The Use of Computer-Driven Technologies in the Treatment of Borderline Personality Disorder: A Systematic Review
Abstract
:1. Introduction
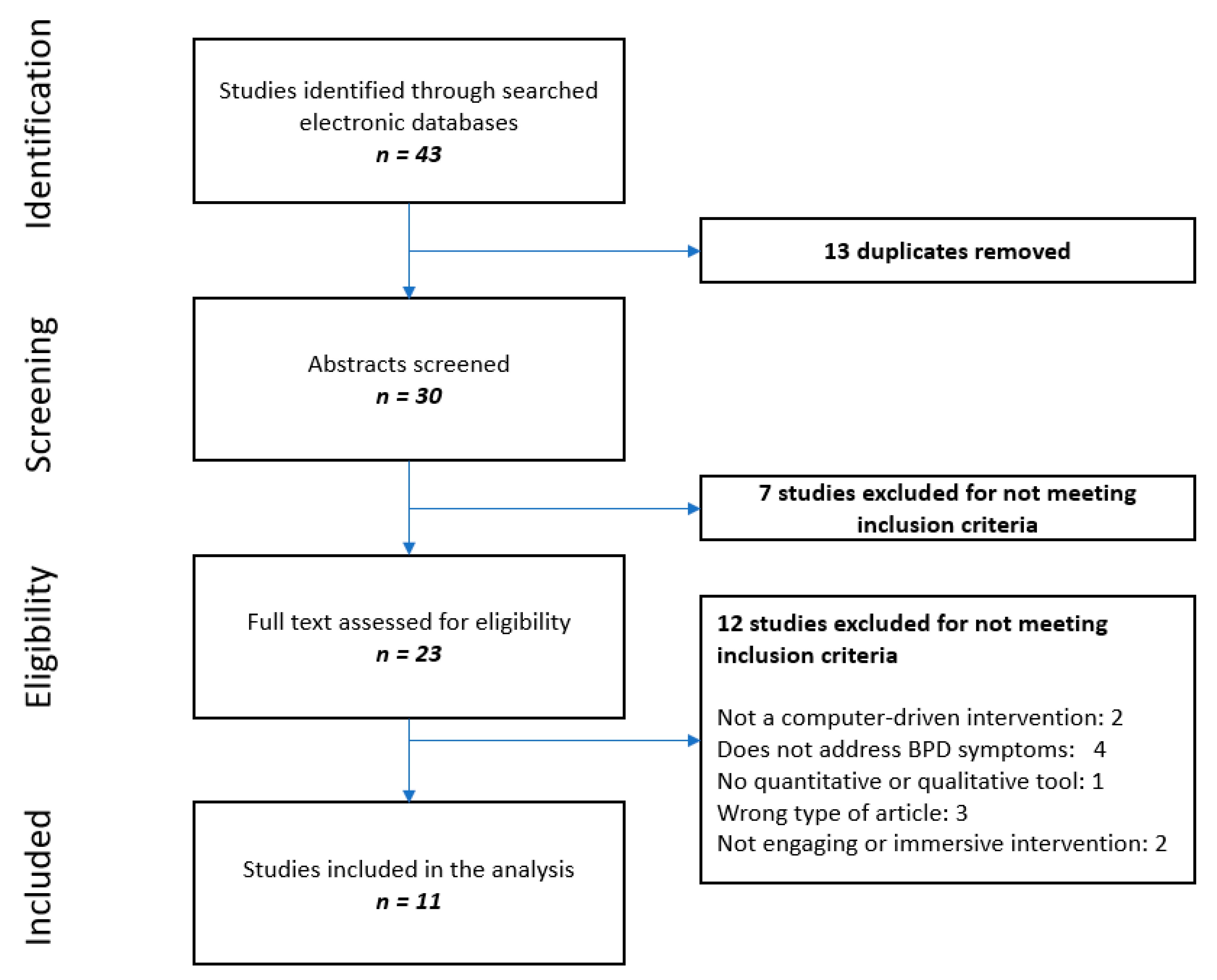
2. Materials and Methods
2.1. Search Strategies
2.2. Study Eligibility
2.3. Data Extraction
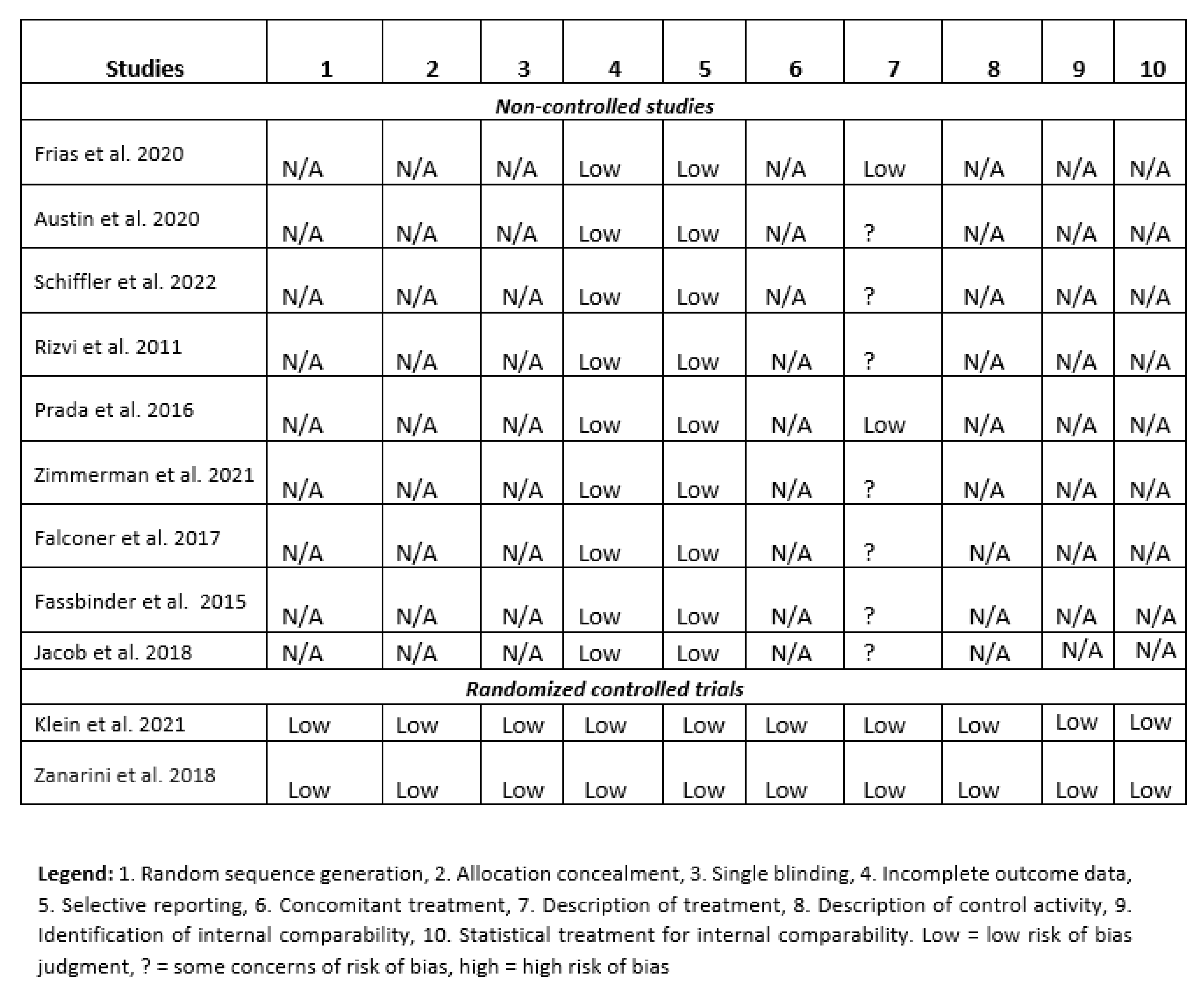
2.4. Quality Analysis of Studies
3. Results
3.1. Description of Studies
3.2. Computer-Driven Interventions
3.2.1. Mobile Applications
3.2.2. Internet-Based Interventions
3.2.3. Telehealth Intervention
3.2.4. Virtual Reality MBT
3.2.5. Dialogue-Based Integrated Interventions
3.3. Outcomes
4. Discussion
4.1. About the Findings
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
- Concept 1
- Concept 2
References
- Ten Have, M.; Verheul, R.; Kaasenbrood, A.; van Dorsselaer, S.; Tuithof, M.; Kleinjan, M.; de Graaf, R. Prevalence rates of borderline personality disorder symptoms: A study based on the Netherlands Mental Health Survey and Incidence Study-2. BMC Psychiatry 2016, 16, 249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gunderson, J.G.; Herpertz, S.C.; Skodol, A.E.; Torgersen, S.; Zanarini, M.C. Borderline personality disorder. Nat. Rev. Dis. Primers. 2018, 4, 18029. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bohus, M.; Stoffers-Winterling, J.; Sharp, C.; Krause-Utz, A.; Schmahl, C.; Lieb, K. Borderline personality disorder. Lancet 2021, 398, 1528–1540. [Google Scholar] [CrossRef]
- Leichsenring, F.; Leibing, E.; Kruse, J.; New, A.S.; Leweke, F. Borderline personality disorder. Lancet 2011, 377, 74–84. [Google Scholar] [CrossRef]
- Paris, J. Suicidality in Borderline Personality Disorder. Medicina 2019, 55, 223. [Google Scholar] [CrossRef] [Green Version]
- Oumaya, M.; Friedman, S.; Pham, A.; Abou Abdallah, T.; Guelfi, J.D.; Rouillon, F. Personnalité borderline, automutilations et suicide: Revue de la littérature [Borderline personality disorder, self-mutilation and suicide: Literature review]. Encephale 2008, 34, 452–458. [Google Scholar] [CrossRef]
- Söderholm, J.J.; Socada, J.L.; Rosenström, T.; Ekelund, J.; Isometsä, E.T. Borderline Personality Disorder With Depression Confers Significant Risk of Suicidal Behavior in Mood Disorder Patients-A Comparative Study. Front. Psychiatry 2020, 11, 290. [Google Scholar] [CrossRef]
- Wagner, T.; Fydrich, T.; Stiglmayr, C.; Marschall, P.; Salize, H.-J.; Rennerberg, B.; Fleßa, S.; Roepke, S. Societal cost-of-illness in patients with borderline personality disorder one year before, during and after dialectical behavior therapy in routine outpatient care. Behav. Res. Ther. 2014, 61, 12–22. [Google Scholar] [CrossRef]
- Hastrup, L.H.; Jennum, P.; Ibsen, R.; Kjellberg, J.; Simonsen, E. Societal costs of Borderline Personality Disorders: A matched-controlled nationwide study of patients and spouses. Acta Psychiatr Scand. 2019, 140, 458–467. [Google Scholar] [CrossRef]
