Clinical Characteristics and Potential Pathogenesis of Cardiac Necrotizing Enterocolitis in Neonates with Congenital Heart Disease: A Narrative Review
Abstract
:1. Introduction
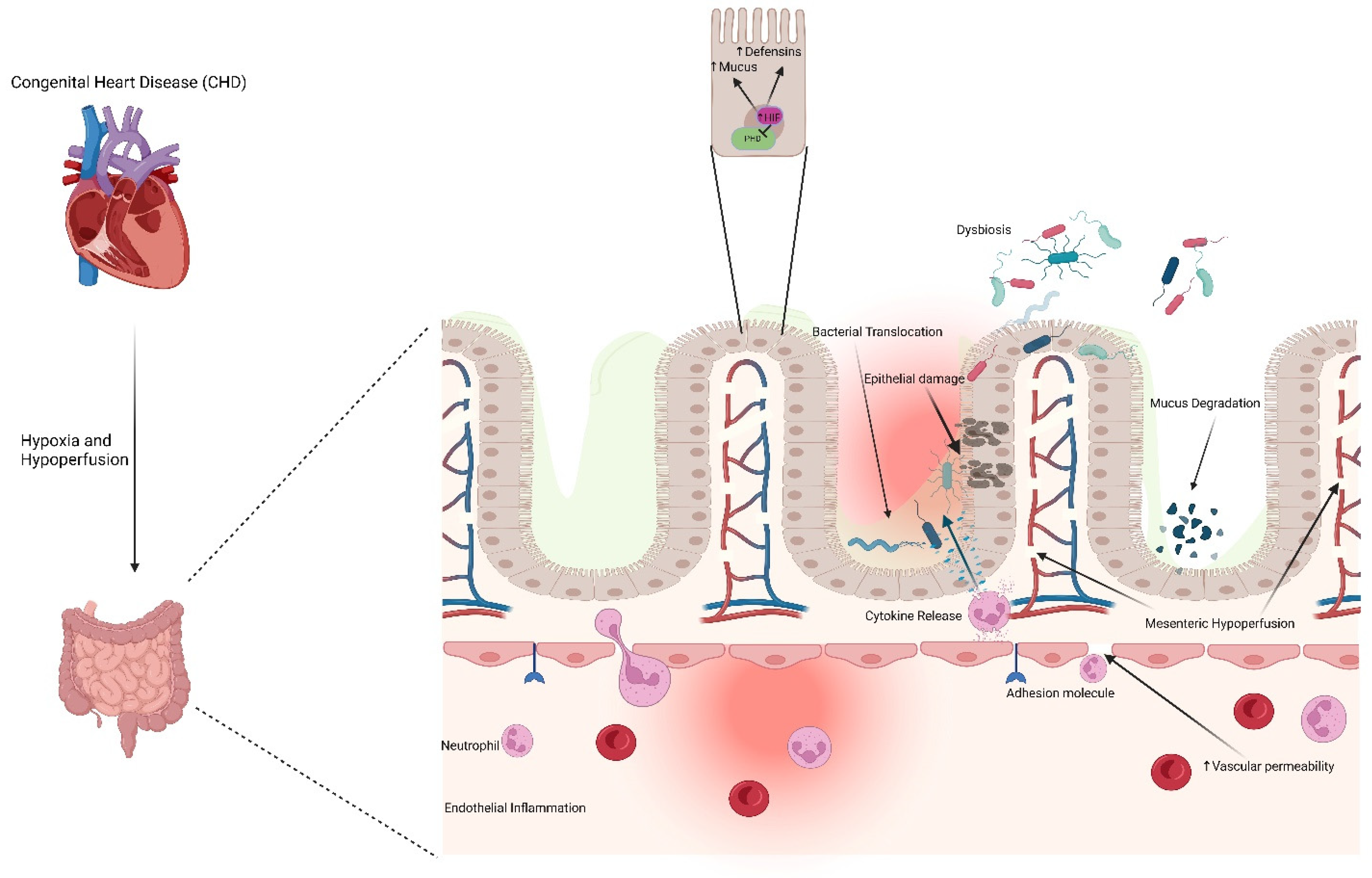
2. Pathogenesis of Intestinal Injury in Congenital Heart Disease
3. Risk Factors Contributing to Cardiac NEC Pathogenesis
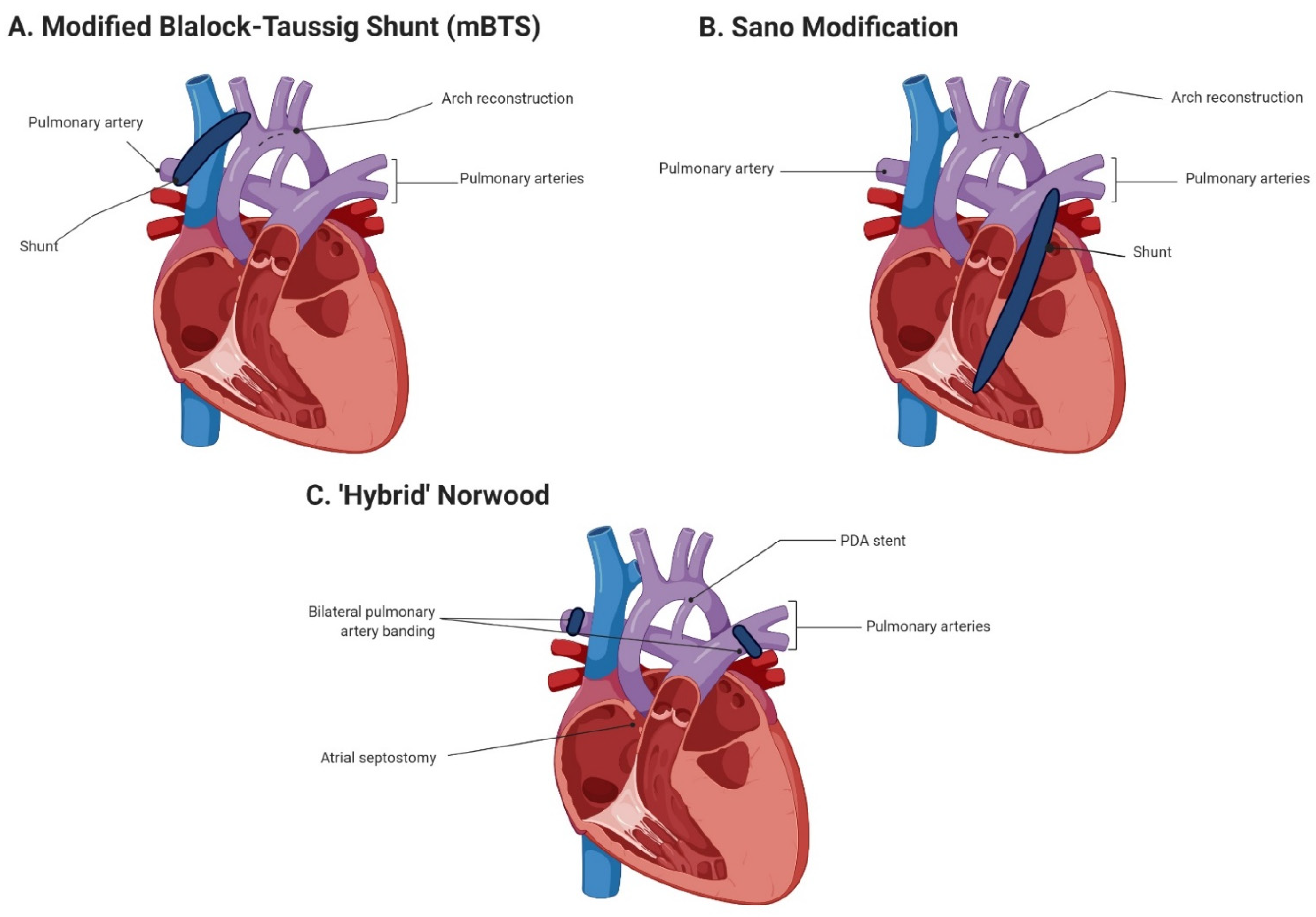
4. Abdominal Complications Relating to HLHS Stage I Palliation
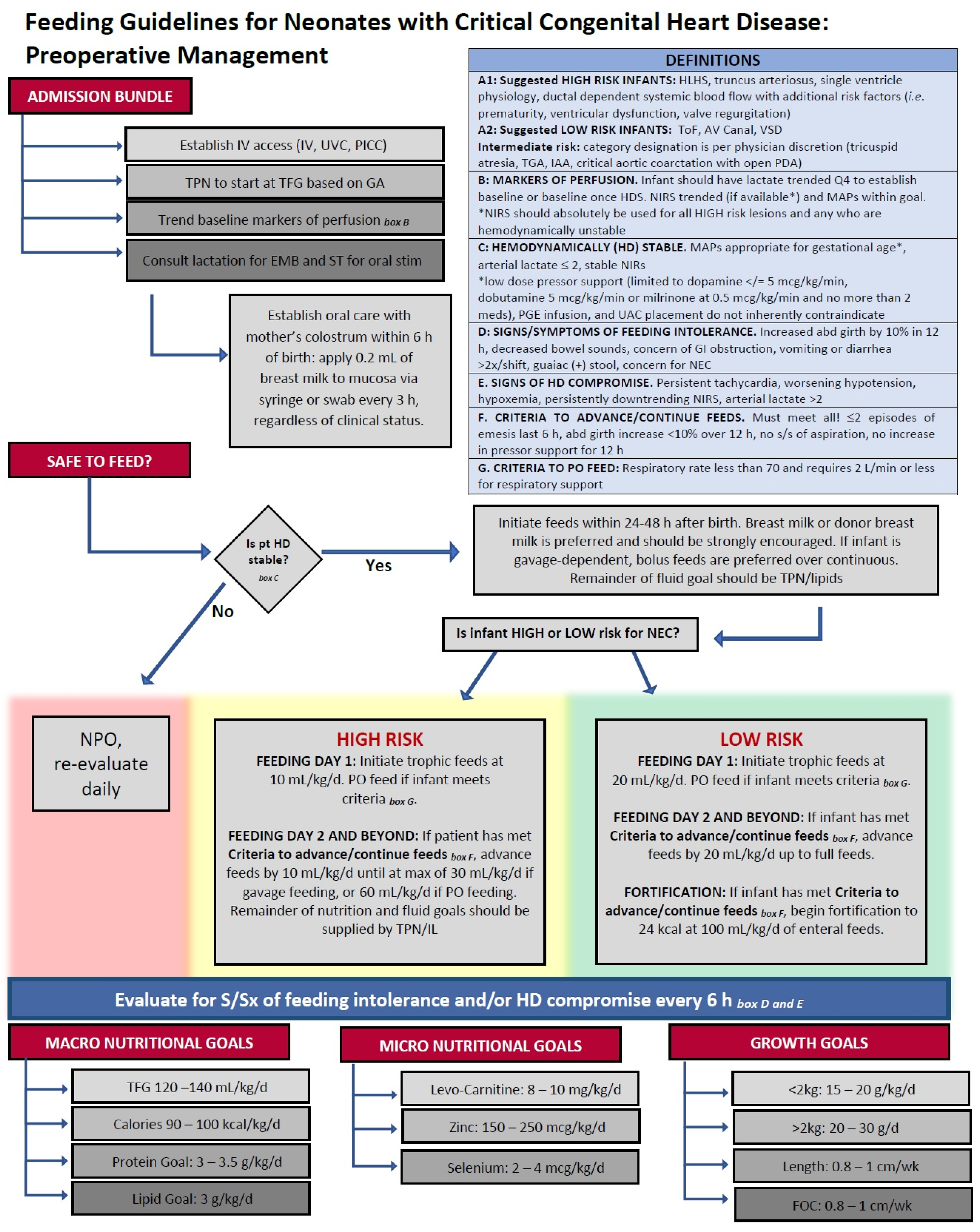
5. Practices for Initiation and Maintenance of Enteral Feeds in Infants with CHD
6. Potential Biomarkers for Cardiac NEC
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jones, I.H.; Hall, N.J. Contemporary Outcomes for Infants with Necrotizing Enterocolitis—A Systematic Review. J. Pediatr. 2020, 220, 86–92.e83. [Google Scholar] [CrossRef] [PubMed]
- Neu, J.; Walker, W.A. Necrotizing enterocolitis. N. Engl. J. Med. 2011, 364, 255–264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Motta, C.; Scott, W.; Mahony, L.; Koch, J.; Wyckoff, M.; Reisch, J.; Burchfield, P.J.; Brion, L.P. The association of congenital heart disease with necrotizing enterocolitis in preterm infants: A birth cohort study. J. Perinatol. 2015, 35, 949–953. [Google Scholar] [CrossRef] [Green Version]
- Baxi, A.C.; Josephson, C.D.; Iannucci, G.J.; Mahle, W.T. Necrotizing enterocolitis in infants with congenital heart disease: The role of red blood cell transfusions. Pediatr. Cardiol. 2014, 35, 1024–1029. [Google Scholar] [CrossRef] [PubMed]
- Velazco, C.S.; Fullerton, B.S.; Hong, C.R.; Morrow, K.A.; Edwards, E.M.; Soll, R.F.; Jaksic, T.; Horbar, J.D.; Modi, B.P. Morbidity and mortality among “big” babies who develop necrotizing enterocolitis: A prospective multicenter cohort analysis. J. Pediatr. Surg. 2018, 53, 108–112. [Google Scholar] [CrossRef]
- Polin, R.A.; Pollack, P.F.; Barlow, B.; Wigger, H.J.; Slovis, T.L.; Santulli, T.V.; Heird, W.C. Necrotizing enterocolitis in term infants. J. Pediatr. 1976, 89, 460–462. [Google Scholar] [CrossRef]
- Lau, P.E.; Cruz, S.M.; Ocampo, E.C.; Nuthakki, S.; Style, C.C.; Lee, T.C.; Wesson, D.E.; Olutoye, O.O. Necrotizing enterocolitis in patients with congenital heart disease: A single center experience. J. Pediatr. Surg. 2018, 53, 914–917. [Google Scholar] [CrossRef]
- Natarajan, G.; Anne, S.R.; Aggarwal, S. Outcomes of congenital heart disease in late preterm infants: Double jeopardy? Acta Paediatr. 2011, 100, 1104–1107. [Google Scholar] [CrossRef]
- Siano, E.; Lauriti, G.; Ceccanti, S.; Zani, A. Cardiogenic Necrotizing Enterocolitis: A Clinically Distinct Entity from Classical Necrotizing Enterocolitis. Eur. J. Pediatr. Surg. 2019, 29, 14–22. [Google Scholar] [CrossRef]
- McElhinney, D.B.; Hedrick, H.L.; Bush, D.M.; Pereira, G.R.; Stafford, P.W.; Gaynor, J.W.; Spray, T.L.; Wernovsky, G. Necrotizing enterocolitis in neonates with congenital heart disease: Risk factors and outcomes. Pediatrics 2000, 106, 1080–1087. [Google Scholar] [CrossRef]
