Accuracy of Dynamic Navigation for Non-Surgical Endodontic Treatment: A Systematic Review
Abstract
:1. Introduction
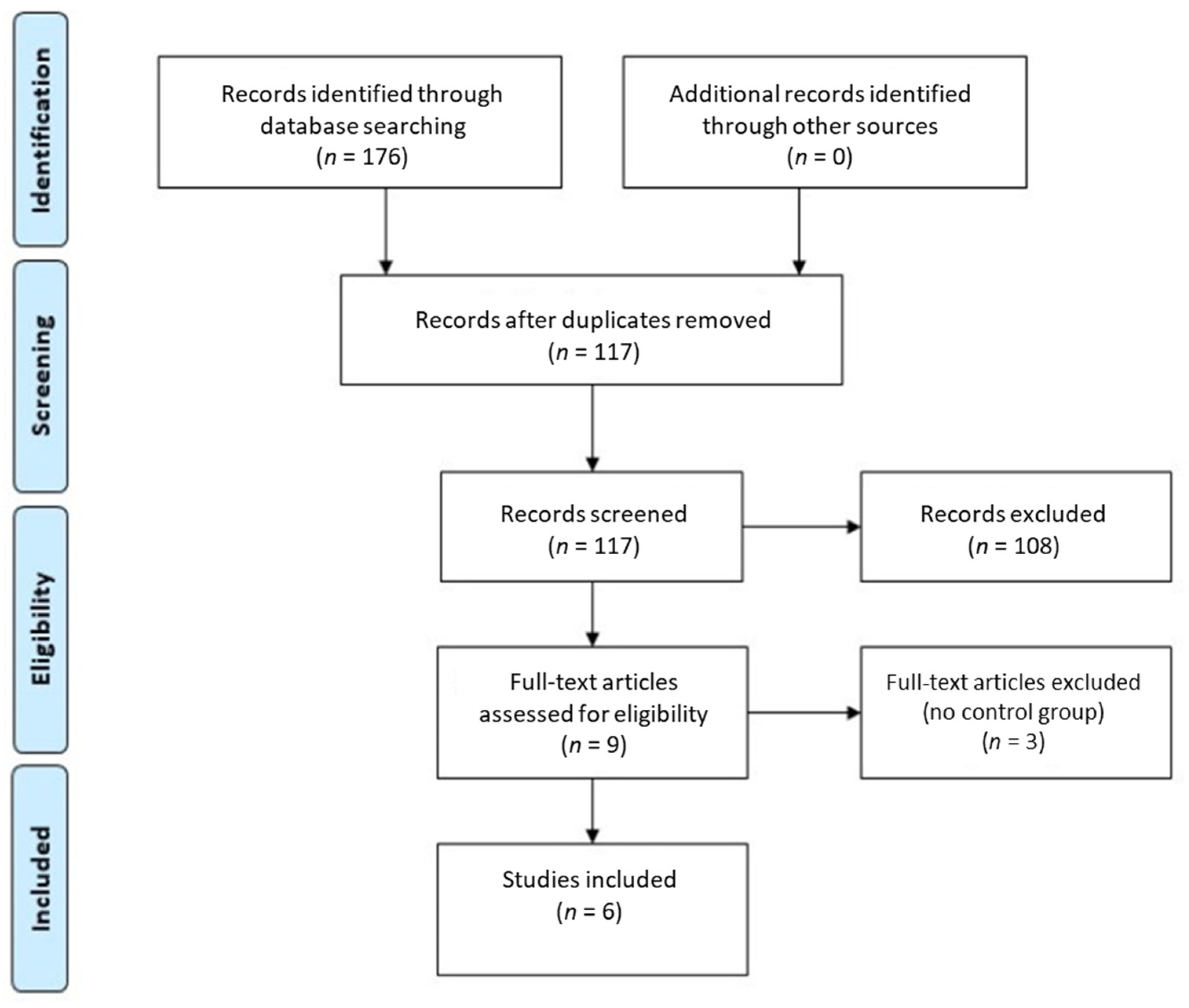
2. Materials and Methods
2.1. Study Design
- Population—human teeth or three-dimensional (3D) printed teeth;
- Intervention—non-surgical endodontic treatment using the dynamic navigation system;
- Comparison—non-surgical endodontic treatment using the conventional freehand technique;
- Outcome—accuracy and efficiency of non-surgical endodontic treatment.
