Postoperative Pain Following Root Canal Instrumentation Using ProTaper Next or Reciproc in Asymptomatic Molars: A Randomized Controlled Single-Blind Clinical Trial
Abstract
:1. Introduction
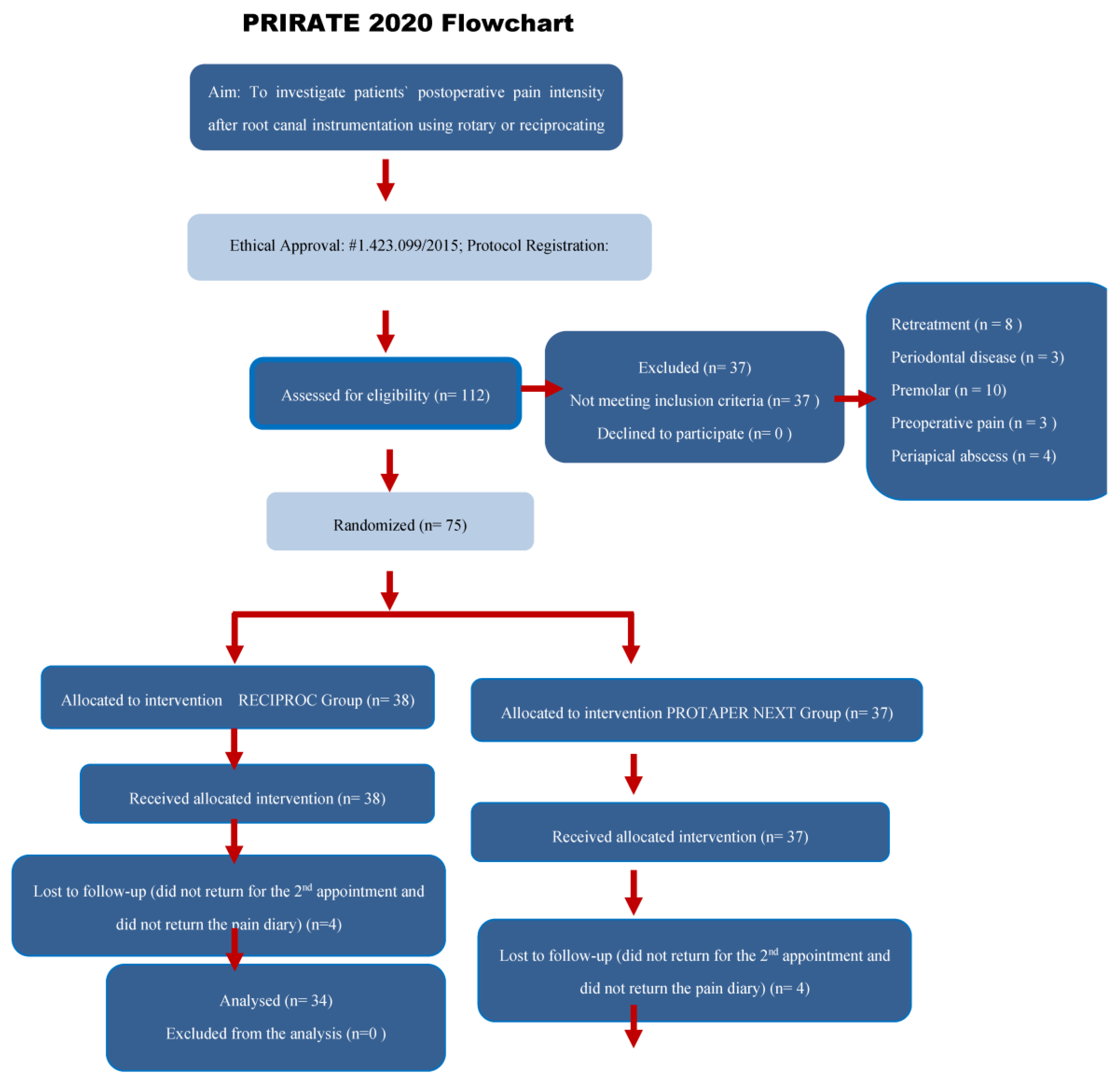
2. Materials and Methods
2.1. Study Design, Setting and Sampling
2.2. Sample Size Calculation
2.3. Eligibility Criteria, Patient Selection and Allocation
2.4. Root Canal Treatment Procedures
- Rotary instrumentation group (PTN): Speed was set at 300 rpm and torque at 2 N/cm. X1 was initially used for cervical preparation, and X1 and X2 reached the WL, using in-and-out movements. X3 was used as a master apical file in narrow canals and X4 in large canals.
