The Effectiveness of Hydrodissection with 5% Dextrose for Persistent and Recurrent Carpal Tunnel Syndrome: A Retrospective Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Inclusion and Exclusion Criteria
2.3. Primary Measures
2.4. Ultrasound-Guided Hydrodissection with 5% Dextrose
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Burton, C.L.; Chesterton, L.S.; Chen, Y.; van der Windt, D.A. Clinical Course and Prognostic Factors in Conservatively Managed Carpal Tunnel Syndrome: A Systematic Review. Arch. Phys. Med. Rehabil. 2016, 97, 836–852.e1. [Google Scholar] [CrossRef] [Green Version]
- Uchiyama, S.; Itsubo, T.; Nakamura, K.; Kato, H.; Yasutomi, T.; Momose, T. Current concepts of carpal tunnel syndrome: Pathophysiology, treatment, and evaluation. J. Orthop. Sci. Off. J. Jpn. Orthop. Assoc. 2010, 15, 1–13. [Google Scholar] [CrossRef]
- Chang, K.V.; Wu, W.T.; Ozcakar, L. Ultrasound imaging and guidance in peripheral nerve entrapment: Hydrodissection highlighted. Pain Manag. 2020, 10, 97–106. [Google Scholar] [CrossRef]
- Atroshi, I.; Gummesson, C.; Johnsson, R.; Ornstein, E.; Ranstam, J.; Rosen, I. Prevalence for clinically proved carpal tunnel syndrome is 4 percent. Lakartidningen 2000, 97, 1668–1670. [Google Scholar]
- Werner, R.A.; Andary, M. Carpal tunnel syndrome: Pathophysiology and clinical neurophysiology. Clin. Neurophysiol. 2002, 113, 1373–1381. [Google Scholar] [CrossRef]
- Padua, L.; Coraci, D.; Erra, C.; Pazzaglia, C.; Paolasso, I.; Loreti, C.; Caliandro, P.; Hobson-Webb, L.D. Carpal tunnel syndrome: Clinical features, diagnosis, and management. Lancet Neurol. 2016, 15, 1273–1284. [Google Scholar] [CrossRef]
- Wu, Y.T.; Ke, M.J.; Chou, Y.C.; Chang, C.Y.; Lin, C.Y.; Li, T.Y.; Shih, F.M.; Chen, L.C. Effect of radial shock wave therapy for carpal tunnel syndrome: A prospective randomized, double-blind, placebo-controlled trial. J. Orthop. Res. 2016, 34, 977–984. [Google Scholar] [CrossRef]
- Lauder, A.; Mithani, S.; Leversedge, F.J. Management of Recalcitrant Carpal Tunnel Syndrome. J. Am. Acad. Orthop. Surg. 2019, 27, 551–562. [Google Scholar] [CrossRef]
- Varitimidis, S.E.; Herndon, J.H.; Sotereanos, D.G. Failed endoscopic carpal tunnel release. Operative findings and results of open revision surgery. J. Hand Surg. 1999, 24, 465–467. [Google Scholar] [CrossRef]
- Beck, J.D.; Brothers, J.G.; Maloney, P.J.; Deegan, J.H.; Tang, X.; Klena, J.C. Predicting the outcome of revision carpal tunnel release. J. Hand Surg. 2012, 37, 282–287. [Google Scholar] [CrossRef]
- Zieske, L.; Ebersole, G.C.; Davidge, K.; Fox, I.; Mackinnon, S.E. Revision carpal tunnel surgery: A 10-year review of intraoperative findings and outcomes. J. Hand Surg. 2013, 38, 1530–1539. [Google Scholar] [CrossRef] [Green Version]
