Symptomatic Bunionette Treated with Sliding Oblique Metatarsal Osteotomy—Case Series
Abstract
:1. Introduction
2. Methods
2.1. Outcome Measures
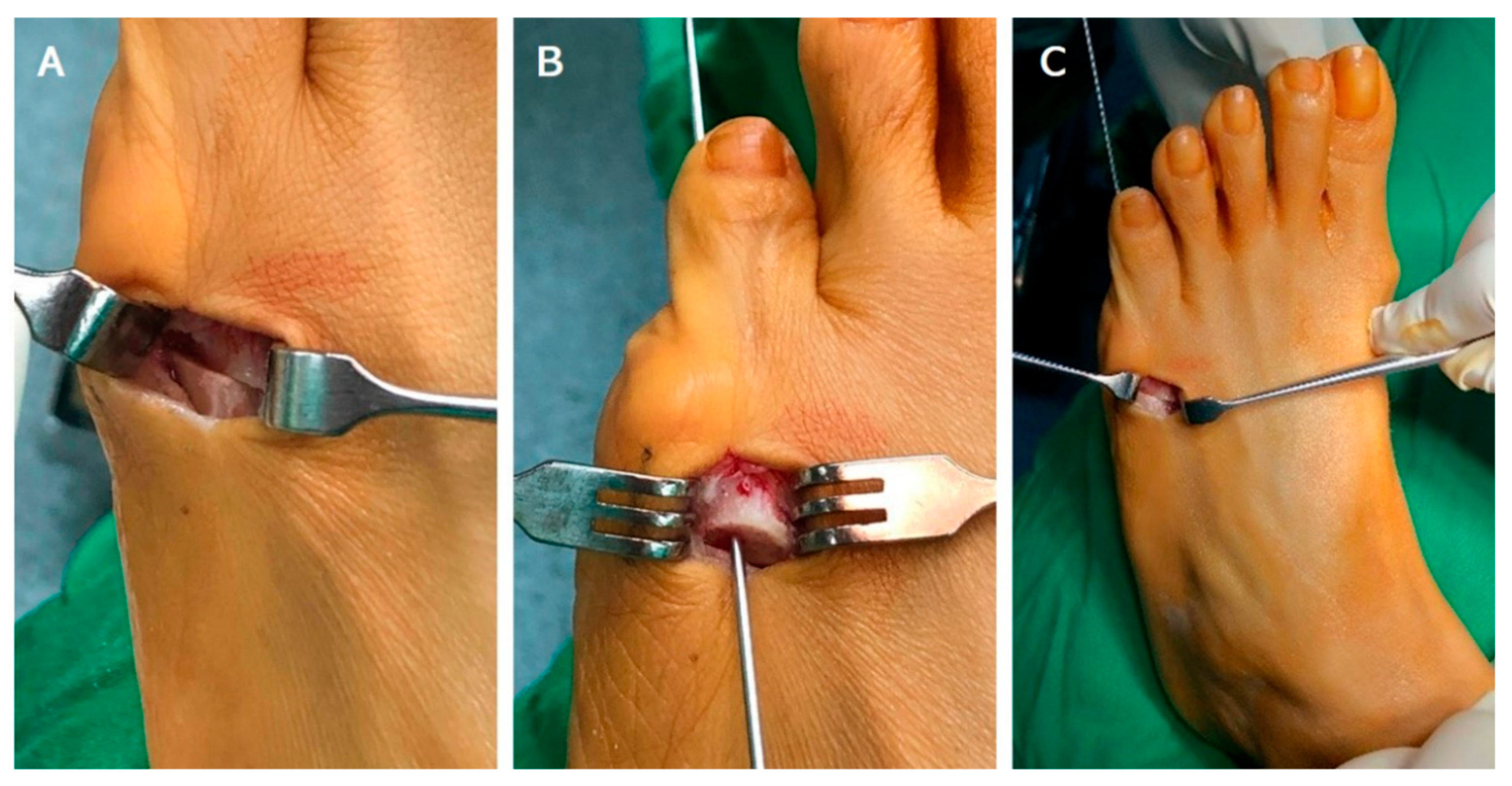
2.2. Operative Technique and Postoperative Care
2.3. Statistical Data Analysis
3. Results
3.1. Patient Demographics
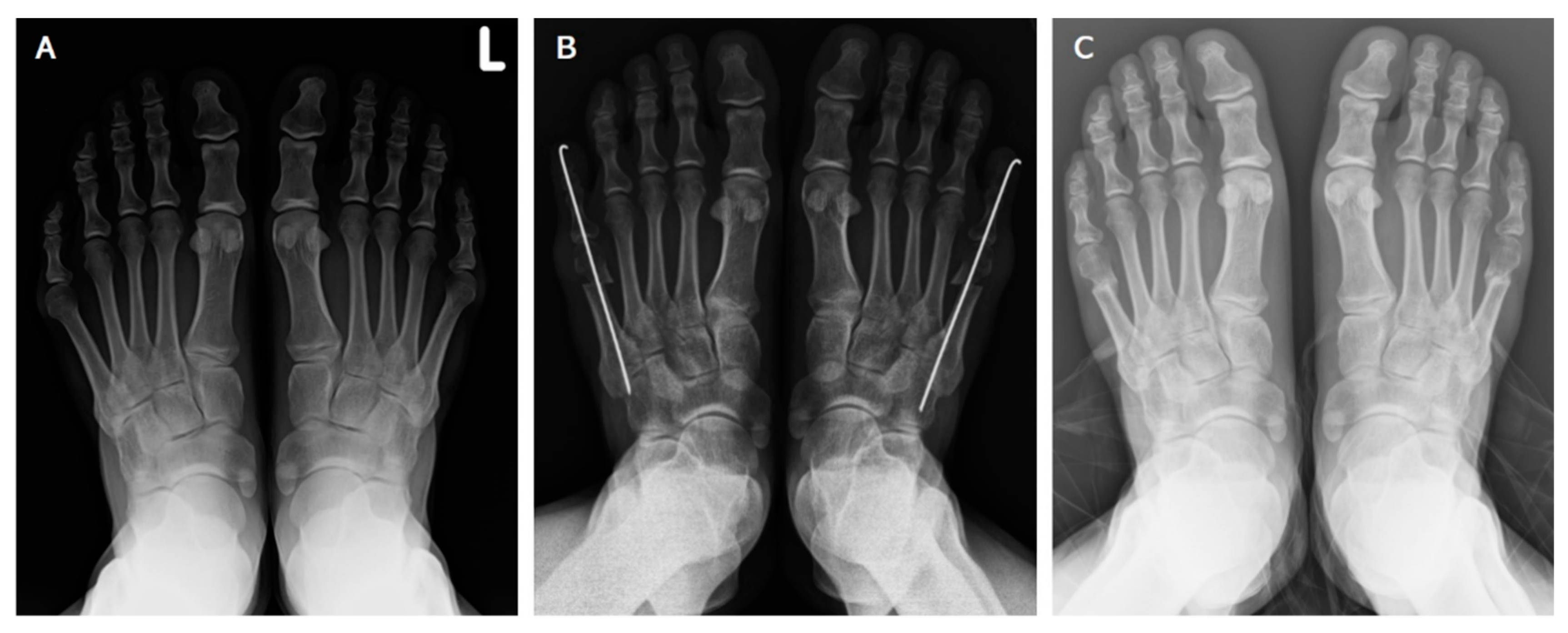
3.2. Radiographic Assessment
3.3. Clinical Assessment
3.4. Subgroup Analysis
3.5. Complication
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Coughlin, M.J. Etiology and treatment of the bunionette deformity. Instr. Course Lect. 1990, 39, 37–48. [Google Scholar] [PubMed]
- Shi, G.G.; Humayun, A.; Whalen, J.L.; Kitaoka, H.B. Management of Bunionette Deformity. J. Am. Acad. Orthop. Surg. 2018, 26, e396–e404. [Google Scholar] [CrossRef] [PubMed]
- Steinke, M.S.; Boll, K.L. Hohmann-Thomasen metatarsal osteotomy for tailor’s bunion (bunionette). J. Bone Jt. Surg. Am. Vol. 1989, 71, 423–426. [Google Scholar] [CrossRef]
- Brown, J.E. Functional and cosmetic correction of metatarsus latus (splay foot). Clin. Orthop. Relat. Res. 1959, 14, 166–170. [Google Scholar]
- Koti, M.; Maffulli, N. Bunionette. J. Bone Jt. Surg. Am. Vol. 2001, 83, 1076–1082. [Google Scholar] [CrossRef]
- Coughlin, M.J. Treatment of bunionette deformity with longitudinal diaphyseal osteotomy with distal soft tissue repair. Foot Ankle 1991, 11, 195–203. [Google Scholar] [CrossRef]
- Kitaoka, H.B.; Holiday, A.D., Jr. Metatarsal head resection for bunionette: Long-term follow-up. Foot Ankle 1991, 11, 345–349. [Google Scholar] [CrossRef]
- Radl, R.; Leithner, A.; Koehler, W.; Scheipl, S.; Windhager, R. The modified distal horizontal metatarsal osteotomy for correction of bunionette deformity. Foot Ankle Int. 2005, 26, 454–457. [Google Scholar] [CrossRef]
- Klenerman, L. Surgery of the foot and ankle. In The British Editorial Society of Bone and Joint Surgery; Coughlin, M.J., Mann, R.A., Saltzman, C.L., Eds.; Elsevier: Philadelphia, PA, USA, 2007; p. 2400. ISBN 13-978-0323-03305-3. [Google Scholar]
- Fallat, L.M. Pathology of the fifth ray, including the tailor’s bunion deformity. Clin. Pediatr. Med. Surg. 1990, 7, 689–715. [Google Scholar]