- Reciprocating instrumentation group (R): R was operated in “Reciproc All” mode. R25 was used in narrow canals, and R40 was used in large canals. Three in-and-out motions were applied with stroke lengths not exceeding 3 mm in the cervical, middle and apical thirds until attaining the established WL.
2.5. Postoperative Pain, Intake of Analgesic and Tenderness on Biting Assessments
2.6. Statistical Analysis
3. Results
4. Discussion
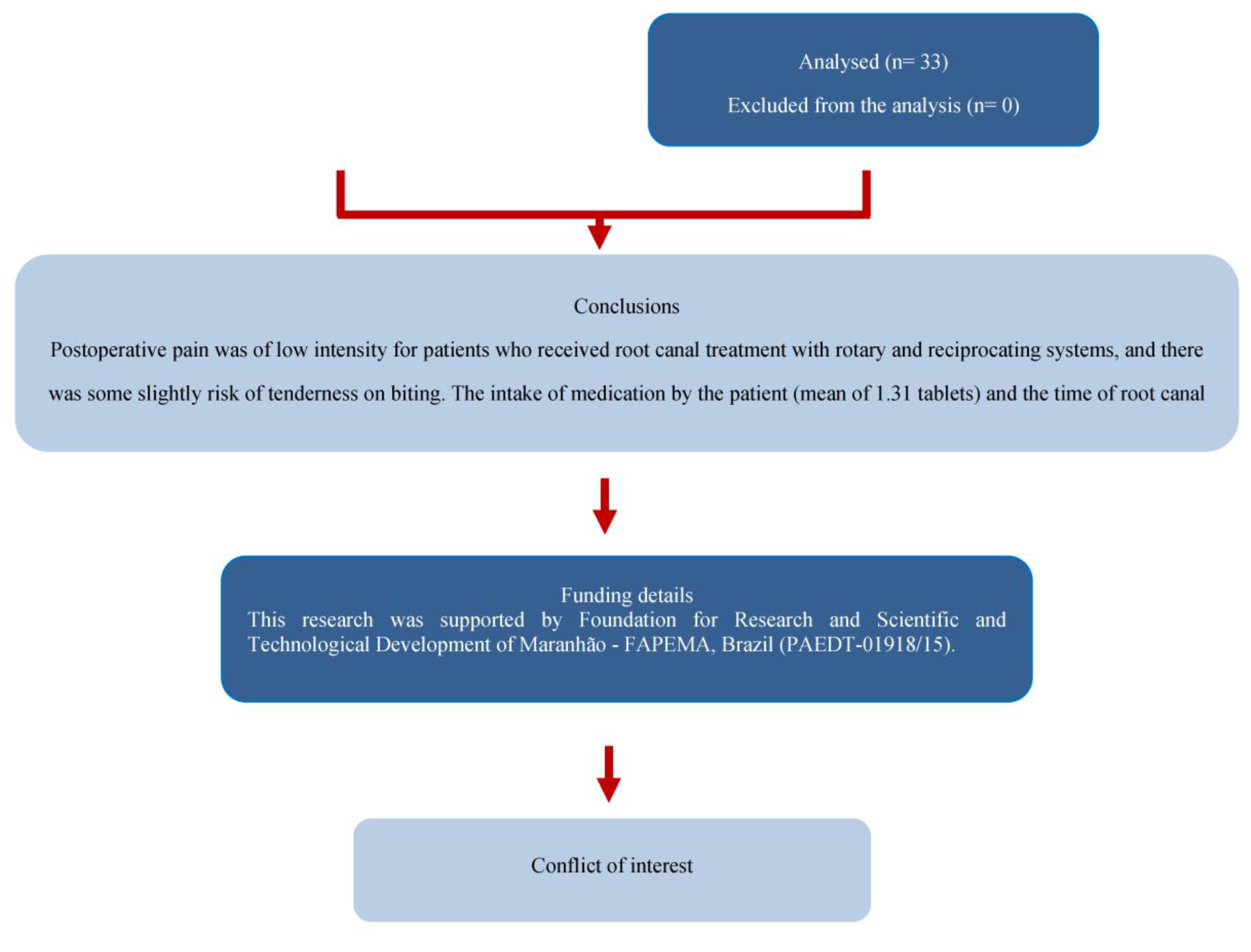
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gondim, E., Jr.; Setzer, F.C.; Dos Carmo, C.B.; Kim, S. Postoperative pain after the application of two different irrigation devices in a prospective randomized clinical trial. J. Endod. 2010, 36, 1295–1301. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kherlakian, D.; Cunha, R.S.; Ehrhardt, I.C.; Zuolo, M.L.; Kishen, A.; da Silveira Bueno, C.E. Comparison of the incidence of postoperative pain after using 2 reciprocating systems and a continuous rotary system: A prospective randomized clinical trial. J. Endod. 2016, 42, 171–176. [Google Scholar] [CrossRef] [PubMed]
- Relvas, J.B.; Bastos, M.M.; Marques, A.A.; Garrido, A.D.; Sponchiado, E.C., Jr. Assessment of postoperative pain after reciprocating or rotary NiTi instrumentation of root canals: A randomized, controlled clinical trial. Clin. Oral Investig. 2016, 20, 1987–1993. [Google Scholar] [CrossRef] [PubMed]
- Arslan, H.; Khalilov, R.; Doğanay, E.; Karatas, E. The effect of various kinematics on postoperative pain after instrumentation: A prospective, randomized clinical study. J. Appl. Oral Sci. 2016, 24, 503–508. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Glennon, J.P.; Ng, Y.L.; Setchell, D.J.; Gulabivala, K. Prevalence of and factors affecting postpreparation pain in patients undergoing two-visit root canal treatment. Int. Endod. J. 2004, 37, 29–37. [Google Scholar] [CrossRef]
- Sinatra, R. Causes and consequences of inadequate management of acute pain. Pain Med. 2010, 11, 1859–1871. [Google Scholar] [CrossRef] [Green Version]
- Pak, J.G.; White, S.N. Pain prevalence and severity before, during, and after root canal treatment: A systematic review. J. Endod. 2011, 37, 429–438. [Google Scholar] [CrossRef]
