Review of 107 Oncoplastic Surgeries Using an Acellular Dermal Matrix with the Round Block Technique
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
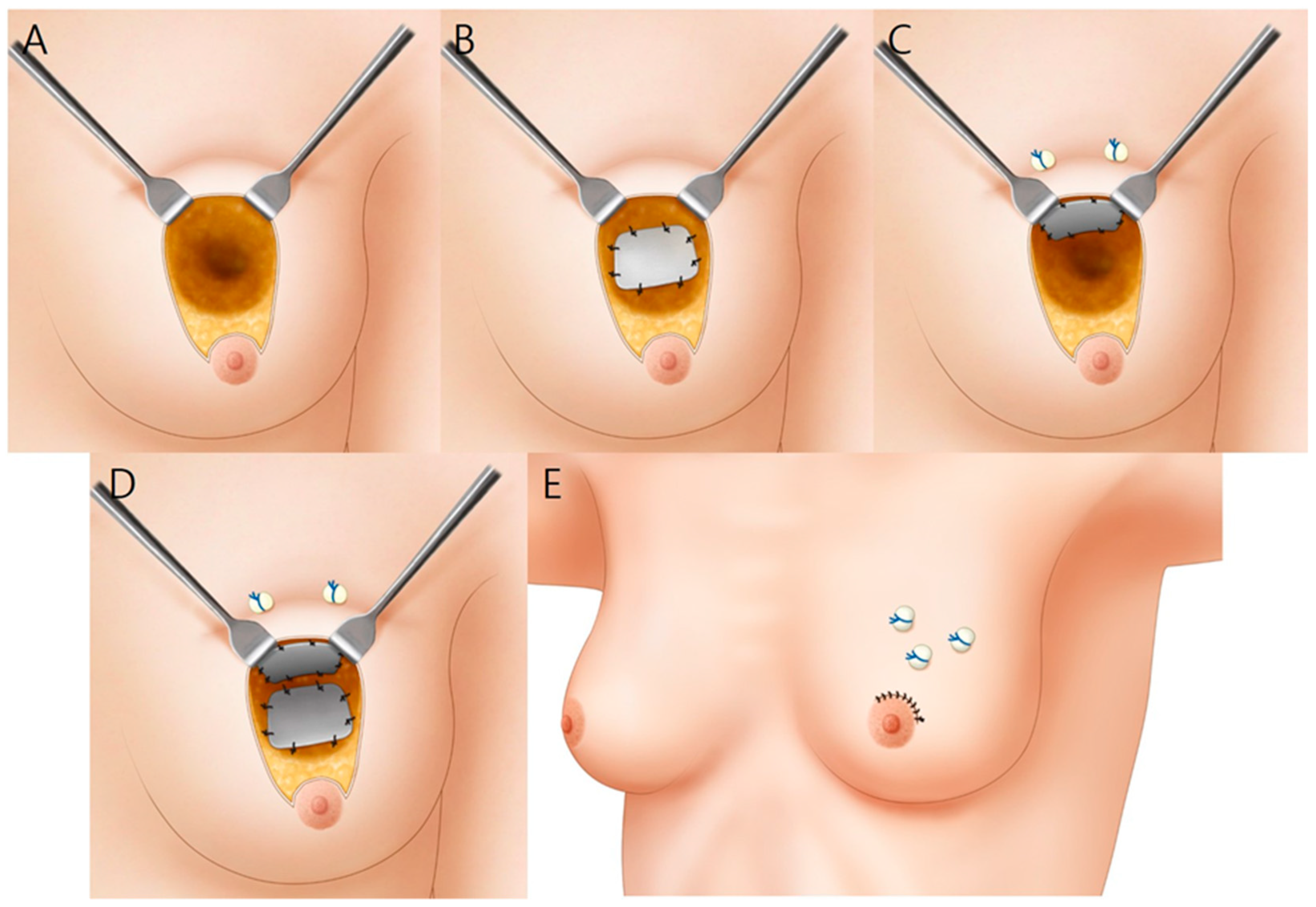
2.2. Surgical Technique
2.3. Satisfaction Survey and Complications
3. Results
3.1. Patients’ Characteristics
3.2. Satisfactory and Cosmetic Outcome Evaluation
3.3. Postoperative Complication Data
4. Discussion
4.1. Oncoplastic BCS
4.2. Surgical Method
4.3. Complications
4.4. ADM
4.5. Oncoplastic Surgery and ADM Usage
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Audretsch, W.P.; Rezai, M.; Kolotas, C.; Zamboglou, N.; Schnabel, T.; Bojar, H. Tumor-specific immediate reconstruction in breast cancer patients. Semin. Plast. Surg. 1998, 11, 71–100. [Google Scholar] [CrossRef] [Green Version]
- Benelli, L. A new periareolar mammaplasty: The “Round block” technique. Aesthetic Plast. Surg. 1990, 14, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Anderson, B.O.; Masetti, R.; Silverstein, M.J. Oncoplastic approaches to partial mastectomy: An overview of volume-displacement techniques. Lancet Oncol. 2005, 6, 145–157. [Google Scholar] [CrossRef]
- Yang, J.D.; Lee, J.W.; Kim, W.W.; Jung, J.H.; Park, H.Y. Oncoplastic Surgical Techniques for Personalized Breast Conserving Surgery in Breast Cancer Patient with Small to Moderate Sized Breast. J. Breast Cancer. 2011, 14, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, T. Usefulness of breast-conserving surgery using the round block technique or modified round block technique in Japanese females. Asian J. Surg. 2014, 37, 8–14. [Google Scholar] [CrossRef] [Green Version]
- Yang, J.D.; Bae, S.G.; Chung, H.Y.; Cho, B.C.; Park, H.Y.; Jung, J.H. The usefulness of oncoplastic volume displacement techniques in the superiorly located breast cancers for Korean patients with small to moderate-sized breasts. Ann. Plast. Surg. 2011, 67, 474–480. [Google Scholar] [CrossRef]
- Cano, S.J.; Klassen, A.F.; Scott, A.M.; Cordeiro, P.G.; Pusic, A.L. The BREAST-Q: Further Validation in Independent Clinical Samples. Plast. Reconstr. Surg. 2012, 129, 293–302. [Google Scholar] [CrossRef]
- Dikmans, R.E.; Nene, L.E.; Bouman, M.B.; de Vet, H.C.; Mureau, M.A.; Buncamper, M.E.; Winters, H.A.; Ritt, M.J.; Mullender, M.G. The Aesthetic Items Scale: A Tool for the Evaluation of Aesthetic Outcome after Breast Reconstruction. Plast. Reconstr. Surg. Glob. Open 2017, 5, e1254. [Google Scholar] [CrossRef]
- Berrino, P.; Campora, E.; Santi, P. Postquadrantectomy Breast Deformities Classification and Techniques of Surgical Correction. Plast. Reconstr. Surg. 1987, 79, 567–572. [Google Scholar] [CrossRef]
- Cochrane, R.A.; Valasiadou, P.; Wilson, A.R.M.; Al-Ghazal, S.K.; Macmillan, R.D. Cosmesis and satisfaction after breast-conserving surgery correlates with the percentage of breast volume excised. Br. J. Surg. 2003, 90, 1505–1509. [Google Scholar] [CrossRef]