- Strasberg, S.R.; Novak, C.B.; Mackinnon, S.E.; Murray, J.F. Subjective and employment outcome following secondary carpal tunnel surgery. Ann. Plast. Surg. 1994, 32, 485–489. [Google Scholar] [CrossRef]
- Wu, Y.T.; Ho, T.Y.; Chou, Y.C.; Ke, M.J.; Li, T.Y.; Tsai, C.K.; Chen, L.C. Six-month Efficacy of Perineural Dextrose for Carpal Tunnel Syndrome: A Prospective, Randomized, Double-Blind, Controlled Trial. Mayo Clin. Proc. 2017, 92, 1179–1189. [Google Scholar] [CrossRef]
- Wu, Y.T.; Ke, M.J.; Ho, T.Y.; Li, T.Y.; Shen, Y.P.; Chen, L.C. Randomized double-blinded clinical trial of 5% dextrose versus triamcinolone injection for carpal tunnel syndrome patients. Ann. Neurol. 2018, 84, 601–610. [Google Scholar] [CrossRef]
- Lin, M.T.; Liao, C.L.; Hsiao, M.Y.; Hsueh, H.W.; Chao, C.C.; Wu, C.H. Volume Matters in Ultrasound-Guided Perineural Dextrose Injection for Carpal Tunnel Syndrome: A Randomized, Double-Blinded, Three-Arm Trial. Front. Pharmacol. 2020, 11, 625830. [Google Scholar] [CrossRef]
- Lin, M.T.; Liu, I.C.; Syu, W.T.; Kuo, P.L.; Wu, C.H. Effect of Perineural Injection with Different Dextrose Volumes on Median Nerve Size, Elasticity and Mobility in Hands with Carpal Tunnel Syndrome. Diagnostics 2021, 11, 849. [Google Scholar] [CrossRef]
- Li, T.Y.; Chen, S.R.; Shen, Y.P.; Chang, C.Y.; Su, Y.C.; Chen, L.C.; Wu, Y.T. Long-term outcome after perineural injection with 5% dextrose for carpal tunnel syndrome: A retrospective follow-up study. Rheumatology 2021, 60, 881–887. [Google Scholar] [CrossRef]
- Chen, L.C.; Ho, T.Y.; Shen, Y.P.; Su, Y.C.; Li, T.Y.; Tsai, C.K.; Wu, Y.T. Perineural Dextrose and Corticosteroid Injections for Ulnar Neuropathy at the Elbow: A Randomized Double-blind Trial. Arch. Phys. Med. Rehabil. 2020, 101, 1296–1303. [Google Scholar] [CrossRef]
- Wu, Y.T.; Chen, S.R.; Li, T.Y.; Ho, T.Y.; Shen, Y.P.; Tsai, C.K.; Chen, L.C. Nerve hydrodissection for carpal tunnel syndrome: A prospective, randomized, double-blind, controlled trial. Muscle Nerve 2019, 59, 174–180. [Google Scholar] [CrossRef]
- Chen, S.-R.; Ho, T.-Y.; Shen, Y.-P.; Li, T.-Y.; Su, Y.-C.; Lam, K.H.S.; Chen, L.-C.; Wu, Y.-T. Comparison of short- and long-axis nerve hydrodissection for carpal tunnel syndrome: A prospective randomized, single-blind trial. Int. J. Med. Sci. 2021, 18, 3488–3497. [Google Scholar] [CrossRef]
