. Condylar remodeling after osteosynthesis of fractures of the condylar head or close to the temporomandibular joint. J. Cranio-Maxillofac. Surg. 2020, 48, 413–420. [Google Scholar] [CrossRef]
- Neff, A.; Mühlberger, G.; Karoglan, M.; Kolk, A.; Mittelmeier, W.; Scheruhn, D.A.; Schieferstein, H. Stability of osteosyntheses for condylar head fractures in the clinic and biomechanical simulation. Mund Kiefer Gesichtschir. 2004, 8, 63–74. [Google Scholar] [CrossRef]
- Neff, A.; Kolk, A.; Meschke, F.; Deppe, H.; Horch, H.-H. Small fragment screws vs. plate osteosynthesis in condylar head fractures. A comparison of functional results based on MRI and axiography. Mund-Kiefer-Und Gesichtschir. 2005, 9, 80–88. [Google Scholar] [CrossRef]
- Hlawitschka, M.; Loukota, R.; Eckelt, U. Functional and radiological results of open and closed treatment of intracapsular (diacapitular) condylar fractures of the mandible. Int. J. Oral Maxillofac. Surg. 2005, 34, 597–604. [Google Scholar] [CrossRef]
- Otsu, N. Threshold Selection Method From Gray-Level Histograms. IEEE Trans. Syst. Man Cybern. 1979, 9, 62–66. [Google Scholar] [CrossRef] [Green Version]
- Schneider, M.; Stadlinger, B.; Loukota, R.; Eckelt, U. Three-dimensional fixation of fractures of the mandibular condyle with a resorbable three-dimensional osteosynthesis mesh. Br. J. Oral Maxillofac. Surg. 2012, 50, 470–473. [Google Scholar] [CrossRef]
- Schneider, M.; Seinige, C.; Pilling, E.; Rasse, M.; Loukota, R.; Stadlinger, B.; Mai, R.; Eckelt, U. Ultrasound-aided resorbable osteosynthesis of fractures of the mandibular condylar base: An experimental study in sheep. Br. J. Oral Maxillofac. Surg. 2012, 50, 528–532. [Google Scholar] [CrossRef]
- Schumann, P.; Lindhorst, D.; Wagner, M.E.; Schramm, A.; Gellrich, N.-C.; Rücker, M. Perspectives on resorbable osteosynthesis materials in craniomaxillofacial surgery. Pathobiology 2013, 80, 211–217. [Google Scholar] [CrossRef]
- Helkimo, M.I.; Bailey, J.O.; Ash, M.M. Correlations of electromyographic silent period duration and the helkimo dysfunction index. Acta Odontol. Scand. 1979, 37, 51–56. [Google Scholar] [CrossRef]
- Prakash, R., Sr.; Ramesh, K.; Alwala, A.M.; Porika, R.; Manjusha; Katkuri, S. Open Reduction and Internal Fixation versus Closed Reduction and Maxillomandibular Fixation of Condylar Fractures of the Mandible: A Prospective Study. Cureus 2022, 14, e21186. [Google Scholar] [CrossRef]



| Clinical Parameters | No. of Cases | [%] |
|---|---|---|
| Total n = 18 | ||
| Cause of trauma | ||
| Fall | 12 | 66.7 |
| Traffic accident | 5 | 27.8 |
| Violence | 1 | 5.6 |
| Fracture classification | ||
| Non/slightly displaced | 1 | 5.6 |
| Displaced | 13 | 72.2 |
| Comminuted and displaced | 11 | 61.1 |
| Additional fractures | ||
| Median | 7 | 38.9 |
| Paramedian | 3 | 16.7 |
| Collum | 3 | 16.7 |
| Total cases with additional fractures | 10 | 55.6 |
| Osteosynthesis type | ||
| 2 positioning screws | 15 | 60.0 |
| 3 positioning screws | 3 | 12.0 |
| 1 × 4-hole plate | 3 | 12.0 |
| 2 plates | 2 | 8.0 |
| Others | 2 | 8.0 |
| Follow up CBCT diagnosis | ||
| No change | 6 | 24.0 |
| Resorption | 14 | 56.0 |
| Arthrosis | 3 | 12.0 |
| Osteosynthesis failure | 1 | 4.0 |
| Intraarticular screw | 4 | 16.0 |
| Sequester | 1 | 4.0 |
| Callus | 4 | 16.0 |
| Clinical Parameters | Mean | SEM | p |
|---|---|---|---|
| MIO preop [mm] | 19.71 | 3.51 | |
| MIO follow up [mm] | 40.47 | 1.70 | 0.0001 |
| Laterotrusion follow up [mm] | 5.56 | 0.83 | |
| Pain preop (VAS) | 5.00 | 0.61 | |
| Pain follow up (VAS) | 0.33 | 0.19 | 0.008 |
| Surgical time pre fracture [min] | 120.09 | 9.03 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Neuhaus, M.-T.; Gellrich, N.-C.; Sander, A.K.; Lethaus, B.; Halama, D.; Zimmerer, R.M. No Significant Bone Resorption after Open Treatment of Mandibular Condylar Head Fractures in the Medium-Term. J. Clin. Med. 2022, 11, 2868. https://doi.org/10.3390/jcm11102868
Neuhaus M-T, Gellrich N-C, Sander AK, Lethaus B, Halama D, Zimmerer RM. No Significant Bone Resorption after Open Treatment of Mandibular Condylar Head Fractures in the Medium-Term. Journal of Clinical Medicine. 2022; 11(10):2868. https://doi.org/10.3390/jcm11102868
Chicago/Turabian StyleNeuhaus, Michael-Tobias, Nils-Claudius Gellrich, Anna Katharina Sander, Bernd Lethaus, Dirk Halama, and Rüdiger M. Zimmerer. 2022. "No Significant Bone Resorption after Open Treatment of Mandibular Condylar Head Fractures in the Medium-Term" Journal of Clinical Medicine 11, no. 10: 2868. https://doi.org/10.3390/jcm11102868
APA StyleNeuhaus, M.-T., Gellrich, N.-C., Sander, A. K., Lethaus, B., Halama, D., & Zimmerer, R. M. (2022). No Significant Bone Resorption after Open Treatment of Mandibular Condylar Head Fractures in the Medium-Term. Journal of Clinical Medicine, 11(10), 2868. https://doi.org/10.3390/jcm11102868






