The Incidence of Chronic Limb-Threatening Ischemia in the Midland Region of New Zealand over a 12-Year Period
Abstract
:1. Introduction
2. Materials and Methods
- Age < 18 years.
- Surgical or endovascular management of acute lower limb ischemia.
- Surgical or endovascular management of aneurysmal disease (unless PAD symptomology with angiographic evidence of PAD concomitant).
- Diagnostic lower limb angiogram without angioplasty.
- Repeated revascularization of previous bypass or endovascular intervention.
- Amputation for trauma, tumor, acute limb ischemia or diabetic foot disease without PAD or infection.
3. Results
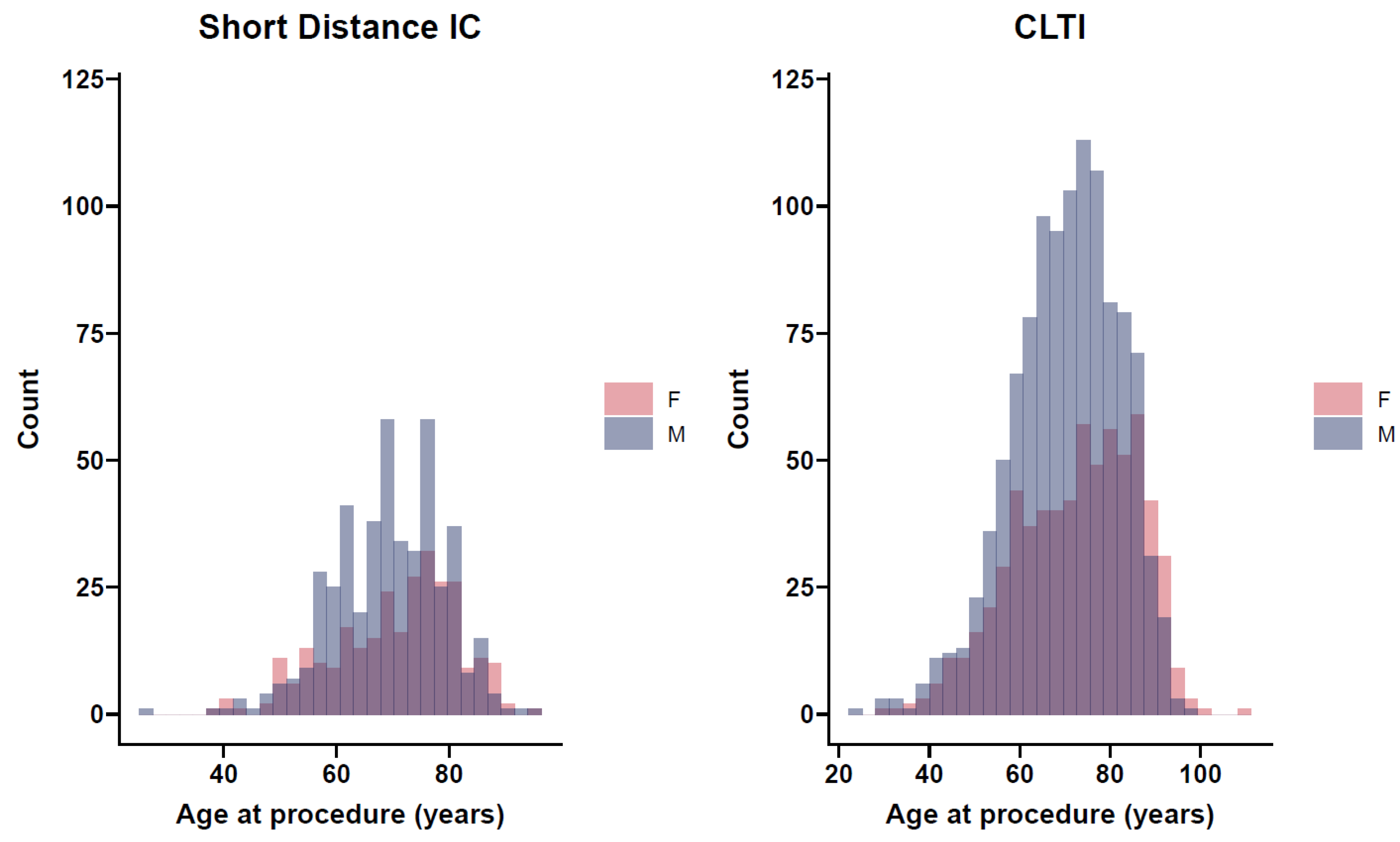
3.1. Demographics
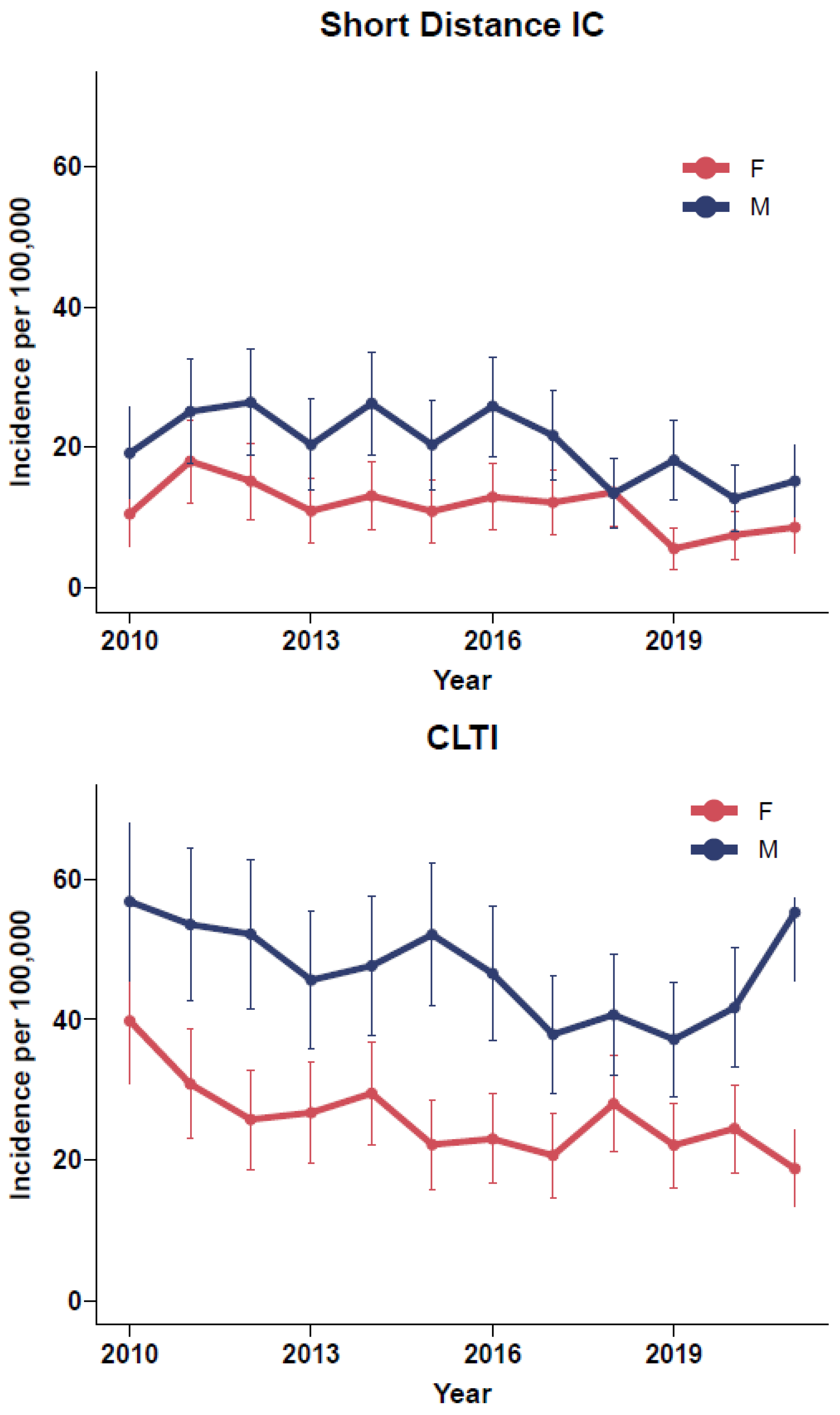
3.2. Incidence
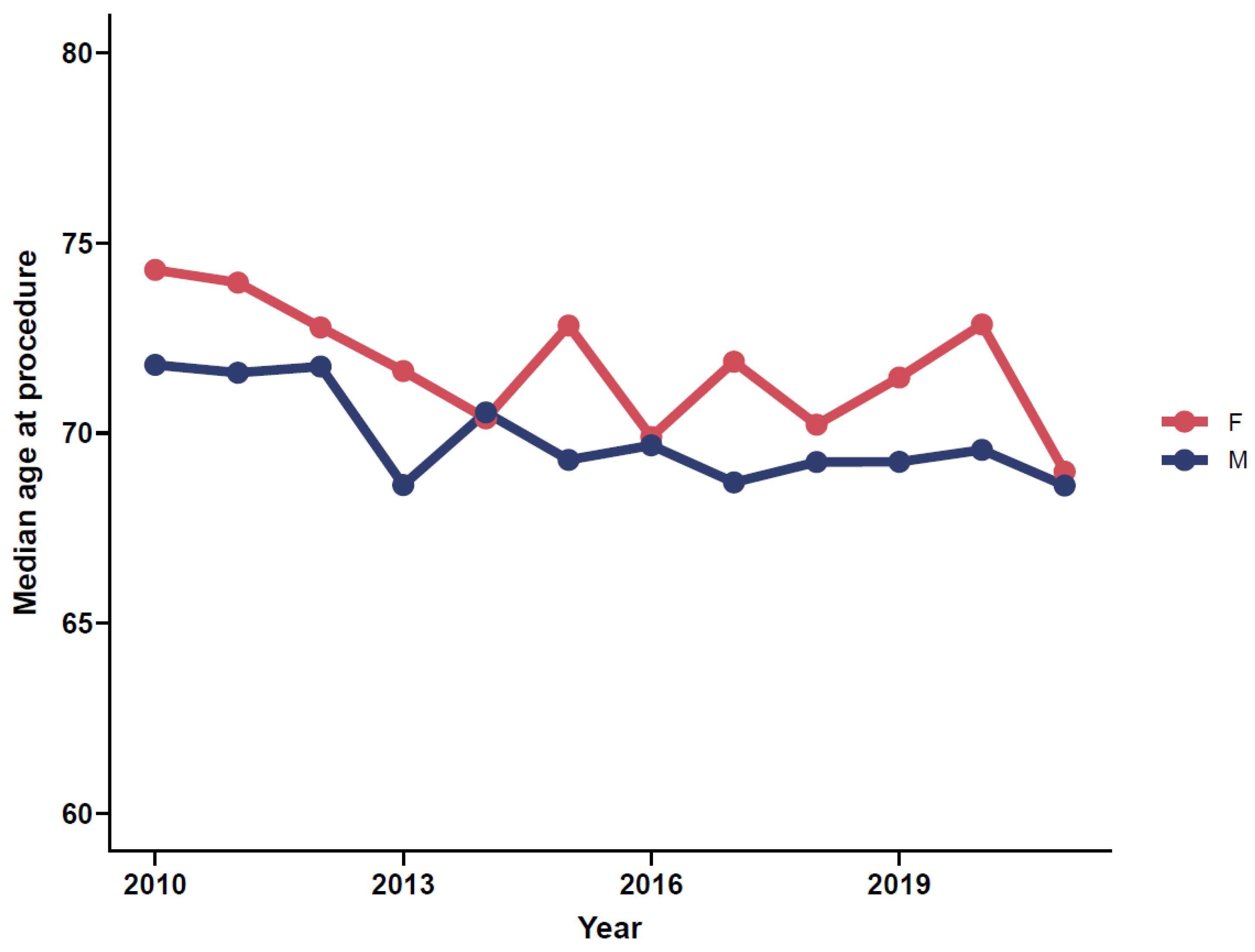
3.3. Impact of Age
3.4. Outcomes
3.4.1. Major Limb Amputation
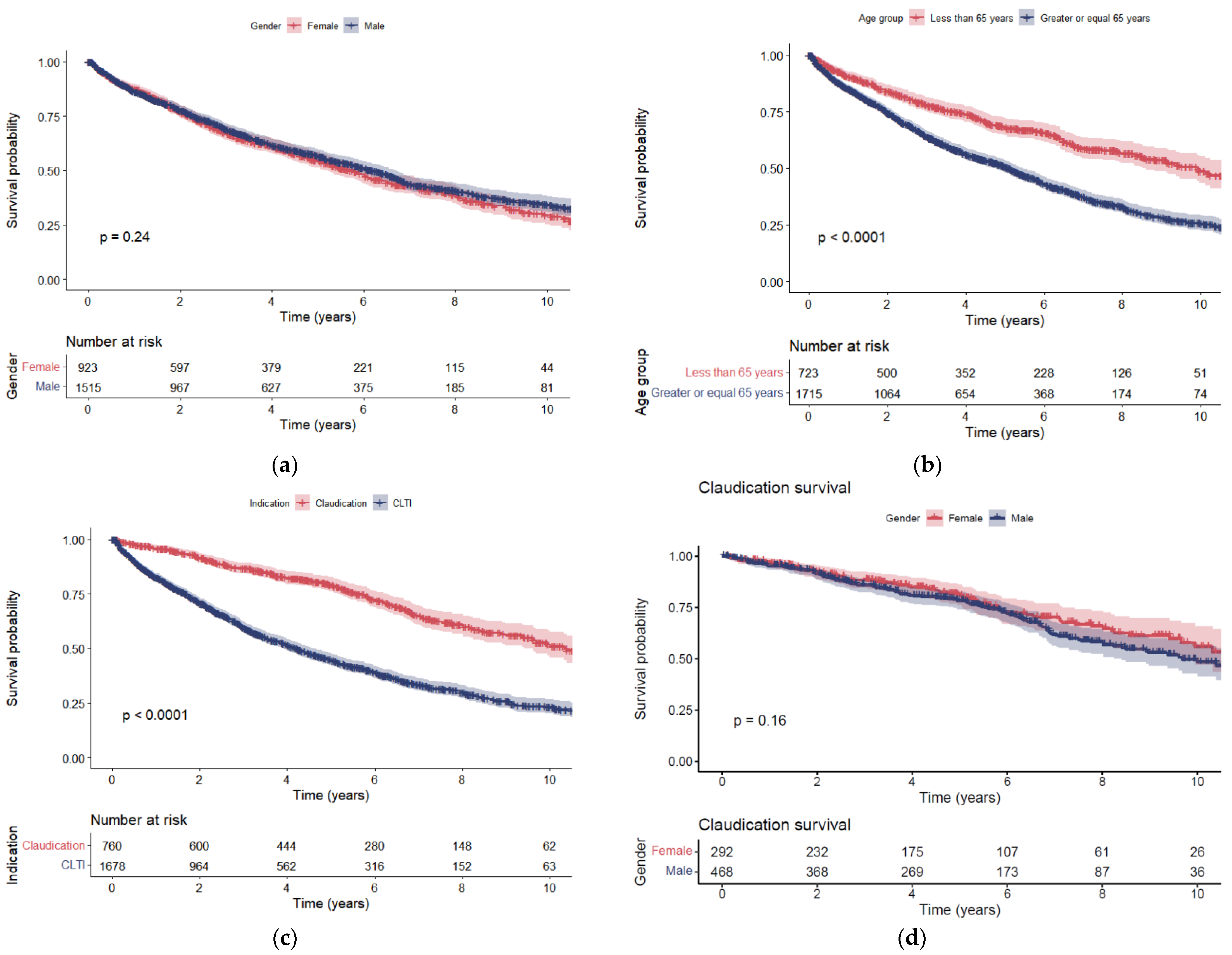
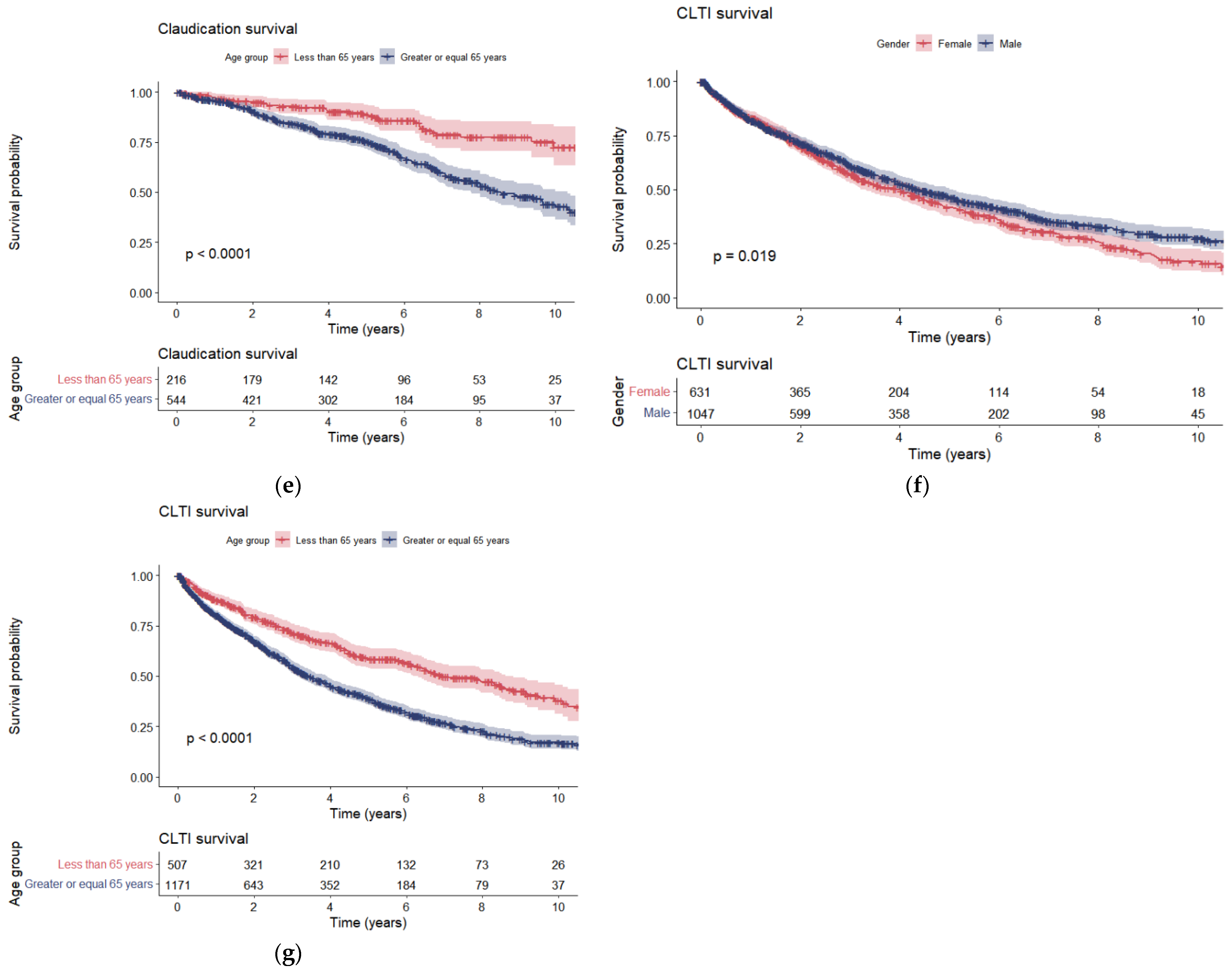
3.4.2. Survival
