Impact of the COVID-19 Pandemic on the Use and Outcomes of Cardiac Procedures in COPD Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population and Variables
2.2. Statistical Analysis
2.3. Sensitivity Analysis
2.4. Ethical Aspects
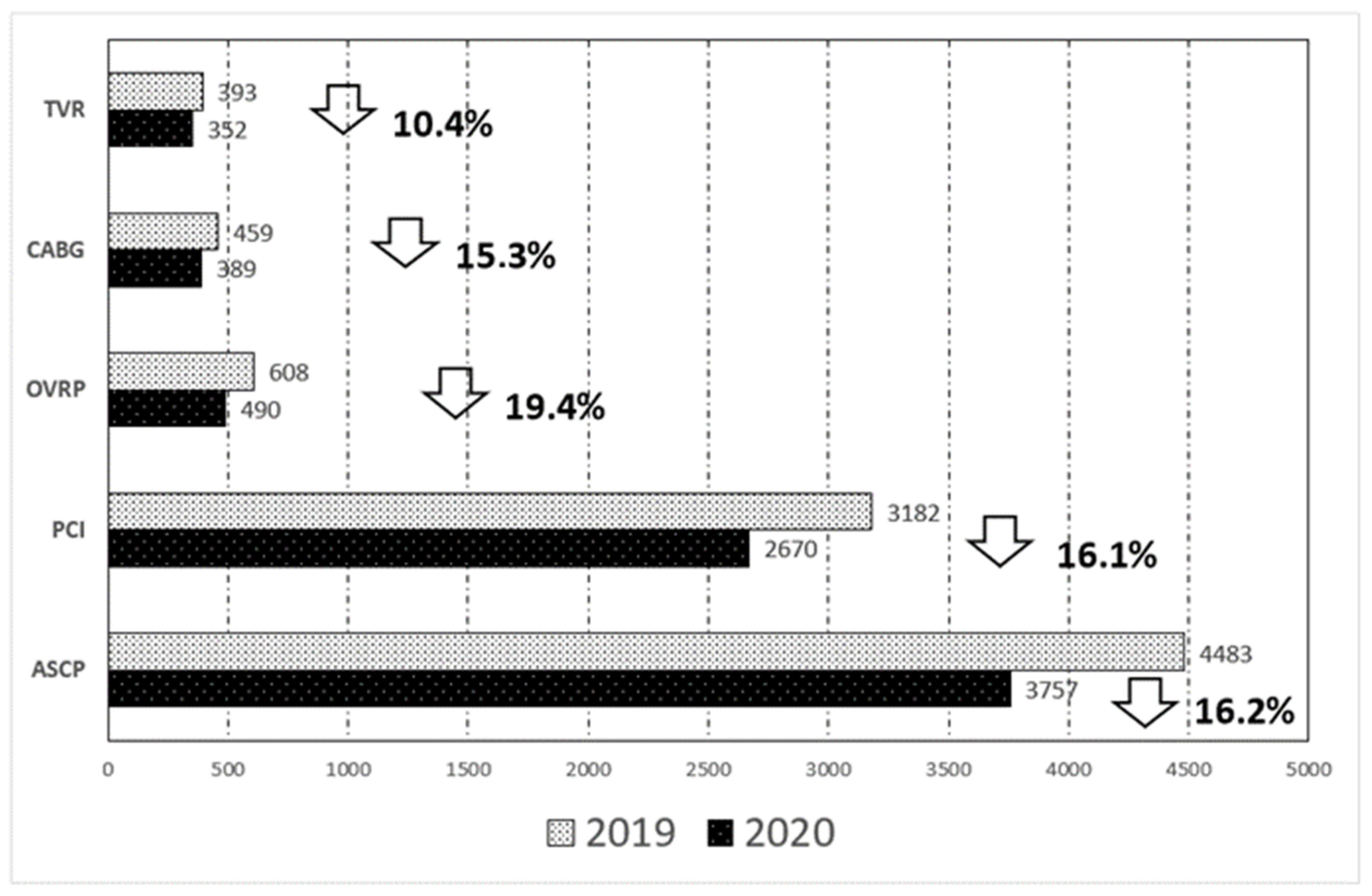
3. Results
Sensitivity Analysis
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhong, S.; Huisingh-Scheetz, M.; Huang, E.S. Delayed medical care and its perceived health impact among US older adults during the COVID-19 pandemic. J. Am. Geriatr. Soc. 2022, 70, 1620–1628. [Google Scholar] [CrossRef] [PubMed]
- Czeisler, M.É.; Marynak, K.; Clarke, K.E.N.; Salah, Z.; Shakya, I.; Thierry, J.M.; Ali, N.; McMillan, H.; Wiley, J.F.; Weaver, M.D.; et al. Delay or avoidance of medical care because of COVID-19–related concerns—United States, June 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1250–1257. [Google Scholar] [CrossRef] [PubMed]
- Pouwels, B.D.C.; Simons, S.O.; Theunissen, M.; Peters, M.L.; Schoenmaekers, J.J.; Bekkers, S.C.; Everdingen, M.H.J.V.D.B.-V. Healthcare use during COVID-19 and the effect on psychological distress in patients with chronic cardiopulmonary disorders in the Netherlands: A cross-sectional study. BMJ Open 2021, 11, e046883. [Google Scholar] [CrossRef] [PubMed]
- Malik, J.A.; Ahmed, S.; Shinde, M.; Almermesh, M.H.S.; Alghamdi, S.; Hussain, A.; Anwar, S. The impact of COVID-19 on comorbidities: A review of recent updates for combating it. Saudi J. Biol. Sci. 2022, 29, 3586–3599. [Google Scholar] [CrossRef]
- Andreen, N.; Andersson, L.-M.; Sundell, N.; Gustavsson, L.; Westin, J. Mortality of COVID-19 is associated with comorbidity in patients with chronic obstructive pulmonary disease. Infect. Dis. 2022, 54, 508–513. [Google Scholar] [CrossRef]
- Keskin, G.; Khalil, E.; Uysal, A. Should we postpone elective cardiovascular procedures and percutaneous coronary interventions during the COVID-19 Pandemic? Heart Surg. Forum 2021, 24, E022–E030. [Google Scholar] [CrossRef]