- Leung, M.P.; Chau, K.T.; Hui, P.W.; Tam, A.Y.; Chan, F.L.; Lai, C.L.; Yeung, C.Y. Necrotizing enterocolitis in neonates with symptomatic congenital heart disease. J. Pediatr. 1988, 113, 1044–1046. [Google Scholar] [CrossRef]
- Scahill, C.J.; Graham, E.M.; Atz, A.M.; Bradley, S.M.; Kavarana, M.N.; Zyblewski, S.C. Preoperative Feeding Neonates with Cardiac Disease. World J. Pediatr. Congenit. Heart Surg. 2017, 8, 62–68. [Google Scholar] [CrossRef] [PubMed]
- ElHassan, N.O.; Tang, X.; Gossett, J.; Zakaria, D.; Ross, A.; Kona, S.K.; Prodhan, P. Necrotizing Enterocolitis in Infants with Hypoplastic Left Heart Syndrome following Stage 1 Palliation or Heart Transplant. Pediatr. Cardiol. 2018, 39, 774–785. [Google Scholar] [CrossRef]
- Steurer, M.A.; Baer, R.J.; Keller, R.L.; Oltman, S.; Chambers, C.D.; Norton, M.E.; Peyvandi, S.; Rand, L.; Rajagopal, S.; Ryckman, K.K.; et al. Gestational Age and Outcomes in Critical Congenital Heart Disease. Pediatrics 2017, 140, e20170999. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kelleher, S.T.; McMahon, C.J.; James, A. Necrotizing Enterocolitis in Children with Congenital Heart Disease: A Literature Review. Pediatr. Cardiol. 2021, 42, 1688–1699. [Google Scholar] [CrossRef] [PubMed]
- Bubberman, J.M.; van Zoonen, A.; Bruggink, J.L.M.; van der Heide, M.; Berger, R.M.F.; Bos, A.F.; Kooi, E.M.W.; Hulscher, J.B.F. Necrotizing Enterocolitis Associated with Congenital Heart Disease: A Different Entity? J. Pediatr. Surg. 2019, 54, 1755–1760. [Google Scholar] [CrossRef] [PubMed]
- Partridge, E.; Rintoul, N. Congenital heart disease (CHD) and necrotizing enterocolitis (NEC). Prog. Pediatr. Cardiol. 2019, 54, 101146. [Google Scholar] [CrossRef]
- Frid, G.; Reppucci, M.; Lum, T.; Paul, M.; Seiden, H.; Coakley, B.A. Comparison of Necrotizing Enterocolitis in Pre-mature Infants vs. Term-Born Infants with Congenital Heart Disease. Front. Pediatr. 2021, 9, 802607. [Google Scholar] [CrossRef]
- Cozzi, C.; Aldrink, J.; Nicol, K.; Nicholson, L.; Cua, C. Intestinal location of necrotizing enterocolitis among infants with congenital heart disease. J. Perinatol. 2013, 33, 783–785. [Google Scholar] [CrossRef]
- Sharma, R.; Hudak, M.L. A clinical perspective of necrotizing enterocolitis: Past, present, and future. Clin. Perinatol. 2013, 40, 27–51. [Google Scholar] [CrossRef]
- Diez, S.; Besendörfer, M.; Weyerer, V.; Hartmann, A.; Moosmann, J.; Weiss, C.; Renner, M.; Müller, H. DMBT1 expression and neutrophil-to-lymphocyte ratio during necrotizing enterocolitis are influenced by impaired perfusion due to cardiac anomalies. Mol. Cell. Pediatr. 2022, 9, 1. [Google Scholar] [CrossRef] [PubMed]
- Becker, K.C.; Hornik, C.P.; Cotten, C.M.; Clark, R.H.; Hill, K.D.; Smith, P.B.; Lenfestey, R.W. Necrotizing enterocolitis in infants with ductal-dependent congenital heart disease. Am. J. Perinatol. 2015, 32, 633–638. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Overman, R.E., Jr.; Criss, C.N.; Gadepalli, S.K. Necrotizing enterocolitis in term neonates: A different disease process? J. Pediatr. Surg. 2019, 54, 1143–1146. [Google Scholar] [CrossRef]