- Simonsen, S.; Bateman, A.; Bohus, M.; Dalewijk, H.; Doering, S.; Kaera, A.; Moran, P.; Renneberg, B.; Ribaudi, J.; Taubner, S.; et al. European guidelines for personality disorders: Past, present and future. Bord. Personal. Disord. Emot. Dysregulation 2019, 6, 9. [Google Scholar] [CrossRef]
- Biskin, R.S.; Paris, J. Management of borderline personality disorder. CMAJ. 2012, 184, 1897–1902. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Storebø, O.J.; Stoffers-Winterling, J.M.; Völlm, B.A.; Kongerslev, M.T.; Mattivi, J.T.; Jørgensen, M.S.; Faltinsen, E.; Todorovac, A.; Sales, C.P.; Callesen, H.E. Psychological therapies for people with borderline personality disorder. Cochrane Database Syst. Rev. 2020, 5, CD012955. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bedics, J.D.; Atkins, D.C.; Comtois, K.A.; Linehan, M.M. Treatment differences in the therapeutic relationship and introject during a 2-year randomized controlled trial of dialectical behavior therapy versus nonbehavioral psychotherapy experts for borderline personality disorder. J. Consult. Clin. Psychol. 2012, 80, 66–77. [Google Scholar] [CrossRef]
- Vogt, K.S.; Norman, P. Is mentalization-based therapy effective in treating the symptoms of borderline personality disorder? A systematic review. Psychol. Psychother. 2019, 92, 441–464. [Google Scholar] [CrossRef]
- Limandri, B.J. Psychopharmacology for Borderline Personality Disorder. J. Psychosoc. Nurs. Ment. Health Serv. 2018, 56, 8–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Del Casale, A.; Bonanni, L.; Bargagna, P.; Novelli, F.; Fiaschè, F.; Paolini, M.; Fprcina, F.; Anibaldi, G.; Cortese, F.N.; Iannuccelli, A.; et al. Current Clinical Psychopharmacology in Borderline Personality Disorder. Curr. Neuropharmacol. 2021, 19, 1760–1779. [Google Scholar] [CrossRef] [PubMed]
- Paris, J. Why patients with severe personality disorders are overmedicated. J. Clin. Psychiatry 2015, 76, e521. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wibbelink, C.; Arntz, A.; Grasman, R.; Sinnaeve, R.; Boog, M.; Bremer, O.; Dek, E.; Alkan, S.; James, C.; Koppeschaar, A.; et al. Towards optimal treatment selection for borderline personality disorder patients (BOOTS): A study protocol for a multicenter randomized clinical trial comparing schema therapy and dialectical behavior therapy. BMC Psychiatry 2022, 22, 89. [Google Scholar] [CrossRef]
- Safdar, M.F.; Bhatti, S.N.; Abbasi, A.S.; Zahra, F.T. Applications and impact of computer technologies in management of multimorbidity. J. Pak. Med. Assoc. 2020, 70, 1572–1576. [Google Scholar] [CrossRef]
- Arane, K.; Behboudi, A.; Goldman, R.D. Virtual reality for pain and anxiety management in children. Can. Fam. Physician 2017, 63, 932–934. [Google Scholar]