- Boyer, M.L.; Deorio, J.K. Bunionette deformity correction with distal chevron osteotomy and single absorbable pin fixation. Foot Ankle Int. 2003, 24, 834–837. [Google Scholar] [CrossRef]
- Castle, J.E.; Cohen, A.H.; Docks, G. Fifth metatarsal distal oblique wedge osteotomy utilizing cortical screw fixation. J. Foot Surg. 1992, 31, 478–485. [Google Scholar] [PubMed]
- Catanzariti, A.R.; Friedman, C.; DiStazio, J. Oblique osteotomy of the fifth metatarsal: A five year review. J. Foot Surg. 1988, 27, 316–320. [Google Scholar] [PubMed]
- Friend, G.; Grace, K.; Stone, H.A. L-osteotomy with absorbable fixation for correction of tailor’s bunion. J. Foot Ankle Surg. 1993, 32, 14–19. [Google Scholar]
- Glover, J.P.; Weil, L., Jr.; Weil, L.S., Sr. Scarfette osteotomy for surgical treatment of bunionette deformity. Foot Ankle Spec. 2009, 2, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Haber, J.H.; Kraft, J. Crescentic osteotomy for fifth metatarsal head lesions. J. Foot Surg. 1980, 19, 66–67. [Google Scholar] [PubMed]
- Kaplan, E.G.; Kaplan, G.; Jacobs, A.M. Management of fifth metatarsal head lesions by biplane osteotomy. J. Foot Surg. 1976, 15, 1–8. [Google Scholar]
- Kitaoka, H.B.; Holiday, A.D., Jr. Lateral condylar resection for bunionette. Clin. Orthop. Relat. Res. 1992, 278, 183–192. [Google Scholar]
- Masquijo, J.J.; Willis, B.R.; Kontio, K.; Dobbs, M.B. Symptomatic bunionette deformity in adolescents: Surgical treatment with metatarsal sliding osteotomy. J. Pediatr. Orthop. 2010, 30, 904–909. [Google Scholar] [CrossRef]
- Frankel, J.P.; Turf, R.M.; King, B.A. Tailor’s bunion: Clinical evaluation and correction by distal metaphyseal osteotomy with cortical screw fixation. J. Foot Surg. 1989, 28, 237–243. [Google Scholar]
- Kitaoka, H.B.; Holiday, A.D., Jr.; Campbell, D.C., 2nd. Distal Chevron metatarsal osteotomy for bunionette. Foot Ankle 1991, 12, 80–85. [Google Scholar] [CrossRef]
- Kitaoka, H.B.; Leventen, E.O. Medial displacement metatarsal osteotomy for treatment of painful bunionette. Clin. Orthop. Relat. Res. 1989, 243, 172–179. [Google Scholar] [CrossRef]
