Is Prehospital Assessment of qSOFA Parameters Associated with Earlier Targeted Sepsis Therapy? A Retrospective Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Acquisition
2.2. Study Endpoints
2.3. Covariables
- Age (years).
- Gender (male/female).
- EMS without emergency physician (only paramedics) versus EMS with emergency physician (of note, this variable is specific to the German emergency system, which provides these two modular care levels).
2.4. Sample Size
2.5. Descriptive Statistics
2.6. Multiple Linear Regression Models
3. Results
3.1. Data Acquisition and Cohort Characteristics
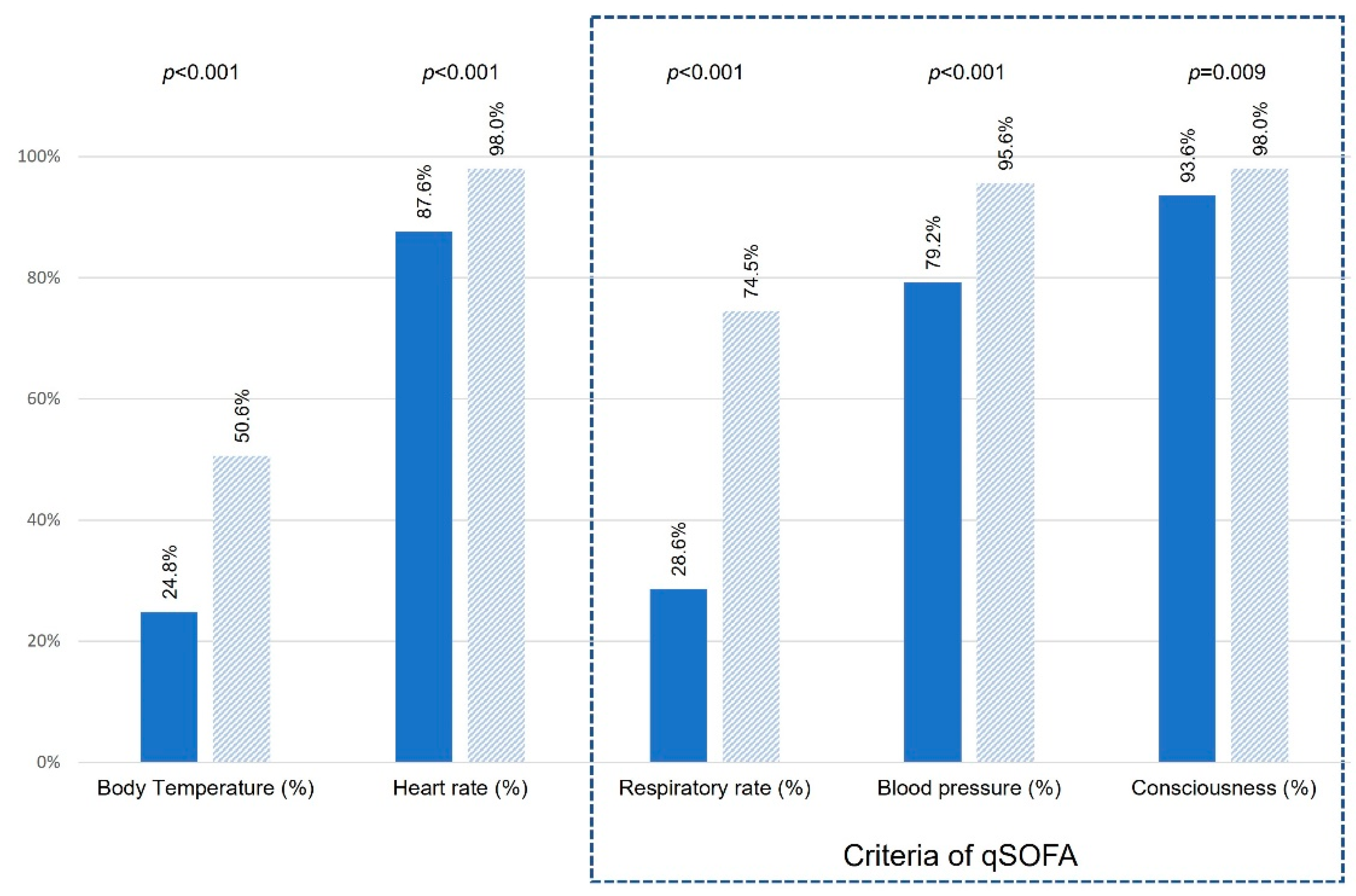
3.2. Assessment of Sepsis Indicators
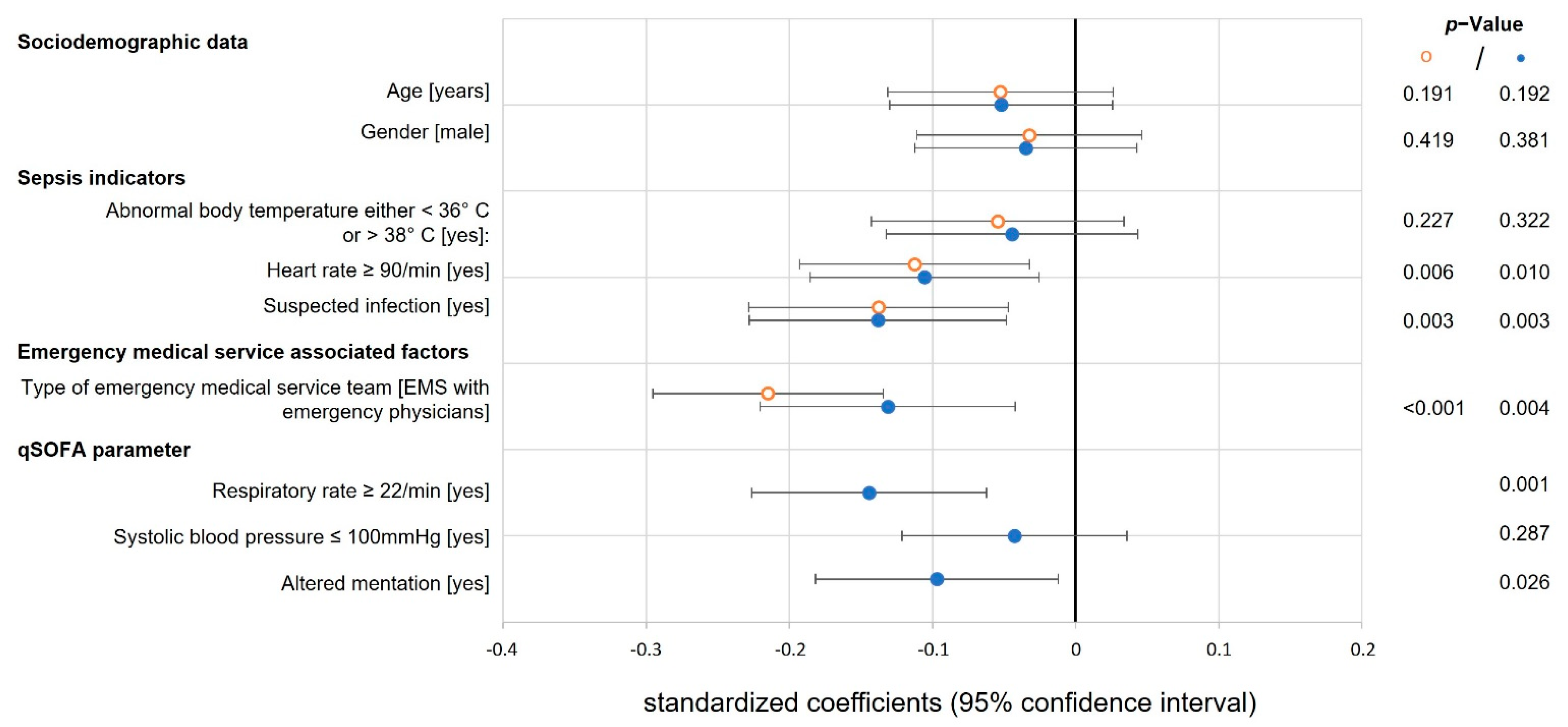
3.3. Multiple Linear Regression Models
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Seymour, C.W.; Liu, V.X.; Iwashyna, T.J.; Brunkhorst, F.M.; Rea, T.D.; Scherag, A.; Rubenfeld, G.; Kahn, J.M.; Shankar-Hari, M.; Singer, M.; et al. Assessment of Clinical Criteria for Sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 762–774. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Song, J.U.; Sin, C.K.; Park, H.K.; Shim, S.R.; Lee, J. Performance of the quick Sequential (sepsis-related) Organ Failure Assessment score as a prognostic tool in infected patients outside the intensive care unit: A systematic review and meta-analysis. Crit. Care 2018, 22, 28. [Google Scholar] [CrossRef] [Green Version]
- Evans, L.; Rhodes, A.; Alhazzani, W.; Antonelli, M.; Coopersmith, C.M.; French, C.; Machado, F.R.; McIntyre, L.; Ostermann, M.; Prescott, H.C.; et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock 2021. Crit. Care Med. 2021, 49, e1063–e1143. [Google Scholar] [CrossRef] [PubMed]
- Angus, D.C.; Linde-Zwirble, W.T.; Lidicker, J.; Clermont, G.; Carcillo, J.; Pinsky, M.R. Epidemiology of severe sepsis in the United States: Analysis of incidence, outcome, and associated costs of care. Crit. Care Med. 2001, 29, 1303–1310. [Google Scholar] [CrossRef]
- Rhodes, A.; Evans, L.E.; Alhazzani, W.; Levy, M.M.; Antonelli, M.; Ferrer, R.; Kumar, A.; Sevransky, J.E.; Sprung, C.L.; Nunnally, M.E.; et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Crit. Care Med. 2017, 45, 486–552. [Google Scholar] [CrossRef] [PubMed]