- Lin, C.P.; Chang, K.V.; Huang, Y.K.; Wu, W.T.; Özçakar, L. Regenerative Injections Including 5% Dextrose and Platelet-Rich Plasma for the Treatment of Carpal Tunnel Syndrome: A Systematic Review and Network Meta-Analysis. Pharmaceuticals 2020, 13, 49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, Y.T.; Wu, C.H.; Lin, J.A.; Su, D.C.; Hung, C.Y.; Lam, S.K.H. Efficacy of 5% Dextrose Water Injection for Peripheral Entrapment Neuropathy: A Narrative Review. Int. J. Mol. Sci. 2021, 22, 12358. [Google Scholar] [CrossRef] [PubMed]
- Buntragulpoontawee, M.; Chang, K.V.; Vitoonpong, T.; Pornjaksawan, S.; Kitisak, K.; Saokaew, S.; Kanchanasurakit, S. The Effectiveness and Safety of Commonly Used Injectates for Ultrasound-Guided Hydrodissection Treatment of Peripheral Nerve Entrapment Syndromes: A Systematic Review. Front. Pharmacol. 2020, 11, 621150. [Google Scholar] [CrossRef]
- Lai, C.Y.; Li, T.Y.; Lam, K.H.S.; Chou, Y.C.; Hueng, D.Y.; Chen, L.C.; Wu, Y.T. The long-term analgesic effectiveness of platelet-rich plasma injection for carpal tunnel syndrome: A cross-sectional cohort study. Pain Med. 2022, pnac011. [Google Scholar] [CrossRef]
- Lam, K.H.S.; Hung, C.Y.; Chiang, Y.P.; Onishi, K.; Su, D.C.J.; Clark, T.B.; Reeves, K.D. Ultrasound-Guided Nerve Hydrodissection for Pain Management: Rationale, Methods, Current Literature, and Theoretical Mechanisms. J. Pain Res. 2020, 13, 1957–1968. [Google Scholar] [CrossRef]
- Lam, K.H.S.; Lai, W.W.; Ngai, H.Y.; Wu, W.K.R.; Wu, Y.-T. Comment on the safety of the ultrasound-guided hydrodissection technique for carpal tunnel syndrome. J. Ultrasound 2022. [Google Scholar] [CrossRef]
- Lam, K.H.S.; Lai, W.W.; Ngai, H.Y.; Wu, W.K.R. Practical Considerations for Ultrasound-Guided Hydrodissection in Pronator Teres Syndrome. Pain Med. 2022, 23, 221–223. [Google Scholar] [CrossRef]
- Tung, T.H.; Mackinnon, S.E. Secondary carpal tunnel surgery. Plast. Reconstr. Surg. 2001, 107, 1830–1843, quiz 1844, 1933. [Google Scholar] [CrossRef]
- Louie, D.; Earp, B.; Blazar, P. Long-term outcomes of carpal tunnel release: A critical review of the literature. Hand 2012, 7, 242–246. [Google Scholar] [CrossRef] [Green Version]
- O’Malley, M.J.; Evanoff, M.; Terrono, A.L.; Millender, L.H. Factors that determine reexploration treatment of carpal tunnel syndrome. J. Hand Surg. 1992, 17, 638–641. [Google Scholar] [CrossRef]
- Chang, B.; Dellon, A.L. Surgical management of recurrent carpal tunnel syndrome. J. Hand Surg. 1993, 18, 467–470. [Google Scholar] [CrossRef]
- Rose, E.H. The use of the palmaris brevis flap in recurrent carpal tunnel syndrome. Hand Clin. 1996, 12, 389–395. [Google Scholar] [CrossRef]
- Lam, S.K.H.; Reeves, K.D.; Cheng, A.L. Transition from deep regional blocks toward deep nerve hydrodissection in the upper body and torso: Method description and results from a retrospective chart review of the analgesic effect of 5% dextrose water as the primary hydrodissection injectate to enhance safety. Biomed Res. Int. 2017, 2017, 7920438. [Google Scholar] [PubMed] [Green Version]