- Leach, R.E.; Igou, R. Metatarsal osteotomy for bunionette deformity. Clin. Orthop. Relat. Res. 1974, 100, 171–175. [Google Scholar] [CrossRef]
- Sponsel, K.H. Bunionette correction by metatarsal osteotomy: Preliminary report. Orthop. Clin. N. Am. 1976, 7, 809–819. [Google Scholar] [CrossRef]
- Cooper, M.T.; Coughlin, M.J. Subcapital oblique osteotomy for correction of bunionette deformity: Medium-term results. Foot Ankle Int. 2013, 34, 1376–1380. [Google Scholar] [CrossRef]
- London, B.P.; Stern, S.F.; Quist, M.A.; Lee, R.K.; Picklesimer, E.K. Long oblique distal osteotomy of the fifth metatarsal for correction of tailor’s bunion: A retrospective review. J. Foot Ankle Surg. 2003, 42, 36–42. [Google Scholar] [CrossRef]
- Guha, A.R.; Mukhopadhyay, S.; Thomas, R.H. ‘Reverse’ scarf osteotomy for bunionette correction: Initial results of a new surgical technique. Foot Ankle Surg. 2012, 18, 50–54. [Google Scholar] [CrossRef]
- Maher, A.J.; Kilmartin, T.E. Scarf osteotomy for correction of Tailor’s bunion: Mid- to long-term followup. Foot Ankle Int. 2010, 31, 676–682. [Google Scholar] [CrossRef]
- Okuda, R.; Kinoshita, M.; Morikawa, J.; Jotoku, T.; Abe, M. Proximal dome-shaped osteotomy for symptomatic bunionette. Clin. Orthop. Relat. Res. 2002, 396, 173–178. [Google Scholar] [CrossRef]
- Giannini, S.; Bevoni, R.; Vannini, F.; Cadossi, M. Hallux Valgus Surgery: The Minimally Invasive Bunion Correction. In Minimally Invasive Surgery in Orthopedics; Scuderi, G.R., Tria, A.J., Eds.; Springer: New York, NY, USA, 2010; pp. 463–471. [Google Scholar]
- Giannini, S.; Faldini, C.; Vannini, F.; Digennaro, V.; Bevoni, R.; Luciani, D. The minimally invasive osteotomy “S.E.R.I.” (simple, effective, rapid, inexpensive) for correction of bunionette deformity. Foot Ankle Int. 2008, 29, 282–286. [Google Scholar] [CrossRef]
- Biz, C.; Corradin, M.; Kanah, W.T.K.; Dalmau-Pastor, M.; Zornetta, A.; Volpin, A.; Ruggieri, P. Medium-Long-Term Clinical and Radiographic Outcomes of Minimally Invasive Distal Metatarsal Metaphyseal Osteotomy (DMMO) for Central Primary Metatarsalgia: Do Maestro Criteria Have a Predictive Value in the Preoperative Planning for This Percutaneous Technique? Biomed. Res. Int. 2018, 2018, 1947024. [Google Scholar] [CrossRef] [Green Version]