- Mostafa, M.; El-Shrief, Y.; Anous, W.; Hassan, M.W.; Salamah, F.T.A.; el Boghdadi, R.M.; El-Bayoumi, M.A.A.; Seyam, R.M.; Abd-El-Kader, K.G.; Amin, S.A.W. Postoperative pain following endodontic irrigation using 1.3% versus 5.25% sodium hypochlorite in mandibular molars with necrotic pulps: A randomized double-blind clinical trial. Int. Endod. J. 2020, 53, 154–166. [Google Scholar] [CrossRef]
- Neelakantan, P.; Sharma, S. Pain after single-visit root canal treatment with two single-file systems based on different kinematics—A prospective randomized multicenter clinical study. Clin. Oral Investig. 2015, 19, 2211–2217. [Google Scholar] [CrossRef]
- Sipavičiūtė, E.; Manelienė, R. Pain and flare-up after endodontic treatment procedures. Stomatologija 2014, 16, 25–30. [Google Scholar]
- Seltzer, S.; Naidorf, I.J. Flare-ups in endodontics: I. Etiological factors. 1985. J. Endod. 2004, 30, 475–476. [Google Scholar] [CrossRef] [PubMed]
- Siqueira, J.F., Jr.; Rôças, I.N.; Favieri, A.; Machado, A.G.; Gahyva, S.M.; Oliveira, J.C.M.; Abad, C.E. Incidence of postoperative pain after intracanal procedures based on an antimicrobial strategy. J. Endod. 2002, 28, 457–460. [Google Scholar] [CrossRef] [PubMed]
- Bürklein, S.; Benten, S.; Schäfer, E. Quantitative evaluation of apically extruded debris with different single-file systems: Reciproc, F360 and OneShape versus Mtwo. Int. Endod. J. 2014, 47, 405–409. [Google Scholar] [CrossRef] [PubMed]
- Nekoofar, M.H.; Sheykhrezae, M.S.; Meraji, N.; Jamee, A.; Shirvani, A.; Jamee, J.; Dummer, P. Comparison of the effect of root canal preparation by using WaveOne and ProTaper on postoperative pain: A randomized clinical trial. J. Endod. 2015, 41, 575–578. [Google Scholar] [CrossRef] [PubMed]
- Çapar, I.D.; Arslan, H.; Akcay, M.; Ertas, H. An in vitro comparison of apically extruded debris and instrumentation times with ProTaper Universal, ProTaper Next, Twisted File Adaptive, and HyFlex instruments. J. Endod. 2014, 40, 1638–1641. [Google Scholar] [CrossRef] [PubMed]
- Silva, E.J.N.L.; Sá, L.; Belladonna, F.; Neves, A.; Accorsi-Mendonça, T.; Vieira, V.; De-Deus, G.; Moreira, E.J. Reciprocating versus rotary systems for root filling removal: Assessment of the apically extruded material. J. Endod. 2014, 40, 2077–2080. [Google Scholar] [CrossRef]
- Dincer, A.; Er, O.; Canakci, B.C. Evaluation of apically extruded debris during root canal retreatment with several NiTi systems. Int. Endod. J. 2015, 48, 1194–1198. [Google Scholar] [CrossRef]