- Hung, C.Y.; Lam, K.H.S.; Wu, Y.T. Dynamic Ultrasound for Carpal Tunnel Syndrome Caused by Squeezed Median Nerve between the Flexor Pollicis Longus and Flexor Digitorum Tendons. Pain Med. 2021, pnab316. [Google Scholar] [CrossRef] [PubMed]
- Lam, K.H.S.; Lai, W.W.; Ngai, H.Y.; Wu, W.K.R.; Wu, Y.-T. Commentary: Ultrasound-Guided Triamcinolone Acetonide Hydrodissection for Carpal Tunnel Syndrome: A Randomized Controlled Trial. Front. Med. 2022, 8, 833862. [Google Scholar] [CrossRef]
- MacIver, M.B.; Tanelian, D.L. Activation of C fibers by metabolic perturbations associated with tourniquet ischemia. Anesthesiology 1992, 76, 617–623. [Google Scholar] [CrossRef]
- Jensen, V.F.; Mølck, A.M.; Bøgh, I.B.; Lykkesfeldt, J. Effect of insulin-induced hypoglycaemia on the peripheral nervous system: Focus on adaptive mechanisms, pathogenesis and histopathological changes. J. Neuroendocrinol. 2014, 26, 482–496. [Google Scholar] [CrossRef]
- Burdakov, D.; Jensen, L.T.; Alexopoulos, H.; Williams, R.H.; Fearon, I.M.; O’Kelly, I.; Gerasimenko, O.; Fugger, L.; Verkhratsky, A. Tandem-pore K+ channels mediate inhibition of orexin neurons by glucose. Neuron 2006, 50, 711–722. [Google Scholar] [CrossRef]
- Carling, D. The AMP-activated protein kinase cascade—A unifying system for energy control. Trends Biochem. Sci. 2004, 29, 18–24. [Google Scholar] [CrossRef]
- Wang, S.; Dai, Y. Roles of AMPK and Its Downstream Signals in Pain Regulation. Life 2021, 11, 836. [Google Scholar] [CrossRef]
- Wu, Y.T.; Chen, Y.P.; Lam, K.H.S.; Reeves, K.D.; Lin, J.A.; Kuo, C.Y. Mechanism of glucose water as a neural injection: A perspective on neuroinflammation. Life 2022, 12, 832. [Google Scholar] [CrossRef] [PubMed]
- Cobb, T.K.; Amadio, P.C.; Leatherwood, D.F.; Schleck, C.D.; Ilstrup, D.M. Outcome of reoperation for carpal tunnel syndrome. J. Hand Surg. 1996, 21, 347–356. [Google Scholar] [CrossRef]
- Stang, F.; Stütz, N.; Lanz, U.; van Schoonhoven, J.; Prommersberger, K.J. Results after revision surgery for carpal tunnel release. Handchir. Mikrochir. Plast. Chir. 2008, 40, 289–293. [Google Scholar] [CrossRef] [PubMed]
- Cass, S.P. Ultrasound-Guided Nerve Hydrodissection: What is it? A review of the literature. Curr. Sports Med. Rep. 2016, 15, 20–22. [Google Scholar] [CrossRef]
- Farrar, J.T.; Young, J.P., Jr.; LaMoreaux, L.; Werth, J.L.; Poole, R.M. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2001, 94, 149–158. [Google Scholar] [CrossRef]