- Watanabe, S.; Shin, J.-H.; Morishita, T.; Takada, D.; Kunisawa, S.; Imanaka, Y. Medium-term impact of the coronavirus disease 2019 pandemic on the practice of percutaneous coronary interventions in Japan. J. Atheroscler. Thromb. 2021, 63194. [Google Scholar] [CrossRef]
- De Filippo, O.; D’Ascenzo, F.; Angelini, F.; Bocchino, P.P.; Conrotto, F.; Saglietto, A.; Secco, G.G.; Campo, G.; Gallone, G.; Verardi, R.; et al. Reduced rate of hospital admissions for ACS during COVID-19 outbreak in Northern Italy. N. Engl. J. Med. 2020, 383, 88–89. [Google Scholar] [CrossRef]
- Braiteh, N.; Rehman, W.U.; Alom, M.; Skovira, V.; Breiteh, N.; Rehman, I.; Yarkoni, A.; Kahsou, H.; Rehman, A. Decrease in acute coronary syndrome presentations during the COVID-19 pandemic in upstate New York. Am. Heart J. 2020, 226, 147–151. [Google Scholar] [CrossRef]
- Morishita, T.; Takada, D.; Shin, J.-H.; Higuchi, T.; Kunisawa, S.; Imanaka, Y. Trends, treatment approaches, and in-hospital mortality for acute coronary syndrome in Japan during the coronavirus disease 2019 pandemic. J. Atheroscler. Thromb. 2021, 29, 597–607. [Google Scholar] [CrossRef]
- Dessie, Z.G.; Zewotir, T. Mortality-related risk factors of COVID-19: A systematic review and meta-analysis of 42 studies and 423,117 patients. BMC Infect. Dis. 2021, 21, 855. [Google Scholar] [CrossRef] [PubMed]
- Benson, R.A.; Nandhra, S. Outcomes of vascular and endovascular interventions performed during the coronavirus disease 2019 (COVID-19) pandemic: The vascular and endovascular research network (VERN) COVID-19 vascular service (COVER) tier 2 study. Ann. Surg. 2021, 273, 630–635. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Sanidad, Consumo y Bienestar Social. Spanish Register of Specialized Care-Basic Minimum Database [Registro de Actividad de Atención Especializada. RAE-CMBD]. Available online: https://www.mscbs.gob.es/estadEstudios/estadisticas/cmbdhome.htm (accessed on 2 February 2022).