- Dellazizzo, L.; Potvin, S.; Phraxayavong, K.; Dumais, A. One-year randomized trial comparing virtual reality-assisted therapy to cognitive-behavioural therapy for patients with treatment-resistant schizophrenia. NPJ Schizophr. 2021, 7, 9. [Google Scholar] [CrossRef] [PubMed]
- Salehi, E.; Mehrabi, M.; Fatehi, F.; Salehi, A. Virtual Reality Therapy for Social Phobia: A Scoping Review. Stud. Health Technol. Inform. 2020, 270, 713–717. [Google Scholar] [CrossRef] [PubMed]
- Karyotaki, E.; Efthimiou, O.; Miguel, C. Internet-Based Cognitive Behavioural Therapy for Depression: A Systematic Review and Individual Patient Data Network Meta-analysis. JAMA Psychiatry 2021, 78, 361–371. [Google Scholar] [CrossRef] [PubMed]
- Frías, Á.; Solves, L.; Navarro, S.; Palma, C.; Farriols, N.; Aliaga, F.; Hernández, M.; Antón, M.; Riera, A. Technology-Based Psychosocial Interventions for People with Borderline Personality Disorder: A Scoping Review of the Literature. Psychopathology 2020, 53, 254–263. [Google Scholar] [CrossRef]
- Higgins, J.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0. Chapter 8: Assessing Risk of Bias in Included Studies. Available online: http://handbook.cochrane.org/ (accessed on 29 May 2022).
- Frías, Á.; Palma, C.; Salvador, A.; Aluco, E.; Navarro, S.; Farriols, N.; Aliaga, F.; Solves, L.; Antón, M. B·RIGHT: Usability and satisfaction with a mobile app for self-managing emotional crises in patients with borderline personality disorder. Australas Psychiatry 2021, 29, 294–298. [Google Scholar] [CrossRef]
- Austin, S.F.; Jansen, J.E.; Petersen, C.J.; Jensen, R.; Simonsen, E. Mobile App Integration Into Dialectical Behavior Therapy for Persons With Borderline Personality Disorder: Qualitative and Quantitative Study. JMIR Ment. Health 2020, 7, e14913. [Google Scholar] [CrossRef]
- Schiffler, T.; Seiler-Ramadas, R.; Štefanac, S.; Haider, S.; Mües, H.M.; Grabovac, I. Implementation of a Mobile DBT App and Its Impact on Suicidality in Transitional Age Youth with Borderline Personality Disorder: A Qualitative Study. Int. J. Environ. Res. Public Health 2022, 19, 701. [Google Scholar] [CrossRef]
- Rizvi, S.L.; Dimeff, L.A.; Skutch, J.; Carroll, D.; Linehan, M.M. A pilot study of the DBT coach: An interactive mobile phone application for individuals with borderline personality disorder and substance use disorder. Behav. Ther. 2011, 42, 589–600. [Google Scholar] [CrossRef]
- Prada, P.; Zamberg, I.; Bouillault, G.; Jimenez, N.; Zimmermann, J.; Hasler, R.; Aubry, J.-M.; Nicastro, R.; Perroud, N. EMOTEO: A Smartphone Application for Monitoring and Reducing Aversive Tension in Borderline Personality Disorder Patients, a Pilot Study. Perspect. Psychiatr. Care 2017, 53, 289–298. [Google Scholar] [CrossRef]
