Latent Classes for the Treatment Outcomes in Women with Gambling Disorder and Buying/Shopping Disorder
Abstract
:1. Introduction
Objectives
2. Materials and Methods
2.1. Participants and Procedure
2.2. Assessment
2.3. CBT Program
2.4. Statistical Analysis
2.5. Ethics
3. Results
3.1. Characteristics of the Sample
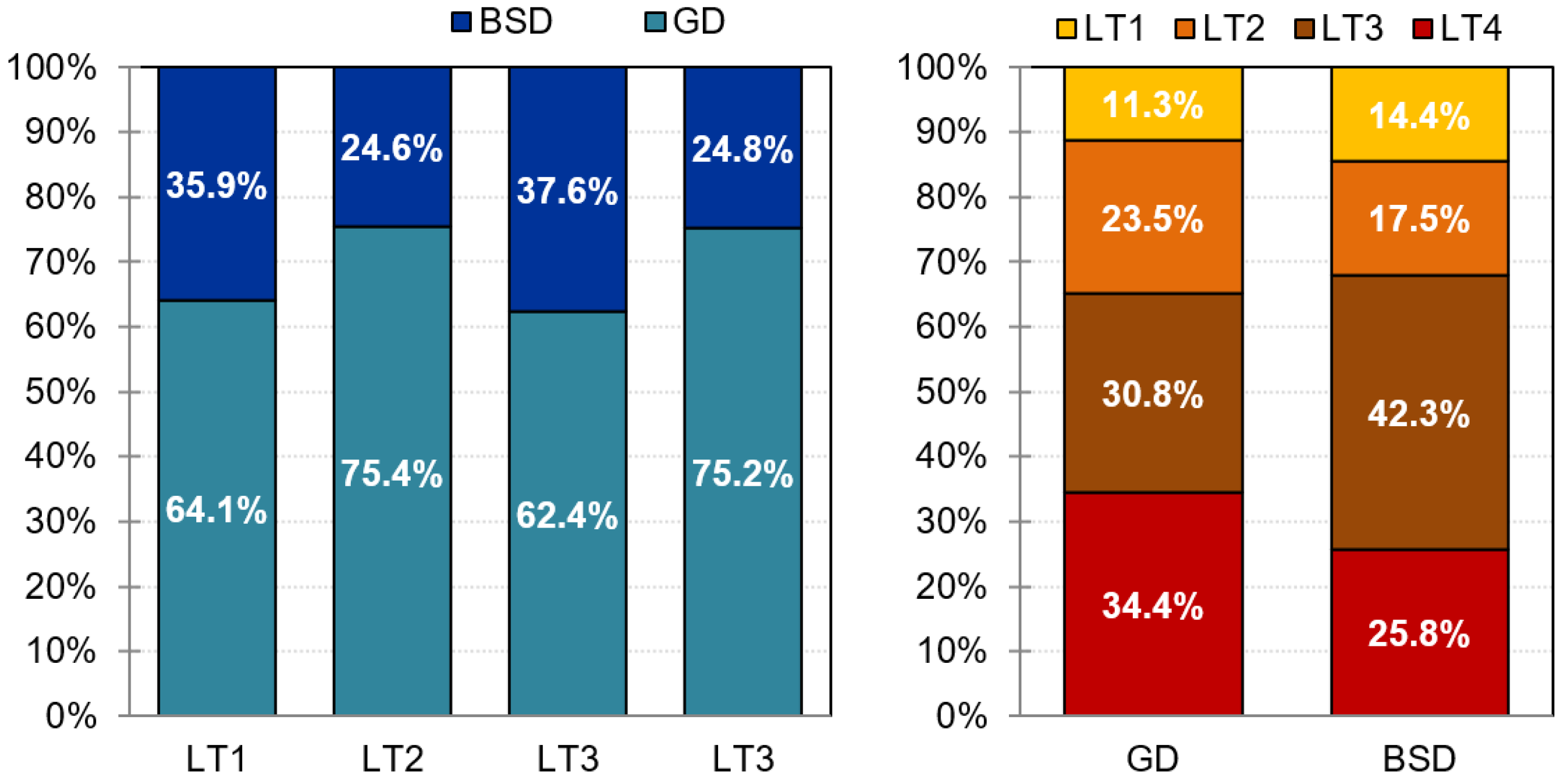
3.2. Latent Classes
3.3. Comparison between the Latent Classes for the Treatment Outcomes
3.4. Comparison between the Latent Classes for Sociodemographic and Diagnosis Profile
3.5. Comparison between the Latent Classes for Clinical Measures at Baseline
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Derevensky, J.L.; Hayman, V.; Gilbeau, L. Behavioral Addictions: Excessive Gambling, Gaming, Internet, and Smartphone Use Among Children and Adolescents. Pediatric Clin. North Am. 2019, 66, 1163–1182. [Google Scholar] [CrossRef] [PubMed]
- Karim, R.; Chaudhri, P. Behavioral Addictions: An Overview. J. Psychoact. Drugs 2012, 44, 5–17. [Google Scholar] [CrossRef] [PubMed]
- Petry, N.M.; Zajac, K.; Ginley, M.K. Behavioral Addictions as Mental Disorders: To Be or Not To Be? Annu. Rev. Clin. Psychol. 2018, 14, 399–423. [Google Scholar] [CrossRef]
- Robbins, T.W.; Clark, L. Behavioral Addictions. Curr. Opin. Neurobiol. 2015, 30, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Babić, R.; Babić, D.; Martinac, M.; Pavlovic, M.; Vasilj, I.; Miljko, M.; Vasilj, M. Addictions without Drugs: Contemporary Addictions or Way of Life? Psychiatr. Danub. 2018, 30 (Suppl. 6), 371–379. [Google Scholar] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Potenza, M.N. Non-Substance Addictive Behaviors in the Context of DSM-5. Addict. Behav. 2014, 39, 1–2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saunders, J.B. Substance Use and Addictive Disorders in DSM-5 and ICD 10 and the Draft ICD 11. Curr. Opin. Psychiatry 2017, 30, 227–237. [Google Scholar] [CrossRef]
- World Health Organization. International Classification of Diseases; 11th Revision; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- World Health Organization. The Epidemiology and Impact of Gambling Disorder and other Gambling-Related Harm. 2017. Available online: https://www.who.int/docs/default-source/substance-use/the-epidemiology-and-impact-of-gambling-disorder-and-other-gambling-relate-harm.pdf (accessed on 10 March 2020).