- Iannucci, G.J.; Oster, M.E.; Mahle, W.T. Necrotising enterocolitis in infants with congenital heart disease: The role of enteral feeds. Cardiol. Young 2013, 23, 553–559. [Google Scholar] [CrossRef]
- Buck, M.L. Prostaglandin E1 treatment of congenital heart disease: Use prior to neonatal transport. DICP 1991, 25, 408–409. [Google Scholar] [CrossRef]
- Pickard, S.S.; Feinstein, J.A.; Popat, R.A.; Huang, L.; Dutta, S. Short- and long-term outcomes of necrotizing enterocolitis in infants with congenital heart disease. Pediatrics 2009, 123, e901–e906. [Google Scholar] [CrossRef]
- Fisher, J.G.; Bairdain, S.; Sparks, E.A.; Khan, F.A.; Archer, J.M.; Kenny, M.; Edwards, E.M.; Soll, R.F.; Modi, B.P.; Yeager, S.; et al. Serious congenital heart disease and necrotizing enterocolitis in very low birth weight neonates. J. Am. Coll. Surg. 2015, 220, 1018–1026.e1014. [Google Scholar] [CrossRef] [PubMed]
- Kessler, U.; Hau, E.M.; Kordasz, M.; Haefeli, S.; Tsai, C.; Klimek, P.; Cholewa, D.; Nelle, M.; Pavlovic, M.; Berger, S. Congenital Heart Disease Increases Mortality in Neonates with Necrotizing Enterocolitis. Front. Pediatr. 2018, 6, 312. [Google Scholar] [CrossRef] [Green Version]
- Cheng, W.; Leung, M.P.; Tam, P.K. Surgical intervention in necrotizing enterocolitis in neonates with symptomatic congenital heart disease. Pediatr. Surg. Int. 1999, 15, 492–495. [Google Scholar] [CrossRef] [Green Version]
- Bazacliu, C.; Neu, J. Pathophysiology of Necrotizing Enterocolitis: An Update. Curr. Pediatr. Rev. 2019, 15, 68–87. [Google Scholar] [CrossRef]
- Carlo, W.F.; Kimball, T.R.; Michelfelder, E.C.; Border, W.L. Persistent diastolic flow reversal in abdominal aortic Doppler-flow profiles is associated with an increased risk of necrotizing enterocolitis in term infants with congenital heart disease. Pediatrics 2007, 119, 330–335. [Google Scholar] [CrossRef] [PubMed]
- Harrison, A.M.; Davis, S.; Reid, J.R.; Morrison, S.C.; Arrigain, S.; Connor, J.T.; Temple, M.E. Neonates with hypoplastic left heart syndrome have ultrasound evidence of abnormal superior mesenteric artery perfusion before and after modified Norwood procedure. Pediatr. Crit. Care Med. 2005, 6, 445–447. [Google Scholar] [CrossRef] [PubMed]
- DeWitt, A.G.; Charpie, J.R.; Donohue, J.E.; Yu, S.; Owens, G.E. Splanchnic near-infrared spectroscopy and risk of necrotizing enterocolitis after neonatal heart surgery. Pediatr. Cardiol. 2014, 35, 1286–1294. [Google Scholar] [CrossRef] [Green Version]
- Miller, T.A.; Minich, L.L.; Lambert, L.M.; Joss-Moore, L.; Puchalski, M.D. Abnormal abdominal aorta hemodynamics are associated with necrotizing enterocolitis in infants with hypoplastic left heart syndrome. Pediatr. Cardiol. 2014, 35, 616–621. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van der Heide, M.; Mebius, M.J.; Bos, A.F.; Roofthooft, M.T.R.; Berger, R.M.F.; Hulscher, J.B.F.; Kooi, E.M.W. Hypoxic/ischemic hits predispose to necrotizing enterocolitis in (near) term infants with congenital heart disease: A case control study. BMC Pediatr. 2020, 20, 553. [Google Scholar] [CrossRef]