- Rivers, E.; Nguyen, B.; Havstad, S.; Ressler, J.; Muzzin, A.; Knoblich, B.; Peterson, E.; Tomlanovich, M.; Early Goal-Directed Therapy Collaborative, G. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N. Engl. J. Med. 2001, 345, 1368–1377. [Google Scholar] [CrossRef] [Green Version]
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef]
- Levy, M.M.; Evans, L.E.; Rhodes, A. The Surviving Sepsis Campaign Bundle: 2018 Update. Crit. Care Med. 2018, 46, 997–1000. [Google Scholar] [CrossRef]
- Im, Y.; Kang, D.; Ko, R.E.; Lee, Y.J.; Lim, S.Y.; Park, S.; Na, S.J.; Chung, C.R.; Park, M.H.; Oh, D.K.; et al. Time-to-antibiotics and clinical outcomes in patients with sepsis and septic shock: A prospective nationwide multicenter cohort study. Crit. Care 2022, 26, 19. [Google Scholar] [CrossRef]
- Yealy, D.M.; Mohr, N.M.; Shapiro, N.I.; Venkatesh, A.; Jones, A.E.; Self, W.H. Early Care of Adults with Suspected Sepsis in the Emergency Department and Out-of-Hospital Environment: A Consensus-Based Task Force Report. Ann. Emerg. Med. 2021, 78, 1–19. [Google Scholar] [CrossRef]
- Levy, M.M.; Fink, M.P.; Marshall, J.C.; Abraham, E.; Angus, D.; Cook, D.; Cohen, J.; Opal, S.M.; Vincent, J.L.; Ramsay, G.; et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit. Care Med. 2003, 31, 1250–1256. [Google Scholar] [CrossRef]
- Koyama, S.; Yamaguchi, Y.; Gibo, K.; Nakayama, I.; Ueda, S. Use of prehospital qSOFA in predicting in-hospital mortality in patients with suspected infection: A retrospective cohort study. PLoS ONE 2019, 14, e0216560. [Google Scholar] [CrossRef] [Green Version]
- Shu, E.; Ives Tallman, C.; Frye, W.; Boyajian, J.G.; Farshidpour, L.; Young, M.; Campagne, D. Pre-hospital qSOFA as a predictor of sepsis and mortality. Am. J. Emerg. Med. 2019, 37, 1273–1278. [Google Scholar] [CrossRef]
- Fischer, M.; Kamp, J.; Garcia-Castrillo Riesgo, L.; Robertson-Steel, I.; Overton, J.; Ziemann, A.; Krafft, T.; Group, E.E.D. Comparing emergency medical service systems—A project of the European Emergency Data (EED) Project. Resuscitation 2011, 82, 285–293. [Google Scholar] [CrossRef] [Green Version]
- Tjelmeland, I.B.M.; Masterson, S.; Herlitz, J.; Wnent, J.; Bossaert, L.; Rosell-Ortiz, F.; Alm-Kruse, K.; Bein, B.; Lilja, G.; Grasner, J.T.; et al. Description of Emergency Medical Services, treatment of cardiac arrest patients and cardiac arrest registries in Europe. Scand. J. Trauma Resusc. Emerg. Med. 2020, 28, 103. [Google Scholar] [CrossRef]
