Immersive Virtual Reality as a Novel Physical Therapy Approach for Nonagenarians: Usability and Effects on Balance Outcomes of a Game-Based Exercise Program
Abstract
:1. Introduction
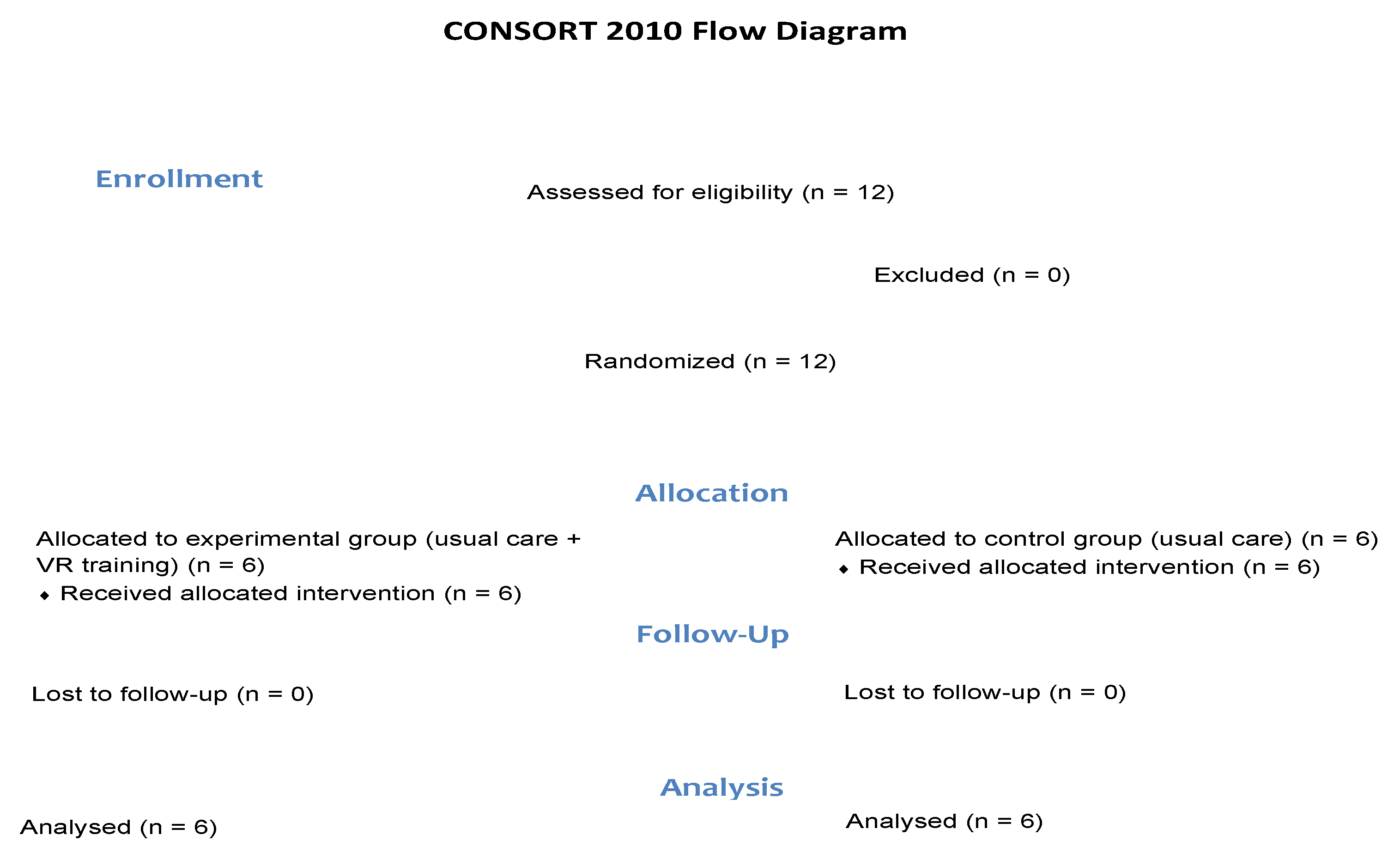
2. Materials and Methods
2.1. Participants
2.2. Intervention
2.3. Assessments
2.4. Statistical Analysis
3. Results
4. Discussion
4.1. Limitations
4.2. Implications of Using Immersive Virtual Reality in Clinical Practice
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Active Ageing: A Policy Framework. 2002. Available online: https://apps.who.int/iris/handle/10665/67215 (accessed on 25 April 2022).