- Quan, H.; Sundararajan, V.; Halfon, P.; Fong, A.; Burnand, B.; Luthi, J.-C.; Saunders, L.D.; Beck, C.A.; Feasby, T.E.; Ghali, W.A. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med. Care 2005, 43, 1130–1139. [Google Scholar] [CrossRef]
- Hosmer, D.W.; Lemeshow, S. Sturdivant RX. In Applied Logistic Regression, 3rd ed.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2013. [Google Scholar]
- Ministerio de Sanidad, Consumo y Bienestar Social. Solicitud de Extracción de Datos—Extraction Request (Spanish National Hospital Discharge Database). Available online: https://www.mscbs.gob.es/estadEstudios/estadisticas/estadisticas/estMinisterio/SolicitudCMBDdocs/2018_Formulario_Peticion_Datos_RAE_CMBD.pdf (accessed on 2 February 2022).
- Tam, D.Y.; Qiu, F.; Manoragavan, R.; Fremes, S.E.; Hassan, A.; Ko, D.T.; Lauck, S.B.; Naimark, D.; Ouzounian, M.; Sander, B.; et al. The impact of the COVID-19 pandemic on cardiac procedure wait list mortality in Ontario, Canada. Can. J. Cardiol. 2021, 37, 1547–1554. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.C.; Shaw, L.; Hirschfeld, C.B.; Maurovich-Horvat, P.; Nørgaard, B.L.; Pontone, G.; Jimenez-Heffernan, A.; Sinitsyn, V.; Sergienko, V.; Ansheles, A.; et al. Impact of COVID-19 on the imaging diagnosis of cardiac disease in Europe. Open Heart 2021, 8, e001681. [Google Scholar] [CrossRef]
- Phua, J.; Weng, L.; Ling, L.; Egi, M.; Lim, C.-M.; Divatia, J.V.; Shrestha, B.R.; Arabi, Y.M.; Ng, J.; Gomersall, C.D.; et al. Intensive care management of coronavirus disease 2019 (COVID-19): Challenges and recommendations. Lancet Respir. Med. 2020, 8, 506–517. [Google Scholar] [CrossRef]
- Hartnett, K.P.; Kite-Powell, A.; Devies, J.; Coletta, M.A.; Boehmer, T.K.; Adjemian, J.; Gundlapalli, A.V. National syndromic surveillance program community of practice impact of the COVID-19 pandemic on emergency department visits—United States, 1 January 2019–30 May 2020. MMWR. Morb. Mortal. Wkly. Rep. 2020, 69, 699–704. [Google Scholar] [CrossRef]
- Vlastos, D.; Chauhan, I.; Mensah, K.; Cannoletta, M.; Asonitis, A.; Elfadil, A.; Petrou, M.; De Souza, A.; Quarto, C.; Bhudia, S.K.; et al. The impact of COVID-19 pandemic on aortic valve surgical service: A single centre experience. BMC Cardiovasc. Disord. 2021, 21, 434. [Google Scholar] [CrossRef]
- Perek, B.; Olasinska-Wisniewska, A.; Misterski, M.; Puslecki, M.; Grygier, M.; Buczkowski, P.; Lesiak, M.; Stankowski, T.; Szarpak, L.; Ruetzler, K.; et al. How the COVID-19 pandemic changed treatment of severe aortic stenosis: A single cardiac center experience. J. Thorac. Dis. 2021, 13, 906–917. [Google Scholar] [CrossRef]