- Bowker, R.M.; Yan, X.; De Plaen, I.G. Intestinal microcirculation and necrotizing enterocolitis: The vascular endothelial growth factor system. Semin. Fetal Neonatal Med. 2018, 23, 411–415. [Google Scholar] [CrossRef]
- Klinke, M.; Wiskemann, H.; Bay, B.; Schäfer, H.J.; Pagerols Raluy, L.; Reinshagen, K.; Vincent, D.; Boettcher, M. Cardiac and Inflammatory Necrotizing Enterocolitis in Newborns Are Not the Same Entity. Front. Pediatr. 2020, 8, 593926. [Google Scholar] [CrossRef]
- Chang, M.; Alsaigh, T.; Kistler, E.B.; Schmid-Schönbein, G.W. Breakdown of mucin as barrier to digestive enzymes in the ischemic rat small intestine. PLoS ONE 2012, 7, e40087. [Google Scholar] [CrossRef] [Green Version]
- Pathan, N.; Burmester, M.; Adamovic, T.; Berk, M.; Ng, K.W.; Betts, H.; Macrae, D.; Waddell, S.; Paul-Clark, M.; Nuamah, R.; et al. Intestinal injury and endotoxemia in children undergoing surgery for congenital heart disease. Am. J. Respir. Crit. Care Med. 2011, 184, 1261–1269. [Google Scholar] [CrossRef]
- Malagon, I.; Onkenhout, W.; Klok, M.; van der Poel, P.F.; Bovill, J.G.; Hazekamp, M.G. Gut permeability in neonates after a stage 1 Norwood procedure. Pediatr. Crit. Care Med. 2005, 6, 547–549. [Google Scholar] [CrossRef]
- Wienecke, L.M.; Cohen, S.; Bauersachs, J.; Mebazaa, A.; Chousterman, B.G. Immunity and inflammation: The neglected key players in congenital heart disease? Heart Fail. Rev. 2021, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Lequier, L.L.; Nikaidoh, H.; Leonard, S.R.; Bokovoy, J.L.; White, M.L.; Scannon, P.J.; Giroir, B.P. Preoperative and postoperative endotoxemia in children with congenital heart disease. Chest 2000, 117, 1706–1712. [Google Scholar] [CrossRef] [PubMed]
- Malagon, I.; Onkenhout, W.; Klok, G.; van der Poel, P.F.; Bovill, J.G.; Hazekamp, M.G. Gut permeability in paediatric cardiac surgery. Br. J. Anaesth. 2005, 94, 181–185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chaaban, H.; Stonestreet, B.S. Intestinal hemodynamics and oxygenation in the perinatal period. Semin. Perinatol. 2012, 36, 260–268. [Google Scholar] [CrossRef] [PubMed]
- Nankervis, C.A.; Giannone, P.J.; Reber, K.M. The neonatal intestinal vasculature: Contributing factors to necrotizing enterocolitis. Semin. Perinatol. 2008, 32, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Nankervis, C.A.; Nowicki, P.T. Role of nitric oxide in regulation of vascular resistance in postnatal intestine. Am. J. Physiol. 1995, 268, G949–G958. [Google Scholar] [CrossRef] [PubMed]
- Nowicki, P.T.; Miller, C.E. Flow-induced dilation in newborn intestine. Pediatr. Res. 1995, 38, 783–791. [Google Scholar] [CrossRef] [Green Version]
- Nankervis, C.A.; Reber, K.M.; Nowicki, P.T. Age-dependent changes in the postnatal intestinal microcirculation. Microcirculation 2001, 8, 377–387. [Google Scholar] [CrossRef]