- Smyth, M.A.; Brace-McDonnell, S.J.; Perkins, G.D. Identification of adults with sepsis in the prehospital environment: A systematic review. BMJ Open 2016, 6, e011218. [Google Scholar] [CrossRef] [Green Version]
- McArthur-Rouse, F. Critical care outreach services and early warning scoring systems: A review of the literature. J. Adv. Nurs. 2001, 36, 696–704. [Google Scholar] [CrossRef]
- Subbe, C.P.; Kruger, M.; Rutherford, P.; Gemmel, L. Validation of a modified Early Warning Score in medical admissions. QJM 2001, 94, 521–526. [Google Scholar] [CrossRef] [Green Version]
- Raith, E.P.; Udy, A.A.; Bailey, M.; McGloughlin, S.; MacIsaac, C.; Bellomo, R.; Pilcher, D.V. Prognostic Accuracy of the SOFA Score, SIRS Criteria, and qSOFA Score for In-Hospital Mortality among Adults with Suspected Infection Admitted to the Intensive Care Unit. JAMA 2017, 317, 290–300. [Google Scholar] [CrossRef]
- Barbara, P.; Graziano, C.; Caputo, W.; Litvak, I.; Battinelli, D.; Hahn, B. The quick sequential organ failure assessment (qSOFA) identifies septic patients in the out-of-hospital setting. Am. J. Emerg. Med. 2018, 36, 1022–1026. [Google Scholar] [CrossRef]
- Bone, R.C.; Balk, R.A.; Cerra, F.B.; Dellinger, R.P.; Fein, A.M.; Knaus, W.A.; Schein, R.M.; Sibbald, W.J. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 1992, 101, 1644–1655. [Google Scholar] [CrossRef] [Green Version]
- Riley, R.D.; Ensor, J.; Snell, K.I.E.; Harrell, F.E., Jr.; Martin, G.P.; Reitsma, J.B.; Moons, K.G.M.; Collins, G.; van Smeden, M. Calculating the sample size required for developing a clinical prediction model. BMJ 2020, 368, m441. [Google Scholar] [CrossRef] [Green Version]
- Casu, S.; Blau, J.; Schempf, B.; Häske, D. If you don’t take a temperature, you can’t find a fever. Awareness in out-of-hospital vital signs in cases of suspected sepsis. Notf. Rett. 2019, 22, 509–513. [Google Scholar] [CrossRef] [Green Version]
- Roest, A.A.; Stoffers, J.; Pijpers, E.; Jansen, J.; Stassen, P.M. Ambulance patients with nondocumented sepsis have a high mortality risk: A retrospective study. Eur. J. Emerg. Med. 2017, 24, 36–43. [Google Scholar] [CrossRef]
- Serafim, R.; Gomes, J.A.; Salluh, J.; Povoa, P. A Comparison of the Quick-SOFA and Systemic Inflammatory Response Syndrome Criteria for the Diagnosis of Sepsis and Prediction of Mortality: A Systematic Review and Meta-Analysis. Chest 2018, 153, 646–655. [Google Scholar] [CrossRef]