- Leclercq, F.; Iemmi, A.; Lattuca, B.; Macia, J.-C.; Gervasoni, R.; Roubille, F.; Gandet, T.; Schmutz, L.; Akodad, M.; Agullo, A.; et al. Feasibility and safety of transcatheter aortic valve implantation performed without intensive care unit admission. Am. J. Cardiol. 2016, 118, 99–106. [Google Scholar] [CrossRef]
- Piccolo, R.; Bruzzese, D.; Mauro, C.; Aloia, A.; Baldi, C.; Boccalatte, M.; Bottiglieri, G.; Briguori, C.; Caiazzo, G.; Calabrò, P.; et al. Population trends in rates of percutaneous coronary revascularization for acute coronary syndromes associated with the COVID-19 outbreak. Circulation 2020, 141, 2035–2037. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Leor, O.; Cid-Álvarez, B.; de Prado, A.P.; Rossello, X.; Ojeda, S.; Serrador, A.; López-Palop, R.; Martín-Moreiras, J.; Rumoroso, J.R.; Cequier, Á.; et al. Impact of COVID-19 on ST-segment elevation myocardial infarction care. The Spanish experience. Rev. Esp. Cardiol. 2020, 73, 994–1002. [Google Scholar] [CrossRef] [PubMed]
- Kwok, C.S.; Gale, C.P.; Kinnaird, T.; Curzen, N.; Ludman, P.; Kontopantelis, E.; Wu, J.; Denwood, T.; Fazal, N.; Deanfield, J.; et al. Impact of COVID-19 on percutaneous coronary intervention for ST-elevation myocardial infarction. Heart 2020, 106, 1805–1811. [Google Scholar] [CrossRef] [PubMed]
- Kwok, C.S.; Gale, C.P.; Curzen, N.; de Belder, M.A.; Ludman, P.; Lüscher, T.F.; Kontopantelis, E.; Roebuck, C.; Denwood, T.; Burton, T.; et al. Impact of the COVID-19 Pandemic on Percutaneous Coronary Intervention in England: Insights from the British cardiovascular intervention society PCI database cohort. Circ. Cardiovasc. Interv. 2020, 13, e009654. [Google Scholar] [CrossRef] [PubMed]
- Gopal, K.; Krishna, N.; Jose, R.; Biju, S.S.C.; Pichandi, J.S.; Varma, P.K. Effects of the COVID-19 pandemic on cardiac surgery practice and outcomes. J. Chest Surg. 2022, 55, 61–68. [Google Scholar] [CrossRef]
- Day, E.; Fiorentino, F.; Abdelkhalek, M.; Smail, H.; Stock, U.A.; Bhudia, S.; De Robertis, F.; Bahrami, T.; Raja, S.; Gaer, J. The results of cardiac surgery during the COVID-19 pandemic compared with previous years: A propensity weighted study of outcomes at six months. J. R. Soc. Med. 2022. [Google Scholar] [CrossRef]
- Alqahtani, J.S.; Oyelade, T.; Aldhahir, A.M.; Alghamdi, S.M.; Almehmadi, M.; Alqahtani, A.S.; Quaderi, S.; Mandal, S.; Hurst, J.R. Prevalence, severity and mortality associated with COPD and smoking in patients with COVID-19: A rapid systematic review and meta-analysis. PLoS ONE 2020, 15, e0233147. [Google Scholar] [CrossRef]