- World Health Organization. World Report on Ageing and Health. 2015. Available online: https://apps.who.int/iris/handle/10665/186463 (accessed on 25 April 2021).
- Harmell, A.L.; Jeste, D.; Depp, C. Strategies for successful aging: A research update. Curr. Psychiatry Rep. 2014, 6, 476. [Google Scholar] [CrossRef] [Green Version]
- Ayers, E.; Barzilai, N.; Crandall, J.P.; Milman, S.; Verghese, J. Association of exceptional parental longevity and physical function in aging. Age 2014, 36, 9677. [Google Scholar] [CrossRef] [Green Version]
- Gopinath, B.; Kifley, A.; Flood, V.M.; Mitchell, P. Physical activity as a determinant of successful aging over ten years. Sci. Rep. 2018, 8, 10522. [Google Scholar] [CrossRef]
- Lagerros, Y.T.; Hantikainen, E.; Michaelsson, K.; Ye, W.; Adami, H.O.; Bellocco, R. Physical activity and the risk of hip fracture in the elderly: A prospective cohort study. Eur. J. Epidemiol. 2017, 32, 983–991. [Google Scholar] [CrossRef]
- Park, J.; Yim, J. A new approach to improve cognition, muscle strength, and postural balance in community-dwelling elderly with a 3-D virtual reality kayak program. Tohoku J. Exp. Med. 2016, 238, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Preschl, B.; Wagner, B.; Forstmeier, S.; Maercker, A. E-health interventions for depression, anxiety disorder, dementia, and other disorders in old age: A review. J. CyberTherapy Rehabil. 2011, 4, 371–386. [Google Scholar]
- Jones, T.S.; Ghosh, T.S.; Horn, K.; Smith, J.; Vogt, R.L. Primary care physicians’ perceptions and practices regarding fall prevention in adult’s 65 years and over. Accid Anal Prev. 2011, 43, 1605–1609. [Google Scholar] [CrossRef] [PubMed]
- Stevens, J.A.; Corso, P.S.; Finkelstein, E.A.; Miller, T.R. The costs of fatal and non-fatal falls among older adults. Inj. Prev. 2006, 12, 290–295. [Google Scholar] [CrossRef] [Green Version]
- Wetmore, S.J.; Eibling, D.E.; Goebel, J.A.; Gottshall, K.R.; Hoffer, M.E.; Magnusson, M.; Raz, Y. Challenges and opportunities in managing the dizzy older adult. Otolaryngol. Head Neck Surg. 2011, 144, 651–656. [Google Scholar] [CrossRef]
- Granacher, U.; Muehlbauer, T.; Gruber, M. A qualitative review of balance and strength performance in healthy older adults: Impact for testing and training. J. Aging Res. 2012, 2012, 708905. [Google Scholar] [CrossRef] [PubMed]
- Howe, T.E.; Rochester, L.; Jackson, A.; Banks, P.M.H.; Blair, V.A. Exercise for improving balance in older people. Cochrane Database Syst. Rev. 2007, 4, CD004963. [Google Scholar]
- Gillespie, L.D.; Robertson, M.C.; Gillespie, W.J.; Sherrington, C.; Gates, S.; Clemson, L.; Lamb, S.E. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012, 9, CD007146. [Google Scholar]
- Hernández-Vicente, A.; Santos-Lozano, A.; Mayolas-Pi, C.; Rodríguez-Romo, G.; Pareja-Galeano, H.; Bustamante, N.; Gómez-Trullén, E.M.; Lucia, A.; Garatachea, N. Physical Activity and Sedentary Behavior at the End of the Human Lifespan. J. Aging Phys. Act. 2019, 27, 899–905. [Google Scholar] [CrossRef] [PubMed]
- Christensen, K.; Doblhammer, G.; Rau, R.; Vaupel, J.W. Ageing populations: The challenges ahead. Lancet 2009, 374, 1196–1208. [Google Scholar] [CrossRef] [Green Version]