- Klein, J.P.; Hauer-von Mauschwitz, A.; Berger, T.; Fassbinder, E.; Mayer, J.; Borgwardt, S.; Wellhöfer, B.; Schweiger, U.; Jacob, G. Effectiveness and safety of the adjunctive use of an internet-based self-management intervention for borderline personality disorder in addition to care as usual: Results from a randomized controlled trial. BMJ Open 2021, 11, e047771. [Google Scholar] [CrossRef]
- Zanarini, M.C.; Conkey, L.C.; Temes, C.M.; Fitzmaurice, G.M. Randomized Controlled Trial of Web-Based Psychoeducation for Women With Borderline Personality Disorder. J. Clin. Psychiatry 2018, 79, 16m11153. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, M.; Ward, M.; D’Avanzato, C.; Tirpak, J.W. Telehealth Treatment of Patients With Borderline Personality Disorder in a Partial Hospital Setting During the COVID-19 Pandemic: Comparative Safety, Patient Satisfaction, and Effectiveness of In-Person Treatment. J. Pers. Disord. 2021, 36, 277–295. [Google Scholar] [CrossRef] [PubMed]
- Falconer, C.J.; Cutting, P.; Bethan Davies, E.; Hollis, C.; Stallard, P.; Moran, P. Adjunctive avatar therapy for mentalization-based treatment of borderline personality disorder: A mixed-methods feasibility study. Evid. Based Ment. Health 2017, 20, 123–127. [Google Scholar] [CrossRef] [PubMed]
- Fassbinder, E.; Hauer, A.; Schaich, A.; Schweiger, U.; Jacob, G.A.; Arntz, A. Integration of e-Health Tools Into Face-to-Face Psychotherapy for Borderline Personality Disorder: A Chance to Close the Gap Between Demand and Supply? J. Clin. Psychol. 2015, 71, 764–777. [Google Scholar] [CrossRef] [PubMed]
- Jacob, G.A.; Hauer, A.; Köhne, S.; Assmann, N.; Schaich, A.; Schweiger, U.; Fassbinder, E. A Schema Therapy-Based eHealth Program for Patients with Borderline Personality Disorder (priovi): Naturalistic Single-Arm Observational Study. JMIR Ment. Health 2018, 5, e10983. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Varma, D.S.; Prosperi, M. A systematic review of the effectiveness of mobile apps for monitoring and management of mental health symptoms or disorders. J. Psychiatr. Res. 2018, 107, 73–78. [Google Scholar] [CrossRef]
- Morris, M.E.; Aguilera, A. Mobile, Social, and Wearable Computing and the Evolution of Psychological Practice. Prof. Psychol Res. Pr 2012, 43, 622–626. [Google Scholar] [CrossRef] [Green Version]
- Hoffner, C.A.; Lee, S. Mobile Phone Use, Emotion Regulation, and Well-Being. Cyberpsychol. Behav. Soc. Netw. 2015, 18, 411–416. [Google Scholar] [CrossRef]
- Brickell, C.M. Diagnosis and Treatment of Borderline Personality Disorder in the College Mental Health Setting. Curr. Psychiatry Rep. 2018, 20, 38. [Google Scholar] [CrossRef]
- Paris, J. Making psychotherapy for borderline personality disorder accessible. Ann. Clin. Psychiatry 2015, 27, 297–301. [Google Scholar]