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Song, P.; Rudan, D.; Zhu, Y.; Fowkes, F.J.I.; Rahimi, K.; Fowkes, F.G.R.; Rudan, I. Global, regional, and national prevalence and risk factors for peripheral artery disease in 2015: An updated systematic review and analysis. Lancet Glob. Health 2019, 7, e1020–e1030. [Google Scholar] [CrossRef] [Green Version]
- Fowkes, F.G.; Rudan, D.; Rudan, I.; Aboyans, V.; Denenberg, J.O.; McDermott, M.M.; Norman, P.E.; Sampson, U.K.; Williams, L.J.; Mensah, G.A.; et al. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: A systematic review and analysis. Lancet 2013, 382, 1329–1340. [Google Scholar] [CrossRef]
- Smith, G.D.; Shipley, M.J.; Rose, G. Intermittent claudication, heart disease risk factors, and mortality. The Whitehall Study. Circulation 1990, 82, 1925–1931. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pande, R.L.; Perlstein, T.S.; Beckman, J.A.; Creager, M.A. Secondary prevention and mortality in peripheral artery disease: National Health and Nutrition Examination Study, 1999 to 2004. Circulation 2011, 124, 17–23. [Google Scholar] [CrossRef] [Green Version]
- Ankle Brachial Index, C.; Fowkes, F.G.; Murray, G.D.; Butcher, I.; Heald, C.L.; Lee, R.J.; Chambless, L.E.; Folsom, A.R.; Hirsch, A.T.; Dramaix, M.; et al. Ankle brachial index combined with Framingham Risk Score to predict cardiovascular events and mortality: A meta-analysis. JAMA 2008, 300, 197–208. [Google Scholar] [CrossRef] [Green Version]
- van Haelst, S.T.W.; Koopman, C.; den Ruijter, H.M.; Moll, F.L.; Visseren, F.L.; Vaartjes, I.; de Borst, G.J. Cardiovascular and all-cause mortality in patients with intermittent claudication and critical limb ischaemia. Br. J. Surg. 2018, 105, 252–261. [Google Scholar] [CrossRef]
- Criqui, M.H.; Aboyans, V. Epidemiology of peripheral artery disease. Circ. Res. 2015, 116, 1509–1526. [Google Scholar] [CrossRef] [Green Version]
- Parvar, S.L.; Thiyagarajah, A.; Nerlekar, N.; King, P.; Nicholls, S.J. A systematic review and meta-analysis of gender differences in long-term mortality and cardiovascular events in peripheral artery disease. J. Vasc. Surg. 2021, 73, 1456–1465.e7. [Google Scholar] [CrossRef]