- Fabre, J.M.; Wood, R.H.; Cherry, K.E.; Su, J.L.; Cress, E.M.; King, C.M.; King, C.; de Veer, M.; Ellis, R.; Jazwinski, M.S. Age-related deterioriation in flexibility is associated with health-related quality of life in nonagenarians. J. Geriatr. Phys. Ther. 2007, 30, 16–22. [Google Scholar] [CrossRef] [Green Version]
- Crespo, A.B.; Idrovo, G.G.; Rodrigues, N.; Pereira, A.A. Virtual reality UAV simulation with body area networks to promote the elder’s life quality. In Proceedings of the International Conference on Technology and Innovation in Sports, Health and Wellbeing (TISHW), Vila Real, Portugal, 1–3 December 2016; pp. 1–7. [Google Scholar]
- Tsatsis, C.G.; Rice, K.E.; Protopopova, V.; Ramos, D.; Jadav, J.; Coppola, J.F.; Broderick, M.; Putrino, D. Lateropulsion rehabilitation using virtual reality for stroke patients. In Proceedings of the Long Island Systems, Applications and Technology Conference (LISAT), Farmingdale, NY, USA, 5 May 2017; pp. 1–6. [Google Scholar]
- Rosa, P.J.; Morais, D.; Gamito, P.; Oliveira, J.; Saraiva, T. The immersive virtual reality experience: A typology of users revealed through multiple correspondence analysis combined with cluster analysis technique. Cyberpsychol. Behav. Soc. Netw. 2016, 19, 209–216. [Google Scholar] [CrossRef]
- Liu, W.; Zeng, N.; Pope, Z.C.; McDonough, D.J.; Gao, Z. Acute effects of immersive virtual reality exercise on young adults’ situational motivation. J. Clin. Med. 2019, 8, 1947. [Google Scholar] [CrossRef] [Green Version]
- Campo-Prieto, P.; Cancela, J.M.C.; Rodríguez-Fuentes, G. Immersive virtual reality as physical therapy in older adults: Present or future (systematic review). Virtual Real. 2021, 25, 1–17. [Google Scholar] [CrossRef]
- Gao, Z.; Lee, J.E.; McDonough, D.J.; Albers, C. Virtual Reality Exercise as a Coping Strategy for Health and Wellness Promotion in Older Adults during the COVID-19 Pandemic. J. Clin. Med. 2020, 9, 1986. [Google Scholar] [CrossRef]
- Celnik, P.; Stefan, K.; Hummel, F.; Duque, J.; Classen, J.; Cohen, L.G. Encoding a motor memory in the older adult by action observation. Neuroimage 2006, 29, 677–684. [Google Scholar] [CrossRef]
- Miller, K.J.; Adair, B.S.; Pearce, A.J.; Said, C.M.; Ozanne, E.; Morris, M.M. Effectiveness and feasibility of virtual reality and gaming system use at home by older adults for enabling physical activity to improve health-related domains: A systematic review. Age Ageing 2014, 43, 188–195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laufer, Y.; Dar, G.; Kodesh, E. Does a Wii-based exercise program enhance balance control of independently functioning older adults? A systematic review. Clin. Interv. Aging 2014, 9, 1803–1813. [Google Scholar] [CrossRef] [Green Version]
- De Oliveira, J.A.; Guaratto, T.F.; Bacha JM, R.; Evangelista, R.A.; Bocalini, D.S.; Greve, J.M.D.A.; Alonso, A.C. Virtual reality in the rehabilitation of the balance in the elderly. Man. Ther. Posturology Rehabil. J. 2017, 15, 1–5. [Google Scholar] [CrossRef] [Green Version]
- Alhasan, H.; Hood, V.; Mainwaring, F. The effect of visual biofeedback on balance in elderly population: A systematic review. Clin. Interv. Aging 2017, 12, 487–497. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cacciata, M.; Stromberg, A.; Lee, J.-A.; Sorkin, D.; Lombardo, D.; Clancy, S.; Nyamathi, A.; Evangelista, L.S. Effect of exergaming on health-related quality of life in older adults: A systematic review. Int. J. Nurs. Stud. 2019, 93, 30–40. [Google Scholar] [CrossRef] [PubMed]