| Cases | Side(L/R) | Gender | Mean Age | Coughlin and Fallat Type |
|---|---|---|---|---|
| n: 51 | 29/22 | F = 34, M = 10 (7 bilateral feet) | 51.01 | Ⅰ = 6 Ⅱ = 10 Ⅲ = 12 Ⅳ = 23 |
| Radiographic Measurements | Preoperative Mean (SD) | Postoperative Mean (SD) | Preoperative and Postoperative Difference | p Value |
|---|---|---|---|---|
| IMA | 9.84 (2.40) | 5.88 (2.29) | 3.96 | p < 0.001 |
| LDA | 4.99 (1.85) | 1.98 (1.41) | 3.01 | p < 0.001 |
| MTPA | 15.72 (5.50) | 6.49 (4.77) | 9.23 | p < 0.001 |
| Clinical Scores | Preoperative Mean (SD) | Postoperative Mean (SD) | Preoperative and Postoperative Difference | p Value |
|---|---|---|---|---|
| AOFAS | 65.43 (10.04) | 93 (10.35) | 27.57 | p < 0.001 |
| VAS | 3.83 (1.02) | 0.17 (0.91) | 3.66 | p < 0.001 |
| Subgroup Type | IMA Mean Difference | LDA Mean Difference | MTPA Mean Difference | AOFAS Mean Difference | VAS Mean Difference |
|---|---|---|---|---|---|
| Type I n = 6 | 2.91 | 2.18 | 11.33 | 29.66 | 3.66 |
| p value | p < 0.001 | p > 0.05 | p < 0.001 | p < 0.001 | p < 0.001 |
| Type II n = 10 | 3.31 | 2.34 | 8.33 | 26.0 | 3.40 |
| p value | p < 0.001 | p < 0.05 | p < 0.001 | p < 0.001 | p < 0.001 |
| Type III n = 12 | 4.15 | 2.80 | 7.04 | 25.83 | 3.08 |
| p value | p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 |
| Type IV n = 10 | 4.37 | 3.61 | 10.21 | 28.31 | 3.61 |
| p value | p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shen, Y.-T.; Huang, P.-J.; Chen, S.-J.; Chang, S.-M. Symptomatic Bunionette Treated with Sliding Oblique Metatarsal Osteotomy—Case Series. J. Clin. Med. 2022, 11, 3962. https://doi.org/10.3390/jcm11143962
Shen Y-T, Huang P-J, Chen S-J, Chang S-M. Symptomatic Bunionette Treated with Sliding Oblique Metatarsal Osteotomy—Case Series. Journal of Clinical Medicine. 2022; 11(14):3962. https://doi.org/10.3390/jcm11143962
Chicago/Turabian StyleShen, Yu-Ting, Peng-Ju Huang, Shu-Jung Chen, and Shun-Min Chang. 2022. "Symptomatic Bunionette Treated with Sliding Oblique Metatarsal Osteotomy—Case Series" Journal of Clinical Medicine 11, no. 14: 3962. https://doi.org/10.3390/jcm11143962