- Calado, F.; Griffiths, M.D. Problem Gambling Worldwide: An Update and Systematic Review of Empirical Research (2000–2015). J. Behav. Addict. 2016, 5, 592–613. [Google Scholar] [CrossRef] [Green Version]
- Allen, A.; King, A.; Hollander, E. Obsessive-Compulsive Spectrum Disorders. Dialogues Clin. Neurosci. 2003, 5, 259–271. [Google Scholar] [CrossRef]
- Black, D.W.; Shaw, M.; Blum, N. Pathological Gambling and Compulsive Buying: Do They Fall within an Obsessive-Compulsive Spectrum? Dialogues Clin. Neurosci. 2010, 12, 175–185. [Google Scholar] [CrossRef]
- Paula, J.J.D.; Costa, D.D.S.; Oliveira, F.; Alves, J.O.; Passos, L.R.; Malloy-Diniz, L.F. Impulsivity and Compulsive Buying Are Associated in a Non-Clinical Sample: An Evidence for the Compulsivity-Impulsivity Continuum? Braz. J. Psychiatry 2015, 37, 242–244. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strong, D.R.; Kahler, C.W. Evaluation of the Continuum of Gambling Problems Using the DSM-IV. Addiction 2007, 102, 713–721. [Google Scholar] [CrossRef] [PubMed]
- Aboujaoude, E. Compulsive Buying Disorder: A Review and Update. Curr. Pharm. Des. 2014, 20, 4021–4025. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Brook, J.S.; Leukefeld, C.G.; de La Rosa, M.; Brook, D.W. Compulsive Buying and Quality of Life: An Estimate of the Monetary Cost of Compulsive Buying among Adults in Early Midlife. Psychiatry Res. 2017, 252, 208–214. [Google Scholar] [CrossRef] [Green Version]
- Grant, J.E.; Chamberlain, S.R. Expanding the Definition of Addiction: DSM-5 vs. ICD-11. CNS Spectr. 2016, 21, 300–303. [Google Scholar] [CrossRef] [Green Version]
- Müller, A.; Brand, M.; Claes, L.; Demetrovics, Z.; de Zwaan, M.; Fernández-Aranda, F.; Frost, R.O.; Jimenez-Murcia, S.; Lejoyeux, M.; Steins-Loeber, S.; et al. Buying-Shopping Disorder-Is There Enough Evidence to Support Its Inclusion in ICD-11? CNS Spectr. 2019, 24, 374–379. [Google Scholar] [CrossRef]
- Maraz, A.; Griffiths, M.D.; Demetrovics, Z. The Prevalence of Compulsive Buying: A Meta-Analysis. Addiction 2016, 111, 408–419. [Google Scholar] [CrossRef] [Green Version]
- Hubert, M.; Hubert, M.; Gwozdz, W.; Raab, G.; Reisch, L. Compulsive Buying: An Increasing Problem? Investigating and Comparing Trends in Germany and Denmark, 2010–2012. J. Consum. Prot. Food Saf. 2014, 9, 280–284. [Google Scholar] [CrossRef]
- Estévez, A.; Jauregui, P.; Momeñe, J.; Macia, L.; López-González, H.; Iruarrizaga, I.; Riquelme-Ortiz, C.; Granero, R.; Fernández-Aranda, F.; Vintró-Alcaraz, C.; et al. Longitudinal Changes in Gambling, Buying and Materialism in Adolescents: A Population-Based Study. Int. J. Environ. Res. Public Health 2021, 18, 2811. [Google Scholar] [CrossRef]
- Müller, A.; Claes, L.; Birlin, A.; Georgiadou, E.; Laskowski, N.M.; Steins-Loeber, S.; Brand, M.; de Zwaan, M. Associations of Buying-Shopping Disorder Symptoms with Identity Confusion, Materialism, and Socially Undesirable Personality Features in a Community Sample. Eur. Addict. Res. 2021, 27, 142–150. [Google Scholar] [CrossRef]
- Nicoli de Mattos, C.; Kim, H.S.; Requião, M.G.; Marasaldi, R.F.; Filomensky, T.Z.; Hodgins, D.C.; Tavares, H. Gender Differences in Compulsive Buying Disorder: Assessment of Demographic and Psychiatric Co-Morbidities. PLoS ONE 2016, 11, e0167365. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Granero, R.; Fernández-Aranda, F.; Baño, M.; Steward, T.; Mestre-Bach, G.; del Pino-Gutiérrez, A.; Moragas, L.; Mallorquí-Bagué, N.; Aymamí, N.; Goméz-Peña, M.; et al. Compulsive Buying Disorder Clustering Based on Sex, Age, Onset and Personality Traits. Compr. Psychiatry 2016, 68, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Iyer, G.R.; Blut, M.; Hong Xiao, S.; Grewal, D. Impulse Buying: A Meta-Analytic Review. J. Acad. Mark. Sci. 2020, 48, 384–404. [Google Scholar] [CrossRef] [Green Version]
- Müller, A.; de Zwaan, M.; Mitchell, J.E.; Zimmermann, T. Pathological Buying and Partnership Status. Psychiatry Res. 2016, 239, 122–123. [Google Scholar] [CrossRef] [PubMed]
- Otero-López, J.M.; Villardefrancos, E. Prevalence, Sociodemographic Factors, Psychological Distress, and Coping Strategies Related to Compulsive Buying: A Cross Sectional Study in Galicia, Spain. BMC Psychiatry 2014, 14, 101. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mandolfo, M.; Lamberti, L. Past, Present, and Future of Impulse Buying Research Methods: A Systematic Literature Review. Front. Psychol. 2021, 12, 687404. [Google Scholar] [CrossRef]
- Jiménez-Murcia, S.; Granero, R.; Moragas, L.; Steiger, H.; Israel, M.; Aymamí, N.; Gómez-Peña, M.; Sauchelli, S.; Agüera, Z.; Sánchez, I.; et al. Differences and Similarities between Bulimia Nervosa, Compulsive Buying and Gambling Disorder. Eur. Eat. Disord. Rev. 2015, 23, 111–118. [Google Scholar] [CrossRef]
- Díez, D.; Aragay, N.; Soms, M.; Prat, G.; Bonet, P.; Casas, M. Women with Compulsive Buying or Gambling Disorder: Similar Profiles for Different Behavioural Addictions. Compr. Psychiatry 2018, 87, 95–99. [Google Scholar] [CrossRef]
- Granero, R.; Fernández-Aranda, F.; Mestre-Bach, G.; Steward, T.; Baño, M.; del Pino-Gutiérrez, A.; Moragas, L.; Mallorquí-Bagué, N.; Aymamí, N.; Gómez-Peña, M.; et al. Compulsive Buying Behavior: Clinical Comparison with Other Behavioral Addictions. Front. Psychol. 2016, 7, 914. [Google Scholar] [CrossRef]
- Yau, Y.H.C.; Potenza, M.N. Gambling Disorder and Other Behavioral Addictions: Recognition and Treatment. Harv Rev. Psychiatry 2015, 23, 134–146. [Google Scholar] [CrossRef]
- Lawrence, L.M.; Elphinstone, B. Coping Associated with Compulsive Buying Tendency. Stress Health 2021, 37, 263–271. [Google Scholar] [CrossRef] [PubMed]
- Velotti, P.; Rogier, G.; Beomonte Zobel, S.; Billieux, J. Association between Gambling Disorder and Emotion (Dys)Regulation: A Systematic Review and Meta-Analysis. Clin. Psychol. Rev. 2021, 87, 102037. [Google Scholar] [CrossRef] [PubMed]