- Rabbani, G.; Islam, S.M.S.; Rahman, M.A.; Amin, N.; Marzan, B.; Robin, R.C.; Alif, S.M. Pre-existing COPD is associated with an increased risk of mortality and severity in COVID-19: A rapid systematic review and meta-analysis. Expert Rev. Respir. Med. 2021, 15, 705–716. [Google Scholar] [CrossRef]
- Gupta, A.K.; Leslie, A.; Hewitt, J.N.; Kovoor, J.G.; Ovenden, C.D.; Edwards, S.; Chan, J.C.Y.; Worthington, M.G. Cardiac surgery on patients with COVID-19: A systematic review and meta-analysis. ANZ J. Surg. 2022, 92, 1007–1014. [Google Scholar] [CrossRef]
- Tereshchenko, L.G.; Bishop, A.; Fisher-Campbell, N.; Levene, J.; Morris, C.C.; Patel, H.; Besson, E.; Blank, J.A.; Beadner, J.N.; Coblens, M.; et al. Risk of cardiovascular events after Covid-19: A double-cohort study. medRxiv 2021. [Google Scholar] [CrossRef]
- Dixon, L.K.; Di Tommaso, E.; Dimagli, A.; Sinha, S.; Sandhu, M.; Benedetto, U.; Angelini, G.D. Impact of sex on outcomes after cardiac surgery: A systematic review and meta-analysis. Int. J. Cardiol. 2021, 343, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Moreno, R.; Díez, J.L.; Diarte, J.A.; Macaya, F.; de la Torre Hernández, J.M.; Rodríguez-Leor, O.; Trillo, R.; Alonso-Briales, J.; Amat-Santos, I.; Romaguera, R.; et al. Consequences of canceling elective invasive cardiac procedures during COVID-19 outbreak. Catheter. Cardiovasc. Interv. 2021, 97, 927–937. [Google Scholar] [CrossRef] [PubMed]
- Di Martino, M.; Septiem, J.G.; González, R.M.; De Nova, J.L.M.; Rodríguez, D.L.H.Á.; Bonito, A.C.; Martín-Pérez, E. Cirugía electiva durante la pandemia por SARS-CoV-2 (COVID-19): Análisis de morbimortalidad y recomendaciones sobre priorización de los pacientes y medidas de seguridad. Cir. Esp. 2020, 98, 525–532. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Caulo, E.A.; Alcázar, M.C.; Jiménez, J.M.G.; Aroca, J.M.B. Encuesta nacional: Impacto de la COVID-19 en los servicios de cirugía cardiovascular de España (Estudio SECCE-COVID-19). Cir. Cardiovasc. 2021, 28, 67–70. [Google Scholar] [CrossRef]
| Variables | Year 2019 | Year 2020 | p-Value |
|---|---|---|---|
| N | 4483 | 3757 | NA |
| Men, n (%) | 3899 (86.97) | 3198 (85.12) | 0.015 |
| Women, n (%) | 584 (13.03) | 559 (14.88) | |
| Age, mean (SD) | 71.81 (9.43) | 71.69 (9.47) | 0.582 |
| 40–54 years, n (%) | 183 (4.08) | 170 (4.52) | 0.626 |
| 55–64 years, n (%) | 834 (18.6) | 688 (18.31) | |
| 65–74 years, n (%) | 1588 (35.42) | 1359 (36.17) | |
| ≥75 years, n (%) | 1878 (41.89) | 1540 (40.99) | |
| CCI index, mean (SD) | 3.03 (1.64) | 3.09 (1.70) | 0.098 |
| Diabetes, n (%) | 1793 (40) | 1517 (40.38) | 0.724 |
| Asthma, n (%) | 115 (2.57) | 106 (2.82) | 0.473 |
| Stroke, n (%) | 48 (1.07) | 39 (1.04) | 0.885 |