- van der Boom, B.; Boumparis, N.; Donker, T.; de Beurs, D.; Arntz, A.; Riper, H. Internet-delivered interventions for personality disorders–A scoping review. Internet Interv. 2022, 28, 100525. [Google Scholar] [CrossRef] [PubMed]
- Wosik, J.; Fudim, M.; Cameron, B.; Gellad, Z.F.; Cho, A.; Phinney, D.; Curtis, S.; Roman, M.; Poon, E.G.; Ferranti, J.; et al. Telehealth transformation: COVID-19 and the rise of virtual care. J. Am. Med. Inform. Assoc. 2020, 27, 957–962. [Google Scholar] [CrossRef] [PubMed]
- Herbert, M.S.; Afari, N.; Liu, L.; Heppner, P.; Rutledge, T.; Williams, K.; Early, S.; VanBuskirk, K.; Nguyen, C.; Bondi, M. Telehealth Versus In-Person Acceptance and Commitment Therapy for Chronic Pain: A Randomized Noninferiority Trial. J. Pain. 2017, 18, 200–211. [Google Scholar] [CrossRef] [PubMed]
- Bateman, A.; Fonagy, P. Mentalization based treatment for borderline personality disorder. World Psychiatry 2010, 9, 11–15. [Google Scholar] [CrossRef] [PubMed]
- Bell, I.H.; Nicholas, J.; Alvarez-Jimenez, M.; Thompson, A.; Valmaggia, L. Virtual reality as a clinical tool in mental health research and practice. Dialogues Clin. Neurosci. 2020, 22, 169–177. [Google Scholar] [CrossRef]
- Sempértegui, G.A.; Karreman, A.; Arntz, A.; Bekker, M.H. Schema therapy for borderline personality disorder: A comprehensive review of its empirical foundations, effectiveness and implementation possibilities. Clin. Psychol. Rev. 2013, 33, 426–447. [Google Scholar] [CrossRef]
- Tan, Y.M.; Lee, C.W.; Averbeck, L.E.; Wilde, O.B.; Farrell, J.; Fassbinder, E.; Jacob, G.A.; Martius, D.; Wastiaux, S.; Zarbock, G. Schema therapy for borderline personality disorder: A qualitative study of patients’ perceptions. PLoS ONE 2018, 13, e0206039. [Google Scholar] [CrossRef] [Green Version]
- Arntz, A.; Jacob, G.A.; Lee, C.W. Effectiveness of Predominantly Group Schema Therapy and Combined Individual and Group Schema Therapy for Borderline Personality Disorder: A Randomized Clinical Trial. JAMA Psychiatry 2022, 79, 287–299. [Google Scholar] [CrossRef]
| Studies | Intervention Type | Number of Participants | Outcome of Interest | Measurement Indicators | Effect Size | General Conclusion |
|---|---|---|---|---|---|---|
| Frias et al., 2020 [26] | B-RIGHT: mobile app for selfmanaging emotional crises | 25 outpatients, 84% female | Satisfaction, usability, emotion dysregulation and depression severity. BSL-23, Difficulties in Emotion Regulation Scale, Beck Depression Inventory | Pearson’s correlation (r) or Spearman’s correlation (rho) | Emotion dysregulation (r = 0.51); depression severity (rho = −0.47) | Promising results. Mobile application may work as a transitional object |
| Austin et al., 2020 [27] | Mobile app integration into dialectical Behaviour therapy | 24 outpatients | Overall experience, facilitate therapeutic alliance | Qualitative | Not applicable | May make many of the therapeutic techniques in DBT treatment easier |