- Estévez, A.; Jauregui, P.; Granero, R.; Munguía, L.; López-González, H.; Macía, L.; López, N.; Momeñe, J.; Corral, S.; Fernández-Aranda, F.; et al. Buying-Shopping Disorder, Emotion Dysregulation, Coping and Materialism: A Comparative Approach with Gambling Patients and Young People and Adolescents. Int. J. Psychiatry Clin. Pract. 2020, 24, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Nicolai, J.; Moshagen, M. Pathological Buying Symptoms Are Associated with Distortions in Judging Elapsed Time. J. Behav. Addict. 2018, 7, 752–759. [Google Scholar] [CrossRef] [PubMed]
- Clark, L.; Boileau, I.; Zack, M. Neuroimaging of Reward Mechanisms in Gambling Disorder: An Integrative Review. Mol. Psychiatry 2019, 24, 674–693. [Google Scholar] [CrossRef]
- Derbyshire, K.L.; Chamberlain, S.R.; Odlaug, B.L.; Schreiber, L.R.N.; Grant, J.E. Neurocognitive Functioning in Compulsive Buying Disorder. Ann. Clin. Psychiatry 2014, 26, 57–63. [Google Scholar]
- Kyrios, M.; Trotzke, P.; Lawrence, L.; Fassnacht, D. Behavioral Neuroscience of Buying-Shopping Disorder: A Review. Curr. Behav. Neurosci. Rep. 2018, 5, 263–270. [Google Scholar] [CrossRef]
- Lawrence, L.M.; Ciorciari, J.; Kyrios, M. Cognitive Processes Associated with Compulsive Buying Behaviours and Related EEG Coherence. Psychiatry Res. 2014, 221, 97–103. [Google Scholar] [CrossRef]
- Potenza, M.N. Clinical Neuropsychiatric Considerations Regarding Nonsubstance or Behavioral Addictions. Dialogues Clin. Neurosci. 2017, 19, 281–291. [Google Scholar] [CrossRef]
- Volkow, N.D.; Koob, G.F.; McLellan, A.T. Neurobiologic Advances from the Brain Disease Model of Addiction. N. Engl. J. Med. 2016, 374, 363–371. [Google Scholar] [CrossRef]
- Zack, M.; St George, R.; Clark, L. Dopaminergic Signaling of Uncertainty and the Aetiology of Gambling Addiction. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2020, 99, 109853. [Google Scholar] [CrossRef] [PubMed]
- Brand, M.; Wegmann, E.; Stark, R.; Müller, A.; Wölfling, K.; Robbins, T.; Potenza, M. The Interaction of Person-Affect-Cognition-Execution (I-PACE) Model for Addictive Behaviors: Update, Generalization to Addictive Behaviors beyond Internet-Use Disorders, and Specification of the Process Character of Addictive Behaviors. Neurosci. Biobehav. Rev. 2019, 104, 1–10. [Google Scholar] [CrossRef]
- Weinsztok, S.; Brassard, S.; Balodis, I.; Martin, L.E.; Amlung, M. Delay Discounting in Established and Proposed Behavioral Addictions: A Systematic Review and Meta-Analysis. Front. Behav. Neurosci. 2021, 15, 786358. [Google Scholar] [CrossRef] [PubMed]
- Dowling, N.A.; Cowlishaw, S.; Jackson, A.C.; Merkouris, S.S.; Francis, K.L.; Christensen, D.R. Prevalence of Psychiatric Co-Morbidity in Treatment-Seeking Problem Gamblers: A Systematic Review and Meta-Analysis. Aust. New Zealand J. Psychiatry 2015, 49, 519–539. [Google Scholar] [CrossRef] [Green Version]
- Grant, J.E.; Chamberlain, S.R. Gambling and Substance Use: Comorbidity and Treatment Implications. Prog. Neuropsychopharmacol. Biol. Psychiatry 2020, 99, 109852. [Google Scholar] [CrossRef]
- Lawrence, L.M.; Ciorciari, J.; Kyrios, M. Relationships That Compulsive Buying Has with Addiction, Obsessive-Compulsiveness, Hoarding, and Depression. Compr. Psychiatry 2014, 55, 1137–1145. [Google Scholar] [CrossRef] [PubMed]
- Mestre-Bach, G.; Steward, T.; Jiménez-Murcia, S.; Fernández-Aranda, F. Differences and Similarities Between Compulsive Buying and Other Addictive Behaviors. Curr. Addict. Rep. 2017, 4, 228–236. [Google Scholar] [CrossRef]
- Yakovenko, I.; Hodgins, D.C. A Scoping Review of Co-Morbidity in Individuals with Disordered Gambling. Int. Gambl. Stud. 2018, 18, 143–172. [Google Scholar] [CrossRef]
- Black, D.W.; Coryell, W.; Crowe, R.; Shaw, M.; McCormick, B.; Allen, J. The Relationship of DSM-IV Pathological Gambling to Compulsive Buying and Other Possible Spectrum Disorders: Results from the Iowa PG Family Study. Psychiatry Res. 2015, 226, 273–276. [Google Scholar] [CrossRef] [Green Version]
- Guerrero-Vaca, D.; Granero, R.; Fernández-Aranda, F.; González-Doña, J.; Müller, A.; Brand, M.; Steward, T.; Mestre-Bach, G.; Mallorquí-Bagué, N.; Aymamí, N.; et al. Underlying Mechanism of the Comorbid Presence of Buying Disorder with Gambling Disorder: A Pathways Analysis. J. Gambl. Stud. 2019, 35, 261–273. [Google Scholar] [CrossRef]
- Tolin, D.F. Is Cognitive-Behavioral Therapy More Effective than Other Therapies? A Meta-Analytic Review. Clin. Psychol. Rev. 2010, 30, 710–720. [Google Scholar] [CrossRef] [PubMed]
- Petry, N.M.; Ginley, M.K.; Rash, C.J. A Systematic Review of Treatments for Problem Gambling. Psychol. Addict. Behav. 2017, 31, 951–961. [Google Scholar] [CrossRef] [PubMed]
- Lourenço Leite, P.; Pereira, V.M.; Nardi, A.E.; Silva, A.C. Psychotherapy for Compulsive Buying Disorder: A Systematic Review. Psychiatry Res. 2014, 219, 411–419. [Google Scholar] [CrossRef]
- Pfund, R.A.; Peter, S.C.; McAfee, N.W.; Ginley, M.K.; Whelan, J.P.; Meyers, A.W. Dropout from Face-to-Face, Multi-Session Psychological Treatments for Problem and Disordered Gambling: A Systematic Review and Meta-Analysis. A Syst. Rev. Meta-Analysis. Psychol. Addict. Behav. 2021, 35, 901–913. [Google Scholar] [CrossRef]
- Hague, B.; Hall, J.; Kellett, S. Treatments for Compulsive Buying: A Systematic Review of the Quality, Effectiveness and Progression of the Outcome Evidence. J. Behav. Addict. 2016, 5, 379–394. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stinchfield, R. Reliability, Validity, and Classification Accuracy of a Measure of DSM-IV Diagnostic Criteria for Pathological Gambling. Am. J. Psychiatry 2003, 160, 180–182. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; American Psychiatric Association: Washington, DC, USA, 2010. [Google Scholar]
- Jiménez-Murcia, S.; Stinchfield, R.; Alvarez-Moya, E.; Jaurrieta, N.; Bueno, B.; Granero, R.; Aymamí, M.N.; Gómez-Peña, M.; Martínez-Giménez, R.; Fernández-Aranda, F.; et al. Reliability, Validity, and Classification Accuracy of a Spanish Translation of a Measure of DSM-IV Diagnostic Criteria for Pathological Gambling. J. Gambl. Stud. 2009, 25, 93–104. [Google Scholar] [CrossRef]
- First, M.B.; Williams, J.B.W.; Spitzer, R.L.; Gibbon, M. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID). Available online: https://eprovide.mapi-trust.org/instruments/structured-clinical-interview-for-dsm-iv-axis-i-disorders (accessed on 10 March 2020).