- Conte, M.S.; Bradbury, A.W.; Kolh, P.; White, J.V.; Dick, F.; Fitridge, R.; Mills, J.L.; Ricco, J.B.; Suresh, K.R.; Murad, M.H.; et al. Global vascular guidelines on the management of chronic limb-threatening ischemia. J. Vasc. Surg. 2019, 69, 3S–125S.e40. [Google Scholar] [CrossRef] [Green Version]
- Norgren, L.; Hiatt, W.R.; Dormandy, J.A.; Nehler, M.R.; Harris, K.A.; Fowkes, F.G.; Group, T.I.W.; Bell, K.; Caporusso, J.; Durand-Zaleski, I.; et al. Inter-society consensus for the management of peripheral arterial disease (TASC II). Eur. J. Vasc. Endovasc. Surg. 2007, 33 (Suppl. S1), S1–S75. [Google Scholar] [CrossRef] [Green Version]
- Nehler, M.R.; Duval, S.; Diao, L.; Annex, B.H.; Hiatt, W.R.; Rogers, K.; Zakharyan, A.; Hirsch, A.T. Epidemiology of peripheral arterial disease and critical limb ischemia in an insured national population. J. Vasc. Surg. 2014, 60, 686–695.e2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Messiha, D.; Petrikhovich, O.; Lortz, J.; Mahabadi, A.A.; Hering, R.; Schulz, M.; Rassaf, T.; Rammos, C. Gender differences in outpatient peripheral artery disease management in Germany: A population based study 2009–2018. Eur. J. Vasc. Endovasc. Surg. 2022, 63, 714–720. [Google Scholar] [CrossRef] [PubMed]
- Woelk, V.; Speck, P.; Kaambwa, B.; Fitridge, R.A.; Ranasinghe, I. Incidence and causes of early unplanned readmission after hospitalisation with peripheral arterial disease in Australia and New Zealand. Med. J. Aust. 2022, 216, 80–86. [Google Scholar] [CrossRef] [PubMed]
- Ward, M.M. Estimating disease prevalence and incidence using administrative data: Some assembly required. J. Rheumatol. 2013, 40, 1241–1243. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Behrendt, C.A. Higher long-term mortality after endovascular vs. open-surgical revascularization of peripheral artery disease in Australia and New Zealand? Eur. Heart J. 2021, 43, 41–43. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ 2007, 335, 806–808. [Google Scholar] [CrossRef] [Green Version]
- Statistics New Zealand. Population Statistics; Statistics New Zealand Tatauranga Aotearoa: Wellington, New Zealand, 2019. Available online: www.stats.govt.nz (accessed on 24 March 2022).