| Peripheral vascular disease, n (%) | 605 (13.50) | 509 (13.55) | 0.945 |
| Ischemic heart disease, n (%) | 3783 (84.39) | 3205 (85.31) | 0.246 |
| Valvular heart disease, n (%) | 1558 (34.75) | 1347 (35.85) | 0.298 |
| Atrial fibrillation, n (%) | 1095 (24.43) | 933 (24.83) | 0.668 |
| Heart failure, n (%) | 1161 (25.9) | 982 (26.14) | 0.805 |
| Chronic kidney disease, n (%) | 766 (17.09) | 624 (16.61) | 0.564 |
| COVID-19, n (%) | NA | 30 (0.8) | - |
| Oxygen prior to hospital admission, n (%) | 195 (4.35) | 152 (4.05) | 0.494 |
| Non-invasive mechanical ventilation, n (%) | 151 (3.37) | 135 (3.59) | 0.578 |
| Invasive mechanical ventilation, n (%) | 319 (7.12) | 238 (6.33) | 0.160 |
| Dialysis, n (%) | 121 (2.7) | 76 (2.02) | 0.045 |
| Admission to ICU, n (%) | 2027 (45.22) | 1733 (46.13) | 0.408 |
| LOHS, mean (SD) | 10.13 (9.42) | 9.37 (9.16) | 0.004 |
| IHM, n (%) | 194 (4.33) | 200 (5.32) | 0.035 |
| Percutaneous Coronary Intervention | Coronary Artery Bypass Graft | |||||
|---|---|---|---|---|---|---|
| Variable | Year 2019 | Year 2020 | p-Value | Year 2019 | Year 2020 | p-Value |
| N (%) | 3182 | 2670 | NA | 459 (100) | 389 (100) | NA |
| Men, n (%) | 2819 (88.59) | 2317 (86.78) | 0.035 | 422 (91.94) | 347 (89.2) | 0.172 |
| Women, n (%) | 363 (11.41) | 353 (13.22) | 37 (8.06) | 42 (10.8) | ||
| Age, mean (SD) | 71.51 (9.62) | 71.4 (9.75) | 0.644 | 69.6 (7.66) | 69.03 (7.25) | 0.270 |
| 40–54 years, n (%) | 137 (4.31) | 138 (5.17) | 0.469 | 19 (4.14) | 11 (2.83) | 0.105 |
| 55–64 years, n (%) | 641 (20.14) | 524 (19.63) | 93 (20.26) | 86 (22.11) | ||
| 65–74 years, n (%) | 1116 (35.07) | 936 (35.06) | 210 (45.75) | 201 (51.67) | ||
| ≥75 years, n (%) | 1288 (40.48) | 1072 (40.15) | 137 (29.85) | 91 (23.39) | ||
| CCI index, mean (SD) | 3.13 (1.65) | 3.22 (1.71) | 0.044 | 2.99 (1.54) | 2.99 (1.66) | 0.990 |
| Diabetes, n (%) | 1315 (41.33) | 1088 (40.75) | 0.655 | 200 (43.57) | 194 (49.87) | 0.067 |
| Asthma, n (%) | 77 (2.42) | 76 (2.85) | 0.308 | 10 (2.18) | 8 (2.06) | 0.902 |
| Stroke, n (%) | 25 (0.79) | 24 (0.9) | 0.636 | 6 (1.31) | 3 (0.77) | 0.448 |
| Peripheral vascular disease, n (%) | 372 (11.69) | 318 (11.91) | 0.796 | 87 (18.95) | 74 (19.02) | 0.980 |
| Valvular heart disease, n (%) | 545 (17.13) | 508 (19.03) | 0.060 | 197 (42.92) | 159 (40.87) | 0.548 |
| Atrial fibrillation, n (%) | 577 (18.13) | 505 (18.91) | 0.444 | 136 (29.63) | 111 (28.53) | 0.727 |
| Heart failure, n (%) | 802 (25.2) | 672 (25.17) | 0.975 | 108 (23.53) | 102 (26.22) | 0.366 |
| Chronic kidney disease, n (%) | 530 (16.66) | 439 (16.44) | 0.826 | 74 (16.12) | 55 (14.14) | 0.423 |
| COVID-19, n (%) | NA | 22 (0.82) | - | NA | 4 (1.03) | - |