- Uzunoglu, E.; Turker, S.A. Impact of different file systems on the amount of apically extruded debris during endodontic retreatment. Eur. J. Dent. 2016, 10, 210–214. [Google Scholar] [CrossRef]
- Çanakçi, B.C.; Ustun, Y.; Er, O.; Genc Sen, O. Evaluation of apically extruded debris from curved root canal filling removal using 5 nickel-titanium systems. J. Endod. 2016, 42, 1101–1104. [Google Scholar] [CrossRef]
- Ahn, S.Y.; Kim, H.C.; Kim, E. Kinematic effects of nickel-titanium instruments with reciprocating or continuous rotation motion: A systematic review of in vitro studies. J. Endod. 2016, 42, 1009–1017. [Google Scholar] [CrossRef]
- Chen, Y.L.; Yang, K.H. Consort 2010. Lancet 2010, 376, 230. [Google Scholar] [CrossRef]
- Nagendrababu, V.; Duncan, H.F.; Bjørndal, L.; Kvist, T.; Priya, E.; Jayaraman, J.; Pulikkotil, S.J.; Dummer, P.M.H. PRIRATE 2020 guidelines for reporting randomized trials in Endodontics: Explanation and Elaboration. Int. Endod. J. 2020, 53, 774–803. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buchanan, L.S. Management of the curved root canal. J. Calif. Dent. Assoc. 1989, 17, 18–27. [Google Scholar] [PubMed]
- Elzaki, W.M.; Abubakr, N.H.; Ziada, H.M.; Ibrahim, Y.E. Double-blind randomized placebo-controlled clinical trial of efficiency of nonsteroidal anti-inflammatory drugs in the control of post-endodontic pain. J. Endod. 2016, 42, 835–842. [Google Scholar] [CrossRef]
- Keskin, C.; Sivas Yilmaz, Ö.; Inan, U.; Özdemir, Ö. Postoperative pain after glide path preparation using manual, reciprocating and continuous rotary instruments: A randomized clinical trial. Int. Endod. J. 2019, 52, 579–587. [Google Scholar] [CrossRef]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef]
- Kuştarci, A.; Akpinar, K.E.; Er, K. Apical extrusion of intracanal debris and irrigant following use of various instrumentation techniques. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2008, 105, 257–262. [Google Scholar] [CrossRef]
- Ferraz, C.C.; Gomes, N.V.; Gomes, B.P.; Zaia, A.A.; Teixeira, F.B.; Souza-Filho, F.J. Apical extrusion of debris and irrigants using two hand and three engine-driven instrumentation techniques. Int. Endod. J. 2001, 34, 354–358. [Google Scholar] [CrossRef]