- Midland DHBs. Regional Services Plan, Strategic Direction 2019–2022; HealthShare Ltd.: Midland, New Zealand, 2019. [Google Scholar]
- Teodorescu, V.J.; Vavra, A.K.; Kibbe, M.R. Peripheral arterial disease in women. J. Vasc. Surg. 2013, 57 (Suppl. S4), 18S–26S. [Google Scholar] [CrossRef] [Green Version]
- New Zealand Guidelines Group. Evidence-Based Best Practice Guideline: The Assessment and Management of Cardiovascular Risk; New Zealand Guidelines Group: Wellington, New Zealand, 2003.
- Ingolfsson, I.O.; Sigurdsson, G.; Sigvaldason, H.; Thorgeirsson, G.; Sigfusson, N. A marked decline in the prevalence and incidence of intermittent claudication in Icelandic men 1968-1986: A strong relationship to smoking and serum cholesterol-the Reykjavik Study. J. Clin. Epidemiol. 1994, 47, 1237–1243. [Google Scholar] [CrossRef]
- Bowlin, S.J.; Medalie, J.H.; Flocke, S.A.; Zyzanski, S.J.; Goldbourt, U. Epidemiology of intermittent claudication in middle-aged men. Am. J. Epidemiol. 1994, 140, 418–430. [Google Scholar] [CrossRef]
- Kannel, W.B.; McGee, D.L. Update on some epidemiologic features of intermittent claudication: The Framingham Study. J. Am. Geriatr. Soc. 1985, 33, 13–18. [Google Scholar] [CrossRef]
- Murabito, J.M.; Evans, J.C.; D’Agostino, R.B., Sr.; Wilson, P.W.; Kannel, W.B. Temporal trends in the incidence of intermittent claudication from 1950 to 1999. Am. J. Epidemiol. 2005, 162, 430–437. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cea-Soriano, L.; Fowkes, F.G.R.; Johansson, S.; Allum, A.M.; Garcia Rodriguez, L.A. Time trends in peripheral artery disease incidence, prevalence and secondary preventive therapy: A cohort study in The Health Improvement Network in the UK. BMJ Open 2018, 8, e018184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sundaram, V.; Bloom, C.; Zakeri, R.; Halcox, J.; Cohen, A.; Bowrin, K.; Briere, J.B.; Banerjee, A.; Simon, D.I.; Cleland, J.G.F.; et al. Temporal trends in the incidence, treatment patterns, and outcomes of coronary artery disease and peripheral artery disease in the UK, 2006-2015. Eur. Heart J. 2020, 41, 1636–1649. [Google Scholar] [CrossRef] [PubMed]
- Criqui, M.H.; Matsushita, K.; Aboyans, V.; Hess, C.N.; Hicks, C.W.; Kwan, T.W.; McDermott, M.M.; Misra, S.; Ujueta, F.; American Heart Association Council on Epidemiology and Prevention; et al. Lower extremity peripheral artery disease: Contemporary epidemiology, management gaps, and future directions: A scientific statement from the American Heart Association. Circulation 2021, 144, e171–e191. [Google Scholar] [CrossRef]
- Olinic, D.M.; Spinu, M.; Olinic, M.; Homorodean, C.; Tataru, D.A.; Liew, A.; Schernthaner, G.H.; Stanek, A.; Fowkes, G.; Catalano, M. Epidemiology of peripheral artery disease in Europe: VAS Educational Paper. Int. Angiol. 2018, 37, 327–334. [Google Scholar] [CrossRef]
- Porras, C.P.; Bots, M.L.; Teraa, M.; van Doorn, S.; Vernooij, R.W.M. Differences in symptom presentation in women and men with confirmed lower limb peripheral artery disease: A systematic review and meta-analysis. Eur. J. Vasc. Endovasc. Surg. 2022, 63, 602–612. [Google Scholar] [CrossRef]
- Eid, M.A.; Mehta, K.; Barnes, J.A.; Wanken, Z.; Columbo, J.A.; Goodney, P.; Mayo-Smith, M. PC102: Global burden of disease of peripheral artery disease. J. Vasc. Surg. 2021, 74, e255. [Google Scholar] [CrossRef]
- Cambou, J.P.; Aboyans, V.; Constans, J.; Lacroix, P.; Dentans, C.; Bura, A. Characteristics and outcome of patients hospitalised for lower extremity peripheral artery disease in France: The COPART Registry. Eur. J. Vasc. Endovasc. Surg. 2010, 39, 577–585. [Google Scholar] [CrossRef]
- Aboyans, V.; Ricco, J.B.; Bartelink, M.E.L.; Bjorck, M.; Brodmann, M.; Cohnert, T.; Collet, J.P.; Czerny, M.; De Carlo, M.; Debus, S.; et al. 2017 ESC guidelines on the diagnosis and treatment of peripheral arterial diseases, in collaboration with the European Society for Vascular Surgery (ESVS): Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteries. Endorsed by: The European Stroke Organization (ESO)The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). Eur. Heart J. 2018, 39, 763–816. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Health. Older Peoples Health Data and Stats, Our Changing Population; New Zealand Government: Wellington, New Zealand, 2016. Available online: https://www.health.govt.nz/nz-health-statistics/health-statistics-and-data-sets/older-peoples-health-data-and-stats/our-changing-population (accessed on 18 May 2022).