| Oxygen prior to hospital admission, n (%) | 141 (4.43) | 117 (4.38) | 0.927 | 4 (0.87) | 6 (1.54) | 0.367 |
| Non-invasive mechanical ventilation, n (%) | 93 (2.92) | 80 (3) | 0.869 | 29 (6.32) | 27 (6.94) | 0.716 |
| Invasive mechanical ventilation, n (%) | 114 (3.58) | 95 (3.56) | 0.960 | 83 (18.08) | 57 (14.65) | 0.180 |
| Dialysis, n (%) | 57 (1.79) | 40 (1.5) | 0.382 | 30 (6.54) | 21 (5.40) | 0.201 |
| Admission to ICU, n (%) | 1143 (35.92) | 959 (35.92) | 0.998 | 349 (76.03) | 319 (82.01) | 0.034 |
| LOHS, mean (SD) | 7.56 (7.48) | 6.88 (6.7) | 0.002 | 19.55 (19.44) | 17.62 (15.6) | 0.115 |
| IHM, n (%) | 126 (3.96) | 126 (4.72) | 0.154 | 23 (5.01) | 21 (5.4) | 0.800 |
| Open Heart Valve Replacement | Transcatheter Valve Replacement | |||||
|---|---|---|---|---|---|---|
| Variable | Year 2019 | Year 2020 | p-Value | Year 2019 | Year 2020 | p-Value |
| N (%) | 608 (100) | 490 (100) | NA | 393 | 352 | NA |
| Men, n (%) | 487 (80.1) | 377 (76.94) | 0.204 | 315 (80.15) | 278 (78.98) | 0.691 |
| Women, n (%) | 121 (19.9) | 113 (23.06) | 78 (19.85) | 74 (21.02) | ||
| Age, mean (SD) | 70.47 (8.22) | 70.08 (7.69) | 0.416 | 78.89 (7.38) | 79.53 (6.57) | 0.217 |
| 40–54 years, n (%) | 26 (4.28) | 20 (4.08) | 0.257 | 2 (0.51) | 1 (0.28) | 0.471 |
| 55–64 years, n (%) | 113 (18.59) | 90 (18.37) | 15 (3.82) | 7 (1.99) | ||
| 65–74 years, n (%) | 248 (40.79) | 227 (46.33) | 78 (19.85) | 68 (19.32) | ||
| ≥75 years, n (%) | 221 (36.35) | 153 (31.22) | 298 (75.83) | 276 (78.41) | ||
| CCI index, mean (SD) | 2.50 (1.45) | 2.49 (1.47) | 0.825 | 2.97 (1.68) | 2.95 (1.7) | 0.595 |
| Diabetes, n (%) | 191 (31.41) | 153 (31.22) | 0.946 | 146 (37.15) | 145 (41.19) | 0.259 |
| Asthma, n (%) | 22 (3.62) | 9 (1.84) | 0.076 | 11 (2.8) | 15 (4.26) | 0.278 |
| Stroke, n (%) | 12 (1.97) | 9 (1.84) | 0.869 | 7 (1.78) | 4 (1.14) | 0.466 |
| Peripheral vascular disease, n (%) | 106 (17.43) | 78 (15.92) | 0.504 | 67 (17.05) | 60 (17.05) | 0.999 |
| Ischemic heart disease, n (%) | 206 (33.88) | 178 (36.33) | 0.398 | 132 (33.59) | 136 (38.64) | 0.152 |
| Atrial fibrillation, n (%) | 276 (45.39) | 228 (46.53) | 0.707 | 171 (43.51) | 142 (40.34) | 0.381 |
| Heart failure, n (%) | 155 (25.49) | 138 (28.16) | 0.320 | 141 (35.88) | 122 (34.66) | 0.728 |
| Chronic kidney disease, n (%) | 86 (14.14) | 69 (14.08) | 0.976 | 103 (26.21) | 83 (23.58) | 0.408 |
| COVID-19, n (%) | NA | 4 (0.82) | - | NA | 2 (0.57) | - |
| Oxygen prior to hospital admission, n (%) | 10 (1.64) | 7 (1.43) | 0.773 | 40 (10.18) | 25 (7.1) | 0.137 |
| Non-invasive mechanical ventilation, n (%) | 28 (4.61) | 32 (6.53) | 0.163 | 14 (3.56) | 6 (1.7) | 0.117 |