- Faber, R.J.; O’Guinn, T.C. A Clinical Screener for Compulsive Buying. J. Consum. Res. 1992, 19, 459–469. [Google Scholar] [CrossRef]
- McElroy, S.L.; Keck, P.E.J.; Pope, H.G.J.; Smith, J.M.; Strakowski, S.M. Compulsive Buying: A Report of 20 Cases. J. Clin. Psychiatry 1994, 55, 242–248. [Google Scholar]
- Tavares, H.; Lobo, D.S.S.; Fuentes, D.; Black, D.W. Compulsive buying disorder: A review and a case vignette. Braz. J. Psychiatry 2008, 30 (Suppl. 1), S16–S23. [Google Scholar] [CrossRef]
- Müller, A.; Mitchell, J.E.; de Zwaan, M. Compulsive Buying. Am. J. Addict. 2015, 24, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Derogatis, L.R. SCL-90-R: Symptom Checklist-90-R. Administration, Scoring and Procedures Manuall—II for the Revised Version; Clinical Psychometric Research: Towson, MD, USA, 1994. [Google Scholar]
- Derogatis, L.R. SCL-90-R. Cuestionario de 90 Síntomas; TEA Ediciones: Madrid, Spain, 1997. [Google Scholar]
- Cloninger, C. The Temperament and Character Inventory-Revised; Center for Psychobiology of Personality, Washington University: St. Louis, MO, USA, 1999. [Google Scholar]
- Gutiérrez-Zotes, J.A.; Bayón, C.; Montserrat, C.; Valero, J.; Labad, A.; Cloninger, C.R.; Fernández-Aranda, F. Inventario Del Temperamento y El Carácter-Revisado (TCI-R ). Baremación y Datos Normativos En Una Muestra de Población General. [Temperament and Character Inventory Revised (TCI-R). Standardization and Normative Data in a General Population Sample]. Actas Españolas Psiquiatr. 2004, 32, 8–15. [Google Scholar]
- Hollingshead, A.B. Four Factor Index of Social Status. Yale J. Sociol. 2011, 8, 21–51. [Google Scholar]
- Jiménez-Murcia, S.; Aymamí-Sanromà, M.; Gómez-Peña, M.; Álvarez-Moya, E.M.; Vallejo-Ruiloba, J. Protocols de Tractament Cognitivoconductual Pel Joc Patològic i d’altres Addiccions No Tòxiques; Hospital Universitari de Bellvitge: Barcelona, Spain, 2006. [Google Scholar]
- Baño, M.; Mestre-Bach, G.; Granero, R.; Fernández-Aranda, F.; Gómez-Peña, M.; Moragas, L.; del Pino-Gutierrez, A.; Codina, E.; Guillén-Guzmán, E.; Valero-Solís, S.; et al. Women and Gambling Disorder: Assessing Dropouts and Relapses in Cognitive Behavioral Group Therapy. Addict. Behav. 2021, 123, 107085. [Google Scholar] [CrossRef] [PubMed]
- Valenciano-Mendoza, E.; Fernández-Aranda, F.; Granero, R.; Gómez-Peña, M.; Moragas, L.; Pino-Gutierrez, A.D.; Mora-Maltas, B.; Baenas, I.; Guillén-Guzmán, E.; Valero-Solís, S.; et al. Suicidal Behavior in Patients with Gambling Disorder and Their Response to Psychological Treatment: The Roles of Gender and Gambling Preference. J. Psychiatr. Res. 2021, 143, 317–326. [Google Scholar] [CrossRef]
- Granero, R.; Fernández-Aranda, F.; Mestre-Bach, G.; Steward, T.; Baño, M.; Agüera, Z.; Mallorquí-Bagué, N.; Aymamí, N.; Gómez-Peña, M.; Sancho, M.; et al. Cognitive Behavioral Therapy for Compulsive Buying Behavior: Predictors of Treatment Outcome. Eur. Psychiatry 2017, 39, 57–65. [Google Scholar] [CrossRef]
- Muthén, L.K.; Muthén, B.O. Mplus Version 8.1; Muthén & Muthén: Los Angeles, CA, USA, 2017. [Google Scholar]
- Nylund, K.L.; Asparouhov, T.; Muthén, B.O. Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling: A Monte Carlo Simulation Study. Struct. Equ. Modeling 2007, 14, 535–569. [Google Scholar] [CrossRef]
- Kelley, K.; Preacher, K.J. On Effect Size. Psychol. Methods 2012, 17, 137–152. [Google Scholar] [CrossRef]
- Finner, H.; Roters, M. On the False Discovery Rate and Expected Type I Errors. Biom. J. 2001, 43, 985–1005. [Google Scholar] [CrossRef]
- Aalen, O.O.; Borgan, O.; Gjessing, H.K. Survival and Event History Analysis: A Process. Point of View; Springer: New York, NY, USA, 2008. [Google Scholar]
- Singer, J.D.; Willett, J.B. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence; Oxford University Press: New York, NY, USA, 2003. [Google Scholar]
- Goslar, M.; Leibetseder, M.; Muench, H.M.; Hofmann, S.G.; Laireiter, A.-R. Treatments for Internet Addiction, Sex Addiction and Compulsive Buying: A Meta-Analysis. J. Behav. Addict. 2020, 9, 14–43. [Google Scholar] [CrossRef] [Green Version]