- Behrendt, C.A.; Sigvant, B.; Szeberin, Z.; Beiles, B.; Eldrup, N.; Thomson, I.A.; Venermo, M.; Altreuther, M.; Menyhei, G.; Nordanstig, J.; et al. International variations in amputation practice: A VASCUNET report. Eur. J. Vasc. Endovasc. Surg. 2018, 56, 391–399. [Google Scholar] [CrossRef] [Green Version]
- Aitken, S.J.; Randall, D.A.; Noguchi, N.; Blyth, F.M.; Naganathan, V. Multiple peri-operative complications are associated with reduced long term amputation free survival following revascularisation for lower limb peripheral artery disease: A population based linked data study. Eur. J. Vasc. Endovasc. Surg. 2020, 59, 437–445. [Google Scholar] [CrossRef] [PubMed]
- Hart, O.; Jansen, S.; Fitridge, R.; Khashram, M. Protocol for a prospective observational study: The Australia and New Zealand Diabetic and Ischaemic Foot Outcomes Study (ANZ-DIFOS). BMJ Open 2021, 11, e050833. [Google Scholar] [CrossRef] [PubMed]
| Short-Distance IC | CLTI | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | Female | Male | Overall | p Value | Female | Male | Overall | p Value | |
| N (%) | 295 (38.4) | 473 (61.6) | 768 | 666 (37.6) | 1107 (62.4) | 1773 | |||
| Age, median (IQR) | 73 (64–79) | 70 (62–77) | 71 (63–77) | 0.024 | 74 (62–83) | 71 (63–79) | 72 (62–81) | <0.001 | |
| DM (%) | DM | 66 (22.4) | 114 (24.1) | 180 (23.4) | 0.234 | 313 (47.0) | 610 (55.1) | 923 (52.1) | 0.002 |
| Pre-DM | 33 (11.2) | 36 (7.6) | 69 (9.0) | 29 (4.4) | 53 (4.8) | 82 (4.6) | |||
| ESRF (%) | 6 (2.0) | 7 (1.5) | 13 (1.7) | 0.771 | 75 (11.3) | 134 (12.1) | 209 (11.8) | 0.647 | |
| COPD (%) | 52 (17.6) | 54 (11.4) | 106 (13.8) | 0.02 | 105 (15.8) | 145 (13.1) | 250 (14.1) | 0.136 | |
| IHD (%) | 99 (33.6) | 183 (38.7) | 282 (36.7) | 0.175 | 212 (31.8) | 416 (37.6) | 628 (35.4) | 0.016 | |
| CHF (%) | 21 (7.1) | 30 (6.3) | 51 (6.6) | 0.786 | 122 (18.3) | 211 (19.1) | 333 (18.8) | 0.745 | |
| Cancer (%) | 45 (15.3) | 68 (14.4) | 113 (14.7) | 0.819 | 113 (17.0) | 168 (15.2) | 281 (15.8) | 0.351 | |
| Cognitive Impairment (%) | Dementia | 1 (0.3) | 3 (0.6) | 4 (0.5) | 0.736 | 626 (94.0) | 1050 (94.9) | 1676 (94.5) | 0.403 |
| MCI | 3 (1.0) | 7 (1.5) | 10 (1.3) | 32 (4.8) | 40 (3.6) | 72 (4.1) | |||
| None | 291 (98.6) | 463 (97.9) | 754 (98.2) | 626 (94.0) | 1050 (94.9) | 1676 (94.5) | |||
| Short-Distance IC | CLTI | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Midland | Female 2 | Male 2 | Overall | Female 2 | Male 2 | Overall | |||||||
| Year | Pop 1 | N | Incidence | N | Incidence | N | Incidence | N | Incidence | N | Incidence | N | Incidence |
| 2010 | 363,372.5 | 20 | 10.5 (5.9–15.1) | 33 | 19.1 (12.6–25.7) | 53 | 14.6 (10.7–18.5) | 76 | 39.8 (30.9–48.8) | 98 | 56.8 (45.6–68.1) | 174 | 47.9 (40.8–55) |
| 2011 | 370,230 | 35 | 18 (12–23.9) | 44 | 25.1 (17.7–32.5) | 79 | 21.3 (16.6–26) | 60 | 30.8 (23–38.6) | 94 | 53.6 (42.7–64.4) | 154 | 41.6 (35–48.2) |