- Spadoni, G.F.; Stratford, P.W.; Solomon, P.E.; Wishart, L.R. The evaluation of change in pain intensity: A comparison of the P4 and single-item numeric pain rating scales. J. Orthop. Sports Phys. Ther. 2004, 34, 187–193. [Google Scholar] [CrossRef]
- Cámara-Lemarroy, C.R.; Guzmán-de la Garza, F.J.; Fernández-Garza, N.E. Molecular inflammatory mediators in peripheral nerve degeneration and regeneration. Neuroimmunomodulation 2010, 17, 314–324. [Google Scholar] [CrossRef]
- Inoue, H.; Saito, I.; Nakazawa, R.; Mukaida, N.; Matsushima, K.; Azuma, N.; Suzuki, M.; Miyasaka, N. Expression of inflammatory cytokines and adhesion molecules in haemodialysis-associated amyloidosis. Nephrol. Dial. Transplant. 1995, 10, 2077–2082. [Google Scholar]
- Deger, A.N.; Deger, H.; Taser, F. The role of neoangiogenesis and vascular endothelial growth factor in the development of carpal tunnel syndrome in patients with diabetes. Niger. J. Clin. Pract. 2016, 19, 189–195. [Google Scholar] [CrossRef] [Green Version]
- Donato, G.; Galasso, O.; Valentino, P.; Conforti, F.; Zuccalà, V.; Russo, E.; Maltese, L.; Perrotta, I.; Tripepi, S.; Amorosi, A. Pathological findings in subsynovial connective tissue in idiopathic carpal tunnel syndrome. Clin. Neuropathol. 2009, 28, 129–135. [Google Scholar] [CrossRef]
- Freeland, A.E.; Tucci, M.A.; Barbieri, R.A.; Angel, M.F.; Nick, T.G. Biochemical evaluation of serum and flexor tenosynovium in carpal tunnel syndrome. Microsurgery 2002, 22, 378–385. [Google Scholar] [CrossRef] [PubMed]
- Hägg, O.; Fritzell, P.; Nordwall, A. The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur. Spine J. 2003, 12, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Bulut, T.; Sener, U.; Yağdi, S.; Kazimoğlu, C.; Sener, M. Relationship between clinical and electrophysiological results in surgically treated carpal tunnel syndrome. Eklem Hastalik. Ve Cerrahisi = Jt. Dis. Relat. Surg. 2011, 22, 140–144. [Google Scholar]
- Naranjo, A.; Ojeda, S.; Rúa-Figueroa, I.; Garcia-Duque, O.; Fernández-Palacios, J.; Carmona, L. Limited value of ultrasound assessment in patients with poor outcome after carpal tunnel release surgery. Scand. J. Rheumatol. 2010, 39, 409–412. [Google Scholar] [CrossRef]
- Kim, J.K.; Koh, Y.D.; Kim, J.O.; Choi, S.W. Changes in Clinical Symptoms, Functions, and the Median Nerve Cross-Sectional Area at the Carpal Tunnel Inlet after Open Carpal Tunnel Release. Clin. Orthop. Surg. 2016, 8, 298–302. [Google Scholar] [CrossRef]
- Ng, A.W.H.; Griffith, J.F.; Tsoi, C.; Fong, R.C.W.; Mak, M.C.K.; Tse, W.L.; Ho, P.C. Ultrasonography Findings of the Carpal Tunnel after Endoscopic Carpal Tunnel Release for Carpal Tunnel Syndrome. Korean J. Radiol. 2021, 22, 1132–1141. [Google Scholar] [CrossRef]