- Clough, K.B.; Kaufman, G.J.; Nos, C.; Buccimazza, I.; Sarfati, I.M. Improving breast cancer surgery: A classification and quadrant per quadrant atlas for oncoplastic surgery. Ann. Surg. Oncol. 2010, 17, 1375–1391. [Google Scholar] [CrossRef] [PubMed]
- Clough, K.B.; Gouveia, P.F.; Benyahi, D.; Massey, E.J.; Russ, E.; Sarfati, I.; Nos, C. Positive Margins After Oncoplastic Surgery for Breast Cancer. Ann. Surg. Oncol. 2015, 22, 4247–4253. [Google Scholar] [CrossRef] [PubMed]
- Kempa, S.; Brix, E.; Heine, N.; Hösl, V.; Strauss, C.; Eigenberger, A.; Brébant, V.; Seitz, S.; Prantl, L. Autologous fat grafting for breast reconstruction after breast cancer: A 12-year experience. Arch. Gynecol. Obstet. 2022, 4, 921–927. [Google Scholar] [CrossRef]
- Gwak, H.K.; Jeon, Y.W.; Lim, S.T.; Park, S.Y.; Suh, Y.J. Volume replacement with diced acellular dermal matrix in oncoplastic breast-conserving surgery: A prospective single-center experience. World J. Surg. Oncol. 2020, 18, 60. [Google Scholar] [CrossRef]
- Lee, J.H.; Kim, H.G.; Lee, W.J. Characterization and tissue incorporation of cross-linked human acellular dermal matrix. Biomaterials 2015, 44, 195–205. [Google Scholar] [CrossRef]
- Bulstrode, N.W.; Shrotria, S. Prediction of cosmetic outcome following conservative breast surgery using breast volume measurements. Breast 2001, 10, 124–126. [Google Scholar] [CrossRef]
- Shin, E.S.; Kim, H.I.; Song, S.Y.; Lew, D.H.; Lee, D.W. Selection of oncoplastic surgical technique in Asian breast cancer patients. Arch. Plast. Surg. 2018, 45, 37–44. [Google Scholar] [CrossRef] [Green Version]
- In, S.K.; Kim, Y.S.; Kim, H.S.; Park, J.H.; Kim, H.I.; Yi, H.S.; Park, J.C.; Jeon, C.W.; Choi, J.H.; Jung, S.U.; et al. Retrospective review of 108 breast reconstructions using the round block technique after breast-conserving surgery: Indications, complications, and outcomes. Arch. Plast. Surg. 2020, 47, 574–582. [Google Scholar] [CrossRef]
- Fasnot, J.; Kovach, S.J., 3rd; Serletti, J.M. Acellular Dermal Matrix: General Principles for the Plastic Surgeon. Aesthet. Surg. J. 2011, 31, 5S–12S. [Google Scholar] [CrossRef] [Green Version]
- Sorkin, M.; Qi, J.; Kim, H.M.; Hamill, J.B.; Kozlow, J.H.; Pusic, A.L.; Wilkins, E.G. Acellular Dermal Matrix in Immediate Expander/Implant Breast Reconstruction: A Multicenter Assessment of Risks and Benefits. Plast. Reconstr. Surg. 2017, 140, 1091–1100. [Google Scholar] [CrossRef]
- Park, J.H.; Choi, J.H.; Jin, U.S.; Minn, K.W. Implant breast reconstruction after mastectomy using CG CryoDerm®: A Comparative Study with Acellular dermal matrix (AlloDerm®). In Proceedings of the Scientific Cooperations International Workshops on Medical Topics, Ankara, Turkey, 7–8 June 2014. [Google Scholar]
- Delay, E.; Guerid, S.; Meruta, A.C. Indications and Controversies in Lipofilling for Partial Breast Reconstruction. Clin. Plast. Surg. 2018, 45, 101–110. [Google Scholar] [CrossRef]