- González, R.; Urbano, J.; Solana, M.J.; Hervías, M.; Pita, A.; Pérez, R.; Álvarez, R.; Teigell, E.; Gil-Jaurena, J.M.; Zamorano, J.; et al. Microcirculatory Differences in Children with Congenital Heart Disease according to Cyanosis and Age. Front. Pediatr. 2019, 7, 264. [Google Scholar] [CrossRef]
- Granger, D.N.; Seifert, H.; Senchenkova, E. Intestinal Ischemia and Reperfusion: Consequences and Mechanisms. In PanVascular Medicine; Lanzer, P., Ed.; Springer: Berlin/Heidelberg, Germany, 2015; pp. 3535–3553. [Google Scholar]
- Nino, D.F.; Sodhi, C.P.; Hackam, D.J. Necrotizing enterocolitis: New insights into pathogenesis and mechanisms. Nat. Rev. Gastroenterol. Hepatol. 2016, 13, 590–600. [Google Scholar] [CrossRef] [Green Version]
- Feng, D.; Christensen, J.T.; Yetman, A.T.; Lindsey, M.L.; Singh, A.B.; Salomon, J.D. The microbiome’s relationship with congenital heart disease: More than a gut feeling. J. Congenital. Cardiol. 2021, 5, 5. [Google Scholar] [CrossRef]
- Ellis, C.L.; Bokulich, N.A.; Kalanetra, K.M.; Mirmiran, M.; Elumalai, J.; Haapanen, L.; Schegg, T.; Rutledge, J.C.; Raff, G.; Mills, D.A.; et al. Probiotic administration in congenital heart disease: A pilot study. J. Perinatol. 2013, 33, 691–697. [Google Scholar] [CrossRef] [PubMed]
- Umenai, T.; Shime, N.; Asahara, T.; Nomoto, K.; Itoi, T. A pilot study of Bifidobacterium breve in neonates undergoing surgery for congenital heart disease. J. Intensive Care 2014, 2, 36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- D’Ignazio, L.; Bandarra, D.; Rocha, S. NF-κB and HIF crosstalk in immune responses. FEBS J. 2016, 283, 413–424. [Google Scholar] [CrossRef] [Green Version]
- Zeitouni, N.E.; Chotikatum, S.; von Köckritz-Blickwede, M.; Naim, H.Y. The impact of hypoxia on intestinal epithelial cell functions: Consequences for invasion by bacterial pathogens. Mol. Cell. Pediatr. 2016, 3, 14. [Google Scholar] [CrossRef] [Green Version]
- Park, A.M.; Sanders, T.A.; Maltepe, E. Hypoxia-inducible factor (HIF) and HIF-stabilizing agents in neonatal care. Semin. Fetal Neonatal Med. 2010, 15, 196–202. [Google Scholar] [CrossRef] [Green Version]
- Maheshwari, A.; Patel, R.M.; Christensen, R.D. Anemia, red blood cell transfusions, and necrotizing enterocolitis. Semin. Pediatr. Surg. 2018, 27, 47–51. [Google Scholar] [CrossRef]
- Bain, J.; Benjamin, D.K., Jr.; Hornik, C.P.; Benjamin, D.K.; Clark, R.; Smith, P.B. Risk of necrotizing enterocolitis in very-low-birth-weight infants with isolated atrial and ventricular septal defects. J. Perinatol. 2014, 34, 319–321. [Google Scholar] [CrossRef] [Green Version]
- Jenkins, K.J. Risk adjustment for congenital heart surgery: The RACHS-1 method. Semin. Thorac. Cardiovasc. Surg. Pediatr. Card. Surg. Annu. 2004, 7, 180–184. [Google Scholar] [CrossRef]
- Rai, S.E.; Sidhu, A.K.; Krishnan, R.J. Transfusion-associated necrotizing enterocolitis re-evaluated: A systematic review and meta-analysis. J. Perinat. Med. 2018, 46, 665–676. [Google Scholar] [CrossRef]