2.2. Search Strategy
2.3. Study Selection
- Randomized experimental trials (RETs) or clinical trials (RCTs);
- Non-surgical endodontic treatment using a dynamic navigation system;
- Outcomes compared to conventional freehand technique;
- Articles available in full text.
2.4. Data Extraction
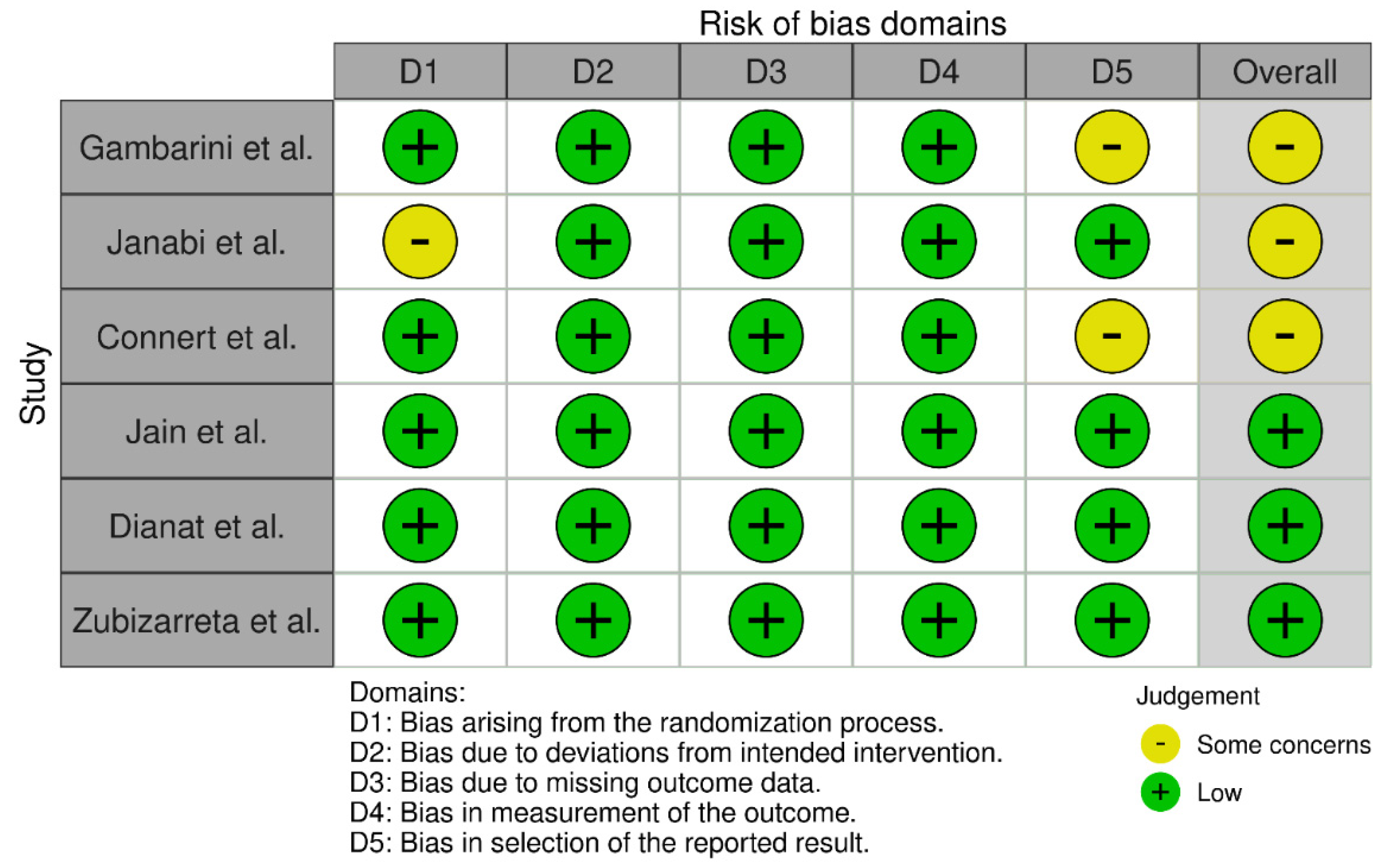
2.5. Quality Assessment
3. Results
3.1. Study Selection
3.2. Study Characteristics
3.3. Quality Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Krasner, P.; Rankow, H.J. Anatomy of the pulp-chamber floor. J. Endod. 2004, 30, 5–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Iandolo, A.; Iandolo, G.; Malvano, M.; Pantaleo, G.; Simeone, M. Modern technologies in Endodontics. G. Ital. Endod. 2016, 30, 2–9. [Google Scholar] [CrossRef] [Green Version]
- Kiefner, P.; Connert, T.; ElAyouti, A.; Weiger, R. Treatment of calcified root canals in elderly people: A clinical study about the accessibility, the time needed and the outcome with a three-year follow-up. Gerodontology 2017, 34, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Karabucak, B.; Bunes, A.; Chehoud, C.; Kohli, M.R.; Setzer, F. Prevalence of Apical Periodontitis in Endodontically Treated Premolars and Molars with Untreated Canal: A Cone-beam Computed Tomography Study. J. Endod. 2016, 42, 538–541. [Google Scholar] [CrossRef] [PubMed]
- Touré, B.; Faye, B.; Kane, A.W.; Lo, C.M.; Niang, B.; Boucher, Y. Analysis of Reasons for Extraction of Endodontically Treated Teeth: A Prospective Study. J. Endod. 2011, 37, 1512–1515. [Google Scholar] [CrossRef]
- Song, M. Dental care for patients taking antiresorptive drugs: A literature review. Restor. Dent. Endod. 2019, 44, e42. [Google Scholar] [CrossRef] [Green Version]
- Zehnder, M.S.; Connert, T.; Weiger, R.; Krastl, G.; Kühl, S. Guided endodontics: Accuracy of a novel method for guided access cavity preparation and root canal location. Int. Endod. J. 2016, 49, 966–972. [Google Scholar] [CrossRef]