- Elliott, L.F.; Ghazi, B.H.; Otterburn, D.M. The Scarless Latissimus Dorsi Flap for Full Muscle Coverage in Device-Based Immediate Breast Reconstruction: An Autologous Alternative to Acellular Dermal Matrix. Plast. Reconstr. Surg. 2011, 128, 71–79. [Google Scholar] [CrossRef]





| Variables | Value * |
|---|---|
| Total number of patients | 105 |
| Total number of oncoplastic surgeries | 107 |
| 1 ADM graft | 57 (53.3%) |
| 2 ADM grafts | 50 (46.7%) |
| Age (year) | 48.3 ± 8.3 (25–67) |
| BMI (kg/m2) | 23.5 ± 2.9 (18.0–32.8) |
| Follow-up period | 15.2 ± 1.9 (12–18) |
| Breast tumor quadrant | |
| Upper outer | 51 (47.7%) |
| Upper inner | 24 (22.4%) |
| Lower outer | 22 (20.6%) |
| Lower inner | 10 (9.3%) |
| Histological type | |
| Invasive ductal carcinoma | 84 (78.5%) |
| Ductal carcinoma in situ | 17 (15.9%) |
| Tubular carcinoma | 3 (2.8%) |
| Mucinous carcinoma | 2 (1.9%) |
| Invasive lobular carcinoma | 1 (0.9%) |
| Mean resected breast tissue (g) | 27.1 ± 17.4 (6–102) |
| 0–50 | 89 (83.2%) |
| 50–100 | 16 (14.9%) |
| >100 | 2 (1.9%) |
| Treatment | |
| Neoadjuvant chemotherapy | 20 (19.0%) |
| Radiotherapy | 104 (99.0%) |
| Adjuvant chemotherapy | 58 (55.2%) |
| Variables | Value * |
|---|---|
| BREAST-Q score | 84.0 ± 9.3 (62–100) |
| Median AIS score | 4.7 ± 0.6 (3.3–4.8) |
| Variables | Value * |
|---|---|
| Postoperative complications | 35 (32.7) |
| Seroma | 33 (30.8) |
| 1 ADM graft | 12 (21.1) |
| 2 ADM grafts | 21 (42.0) |
| Hematoma | 1 (0.9) |
| Infection | 1 (0.9) |
| Cosmetic problems | 5 (4.6) |
| Depression deformity | 4 (3.7) |
| Bulging deformity | 1 (0.9) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.-I.; Kim, B.-S.; Kim, Y.-S.; Yi, H.-S.; Park, J.-H.; Choi, J.-H.; Jung, S.-U.; Kim, H.-Y. Review of 107 Oncoplastic Surgeries Using an Acellular Dermal Matrix with the Round Block Technique. J. Clin. Med. 2022, 11, 3005. https://doi.org/10.3390/jcm11113005
Kim H-I, Kim B-S, Kim Y-S, Yi H-S, Park J-H, Choi J-H, Jung S-U, Kim H-Y. Review of 107 Oncoplastic Surgeries Using an Acellular Dermal Matrix with the Round Block Technique. Journal of Clinical Medicine. 2022; 11(11):3005. https://doi.org/10.3390/jcm11113005
Chicago/Turabian StyleKim, Hong-Il, Byeong-Seok Kim, Yoon-Soo Kim, Hyung-Suk Yi, Jin-Hyung Park, Jin-Hyuk Choi, Sung-Ui Jung, and Hyo-Young Kim. 2022. "Review of 107 Oncoplastic Surgeries Using an Acellular Dermal Matrix with the Round Block Technique" Journal of Clinical Medicine 11, no. 11: 3005. https://doi.org/10.3390/jcm11113005
APA StyleKim, H.-I., Kim, B.-S., Kim, Y.-S., Yi, H.-S., Park, J.-H., Choi, J.-H., Jung, S.-U., & Kim, H.-Y. (2022). Review of 107 Oncoplastic Surgeries Using an Acellular Dermal Matrix with the Round Block Technique. Journal of Clinical Medicine, 11(11), 3005. https://doi.org/10.3390/jcm11113005