| Schiffler et al., 2022 [28] | Mobile DBT application | 13 transitional age youth (18–23 years old) | Experiences and associated emotions before and after a testing period of 30 days | Qualitative | Not applicable | Did not bring about any changes in the subjective view of suicidality |
| Rizvi et al., 2011 [29] | Mobile phone application: DBT coach | 22 patients with BPD and substance use | Emotion intensity and urges to use substances | Beck Depression Inventory, Behavorial Confidence Questionnaire, Brief Symptom Inventory | Reduction in emotional intensity from precoaching to postcoaching was significant, B = −1.26, SE = 0.20, t(21) = −6.17, p < 0.001. Reduction in urges to use substances was also significant, B = −0.92, SE = 0.22, t(21) = −4.22, p < 0.001 | May be a useful tool for reducing urges to use substances and engage in other maladaptive behaviour |
| Prada et al., 2016 [30] | EMOTEO: A smartphone application for monitoring and reducing aversive tension in BPD | 16 patients with BPD | Aversive tension | Self-reported homemade questionnaire | No effect size reported. Regarding aversive tension, users reported a mean of 4.5 (on a scale ranging from 1 to 5, where 5 is the best outcome) with an SD of 0.71 | EMOTEO was user-friendly and efficient in reducing aversive tension in BPD patients |
| Klein et al., 2021 [31] | Internet-based self-management intervention for BPD | 204 patients with BPD, randomized in two groups: care as usual and care as usual + internet-based system | Effectiveness and safety | BPDSI | At 12 months, Cohen’s D of 1.38 for intervention group and 1.02 for the control group | No significant difference between the intervention and care as usual for the intention-to-treat protocol; however there were significant differences in the per-protocol |
| Zanarini et al., 2018 [32] | Web-based psychoeducation | 80 women with BDP, randomized in two groups of 40: with web-based psychoeducation and without web-based psychoeducation | BPD symptoms | Zanarini Rating Scale for Borderline Personality Disorder | Treatment group reported a significantly greater decline in all five studied areas of borderline psychopathology: affective symptoms (z = −2.31, p = 0.021), cognitive symptoms (z = −3.20, p = 0.001), impulsivity (z = −2.44, p = 0.015), interpersonal difficulties (z = −2.15, p = 0.032), and overall borderline personality disorder symptoms (z = −2.11, p = 0.035) | Internet-based psychoeducation is an effective form of early treatment for reducing the symptom severity of BPD |