- Connert, T.; Weiger, R.; Krastl, G. Present status and future directions—Guided endodontics. Int. Endod. J. 2022; accepted for publication. [Google Scholar] [CrossRef]
- Panchal, N.; Mahmood, L.; Retana, A.; Emery, R. Dynamic Navigation for Dental Implant Surgery. Oral Maxillofac. Surg. Clin. 2019, 31, 539–547. [Google Scholar] [CrossRef]
- Chong, B.S.; Dhesi, M.; Makdissi, J. Computer-aided dynamic navigation: A novel method for guided endodontics. Quintessence Int. 2019, 50, 196–202. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef] [PubMed]
- Janabi, A.; Tordik, P.A.; Griffin, I.L.; Mostoufi, B.; Price, J.B.; Chand, P.; Martinho, F.C. Accuracy and Efficiency of 3-dimensional Dynamic Navigation System for Removal of Fiber Post from Root Canal-Treated Teeth. J. Endod. 2021, 47, 1453–1460. [Google Scholar] [CrossRef] [PubMed]
- Dianat, O.; Nosrat, A.; Tordik, P.A.; Aldahmash, S.A.; Romberg, E.; Price, J.B.; Mostoufi, B. Accuracy and Efficiency of a Dynamic Navigation System for Locating Calcified Canals. J. Endod. 2020, 46, 1719–1725. [Google Scholar] [CrossRef] [PubMed]
- Zubizarreta-Macho, Á.; Muñoz, A.P.; Deglow, E.R.; Agustín-Panadero, R.; Álvarez, J.M. Accuracy of Computer-Aided Dynamic Navigation Compared to Computer-Aided Static Procedure for Endodontic Access Cavities: An In Vitro Study. J. Clin. Med. 2020, 9, 129. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gambarini, G.; Galli, M.; Morese, A.; Stefanelli, L.V.; Abduljabbar, F.; Giovarruscio, M.; Di Nardo, D.; Seracchiani, M.; Testarelli, L. Precision of Dynamic Navigation to Perform Endodontic Ultraconservative Access Cavities: A Preliminary In Vitro Analysis. J. Endod. 2020, 46, 1286–1290. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.D.; Saunders, M.W.; Carrico, C.K.; Jadhav, A.; Deeb, J.G.; Myers, G.L. Dynamically Navigated versus Freehand Access Cavity Preparation: A Comparative Study on Substance Loss Using Simulated Calcified Canals. J. Endod. 2020, 46, 1745–1751. [Google Scholar] [CrossRef] [PubMed]