| Invasive mechanical ventilation, n (%) | 133 (21.88) | 107 (21.84) | 0.988 | 16 (4.07) | 7 (1.99) | 0.101 |
| Dialysis, n (%) | 37 (6.09) | 24 (4.9) | 0.393 | 9 (2.29) | 12 (3.41) | 0.357 |
| Admission to ICU, n (%) | 460 (75.66) | 409 (83.47) | 0.002 | 198 (50.38) | 163 (46.31) | 0.267 |
| LOHS, mean (SD) | 18.52 (18.32) | 18.7 (18.07) | 0.873 | 11.36 (10.25) | 10.03 (8.7) | 0.058 |
| IHM, n (%) | 41 (6.74) | 43 (8.78) | 0.208 | 14 (3.56) | 15 (4.26) | 0.622 |
| Any Cardiac Procedure | PCI | CABG | OVRP | TVR | |
|---|---|---|---|---|---|
| VARIABLE | OR (95% CI) | OR(95% CI) | OR(95% CI) | OR(95% CI) | OR(95% CI) |
| Men | Reference | Reference | Reference | Reference | Reference |
| Women | 1.78 (1.37–2.32) | 1.23 (0.84–1.81) | 2.99 (1.30–6.87) | 3.34 (2.07–5.38) | 0.86 (0.32–2.31) |
| CCI * | 1.28 (1.22–1.35) | 1.28 (1.21–1.36) | 1.40 (1.15–1.60) | 1.39 (1.22–1.59) | 1.25 (1.03–1.52) |
| Age * | 1.02 (1.00–1.04) | 1.01 (0.96–1.06) | 1.05 (1.02–1.08) | 1.04 (1.01–1.07) | 1.08 (0.95–1.21) |
| Year 2019 | Reference | Reference | Reference | Reference | Reference |
| Year 2020 | 1.18 (1.03–1.47) | 1.16 (0.90–1.50) | 1.03 (0.54–1.90) | 1.29 (0.81–2.03) | 1.19 (0.57–2.53) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Miguel-Diez, J.; Jimenez-Garcia, R.; de Miguel-Yanes, J.M.; Hernández-Barrera, V.; Carabantes-Alarcon, D.; Zamorano-Leon, J.J.; Noriega, C.; Lopez-de-Andres, A. Impact of the COVID-19 Pandemic on the Use and Outcomes of Cardiac Procedures in COPD Patients. J. Clin. Med. 2022, 11, 3924. https://doi.org/10.3390/jcm11133924
de Miguel-Diez J, Jimenez-Garcia R, de Miguel-Yanes JM, Hernández-Barrera V, Carabantes-Alarcon D, Zamorano-Leon JJ, Noriega C, Lopez-de-Andres A. Impact of the COVID-19 Pandemic on the Use and Outcomes of Cardiac Procedures in COPD Patients. Journal of Clinical Medicine. 2022; 11(13):3924. https://doi.org/10.3390/jcm11133924
Chicago/Turabian Stylede Miguel-Diez, Javier, Rodrigo Jimenez-Garcia, Jose M. de Miguel-Yanes, Valentin Hernández-Barrera, David Carabantes-Alarcon, Jose J. Zamorano-Leon, Concepción Noriega, and Ana Lopez-de-Andres. 2022. "Impact of the COVID-19 Pandemic on the Use and Outcomes of Cardiac Procedures in COPD Patients" Journal of Clinical Medicine 11, no. 13: 3924. https://doi.org/10.3390/jcm11133924
APA Stylede Miguel-Diez, J., Jimenez-Garcia, R., de Miguel-Yanes, J. M., Hernández-Barrera, V., Carabantes-Alarcon, D., Zamorano-Leon, J. J., Noriega, C., & Lopez-de-Andres, A. (2022). Impact of the COVID-19 Pandemic on the Use and Outcomes of Cardiac Procedures in COPD Patients. Journal of Clinical Medicine, 11(13), 3924. https://doi.org/10.3390/jcm11133924