| Zimmerman et al., 2021 [33] | Telehealth treatment of patients with borderline personality disorder in a partial hospital setting: comparative study | 54 in-person patients with BDP, 28 patients with BDP using the telehealth modality | Symptoms, depression, anxiety, anger, physical pain, positive mental health, functioning, coping skills, well-being | Remission from Depression Questionnaire | Effect sizes (Cohen’s D) of 1.81, 1.98, 1.48, 1.03, 0.53, 1.45, 1.63, 1.61 and 1.78, respectively | Significantly greater improvement in functioning in the virtual program, less improvement in anger |
| Falconer et al., 2017 [34] | Avatar-based MBT | 11 outpatients | Perspective taking, expression, emotional distancing; 21-item Depression, Anxiety and Stress Scales; Mentalization Questionnaire; semi-structured interviews | Mean and standard deviation analysis via ANOVA; thematic annotations | No effect from the ANOVA. May enhance the therapeutic efficacy of standard MBT | Avatar-MBT is a promising enhancement of therapy for BPD |
| Fassbinder et al., 2015 [35] | Priovi: dialogue-based integrated structure | 1 case example | Skills and experiences in patients with BPD | Borderline Personality Disorder Severity Index (BPDSI); WHODAS 2.0, overall score; Schema Mode Inventory | Decrease of 27 points in the BPDSI | Could potentially increase treatment intensity and enhance treatment effects |
| Jacob et al., 2018 [36] | Priovi: observational study | 13 participants diagnosed with BDP: 11 females, 2 males | BPD symptoms | BPDSI-IV, BPD-CL, qualitative patient interviews, qualitative therapist interviews | Reduction of 9.6 points in the BPDSI (Cohen’s D = 1.0) and of 29.9 in BPD-CL (Cohen’s D = 1.2) | Priovi could be a potentially helpful tool in the improvements of BPD symptoms |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hudon, A.; Gaudreau-Ménard, C.; Bouchard-Boivin, M.; Godin, F.; Cailhol, L. The Use of Computer-Driven Technologies in the Treatment of Borderline Personality Disorder: A Systematic Review. J. Clin. Med. 2022, 11, 3685. https://doi.org/10.3390/jcm11133685
Hudon A, Gaudreau-Ménard C, Bouchard-Boivin M, Godin F, Cailhol L. The Use of Computer-Driven Technologies in the Treatment of Borderline Personality Disorder: A Systematic Review. Journal of Clinical Medicine. 2022; 11(13):3685. https://doi.org/10.3390/jcm11133685
Chicago/Turabian StyleHudon, Alexandre, Caroline Gaudreau-Ménard, Marissa Bouchard-Boivin, Francis Godin, and Lionel Cailhol. 2022. "The Use of Computer-Driven Technologies in the Treatment of Borderline Personality Disorder: A Systematic Review" Journal of Clinical Medicine 11, no. 13: 3685. https://doi.org/10.3390/jcm11133685
APA StyleHudon, A., Gaudreau-Ménard, C., Bouchard-Boivin, M., Godin, F., & Cailhol, L. (2022). The Use of Computer-Driven Technologies in the Treatment of Borderline Personality Disorder: A Systematic Review. Journal of Clinical Medicine, 11(13), 3685. https://doi.org/10.3390/jcm11133685