- Miller, K.J.; Suárez-Iglesias, D.; Varela, S.; Rodríguez, D.; Ayán, C. Exercise for Nonagenarians: A Systematic Review. J. Geriatr. Phys. Ther. 2020, 43, 208–218. [Google Scholar] [CrossRef]
- Campo-Prieto, P.; Carral, J.M.C.; Oliveira, I.; Rodríguez-Fuentes, G. Immersive virtual reality in older people: A case study. Retos 2021, 39, 1001–1005. [Google Scholar]
- Campo-Prieto, P.; Rodríguez-Fuentes, G.; Cancela-Carral, J.M. Immersive Virtual Reality Exergame Promotes the Practice of Physical Activity in Older People: An Opportunity during COVID-19. Mutimodal. Technol. Interact. 2021, 5, 52. [Google Scholar] [CrossRef]
- Mora, J.C.; Valencia, W.M. Exercise and Older Adults. Clin. Geriatr. Med. 2017, 34, 145–162. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Williams, T.F.; Mayewski, R. Fall risk index for elderly patients based on number of chronic disabilities. Am. J. Med. 1986, 80, 429–434. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Campo-Prieto, P.; Rodríguez-Fuentes, G.; Cancela-Carral, J.M. Translation and cross-cultural adaptation to Spanish of the Simulator Sickness Questionnaire. Retos 2021, 43, 503–509. [Google Scholar] [CrossRef]
- Brooke, J. SUS: A quick and dirty usability scale. Usability Eval. Ind. 1995, 189, 4–7. [Google Scholar]
- Kennedy, R.S.; Lane, N.E.; Berbaum, K.S.; Lilienthal, M.G. Simulator sickness questionnaire: An enhanced method for quantifying simulator sickness. Int. J. Aviat. Psychol. 1993, 3, 203–220. [Google Scholar] [CrossRef]
- Kennedy, R.S.; Drexler, J.; Kennedy, R.C. Research in visually induced motion sickness. Appl. Ergon. 2010, 41, 494–503. [Google Scholar] [CrossRef]
- Lawson, B.D.; Graeber, D.A.; Mead, A.M.; Muth, E.R. Signs and symptoms of human syndromes associated with synthetic experiences. In Handbook of Virtual Environments: Design, Implementation, and Applications; Hale, K.S., Stanney, K.M., Eds.; Lawrence Erlbaum Associates Publishers: Mahwah, NJ, USA, 2002; pp. 589–618. [Google Scholar]
- Aguilar, M.I.H.; Villegas, A.A.G. Comparative analysis of the system usability scale (SUS) in two versions. Rev. Iberoam. Cienc. Comput. Inf. 2016, 5, 44–58. [Google Scholar]
- Campo-Prieto, P.; Rodríguez-Fuentes, G.; Cancela-Carral, J.M. Can Immersive Virtual Reality Videogames Help Parkinson’s Disease Patients? A Case Study. Sensors 2021, 21, 4825. [Google Scholar] [CrossRef]
- World Health Organization. Women’s Mental Health: An Evidence-Based Review. 2000. Available online: https://apps.who.int/iris/handle/10665/66539 (accessed on 10 May 2022).
- United Nations. Department of Economic and Social Affairs. Population Dynamics. World Population Prospect. 2019. Available online: https://population.un.org/wpp/Download/Standard/Population/ (accessed on 10 May 2022).
- INE Statistics. Statistics National Institute of Spain. Demographic Basics Data. 2020. Available online: https://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736177003&menu=ultiDatos&idp=1254735573002 (accessed on 10 May 2022).