- Cunningham, K.E.; Okolo, F.C.; Baker, R.; Mollen, K.P.; Good, M. Red blood cell transfusion in premature infants leads to worse necrotizing enterocolitis outcomes. J. Surg. Res. 2017, 213, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Huggard, D.; Doherty, D.G.; Molloy, E.J. Immune Dysregulation in Children with Down Syndrome. Front. Pediatr. 2020, 8, 73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holmes, G. Gastrointestinal disorders in Down syndrome. Gastroenterol. Hepatol. Bed Bench 2014, 7, 6–8. [Google Scholar] [PubMed]
- Cua, C.L.; Haque, U.; Miao, Y.; Backes, C.H. Necrotizing Enterocolitis Incidence, Characteristics, and Outcomes in Neonatal Down Syndrome Patients. Am. J. Perinatol. 2017, 34, 1368–1374. [Google Scholar] [CrossRef] [PubMed]
- Boghossian, N.S.; Hansen, N.I.; Bell, E.F.; Stoll, B.J.; Murray, J.C.; Laptook, A.R.; Shankaran, S.; Walsh, M.C.; Das, A.; Higgins, R.D. Survival and morbidity outcomes for very low birth weight infants with Down syndrome. Pediatrics 2010, 126, 1132–1140. [Google Scholar] [CrossRef] [Green Version]
- Ni She, R.; Filan, P.M. Trisomy 21—Incidence and outcomes in the first year, in Ireland today. Ir. Med. J. 2014, 107, 248–249. [Google Scholar]
- Lopez, N.L.; Gowda, C.; Backes, C.H.; Nandi, D.; Miller-Tate, H.; Fichtner, S.; Allen, R.; Stewart, J.; Cua, C.L. Differences in midterm outcomes in infants with hypoplastic left heart syndrome diagnosed with necrotizing enterocolitis: NPCQIC database analysis. Congenit. Heart Dis. 2018, 13, 512–518. [Google Scholar] [CrossRef]
- Ohye, R.G.; Sleeper, L.A.; Mahony, L.; Newburger, J.W.; Pearson, G.D.; Lu, M.; Goldberg, C.S.; Tabbutt, S.; Frommelt, P.C.; Ghanayem, N.S.; et al. Comparison of shunt types in the Norwood procedure for single-ventricle lesions. N. Engl. J. Med. 2010, 362, 1980–1992. [Google Scholar] [CrossRef]
- Jeffries, H.E.; Wells, W.J.; Starnes, V.A.; Wetzel, R.C.; Moromisato, D.Y. Gastrointestinal morbidity after Norwood palliation for hypoplastic left heart syndrome. Ann. Thorac. Surg. 2006, 81, 982–987. [Google Scholar] [CrossRef]
- Cua, C.L.; Thiagarajan, R.R.; Gauvreau, K.; Lai, L.; Costello, J.M.; Wessel, D.L.; Del Nido, P.J.; Mayer, J.E., Jr.; Newburger, J.W.; Laussen, P.C. Early postoperative outcomes in a series of infants with hypoplastic left heart syndrome undergoing stage I palliation operation with either modified Blalock-Taussig shunt or right ventricle to pulmonary artery conduit. Pediatr. Crit. Care Med. 2006, 7, 238–244. [Google Scholar] [CrossRef] [Green Version]
- Pizarro, C.; Malec, E.; Maher, K.O.; Januszewska, K.; Gidding, S.S.; Murdison, K.A.; Baffa, J.M.; Norwood, W.I. Right ventricle to pulmonary artery conduit improves outcome after stage I Norwood for hypoplastic left heart syndrome. Circulation 2003, 108 (Suppl. S1), II155–II160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnson, J.N.; Ansong, A.K.; Li, J.S.; Xu, M.; Gorentz, J.; Hehir, D.A.; del Castillo, S.L.; Lai, W.W.; Uzark, K.; Pasquali, S.K. Celiac artery flow pattern in infants with single right ventricle following the Norwood procedure with a modified Blalock-Taussig or right ventricle to pulmonary artery shunt. Pediatr. Cardiol. 2011, 32, 479–486. [Google Scholar] [CrossRef] [Green Version]