- Comparin, D.; Moreira, E.J.L.; Souza, E.M.; De-Deus, G.; Arias, A.; Silva, E.J.N.L. Postoperative Pain after Endodontic Retreatment Using Rotary or Reciprocating Instruments: A Randomized Clinical Trial. J. Endod. 2017, 43, 1084–1088. [Google Scholar] [CrossRef]
- Genet, J.M.; Hart, A.A.M.; Wesselink, P.R.; Thoden van Velzen, S.K. Preoperative and operative factors associated with pain after the first visit. Int. Endod. J. 1987, 20, 53–54. [Google Scholar] [CrossRef]
- Arias, A.; de la Macorra, J.C.; Hidalgo, J.J.; Azabal, M. Predictive models of pain following root canal treatment: A prospective clinical study. Int. Endod. J. 2013, 46, 784–793. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Younger, J.; McCue, R.; Mackey, S. Pain outcomes: A brief review of instruments and techniques. Curr. Pain Headache Rep. 2009, 13, 39–43. [Google Scholar] [CrossRef] [PubMed]
- Calderon, P.D.S.; Peixoto, R.F.; Gomes, V.M.; Corrêa, A.S.D.M.; De Alencar, E.N.; Rossetti, L.M.N.; Conti, P.C.R. Concordance among different pain scales in patients with dental pain. J. Orofac. Pain 2012, 26, 126–131. [Google Scholar]
- Jensen, M.P.; Castarlenas, E.; Roy, R.; Pires, C.T.; Racine, M.; Pathak, A.; Miró, J. The utility and construct validity of four measures of pain intensity: Results from a University-based study in Spain. Pain Med. 2019, 20, 2411–2420. [Google Scholar] [CrossRef]
- Abdulrab, S.; Rodrigues, J.C.; Al-Maweri, S.A.; Halboub, E.; Alqutaibi, A.Y.; Alhadainy, H. Effect of Apical Patency on Postoperative Pain: A Meta-analysis. J. Endod. 2018, 44, 1467–1473. [Google Scholar] [CrossRef]
| Rotary (PTN) | Reciprocating (R) | p-Value | ||
|---|---|---|---|---|
| n (%) | n (%) | |||
| Patient’s gender | Male | 16 (48.5) | 11 (32.4) | 0.178 * |
| Female | 17 (51.5) | 23 (67.6) | ||
| Tooth location | Maxillary Molar | 12 (36.4) | 9 (26.5) | 0.383 * |
| Mandibular Molar | 21 (63.6) | 25 (73.5) | ||
| Number of canals | 2 | 3 (9.1) | 1 (2.9) | 0.764 ** |
| 3 | 24 (72.7) | 30 (88.2) | ||
| 4 | 6 (18.2) | 3 (8.8) | ||
| Mean (SD) | Mean (SD) | |||
| Patient’s age | 31.12 ± 6.59 | 32.09 ± 11.10 | 0.559 § | |
| Instrumentation time (min) | 13.21 ± 9.13 | 10.62 ± 4.30 | 0.536 § | |
| Number of analgesics taken | 1.30 ± 2.88 | 1.32 ± 2.80 | 0.988 § |
| Scale | Group | 6 h | 12 h | 24 h | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 | Day 7 | p * |