- Connert, T.; Leontiev, W.; Dagassan-Berndt, D.; Kühl, S.; ElAyouti, A.; Krug, R.; Krastl, G.; Weiger, R. Real-Time Guided Endodontics with a Miniaturized Dynamic Navigation System Versus Conventional Freehand Endodontic Access Cavity Preparation: Substance Loss and Procedure Time. J. Endod. 2021, 47, 1651–1656. [Google Scholar] [CrossRef]
- Schwartz, R.S.; Robbins, J.W. Post placement and restoration of endodontically treated teeth: A literature review. J. Endod. 2004, 30, 289–301. [Google Scholar] [CrossRef]
- Jain, S.D.; Carrico, C.K.; Bermanis, I.; Rehil, S. Intraosseous Anesthesia Using Dynamic Navigation Technology. J. Endod. 2020, 46, 1894–1900. [Google Scholar] [CrossRef]
- Torres, A.; Boelen, G.J.; Lambrechts, P.; Pedano, M.S.; Jacobs, R. Dynamic navigation: A laboratory study on the accuracy and potential use of guided root canal treatment. Int. Endod. J. 2021, 54, 1659–1667. [Google Scholar] [CrossRef]
- de Toubes, K.M.P.S.; de Oliveira, P.A.D.; Machado, S.N.; Pelosi, V.; Nunes, E.; Silveira, F.F. Clinical approach to pulp canal obliteration: A case series. Iran Endod. J. 2017, 12, 527–533. [Google Scholar] [PubMed]
- Carvalho, T.S.; Lussi, A. Age-related morphological, histological and functional changes in teeth. J. Oral Rehabil. 2017, 44, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Dikbas, I.; Tanalp, J. An Overview of Clinical Studies on Fiber Post Systems. Sci. World J. 2013, 2013, 171380. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garcia, P.P.; Wambier, L.M.; de Geus, J.L.; da Cunha, L.F.; Correr, G.M.; Gonzaga, C.C. Do anterior and posterior teeth treated with post-and-core restorations have similar failure rates? A systematic review and meta-analysis. J. Prosthet. Dent. 2019, 121, 887–894. [Google Scholar] [CrossRef] [PubMed]
- American Association of Endodontists. AAE Endodontic Case Difficulty Assessment Form and Guidelines. Available online: https://www.aae.org/specialty/wp-content/uploads/sites/2/2019/02/19AAE_CaseDifficultyAssessmentForm.pdf (accessed on 12 March 2022).