- Merkouris, S.S.; Thomas, S.A.; Browning, C.J.; Dowling, N.A. Predictors of Outcomes of Psychological Treatments for Disordered Gambling: A Systematic Review. Clin. Psychol. Rev. 2016, 48, 7–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mallorquí-Bagué, N.; Mestre-Bach, G.; Lozano-Madrid, M.; Fernandez-Aranda, F.; Granero, R.; Vintró-Alcazaz, C.; del Pino-Gutiérrez, A.; Steward, T.; Gómez-Peña, M.; Aymamí, N.; et al. Trait Impulsivity and Cognitive Domains Involving Impulsivity and Compulsivity as Predictors of Gambling Disorder Treatment Response. Addict. Behav. 2018, 87, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Maniaci, G.; la Cascia, C.; Picone, F.; Lipari, A.; Cannizzaro, C.; la Barbera, D. Predictors of Early Dropout in Treatment for Gambling Disorder: The Role of Personality Disorders and Clinical Syndromes. Psychiatry Res. 2017, 257, 540–545. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, E.O.; Afonso, N.H.; Morgado, P. Non-Pharmacological Treatment of Gambling Disorder: A Systematic Review of Randomized Controlled Trials. BMC Psychiatry 2021, 21, 105. [Google Scholar] [CrossRef] [PubMed]
- Casey, L.M.; Oei, T.P.S.; Raylu, N.; Horrigan, K.; Day, J.; Ireland, M.; Clough, B.A. Internet-Based Delivery of Cognitive Behaviour Therapy Compared to Monitoring, Feedback and Support for Problem Gambling: A Randomised Controlled Trial. J. Gambl. Stud. 2017, 33, 993–1010. [Google Scholar] [CrossRef] [PubMed]
- Lara-Huallipe, M.L.; Granero, R.; Fernández-Aranda, F.; Gómez-Peña, M.; Moragas, L.; del Pino-Gutierrez, A.; Valenciano-Mendoza, E.; Mora-Maltas, B.; Baenas, I.; Etxandi, M.; et al. Clustering Treatment Outcomes in Women with Gambling Disorder. J. Gambl. Stud. in press. 2022. [Google Scholar] [CrossRef]
- Mestre-Bach, G.; Granero, R.; Vintró-Alcaraz, C.; Juvé-Segura, G.; Marimon-Escudero, M.; Rivas-Pérez, S.; Valenciano-Mendoza, E.; Mora-Maltas, B.; del Pino-Gutierrez, A.; Gómez-Peña, M.; et al. Youth and Gambling Disorder: What about Criminal Behavior? Addict. Behav. 2021, 113, 106684. [Google Scholar] [CrossRef]
- Håkansson, A.; Karlsson, A.; Widinghoff, C. Primary and Secondary Diagnoses of Gambling Disorder and Psychiatric Comorbidity in the Swedish Health Care System-A Nationwide Register Study. Front. Psychiatry 2018, 9, 426. [Google Scholar] [CrossRef] [Green Version]
- Håkansson, A.; Widinghoff, C. Over-Indebtedness and Problem Gambling in a General Population Sample of Online Gamblers. Front. Psychiatry 2020, 11, 7. [Google Scholar] [CrossRef] [Green Version]
- Bjelde, K.; Chromy, B.; Pankow, D. Casino Gambling among Older Adults in North Dakota: A Policy Analysis. J. Gambl Stud. 2008, 24, 423–440. [Google Scholar] [CrossRef]
- Bangma, D.F.; Fuermaier, A.B.M.; Tucha, L.; Tucha, O.; Koerts, J. The Effects of Normal Aging on Multiple Aspects of Financial Decision-Making. PLoS ONE 2017, 12, e0182620. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Medeiros, G.C.; Redden, S.A.; Chamberlain, S.R.; Grant, J.E. Gambling Disorder: Association between Duration of Illness, Clinical, and Neurocognitive Variables. J. Behav. Addict. 2017, 6, 194–202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tira, C.; Jackson, A.C.; Tomnay, J.E. Pathways to Late-Life Problematic Gambling in Seniors: A Grounded Theory Approach. Gerontologist 2014, 54, 1035–1048. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parke, A.; Griffiths, M.; Pattinson, J.; Keatley, D. Age-Related Physical and Psychological Vulnerability as Pathways to Problem Gambling in Older Adults. J. Behav. Addict. 2018, 7, 137–145. [Google Scholar] [CrossRef]
- Platzer, E.; Singler, K.; Dovjak, P.; Wirnsberger, G.; Perl, A.; Lindner, S.; Liew, A.; Roller-Wirnsberger, R.E. Evidence of Inter-Professional and Multi-Professional Interventions for Geriatric Patients: A Systematic Review. Int. J. Integr. Care 2020, 20, 6. [Google Scholar] [CrossRef]

| GD (n = 221) | BSD (n = 97) | |||||
|---|---|---|---|---|---|---|
| Sociodemographic variables | n | % | n | % | p | |d| |
| Education Primary | 134 | 60.6% | 38 | 39.2% | 0.001 * | 0.43 |
| Secondary | 76 | 34.4% | 38 | 39.2% | 0.10 | |
| University | 11 | 5.0% | 21 | 21.6% | 0.52 † | |
| Marital status Single | 95 | 43.0% | 37 | 38.1% | 0.649 | 0.10 |
| Married/couple | 84 | 38.0% | 42 | 43.3% | 0.11 | |
| Divorced/Separated | 42 | 19.0% | 18 | 18.6% | 0.01 | |
| Employment Unemployed | 110 | 49.8% | 47 | 48.5% | 0.828 | 0.03 |
| Employed | 111 | 50.2% | 50 | 51.5% | 0.03 | |
| Social Mean-high | 10 | 4.5% | 19 | 19.6% | 0.001 * | 0.51 † |
| Mean | 26 | 11.8% | 12 | 12.4% | 0.02 | |
| Mean-low | 37 | 16.7% | 26 | 26.8% | 0.25 | |
| Low | 148 | 67.0% | 40 | 41.2% | 0.52 † | |
| Age-onset-duration | Mean | SD | Mean | SD | p | |d| |
| Age (yrs-old) | 49.14 | 12.28 | 43.22 | 11.44 | 0.001 * | 0.50 † |
| Onset of the addiction (yrs) | 37.61 | 12.22 | 34.46 | 11.61 | 0.032 * | 0.26 |