- Alam, N.; Oskam, E.; Stassen, P.M.; Exter, P.V.; van de Ven, P.M.; Haak, H.R.; Holleman, F.; Zanten, A.V.; Leeuwen-Nguyen, H.V.; Bon, V.; et al. Prehospital antibiotics in the ambulance for sepsis: A multicentre, open label, randomised trial. Lancet Respir. Med. 2018, 6, 40–50. [Google Scholar] [CrossRef]
- Peltan, I.D.; Brown, S.M.; Bledsoe, J.R.; Sorensen, J.; Samore, M.H.; Allen, T.L.; Hough, C.L. ED Door-to-Antibiotic Time and Long-term Mortality in Sepsis. Chest 2019, 155, 938–946. [Google Scholar] [CrossRef]
- Band, R.A.; Gaieski, D.F.; Hylton, J.H.; Shofer, F.S.; Goyal, M.; Meisel, Z.F. Arriving by emergency medical services improves time to treatment endpoints for patients with severe sepsis or septic shock. Acad. Emerg. Med. 2011, 18, 934–940. [Google Scholar] [CrossRef] [PubMed]
- Fernando, S.M.; Tran, A.; Taljaard, M.; Cheng, W.; Rochwerg, B.; Seely, A.J.E.; Perry, J.J. Prognostic Accuracy of the Quick Sequential Organ Failure Assessment for Mortality in Patients with Suspected Infection: A Systematic Review and Meta-analysis. Ann. Intern. Med. 2018, 168, 266–275. [Google Scholar] [CrossRef]
- Herwanto, V.; Shetty, A.; Nalos, M.; Chakraborty, M.; McLean, A.; Eslick, G.D.; Tang, B. Accuracy of Quick Sequential Organ Failure Assessment Score to Predict Sepsis Mortality in 121 Studies Including 1,716,017 Individuals: A Systematic Review and Meta-Analysis. Crit. Care Explor. 2019, 1, e0043. [Google Scholar] [CrossRef]
- Lane, D.; Ichelson, R.I.; Drennan, I.R.; Scales, D.C. Prehospital management and identification of sepsis by emergency medical services: A systematic review. Emerg. Med. J. 2016, 33, 408–413. [Google Scholar] [CrossRef] [PubMed]
- Lane, D.J.; Wunsch, H.; Saskin, R.; Cheskes, S.; Lin, S.; Morrison, L.J.; Scales, D.C. Screening strategies to identify sepsis in the prehospital setting: A validation study. CMAJ 2020, 192, E230–E239. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| All Patients | |
|---|---|
| (n = 702) | |
| Sociodemographic data | |
| Age (years) | 68.4 ± 14.9 |
| Gender male | 411 (58.5%) |
| Emergency service data | |
| Urban area | 645 (91.9%) |
| Admission to emergency room | 197 (28.1%) |
| EMS with paramedics only | 451 (64.2%) |
| EMS with emergency physicians | 251 (35.8%) |
| Final diagnosis (at discharge) | |
| Sepsis | 585 (83.3%) |
| Severe sepsis | 22 (3.1%) |