- Torres, A., Jr. Classic Norwood versus Sano modification versus hybrid approach: Necrotizing enterocolitis or no necrotizing enterocolitis? Pediatr. Crit. Care Med. 2011, 12, 109–110. [Google Scholar] [CrossRef] [PubMed]
- del Castillo, S.L.; McCulley, M.E.; Khemani, R.G.; Jeffries, H.E.; Thomas, D.W.; Peregrine, J.; Wells, W.J.; Starnes, V.A.; Moromisato, D.Y. Reducing the incidence of necrotizing enterocolitis in neonates with hypoplastic left heart syndrome with the introduction of an enteral feed protocol. Pediatr. Crit. Care Med. 2010, 11, 373–377. [Google Scholar] [CrossRef] [PubMed]
- Weiss, S.L.; Gossett, J.G.; Kaushal, S.; Wang, D.; Backer, C.L.; Wald, E.L. Comparison of gastrointestinal morbidity after Norwood and hybrid palliation for complex heart defects. Pediatr. Cardiol. 2011, 32, 391–398. [Google Scholar] [CrossRef] [PubMed]
- Brinkmann, V.; Reichard, U.; Goosmann, C.; Fauler, B.; Uhlemann, Y.; Weiss, D.S.; Weinrauch, Y.; Zychlinsky, A. Neutrophil extracellular traps kill bacteria. Science 2004, 303, 1532–1535. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Zhang, G.; Benson, L.; Holtby, H.; Cai, S.; Humpl, T.; Van Arsdell, G.S.; Redington, A.N.; Caldarone, C.A. Comparison of the profiles of postoperative systemic hemodynamics and oxygen transport in neonates after the hybrid or the Norwood procedure: A pilot study. Circulation 2007, 116, I179–I187. [Google Scholar] [CrossRef] [Green Version]
- Luce, W.A.; Schwartz, R.M.; Beauseau, W.; Giannone, P.J.; Boettner, B.L.; Cheatham, J.P.; Galantowicz, M.E.; Cua, C.L. Necrotizing enterocolitis in neonates undergoing the hybrid approach to complex congenital heart disease. Pediatr. Crit. Care Med. 2011, 12, 46–51. [Google Scholar] [CrossRef]
- Schranz, D.; Esmaeili, A.; Akintuerk, H. Hypoplastic Left Heart: Stage-I Will be Performed Interventionally, Soon. Pediatr. Cardiol. 2021, 42, 727–735. [Google Scholar] [CrossRef]
- Ou, J.; Courtney, C.M.; Steinberger, A.E.; Tecos, M.E.; Warner, B.W. Nutrition in Necrotizing Enterocolitis and following Intestinal Resection. Nutrients 2020, 12, 520. [Google Scholar] [CrossRef] [Green Version]
- Colgan, S.P.; Taylor, C.T. Hypoxia: An alarm signal during intestinal inflammation. Nat. Rev. Gastroenterol. Hepatol. 2010, 7, 281–287. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cognata, A.; Kataria-Hale, J.; Griffiths, P.; Maskatia, S.; Rios, D.; O’Donnell, A.; Roddy, D.J.; Mehollin-Ray, A.; Hagan, J.; Placencia, J.; et al. Human Milk Use in the Preoperative Period Is Associated with a Lower Risk for Necrotizing Enterocolitis in Neonates with Complex Congenital Heart Disease. J. Pediatr. 2019, 215, 11–16.e12. [Google Scholar] [CrossRef] [PubMed]