| Duration of the addiction(yrs) | 5.62 | 5.61 | 5.75 | 5.01 | 0.841 | 0.02 |
| Psychopathology(SCL-90R) | Mean | SD | Mean | SD | p | |d| |
| Somatic | 1.64 | 0.91 | 1.45 | 1.08 | 0.103 | 0.19 |
| Obsessive–compulsive | 1.59 | 0.84 | 1.82 | 1.02 | 0.034 * | 0.25 |
| Interpersonal sensitivity | 1.45 | 0.87 | 1.50 | 1.02 | 0.670 | 0.05 |
| Depressive | 2.15 | 0.90 | 2.14 | 1.10 | 0.890 | 0.02 |
| Anxiety | 1.54 | 0.92 | 1.55 | 1.07 | 0.896 | 0.02 |
| Hostility | 1.10 | 0.84 | 1.30 | 1.00 | 0.066 | 0.22 |
| Phobic | 0.93 | 0.92 | 0.89 | 1.00 | 0.745 | 0.04 |
| Paranoid | 1.27 | 0.81 | 1.37 | 0.95 | 0.356 | 0.11 |
| Psychotic | 1.19 | 0.78 | 1.22 | 0.90 | 0.793 | 0.03 |
| GSI score | 1.54 | 0.74 | 1.56 | 0.89 | 0.838 | 0.02 |
| PST score | 56.81 | 18.46 | 54.79 | 21.42 | 0.393 | 0.10 |
| PSDI score | 2.28 | 0.59 | 2.36 | 0.70 | 0.308 | 0.12 |
| Personality (TCI-R) | Mean | SD | Mean | SD | p | |d| |
| Novelty seeking | 109.71 | 12.08 | 115.07 | 13.78 | 0.001 * | 0.41 |
| Harm avoidance | 110.98 | 15.62 | 111.64 | 19.78 | 0.749 | 0.04 |
| Reward dependence | 101.14 | 13.06 | 103.53 | 16.36 | 0.168 | 0.16 |
| Persistence | 103.86 | 17.48 | 105.05 | 19.21 | 0.589 | 0.06 |
| Self-directedness | 117.96 | 18.09 | 121.43 | 22.77 | 0.147 | 0.17 |
| Cooperativeness | 133.01 | 13.25 | 134.32 | 15.84 | 0.445 | 0.09 |
| Self-transcendence | 68.29 | 15.15 | 66.89 | 16.67 | 0.460 | 0.09 |
| Model | Akaike | Bayesian | Sample-Size | Sample Size | Online | |||
|---|---|---|---|---|---|---|---|---|
| # Class. | (AIC) | (BIC) | Adjusted BIC | Entropy | Count | % | Probab. | |
| 1 | 39,372.954 | 39,508.388 | 39,394.203 | 1.000 | T1 | 318 | 100.0% | 1.000 |
| 2 | 20,854.429 | 20,986.101 | 20,875.089 | 0.959 | T1 | 188 | 59.1% | 0.993 |
| T2 | 130 | 40.9% | 0.983 | |||||
| 3 | 20,713.397 | 20,916.548 | 20,745.272 | 0.924 | T1 | 44 | 13.8% | 0.951 |
| T2 | 125 | 39.3% | 0.972 | |||||
| T3 | 149 | 46.9% | 0.974 | |||||
| 4 | 20,625.497 | 20,900.127 | 20,668.587 | 0.939 | T1 | 39 | 12.3% | 0.997 |
| T2 | 69 | 21.7% | 0.912 | |||||
| T3 | 109 | 34.3% | 0.997 | |||||
| T4 | 101 | 31.8% | 0.963 | |||||
| 5 | 20,762.98 | 21,109.089 | 20,817.285 | 0.895 | T1 | 10 | 3.1% | 0.973 |
| T2 | 40 | 12.6% | 0.847 | |||||
| T3 | 206 | 64.8% | 0.962 | |||||
| T4 | 52 | 16.4% | 0.916 | |||||
| T5 | 10 | 3.1% | 0.979 | |||||
| 6 | 20,591.177 | 21,008.764 | 20,656.696 | 0.894 | T1 | 11 | 3.5% | 0.957 |
| T2 | 33 | 10.4% | 0.931 | |||||
| T3 | 112 | 35.2% | 0.953 | |||||
| T4 | 100 | 31.4% | 0.903 | |||||
| T5 | 42 | 13.2% | 0.945 | |||||
| T6 | 20 | 6.3% | 0.937 | |||||
| LT1; n = 39 | LT2; n = 69 | LT3; n = 109 | LT4; n = 101 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |||||
| Risk of dropout | 21 | 53.8% | 39 | 56.5% | 77 | 70.6% | 52 | 51.5% | ||||
| Risk of relapse | 4 | 10.3% | 27 | 39.1% | 43 | 39.4% | 51 | 50.5% | ||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||||
| 1 Number of sessions | 9.26 | 3.04 | 8.41 | 2.90 | 8.03 | 2.83 | 8.59 | 2.93 | ||||
| 1 Number of relapses | 0.41 | 0.76 | 0.87 | 1.28 | 0.97 | 1.38 | 1.63 | 2.07 | ||||
| 1 Euros spent/relapses | 36.8 | 37.3 | 155.6 | 156.1 | 116.9 | 117.4 | 116.5 | 117.0 | ||||
| Pairwise comparisons | ||||||||||||
| LT1–LT2 | LT1–LT3 | LT1–LT4 | LT2–LT3 | LT2–LT4 | LT3–LT4 | |||||||
| p | |d| | p | |d| | p | |d| | p | |d| | p | |d| | p | |d| | |
| Risk of dropout | 0.788 | 0.05 | 0.057 | 0.35 | 0.802 | 0.05 | 0.054 | 0.29 | 0.518 | 0.10 | 0.004 * | 0.40 |
| Risk of relapse | 0.001 * | 0.70 † | 0.001 * | 0.71 † | 0.001 * | 0.93 † | 0.966 | 0.01 | 0.144 | 0.23 | 0.108 | 0.22 |
| p | |d| | p | |d| | p | |d| | p | |d| | p | |d| | p | |d| | |
| 1 Number of sessions | 0.156 | 0.29 | 0.028 * | 0.42 | 0.243 | 0.22 | 0.392 | 0.13 | 0.679 | 0.06 | 0.155 | 0.20 |
| 1 Number of relapses | 0.019 * | 0.44 | 0.002 * | 0.50 † | 0.001 * | 0.78 † | 0.612 | 0.08 | 0.003 * | 0.44 | 0.007 * | 0.37 |
| 1 Euros spent/relapses | 0.001 * | 1.05 † | 0.001 * | 0.92 † | 0.001 * | 0.92 † | 0.077 | 0.28 | 0.077 | 0.28 | 0.981 | 0.00 |
| LT1; n = 39 | LT2; n = 69 | LT3; n = 109 | LT4; n = 101 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |||||
| Diagnosis GD | 25 | 64.1% | 52 | 75.4% | 68 | 62.4% | 76 | 75.2% | ||||
| BSD | 14 | 35.9% | 17 | 24.6% | 41 | 37.6% | 25 | 24.8% | ||||
| Education Prim. | 14 | 35.9% | 50 | 72.5% | 60 | 55.0% | 48 | 47.5% | ||||
| Secondary | 18 | 46.2% | 14 | 20.3% | 40 | 36.7% | 42 | 41.6% | ||||
| University | 7 | 17.9% | 5 | 7.2% | 9 | 8.3% | 11 | 10.9% | ||||