| Septic shock | 95 (13.5%) |
| Sepsis focus (discharge diagnosis) | |
| Respiratory | 253 (36.0%) |
| Genitourinary tract | 180 (25.6%) |
| Abdominal | 96 (13.7%) |
| Blood stream | 54 (7.7%) |
| Skin | 36 (5.1%) |
| CNS | 12 (1.7%) |
| Other | 29 (4.1%) |
| Unknow | 42 (6.0%) |
| Prehospital assessed sepsis indicators b | |
| Abnormal body temperature a | 165 (23.5%) |
| Elevated heart rate (>90/min) a | 468 (66.6%) |
| Suspected infection a | 242 (34.5%) |
| Prehospital assessed qSOFA parameters b | |
| Respiratory rate ≥ 22/min a | 80 (11.4%) |
| Systolic blood pressure ≤ 100 mmHg a | 241 (34.4%) |
| Altered mentation a | 223 (31.7%) |
| Primary and secondary endpoints | |
| Time to antibiotics (min) c | 238.1 ± 195.2 |
| Time to fluid resuscitation (min) d | 255.3 ± 254.3 |
| ICU admission rate | 535 (76.2%) |
| Length of ICU stay (days) | 7 (4–14) |
| Length of hospital stay (days) | 11 (7–21) |
| In-hospital mortality (%) | 76 (10.8%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dankert, A.; Kraxner, J.; Breitfeld, P.; Bopp, C.; Issleib, M.; Doehn, C.; Bathe, J.; Krause, L.; Zöllner, C.; Petzoldt, M. Is Prehospital Assessment of qSOFA Parameters Associated with Earlier Targeted Sepsis Therapy? A Retrospective Cohort Study. J. Clin. Med. 2022, 11, 3501. https://doi.org/10.3390/jcm11123501
Dankert A, Kraxner J, Breitfeld P, Bopp C, Issleib M, Doehn C, Bathe J, Krause L, Zöllner C, Petzoldt M. Is Prehospital Assessment of qSOFA Parameters Associated with Earlier Targeted Sepsis Therapy? A Retrospective Cohort Study. Journal of Clinical Medicine. 2022; 11(12):3501. https://doi.org/10.3390/jcm11123501
Chicago/Turabian StyleDankert, André, Jochen Kraxner, Philipp Breitfeld, Clemens Bopp, Malte Issleib, Christoph Doehn, Janina Bathe, Linda Krause, Christian Zöllner, and Martin Petzoldt. 2022. "Is Prehospital Assessment of qSOFA Parameters Associated with Earlier Targeted Sepsis Therapy? A Retrospective Cohort Study" Journal of Clinical Medicine 11, no. 12: 3501. https://doi.org/10.3390/jcm11123501
APA StyleDankert, A., Kraxner, J., Breitfeld, P., Bopp, C., Issleib, M., Doehn, C., Bathe, J., Krause, L., Zöllner, C., & Petzoldt, M. (2022). Is Prehospital Assessment of qSOFA Parameters Associated with Earlier Targeted Sepsis Therapy? A Retrospective Cohort Study. Journal of Clinical Medicine, 11(12), 3501. https://doi.org/10.3390/jcm11123501