- Longstaff, L.; Milner, R.H.; O’sullivan, S.; Fawcett, P. Carpal tunnel syndrome: The correlation between outcome, symptoms and nerve conduction study findings. J. Hand Surg. 2001, 26, 475–480. [Google Scholar] [CrossRef]
- Shi, D.D.; Balboni, T.A.; Krishnan, M.S.; Spektor, A.; Huynh, M.A.; Shiloh, R.Y.; Skamene, S.; Zaslowe-Dude, C.; Hertan, L.M. Quantitative-qualitative analyses of patient-reported pain response after palliative radiation therapy. Supportive Care Cancer Off. J. Multinatl. Assoc. Supportive Care Cancer 2021, 29, 3707–3714. [Google Scholar] [CrossRef]
| All Patients (n = 36) | Effective Outcome (n = 22) | Poor Outcome (n = 14) | ap Value | |
|---|---|---|---|---|
| Gender, n (%) | 0.217 | |||
| Female | 28 (77.8) | 19 (86.4) | 9 (64.3) | |
| Male | 8 (22.2) | 3 (13.6) | 5 (35.7) | |
| Age (year) ± SE (range) | 59.2 ± 1.6 (34–77) | 57.8 ± 1.9 (34–67) | 61.4 ± 2.7 (39–77) | 0.267 |
| BH (cm) ± SE (range) | 157.6 ± 1.0 (148–174) | 158.3 ± 1.5 (148–174) | 156.5 ± 1.3 (150–165) | 0.810 |
| BW (kg) ± SE (range) | 62.6 ± 1.9 (45–93) | 63.4 ± 2.8 (46–93) | 61.4 ± 2.4 (45–75) | 0.936 |
| DM (%) | 10 (27.8) | 6 (27.3) | 4 (28.6) | 0.932 |
| Hypertension (%) | 8 (22.2) | 6 (27.3) | 2 (14.3) | 0.441 |
| Lesion site, n (%) | 0.879 | |||
| Left | 16 (44.4) | 10 (45.5) | 6 (42.9) | |
| Right | 20 (55.6) | 12 (54.5) | 8 (57.1) | |
| Duration (month) ± SE (range) | 15.1 ± 2.4 (1–48) | 15.1 ± 3.1 (2–40) | 15.1 ± 4.1 (1–48) | 0.689 |
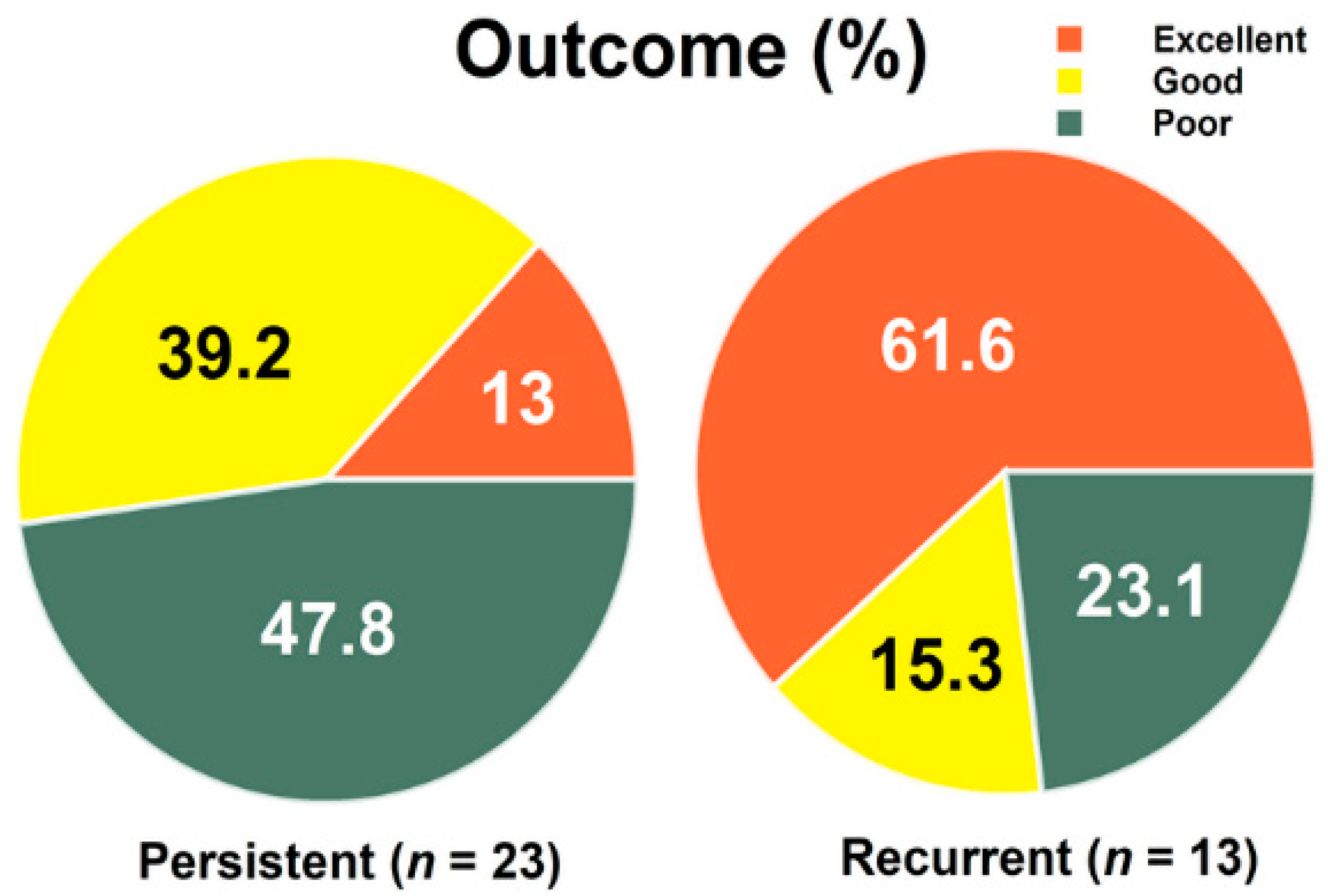
| Classification (%) | 0.175 | |||
| Persistent | 23 (63.9) | 12 (54.5) | 11 (78.6) | |
| Recurrent | 13 (36.1) | 10 (45.5) | 3 (21.4) | |
| CSA (mm2) (SE) | 14.1 ± 0.8 | 14.3 ± 1.2 | 13.6 ± 0.9 | 0.835 |
| No. of injection (SE) | 3.1 ± 0.3 | 3.1 ± 0.5 | 3.2 ± 0.5 | 0.597 |
| Other treatment, (%) | 11 (30.6) | 5 (22.7) | 6 (42.9) | 0.671 |
| Follow-up period (month), (SE) (range) | 33.0 ± 2.8 (6–67) | 35.9 ± 3.6 (7–67) | 28.5 ± 4.4 (6–55) | 0.160 |
| Persistent (n = 23) | Recurrence (n = 13) | ap Value | |
|---|---|---|---|
| Gender, n (%) | 0.682 | ||
| Female | 17 (73.9) | 11 (84.6) | |
| Male | 6 (26.1) | 2 (15.4) | |
| Age (year) ± SE (range) | 57.6 ± 2.3 (34–77) | 61.9 ± 1.2 (55–69) | 0.281 |
| BH (cm) ± SE (range) | 158.6 ± 0.9 (150–170) | 155.9 ± 2.3 (148–174) | 0.006 |
| BW (kg) ± SE (range) | 62.7 ± 1.6 (46–75) | 62.5 ± 4.7 (45–93) | 0.361 |
| DM (%) | 6 (26.1) | 4 (30.8) | 0.763 |
| Hypertension (%) | 4 (17.4) | 4 (30.8) | 0.422 |
| Lesion site, n (%) | 0.731 | ||
| Left | 11 (47.8) | 5 (38.5) | |
| Right | 12 (52.2) | 8 (61.5) | |
| Duration (month) ± SE (range) | 17.0 ± 3.3 (1–48) | 11.7 ± 3.2 (2–36) | 0.580 |