| Marital Single | 12 | 30.8% | 28 | 40.6% | 52 | 47.7% | 40 | 39.6% | ||||
| Married | 19 | 48.7% | 27 | 39.1% | 41 | 37.6% | 39 | 38.6% | ||||
| Divorced | 8 | 20.5% | 14 | 20.3% | 16 | 14.7% | 22 | 21.8% | ||||
| Employed Unempl. | 9 | 23.1% | 46 | 66.7% | 46 | 42.2% | 56 | 55.4% | ||||
| Employed | 30 | 76.9% | 23 | 33.3% | 63 | 57.8% | 45 | 44.6% | ||||
| Social Mean-high | 7 | 17.9% | 5 | 7.2% | 10 | 9.2% | 7 | 6.9% | ||||
| Mean | 7 | 17.9% | 5 | 7.2% | 12 | 11.0% | 14 | 13.9% | ||||
| Mean-low | 8 | 20.5% | 8 | 11.6% | 29 | 26.6% | 18 | 17.8% | ||||
| Low | 17 | 43.6% | 51 | 73.9% | 58 | 53.2% | 62 | 61.4% | ||||
| Pairwise comparisons | ||||||||||||
| LT1–LT2 | LT1–LT3 | LT1–LT4 | LT2–LT3 | LT2–LT4 | LT3–LT4 | |||||||
| p | |d| | p | |d| | p | |d| | p | |d| | p | |d| | p | |d| | |
| Diagnosis GD | 0.214 | 0.25 | 0.849 | 0.04 | 0.187 | 0.24 | 0.072 | 0.28 | 0.986 | 0.00 | 0.096 | 0.28 |
| BSD | ||||||||||||
| Education Prim. | 0.001 * | 0.75 † | 0.072 | 0.39 | 0.352 | 0.24 | 0.053 | 0.36 | 0.005 * | 0.52 † | 0.528 | 0.15 |
| Secondary | 0.56 † | 0.19 | 0.09 | 0.37 | 0.47 † | 0.10 | ||||||
| University | 0.33 | 0.29 | 0.20 | 0.04 | 0.13 | 0.09 | ||||||
| Marital Single | 0.553 | 0.21 | 0.184 | 0.35 | 0.521 | 0.19 | 0.524 | 0.14 | 0.973 | 0.02 | 0.323 | 0.16 |
| Married | 0.19 | 0.22 | 0.20 | 0.03 | 0.01 | 0.02 | ||||||
| Divorced | 0.01 | 0.15 | 0.03 | 0.15 | 0.04 | 0.18 | ||||||
| Employed Unemplo. | 0.001 * | 0.91 † | 0.034 * | 0.41 | 0.001 * | 0.68 † | 0.001 * | 0.50 † | 0.143 | 0.23 | 0.055 | 0.27 |
| Employed | ||||||||||||
| Social Mean-high | 0.018 * | 0.33 | 0.266 | 0.26 | 0.144 | 0.34 | 0.039 * | 0.07 | 0.306 | 0.01 | 0.378 | 0.08 |
| Mean | 0.33 | 0.20 | 0.11 | 0.13 | 0.22 | 0.09 | ||||||
| Mean-low | 0.25 | 0.14 | 0.07 | 0.39 | 0.18 | 0.21 | ||||||
| Low | 0.63 † | 0.19 | 0.36 | 0.43 | 0.27 | 0.17 | ||||||
| LT1; n = 39 | LT2; n = 69 | LT3; n = 109 | LT4; n = 101 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||||
| Age (yrs) | 44.69 | 8.45 | 61.51 | 7.05 | 35.87 | 7.50 | 51.04 | 7.79 | ||||
| Onset of BA (yrs) | 34.37 | 8.40 | 52.94 | 6.38 | 25.00 | 5.52 | 38.96 | 6.23 | ||||
| Duration of BA (yrs) | 5.21 | 4.58 | 4.12 | 3.70 | 7.08 | 6.60 | 5.36 | 5.01 | ||||
| SCL-90R Somatic | 0.64 | 0.65 | 1.40 | 0.80 | 1.72 | 1.02 | 1.92 | 0.87 | ||||
| SCL-90R Obses.co. | 0.66 | 0.56 | 1.35 | 0.73 | 1.91 | 0.84 | 2.00 | 0.83 | ||||
| SCL-90R Sensitivity | 0.42 | 0.47 | 1.22 | 0.69 | 1.74 | 0.89 | 1.75 | 0.89 | ||||
| SCL-90R Depressive | 0.91 | 0.79 | 1.88 | 0.79 | 2.43 | 0.80 | 2.50 | 0.85 | ||||
| SCL-90R Anxiety | 0.46 | 0.48 | 1.27 | 0.72 | 1.76 | 1.00 | 1.92 | 0.86 | ||||
| SCL-90R Hostility | 0.37 | 0.42 | 0.83 | 0.63 | 1.42 | 0.91 | 1.42 | 0.92 | ||||
| SCL-90R Phobic | 0.12 | 0.17 | 0.68 | 0.69 | 1.07 | 1.01 | 1.23 | 0.98 | ||||
| SCL-90R Paranoid | 0.49 | 0.46 | 1.03 | 0.62 | 1.47 | 0.85 | 1.62 | 0.85 | ||||
| SCL-90R Psychotic | 0.32 | 0.40 | 0.95 | 0.62 | 1.34 | 0.80 | 1.55 | 0.78 | ||||
| SCL-90R GSI score | 0.56 | 0.42 | 1.29 | 0.58 | 1.75 | 0.76 | 1.88 | 0.69 | ||||
| SCL-90R PST score | 27.90 | 15.53 | 50.43 | 15.41 | 61.74 | 16.80 | 65.08 | 13.64 | ||||
| SCL-90R PSDI score | 1.69 | 0.56 | 2.19 | 0.59 | 2.43 | 0.55 | 2.48 | 0.59 | ||||
| TCI-R Novelty.se. | 114.4 | 13.9 | 108.3 | 12.0 | 112.4 | 12.8 | 111.1 | 12.8 | ||||
| TCI-R Harm avoid. | 89.2 | 12.7 | 106.8 | 13.3 | 116.3 | 14.6 | 117.1 | 15.3 | ||||
| TCI-R Reward dep. | 109.6 | 12.5 | 102.0 | 13.1 | 102.2 | 15.7 | 98.4 | 12.5 | ||||
| TCI-R Persistence | 109.7 | 15.5 | 106.7 | 14.7 | 103.2 | 19.5 | 101.6 | 18.9 | ||||
| TCI-R Self-directed. | 142.4 | 17.2 | 122.5 | 13.4 | 116.0 | 19.3 | 110.9 | 17.0 | ||||
| TCI-R Cooperative. | 142.3 | 13.5 | 134.5 | 12.1 | 132.3 | 15.2 | 130.4 | 12.9 | ||||
| TCI-R Self-Transcen. | 62.8 | 17.3 | 72.2 | 13.3 | 66.5 | 16.6 | 68.4 | 14.7 | ||||
| n | % | n | % | n | % | n | % | |||||
| Debts due to BA | 19 | 48.7% | 20 | 29.0% | 57 | 52.3% | 47 | 46.5% | ||||
| Autolysis behavior | 4 | 10.3% | 4 | 5.8% | 20 | 18.3% | 14 | 13.9% | ||||
| Suicidal ideation | 6 | 15.4% | 15 | 21.7% | 18 | 16.5% | 22 | 21.8% | ||||
| Pairwise comparisons | ||||||||||||
| LT1–LT2 | LT1–LT3 | LT1–LT4 | LT2–LT3 | LT2–LT4 | LT3–LT4 | |||||||
| p | |d| | p | |d| | p | |d| | p | |d| | p | |d| | p | |d| | |
| Age (yrs) | 0.001 * | 2.16 † | 0.001 * | 1.10 † | 0.001 * | 0.78 † | 0.001 * | 3.52 † | 0.001 * | 1.41 † | 0.001 * | 1.98 † |
| Onset of BA (yrs) | 0.001 * | 2.49 † | 0.001 * | 1.32 † | 0.001 * | 0.62 † | 0.001 * | 4.68 † | 0.001 * | 2.22 † | 0.001 * | 2.37 † |