- Zhan, Y.; Wang, M.; Cheng, X.; Li, Y.; Shi, X.; Liu, F. Evaluation of a dynamic navigation system for training students in dental implant placement. J. Dent. Educ. 2021, 85, 120–127. [Google Scholar] [CrossRef]
- Golob Deeb, J.; Bencharit, S.; Carrico, C.K.; Lukic, M.; Hawkins, D.; Rener-Sitar, K.; Deeb, G.R. Exploring training dental implant placement using computer-guided implant navigation system for predoctoral students: A pilot study. Eur. J. Dent. Educ. 2019, 23, 415–423. [Google Scholar] [CrossRef]
- Jorba-García, A.; González-Barnadas, A.; Camps-Font, O.; Figueiredo, R.; Valmaseda-Castellón, E. Accuracy assessment of dynamic computer–aided implant placement: A systematic review and meta-analysis. Clin. Oral. Investig. 2021, 25, 2479–2494. [Google Scholar] [CrossRef]
- Gambarini, G.; Galli, M.; Stefanelli, L.V.; Di Nardo, D.; Morese, A.; Seracchiani, M.; De Angelis, F.; Di Carlo, S.; Testarelli, L. Endodontic Microsurgery Using Dynamic Navigation System: A Case Report. J. Endod. 2019, 45, 1397–1402. [Google Scholar] [CrossRef]
- Dianat, O.; Gupta, S.; Price, J.B.; Mostoufi, B. Guided Endodontic Access in a Maxillary Molar Using a Dynamic Navigation System. J. Endod. 2021, 47, 658–662. [Google Scholar] [CrossRef]
- Bardales-Alcocer, J.; Ramírez-Salomón, M.; Vega-Lizama, E.; López-Villanueva, M.; Alvarado-Cárdenas, G.; Serota, K.S.; Ramírez-Wong, J. Endodontic Retreatment Using Dynamic Navigation: A Case Report. J. Endod. 2021, 47, 1007–1013. [Google Scholar] [CrossRef]
- Lu, Y.J.; Chiu, L.H.; Tsai, L.Y.; Fang, C.Y. Dynamic navigation optimizes endodontic microsurgery in an anatomically challenging area. J. Dent. Sci. 2022, 17, 580–582. [Google Scholar] [CrossRef]
| Study | Sample Size | DN System | Specimens | Outcome Measure | DN Technique Results ± SD (95% CI) | FH Technique Results ± SD (95% CI) |
|---|---|---|---|---|---|---|
| Gambarini et al., 2020 (Italy) [15] | 20 (n = 10) | Navident (ClaroNav) | Artificial, made of resin upper right first molars. |
|
|
|
| Janabi et al., 2021 (USA) [12] | 26 (n = 13) | X-guide system (X-Nav Technologies) | Extracted human maxillary single-rooted teeth (incisors and canines). Teeth were endodontically treated and restored with fiber post. |
|
|
|
| Connert et al., 2021 (Switzerland) [17] | 72 (n = 18) | DENACAM system (Mininavident AG) | 3D printed using resin maxillary single-rooted teeth (incisors and canines). |
|
|
|
| Jain et al., 2020 (USA) [16] | 40 (n = 20) | Navident (ClaroNav) | 3D printed single-rooted teeth with simulated pulp canal obliteration (maxillary and mandibular central incisors). |
|
|
|
| Dianat et al., 2020 (USA) [13] | 60 (n = 15) | X-Guide system (X-Nav Technologies) | Extracted human single-rooted teeth with pulp canal obliteration (maxillary and mandibular incisors, canines and premolars). |
|
|
|
| Zubizarreta et al., 2020 (Spain) [14] | 30 (n = 10) | Navident (ClaroNav) | Extracted human single-rooted teeth (lower central incisors). |
|
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jonaityte, E.M.; Bilvinaite, G.; Drukteinis, S.; Torres, A. Accuracy of Dynamic Navigation for Non-Surgical Endodontic Treatment: A Systematic Review. J. Clin. Med. 2022, 11, 3441. https://doi.org/10.3390/jcm11123441
Jonaityte EM, Bilvinaite G, Drukteinis S, Torres A. Accuracy of Dynamic Navigation for Non-Surgical Endodontic Treatment: A Systematic Review. Journal of Clinical Medicine. 2022; 11(12):3441. https://doi.org/10.3390/jcm11123441
Chicago/Turabian StyleJonaityte, Egle Marija, Goda Bilvinaite, Saulius Drukteinis, and Andres Torres. 2022. "Accuracy of Dynamic Navigation for Non-Surgical Endodontic Treatment: A Systematic Review" Journal of Clinical Medicine 11, no. 12: 3441. https://doi.org/10.3390/jcm11123441
APA StyleJonaityte, E. M., Bilvinaite, G., Drukteinis, S., & Torres, A. (2022). Accuracy of Dynamic Navigation for Non-Surgical Endodontic Treatment: A Systematic Review. Journal of Clinical Medicine, 11(12), 3441. https://doi.org/10.3390/jcm11123441