- Cobos, F.M.; Almendro, J.M.E. Envejecimiento activo y desigualdades de género. Aten. Primaria 2008, 40, 305–309. [Google Scholar] [CrossRef]
- Lesinski, M.; Hortobágyi, T.; Muehlbauer, T.; Gollhofer, A.; Granacher, U. Effects of Balance Training on Balance Performance in Healthy Older Adults: A Systematic Review and Meta-analysis. Sports Med. 2015, 45, 1721–1738. [Google Scholar] [CrossRef] [Green Version]
- Cancela, J.M.; Perez, C.A.; Rodrigues, L.P.; Bezerra, P. The Long-Term Benefits of a Multicomponent Physical Activity Program to Body Composition, Muscle Strength, Cardiorespiratory Capacity, and Bone Mineral Density in a Group of Nonagenarians. Rejuvenation Res. 2020, 23, 217–223. [Google Scholar] [CrossRef]
- Winter, C.; Kern, F.; Gall, D.; Latoschik, M.E.; Pauli, P.; Käthner, I. Immersive virtual reality during gait rehabilitation increases walking speed and motivation: A usability evaluation with healthy participants and patients with multiple sclerosis and stroke. J. Neuroeng. Rehabil. 2021, 18, 68. [Google Scholar] [CrossRef] [PubMed]
- Thapa, N.; Park, H.J.; Yang, J.G.; Son, H.; Jang, M.; Lee, J.; Kang, S.W.; Park, K.W.; Park, H. The Effect of a Virtual Reality-Based Intervention Program on Cognition in Older Adults with Mild Cognitive Impairment: A Randomized Control Trial. J. Clin. Med. 2020, 9, 1283. [Google Scholar] [CrossRef] [PubMed]
- Campo-Prieto, P.; Cancela-Carral, J.M.; Rodríguez-Fuentes, G. Wearable Immersive Virtual Reality Device for Promoting Physical Activity in Parkinson’s Disease Patients. Sensors 2022, 22, 3302. [Google Scholar] [CrossRef] [PubMed]



| Experimental Group (n = 6) | Control Group (n = 6) | |||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Age (years) | 91.67 | 1.63 | 90.83 | 2.64 |
| Height (m) | 1.51 | 0.03 | 1.45 | 0.07 |
| Weight (kg) | 61.65 | 14.32 | 54.87 | 9.87 |
| MEC | 27.66 | 2.87 | 24.45 | 1.56 |
| BMI (kg/m2) | 26.95 | 6.02 | 25.95 | 3.45 |
| Experimental Group (n = 6) | Control Group (n = 6) | Anova (2 × 2) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | % Improve | Wilcoxon Test | Pre | Post | % Improve | Wilcoxon Test | |||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||||||
| Tinettii test | Balance | 12.17 | 1.60 | 13.67 | 1.03 | 10.97 | Z = −3.503; Sig = 0.017 | 12.67 | 1.03 | 11.00 | 0.89 | −15.18 | Z = 3.371; Sig = 0.020 | H1,24 = 10.939; Sig = 0.004 |
| Walk | 9.83 | 1.94 | 10.83 | 0.98 | 9.23 | Z = −2.236; Sig = 0.047 | 8.83 | 2.14 | 8.67 | 1.37 | −1.84 | Z = −0.349; Sig = 0.741 | H1,24 = 0.731; Sig = 0.403 | |
| Total | 22.00 | 2.45 | 24.50 | 1.52 | 10.20 | Z = −3.727; Sig = 0.014 | 21.50 | 3.08 | 19.67 | 1.86 | −9.30 | Z = 2.101; Sig = 0.090 | H1,24 = 5.298; Sig = 0.032 | |
| Timed up and go test (TUG) | Sit to Stand | 2.60 | 1.36 | 3.49 | 2.76 | −25.50 | Z = −1.376; Sig = 0.227 | 5.99 | 1.94 | 7.19 | 4.26 | 16.68 | Z = −0.755; Sig = 0.484 | H1,24 = 0.018; Sig = 0.894 |
| Gait | 5.73 | 3.45 | 5.04 | 0.79 | 13.69 | Z = 0.505; Sig = 0.635 | 7.47 | 3.48 | 7.42 | 3.61 | 0.67 | Z = 0.023; Sig = 0.983 | H1,24 = 0.066; Sig = 0.801 | |