|---|---|---|---|---|---|---|---|---|---|---|---|
| VAS | Rotary (PTN) § | 1.41 ± 2.35 a (0.52–2.31) | 1.28 ± 2.05 a (0.50–2.06) | 1.14 ± 1.36 a (0.62–1.65) | 1.10 ± 1.32 a (0.60–1.61) | 1.10 ± 1.42 a (0.56–1.64) | 1.03 ± 1.84 a (0.33–1.74) | 0.52 ± 0.91 b (0.17–0.86) | 0.21 ± 0.62 c (−0.03–0.44) | 0.14 ± 0.52 c (−0.06–0.33) | <0.001 |
| Reciprocating (R) § | 1.00 ± 1.56 a (0.34–1.66) | 0.96 ± 1.62 a (0.29–1.70) | 0.71 ± 1.30 a (0.16–1.26) | 0.71 ± 1.16 a (0.22–1.20) | 0.54 ± 1.02 a (0.11–0.97) | 0.42 ± 0.97 a (0.01–0.83) | 0.25 ± 0.74 a (−0.06–0.56) | 0.21±0.59 a (−0.04–0.46) | 0.08 ± 0.41 a (−0.09–0.26) | 0.001 | |
| p ** | 0.795 | 0.903 | 0.082 | 0.146 | 0.052 | 0.115 | 0.193 | 0.845 | 0.672 | ||
| d | 0.21 | 0.17 | 0.32 | 0.31 | 0.45 | 0.41 | 0.33 | 0.00 | 0.13 | ||
| NRS | Rotary (PTN) § | 1.48 ± 2.4 a (0.57–2.40) | 1.45 ± 2.20 a (0.61–2.28) | 1.41 ± 1.62 a (0.80–2.03) | 1.31 ± 1.61 a (0.70–1.92) | 1.45 ± 1.94 a (0.71–2.19) | 1.07 ± 2.05 a (0.29–1.85) | 0.41 ± 0.83 b (0.10–0.73) | 0.28 ± 0.75 b (−0.01–0.56) | 0.17 ± 0.54 b (−0.03–0.38) | <0.001 |
| Reciprocating (R) § | 1.13 ± 1.78 a (0.37–1.88) | 1.33 ± 1.76 a (0.59–2.08) | 0.92 ± 1.47 a (0.30–1.54) | 0.96 ± 1.40a (0.37–1.55) | 0.88 ± 1.30 a (0.33–1.42) | 0.42 ± 0.93 b (0.02–0.81) | 0.46 ± 1.06 b (0.01–0.91) | 0.25 ± 0.61 b (−0.01–0.51) | 0.17 ± 0.48 b (−0.04–0.37) | 0.002 | |
| p ** | 0.983 | 0.770 | 0.094 | 0.304 | 0.188 | 0.228 | 0.845 | 0.841 | 0.845 | ||
| d | 0.17 | 0.06 | 0.32 | 0.23 | 0.35 | 0.41 | −0.05 | 0.04 | 0 |
| Group | p-Value | Absolute Risk (95% CI) | Relative Risk (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| Primary Outcome | No | Yes | |||||
| Number of patients who experienced postoperative pain | Rotary (PTN) Reciprocating (R) | 19 21 | 14 13 | 0.727 § | 0.10 (0.71–0.97) 0.41 (0.67–0.92) | 1.33 (0.48–3.71) | |
| Secondary Outcome | Number of patients who experienced tenderness on biting | Rotary (PTN) Reciprocating (R) | 29 25 | 4 9 | 0.217 δ | 0.12 (0.05–0.27) 0.26 (0.67–0.92) | 0.32 (0.08–1.32) |
| Postoperative Pain | ||||||
|---|---|---|---|---|---|---|
| Independent variables | NO n (%) | YES n (%) | RR (95% CI) | p | RR-Adjusted (95% CI) | p |
| Gender | 0.278 | 0.187 | ||||
| Male | 14 (35) | 13 (48.1) | 1.40 (0.77–2.45) | 1.46 (0.83–2.57) | ||