| 2012 | 376,277.5 | 30 | 15.1 (9.7–20.6) | 47 | 26.4 (18.8–33.9) | 77 | 20.5 (15.9–25) | 51 | 25.8 (18.7–32.8) | 93 | 52.2 (41.6–62.8) | 144 | 38.3 (32–44.5) |
| 2013 | 383,995 | 22 | 10.9 (6.3–15.4) | 37 | 20.3 (13.8–26.9) | 59 | 15.4 (11.4–19.3) | 54 | 26.7 (19.6–33.9) | 83 | 45.6 (35.8–55.4) | 137 | 35.7 (29.7–41.7) |
| 2014 | 393,667.5 | 27 | 13 (8.1–18) | 49 | 26.2 (18.9–33.6) | 76 | 19.3 (15–23.6) | 61 | 29.5 (22.1–36.9) | 89 | 47.7 (37.8–57.6) | 150 | 38.1 (32–44.2) |
| 2015 | 403,932.5 | 23 | 10.8 (6.4–15.3) | 39 | 20.3 (13.9–26.7) | 62 | 15.3 (11.5–19.2) | 47 | 22.2 (15.8–28.5) | 100 | 52.1 (41.9–62.3) | 147 | 36.4 (30.5–42.3) |
| 2016 | 415,117.5 | 28 | 12.9 (8.1–17.6) | 51 | 25.8 (18.7–32.9) | 79 | 19 (14.8–23.2) | 50 | 23 (16.6–29.4) | 92 | 46.6 (37.1–56.1) | 142 | 34.2 (28.6–39.8) |
| 2017 | 426,322.5 | 27 | 12.1 (7.5–16.7) | 44 | 21.6 (15.2–28) | 71 | 16.7 (12.8–20.5) | 46 | 20.6 (14.7–26.6) | 77 | 37.9 (29.4–46.3) | 123 | 28.9 (23.8–34) |
| 2018 | 437,605 | 31 | 13.6 (8.8–18.3) | 28 | 13.4 (8.4–18.4) | 59 | 13.5 (10–16.9) | 64 | 28 (21.1–34.8) | 85 | 40.7 (32–49.3) | 149 | 34 (28.6–39.5) |
| 2019 | 450,645 | 13 | 5.5 (2.5–8.5) | 39 | 18.1 (12.4–23.8) | 52 | 11.5 (8.4–14.7) | 52 | 22.1 (16.1–28.1) | 80 | 37.2 (29–45.3) | 132 | 29.3 (24.3–34.3) |
| 2020 | 461,960 | 18 | 7.5 (4–10.9) | 28 | 12.7 (8–17.4) | 46 | 10 (7.1–12.8) | 59 | 24.5 (18.2–30.7) | 92 | 41.7 (33.2–50.2) | 151 | 32.7 (27.5–37.9) |
| 2021 | 450,645 | 21 | 8.6 (4.9–12.2) | 34 | 15.2 (10.1–20.2) | 55 | 12.2 (9–15.4) | 46 | 18.7 (13.3–24.1) | 124 | 55.3 (45.5–65) | 170 | 37.7 (32.1–43.4) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hart, O.; Xue, N.; Davis-Havill, B.; Pottier, M.; Prakash, M.; Reimann, S.-A.; King, J.; Xu, W.; Khashram, M. The Incidence of Chronic Limb-Threatening Ischemia in the Midland Region of New Zealand over a 12-Year Period. J. Clin. Med. 2022, 11, 3303. https://doi.org/10.3390/jcm11123303
Hart O, Xue N, Davis-Havill B, Pottier M, Prakash M, Reimann S-A, King J, Xu W, Khashram M. The Incidence of Chronic Limb-Threatening Ischemia in the Midland Region of New Zealand over a 12-Year Period. Journal of Clinical Medicine. 2022; 11(12):3303. https://doi.org/10.3390/jcm11123303
Chicago/Turabian StyleHart, Odette, Nicole Xue, Brittany Davis-Havill, Mark Pottier, Minesh Prakash, Sascha-Akito Reimann, Jasmin King, William Xu, and Manar Khashram. 2022. "The Incidence of Chronic Limb-Threatening Ischemia in the Midland Region of New Zealand over a 12-Year Period" Journal of Clinical Medicine 11, no. 12: 3303. https://doi.org/10.3390/jcm11123303
APA StyleHart, O., Xue, N., Davis-Havill, B., Pottier, M., Prakash, M., Reimann, S.-A., King, J., Xu, W., & Khashram, M. (2022). The Incidence of Chronic Limb-Threatening Ischemia in the Midland Region of New Zealand over a 12-Year Period. Journal of Clinical Medicine, 11(12), 3303. https://doi.org/10.3390/jcm11123303