| Turning | 1.56 | 0.51 | 2.25 | 1.02 | −30.66 | Z = −2.023; Sig = 0.039 | 2.41 | 0.78 | 4.27 | 5.07 | −43.55 | Z = −2.005; Sig = 0.031 | H1,24 = 0.294; Sig = 0.594 | |
| Gait return | 5.58 | 3.73 | 5.07 | 3.59 | 10.05 | Z = 1.055; Sig = 0.340 | 6.46 | 2.99 | 6.73 | 1.78 | −4.01 | Z = −0.302; Sig = 0.775 | H1,24 = 0.093; Sig = 0.764 | |
| Stand to sit | 4.10 | 1.24 | 5.27 | 2.06 | −22.20 | Z = −2.236; Sig = 0.144 | 5.34 | 1.73 | 6.36 | 2.60 | −16.03 | Z = −0.930; Sig = 0.395 | H1,24 = 0.008; Sig = 0.931 | |
| Total | 19.56 | 8.95 | 19.65 | 8.94 | −0.45 | Z = −2.236; Sig = 0.917 | 27.67 | 8.33 | 32.47 | 10.42 | −14.78 | Z = −2.198; Sig = 0.079 | H1,24 = 0.393; Sig = 0.538 | |
| Mean | SD | |
|---|---|---|
| Simulation Sickness Questionnaire (SSQ) | ||
| Total Score | 0.00 | 0.00 |
| System Usability Scale (SUS) | ||
| 1. I think that I would like to use this system frequently. | 3.00 | 1.41 |
| 2. I found the system unnecessarily complex. | 2.50 | 1.22 |
| 3. I thought the system was easy to use. | 3.83 | 0.98 |
| 4. I think that I would need the support of a technical person to be able to use this system. | 2.00 | 1.67 |
| 5. I found the various functions in this system were well integrated. | 4.00 | 0.63 |
| 6. I thought there was too much inconsistency in this system. | 3.33 | 1.21 |
| 7. I would imagine that most people would learn to use this system very quickly. | 3.17 | 0.75 |
| 8. I found the system very cumbersome to use. | 2.83 | 1.47 |
| 9. I felt very confident using the system. | 4.00 | 0.63 |
| 10. I needed to learn a lot of things before I could get going with this system. | 3.33 | 0.82 |
| Total Score | 78.33 | 7.69 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Campo-Prieto, P.; Cancela-Carral, J.M.; Alsina-Rey, B.; Rodríguez-Fuentes, G. Immersive Virtual Reality as a Novel Physical Therapy Approach for Nonagenarians: Usability and Effects on Balance Outcomes of a Game-Based Exercise Program. J. Clin. Med. 2022, 11, 3911. https://doi.org/10.3390/jcm11133911
Campo-Prieto P, Cancela-Carral JM, Alsina-Rey B, Rodríguez-Fuentes G. Immersive Virtual Reality as a Novel Physical Therapy Approach for Nonagenarians: Usability and Effects on Balance Outcomes of a Game-Based Exercise Program. Journal of Clinical Medicine. 2022; 11(13):3911. https://doi.org/10.3390/jcm11133911
Chicago/Turabian StyleCampo-Prieto, Pablo, José Mª Cancela-Carral, Borja Alsina-Rey, and Gustavo Rodríguez-Fuentes. 2022. "Immersive Virtual Reality as a Novel Physical Therapy Approach for Nonagenarians: Usability and Effects on Balance Outcomes of a Game-Based Exercise Program" Journal of Clinical Medicine 11, no. 13: 3911. https://doi.org/10.3390/jcm11133911
APA StyleCampo-Prieto, P., Cancela-Carral, J. M., Alsina-Rey, B., & Rodríguez-Fuentes, G. (2022). Immersive Virtual Reality as a Novel Physical Therapy Approach for Nonagenarians: Usability and Effects on Balance Outcomes of a Game-Based Exercise Program. Journal of Clinical Medicine, 11(13), 3911. https://doi.org/10.3390/jcm11133911