| CSA (mm2) (SE) | 13.9 ± 0.8 | 14.3 ± 1.9 | 0.474 |
| No. of injection (SE) | 3.2 ± 0.5 | 3.0 ± 0.4 | 0.845 |
| Outcome | 0.165 | ||
| Effective | 12 (52.2) | 10 (76.9) | |
| Poor | 11 (47.8) | 3 (23.1) | |
| Other treatment, (%) | 6 (26.1) | 5 (38.5) | 0.475 |
| Follow-up period, (months) (SE) (range) | 30.7 ± 3.1 (6–67) | 37.2 ± 5.5 (7–62) | 0.281 |
| <2 Years (n = 11) | 2–4 Years (n = 18) | >4 Years (n = 7) | ap Value | |
|---|---|---|---|---|
| Gender, n (%) | 0.182 | |||
| Female | 7 (63.6) | 14 (77.8) | 7 (100) | |
| Male | 4 (36.4) | 4 (22.2) | 0 (0) | |
| Age (year) ± SE (range) | 59.5 ± 2.1 (48–77) | 57.8 ± 2.8 (34–75) | 62.3 ± 1.3 (56–66) | 0.454 |
| BH (cm) ± SE (range) | 157.1 ± 1.5 (148–165) | 159.4 ± 1.6 (150–174) | 153.6 ± 1.0 (150–157) | 0.810 |
| BW (kg) ± SE (range) | 63.0 ± 2.8 (45–75) | 64.7 ± 3.1 (46–93) | 56.6 ± 4.0 (45–76) | 0.936 |
| DM (%) | 1 (9.1) | 8 (44.4) | 1 (14.3) | 0.104 |
| Hypertension (%) | 2 (18.2) | 6 (33.3) | 0 (0) | 0.216 |
| Lesion site, n (%) | 0.903 | |||
| Left | 4 (36.4) | 9 (50.0) | 3 (42.9) | |
| Right | 7 (63.6) | 9 (50.0) | 4 (57.1) | |
| Duration (month) ± SE (range) | 10.4 ± 4.3 (1–48) | 12.7 ± 2.9 (2–38) | 28.6 ± 5.6 (12–48) | 0.016 |
| Classification (%) | 0.113 | |||
| Persistent | 7 (63.6) | 14 (77.8) | 2 (28.6) | |
| Recurrence | 4 (36.4) | 4 (22.2) | 5 (71.4) | |
| CSA (mm2) (SE) | 14.0 ± 1.1 | 15.1 ± 1.4 | 11.6 ± 1.0 | 0.414 |
| No. of injection (SE) | 3.7 ± 0.5 | 3.1 ± 0.5 | 2.3 ± 0.6 | 0.206 |
| Outcome | 0.077 | |||
| Effective | 4 (36.4) | 14 (77.8) | 4 (57.1) | |
| Poor | 7 (63.6) | 4 (22.2) | 3 (42.9) | |
| Other treatment, (%) | 2 (18.2) | 7 (38.9) | 2 (28.6) | 0.640 |
| Follow-up period (months) (SE) (range) | 14.6 ± 2.1 (6–23) | 35.1 ± 2.0 (25–47) | 56.7 ± 2.6 (50–67) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chao, T.-C.; Reeves, K.D.; Lam, K.H.S.; Li, T.-Y.; Wu, Y.-T. The Effectiveness of Hydrodissection with 5% Dextrose for Persistent and Recurrent Carpal Tunnel Syndrome: A Retrospective Study. J. Clin. Med. 2022, 11, 3705. https://doi.org/10.3390/jcm11133705
Chao T-C, Reeves KD, Lam KHS, Li T-Y, Wu Y-T. The Effectiveness of Hydrodissection with 5% Dextrose for Persistent and Recurrent Carpal Tunnel Syndrome: A Retrospective Study. Journal of Clinical Medicine. 2022; 11(13):3705. https://doi.org/10.3390/jcm11133705
Chicago/Turabian StyleChao, Ta-Chung, Kenneth Dean Reeves, King Hei Stanley Lam, Tsung-Ying Li, and Yung-Tsan Wu. 2022. "The Effectiveness of Hydrodissection with 5% Dextrose for Persistent and Recurrent Carpal Tunnel Syndrome: A Retrospective Study" Journal of Clinical Medicine 11, no. 13: 3705. https://doi.org/10.3390/jcm11133705