| Duration of BA (yrs) | 0.309 | 0.26 | 0.060 | 0.33 | 0.881 | 0.03 | 0.001 * | 0.55 † | 0.138 | 0.28 | 0.020 * | 0.29 |
| SCL-90R Somatic | 0.001 * | 1.05 † | 0.001 * | 1.26 † | 0.001 * | 1.67 † | 0.021 * | 0.35 | 0.001 * | 0.62 † | 0.102 | 0.21 |
| SCL-90R Obses.co. | 0.001 * | 1.06 † | 0.001 * | 1.74 † | 0.001 * | 1.89 † | 0.001 * | 0.70 † | 0.001 * | 0.83 † | 0.392 | 0.11 |
| SCL-90R Sensitivity | 0.001 * | 1.36 † | 0.001 * | 1.87 † | 0.001 * | 1.89 † | 0.001 * | 0.66 † | 0.001 * | 0.68 † | 0.927 | 0.01 |
| SCL-90R Depressive | 0.001 * | 1.22 † | 0.001 * | 1.91 † | 0.001 * | 1.93 † | 0.001 * | 0.70 † | 0.001 * | 0.76 † | 0.543 | 0.08 |
| SCL-90R Anxiety | 0.001 * | 1.33 † | 0.001 * | 1.66 † | 0.001 * | 2.11 † | 0.001 * | 0.57 † | 0.001 * | 0.83 † | 0.167 | 0.17 |
| SCL-90R Hostility | 0.005 * | 0.85 † | 0.001 * | 1.49 † | 0.001 * | 1.47 † | 0.001 * | 0.77 † | 0.001 * | 0.76 † | 0.978 | 0.00 |
| SCL-90R Phobic | 0.002 * | 1.12 † | 0.001 * | 1.32 † | 0.001 * | 1.57 † | 0.004 * | 0.45 | 0.001 * | 0.65 † | 0.192 | 0.16 |
| SCL-90R Paranoid | 0.001 * | 0.98 † | 0.001 * | 1.43 † | 0.001 * | 1.65 † | 0.001 * | 0.60 † | 0.001 * | 0.80 † | 0.163 | 0.17 |
| SCL-90R Psychotic | 0.001 * | 1.19 † | 0.001 * | 1.62 † | 0.001 * | 1.99 † | 0.001 * | 0.56 † | 0.001 * | 0.86 † | 0.037 * | 0.26 |
| SCL-90R GSI score | 0.001 * | 1.44 † | 0.001 * | 1.92 † | 0.001 * | 2.31 † | 0.001 * | 0.67 † | 0.001 * | 0.92 † | 0.150 | 0.18 |
| SCL-90R PST score | 0.001 * | 1.46 † | 0.001 * | 2.09 † | 0.001 * | 2.54 † | 0.001 * | 0.70 † | 0.001 * | 1.01 † | 0.118 | 0.22 |
| SCL-90R PSDI score | 0.001 * | 0.88 † | 0.001 * | 1.35 † | 0.001 * | 1.38 † | 0.007 * | 0.42 | 0.001 * | 0.50 † | 0.507 | 0.09 |
| TCI-R Novelty.se. | 0.017 * | 0.47 | 0.403 | 0.15 | 0.163 | 0.25 | 0.035 * | 0.34 | 0.162 | 0.22 | 0.437 | 0.11 |
| TCI-R Harm avoid. | 0.001 * | 1.36 † | 0.001 * | 1.98 † | 0.001 * | 1.98 † | 0.001 * | 0.68 † | 0.001 * | 0.72 † | 0.660 | 0.06 |
| TCI-R Reward dep. | 0.007 * | 0.59 † | 0.004 * | 0.52 † | 0.001 * | 0.89 † | 0.944 | 0.01 | 0.094 | 0.28 | 0.049 * | 0.27 |
| TCI-R Persistence | 0.397 | 0.20 | 0.052 | 0.37 | 0.017 * | 0.47 | 0.207 | 0.20 | 0.071 | 0.30 | 0.523 | 0.08 |
| TCI-R Self-directed. | 0.001 * | 1.29 † | 0.001 * | 1.44 † | 0.001 * | 1.84 † | 0.014 * | 0.39 | 0.001 * | 0.76 † | 0.031 * | 0.28 |
| TCI-R Cooperative. | 0.005 * | 0.61 † | 0.001 * | 0.70 † | 0.001 * | 0.90 † | 0.301 | 0.16 | 0.054 | 0.33 | 0.301 | 0.14 |
| TCI-R Self-Transcen. | 0.002 * | 0.61 † | 0.201 | 0.22 | 0.054 | 0.35 | 0.016 * | 0.38 | 0.114 | 0.27 | 0.366 | 0.12 |
| p | |d| | p | |d| | p | |d| | p | |d| | p | |d| | p | |d| | |
| Debts due to BA | 0.040 * | 0.41 | 0.701 | 0.07 | 0.817 | 0.04 | 0.002 † | 0.51 * | 0.021 † | 0.36 | 0.404 | 0.12 |
| Autolysis behavior | 0.395 | 0.17 | 0.239 | 0.23 | 0.568 | 0.11 | 0.017 † | 0.40 | 0.093 | 0.28 | 0.378 | 0.12 |
| Suicidal ideation | 0.423 | 0.16 | 0.870 | 0.03 | 0.396 | 0.17 | 0.382 | 0.13 | 0.995 | 0.00 | 0.331 | 0.13 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Granero, R.; Fernández-Aranda, F.; Lara-Huallipe, M.L.; Gómez-Peña, M.; Moragas, L.; Baenas, I.; Müller, A.; Brand, M.; Sisquellas, C.; Jiménez-Murcia, S. Latent Classes for the Treatment Outcomes in Women with Gambling Disorder and Buying/Shopping Disorder. J. Clin. Med. 2022, 11, 3917. https://doi.org/10.3390/jcm11133917
Granero R, Fernández-Aranda F, Lara-Huallipe ML, Gómez-Peña M, Moragas L, Baenas I, Müller A, Brand M, Sisquellas C, Jiménez-Murcia S. Latent Classes for the Treatment Outcomes in Women with Gambling Disorder and Buying/Shopping Disorder. Journal of Clinical Medicine. 2022; 11(13):3917. https://doi.org/10.3390/jcm11133917
Chicago/Turabian StyleGranero, Roser, Fernando Fernández-Aranda, Milagros Lizbeth Lara-Huallipe, Mónica Gómez-Peña, Laura Moragas, Isabel Baenas, Astrid Müller, Matthias Brand, Claudia Sisquellas, and Susana Jiménez-Murcia. 2022. "Latent Classes for the Treatment Outcomes in Women with Gambling Disorder and Buying/Shopping Disorder" Journal of Clinical Medicine 11, no. 13: 3917. https://doi.org/10.3390/jcm11133917
APA StyleGranero, R., Fernández-Aranda, F., Lara-Huallipe, M. L., Gómez-Peña, M., Moragas, L., Baenas, I., Müller, A., Brand, M., Sisquellas, C., & Jiménez-Murcia, S. (2022). Latent Classes for the Treatment Outcomes in Women with Gambling Disorder and Buying/Shopping Disorder. Journal of Clinical Medicine, 11(13), 3917. https://doi.org/10.3390/jcm11133917