| Female | 26 (65) | 14 (51.9) | 1 | 1 | ||
| Oral hygiene status | 0.921 0.015 | 0.424 0.012 | ||||
| Poor | 2 (5.0) | 3(11.1) | 0.96 (0.43–2.16) | 0.73 (0.34–1.57) | ||
| Moderate | 32 (80.0) | 14 (51.9) | 0.49 (0.27–0.87) | 0.48 (0.27–0.85) | ||
| Good | 6 (15.0) | 10 (37) | 1 | 1 | ||
| Tooth location | 0.041 | 0.085 | ||||
| Mandibular | 23 (57.5) | 23 (85.2) | 2.63 (1.04–6.64) | 2.33 (0.89–6.11) | ||
| Maxillary | 17 (42.5) | 4 (14.8) | 1 | 1 | ||
| Instrumentation technique | 0.727 | 0.88 (0.49–1.58) | 0.668 | |||
| R | 21 (52.5) | 13 (48.1) | 0.90 (0.50–1.62) | |||
| PTN | 19 (47.5) | 14 (451.9) | 1 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oliveira, P.S.; Ferreira, M.C.; Paula, N.G.N.; Loguercio, A.D.; Grazziotin-Soares, R.; da Silva, G.R.; da Mata, H.C.S.; Bauer, J.; Carvalho, C.N. Postoperative Pain Following Root Canal Instrumentation Using ProTaper Next or Reciproc in Asymptomatic Molars: A Randomized Controlled Single-Blind Clinical Trial. J. Clin. Med. 2022, 11, 3816. https://doi.org/10.3390/jcm11133816
Oliveira PS, Ferreira MC, Paula NGN, Loguercio AD, Grazziotin-Soares R, da Silva GR, da Mata HCS, Bauer J, Carvalho CN. Postoperative Pain Following Root Canal Instrumentation Using ProTaper Next or Reciproc in Asymptomatic Molars: A Randomized Controlled Single-Blind Clinical Trial. Journal of Clinical Medicine. 2022; 11(13):3816. https://doi.org/10.3390/jcm11133816
Chicago/Turabian StyleOliveira, Patrícia Santos, Meire Coelho Ferreira, Natália Gomes Nascimento Paula, Alessandro Dourado Loguercio, Renata Grazziotin-Soares, Gisele Rodrigues da Silva, Helena Cristina Santos da Mata, José Bauer, and Ceci Nunes Carvalho. 2022. "Postoperative Pain Following Root Canal Instrumentation Using ProTaper Next or Reciproc in Asymptomatic Molars: A Randomized Controlled Single-Blind Clinical Trial" Journal of Clinical Medicine 11, no. 13: 3816. https://doi.org/10.3390/jcm11133816
APA StyleOliveira, P. S., Ferreira, M. C., Paula, N. G. N., Loguercio, A. D., Grazziotin-Soares, R., da Silva, G. R., da Mata, H. C. S., Bauer, J., & Carvalho, C. N. (2022). Postoperative Pain Following Root Canal Instrumentation Using ProTaper Next or Reciproc in Asymptomatic Molars: A Randomized Controlled Single-Blind Clinical Trial. Journal of Clinical Medicine, 11(13), 3816. https://doi.org/10.3390/jcm11133816