- Burge, K.; Eckert, J.; Wilson, A.; Trammell, M.; Lueschow, S.R.; McElroy, S.J.; Dyer, D.; Chaaban, H. Hyaluronic Acid 35 kDa Protects against a Hyperosmotic, Formula Feeding Model of Necrotizing Enterocolitis. Nutrients 2022, 14, 1779. [Google Scholar] [CrossRef] [PubMed]
- Lueschow, S.R.; Kern, S.L.; Gong, H.; Grobe, J.L.; Segar, J.L.; Carlson, S.J.; McElroy, S.J. Feeding Formula Eliminates the Necessity of Bacterial Dysbiosis and Induces Inflammation and Injury in the Paneth Cell Disruption Murine NEC Model in an Osmolality-Dependent Manner. Nutrients 2020, 12, 900. [Google Scholar] [CrossRef] [Green Version]
- Pearson, F.; Johnson, M.J.; Leaf, A.A. Milk osmolality: Does it matter? Arch. Dis. Child. Fetal Neonatal Ed. 2013, 98, F166–F169. [Google Scholar] [CrossRef]
- Malhotra, A.; Veldman, A.; Menahem, S. Does milk fortification increase the risk of necrotising enterocolitis in preterm infants with congenital heart disease? Cardiol. Young 2013, 23, 450–453. [Google Scholar] [CrossRef]
- Day, T.G.; Dionisio, D.; Zannino, D.; Brizard, C.; Cheung, M.M.H. Enteral feeding in duct-dependent congenital heart disease. J. Neonatal-Perinat. Med. 2019, 12, 9–12. [Google Scholar] [CrossRef]
- Kataria-Hale, J.; Osborne, S.W.; Hair, A.; Hagan, J.; Pammi, M. Preoperative Feeds in Ductal-Dependent Cardiac Disease: A Systematic Review and Meta-analysis. Hosp. Pediatr. 2019, 9, 998–1006. [Google Scholar] [CrossRef]
- Cheung, Y.F.; Ho, M.H.; Cheng, V.Y. Mesenteric blood flow response to feeding after systemic-to-pulmonary arterial shunt palliation. Ann. Thorac. Surg. 2003, 75, 947–951. [Google Scholar] [CrossRef]
- Toms, R.; Jackson, K.W.; Dabal, R.J.; Reebals, C.H.; Alten, J.A. Preoperative trophic feeds in neonates with hypoplastic left heart syndrome. Congenit. Heart Dis. 2015, 10, 36–42. [Google Scholar] [CrossRef]
- Slicker, J.; Sables-Baus, S.; Lambert, L.M.; Peterson, L.E.; Woodard, F.K.; Ocampo, E.C. Perioperative Feeding Approaches in Single Ventricle Infants: A Survey of 46 Centers. Congenit. Heart Dis. 2016, 11, 707–715. [Google Scholar] [CrossRef] [PubMed]
- Fallon, E.M.; Nehra, D.; Potemkin, A.K.; Gura, K.M.; Simpser, E.; Compher, C.; Puder, M.A.S.P.E.N. clinical guidelines: Nutrition support of neonatal patients at risk for necrotizing enterocolitis. J. Parenter. Enteral. Nutr. 2012, 36, 506–523. [Google Scholar] [CrossRef] [PubMed]
- Tume, L.N.; Balmaks, R.; da Cruz, E.; Latten, L.; Verbruggen, S.; Valla, F.V. Enteral Feeding Practices in Infants With Congenital Heart Disease Across European PICUs: A European Society of Pediatric and Neonatal Intensive Care Survey. Pediatr. Crit. Care Med. 2018, 19, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Karpen, H.E. Nutrition in the Cardiac Newborns: Evidence-based Nutrition Guidelines for Cardiac Newborns. Clin. Perinatol. 2016, 43, 131–145. [Google Scholar] [CrossRef] [PubMed]
- McCallie, K.R.; Lee, H.C.; Mayer, O.; Cohen, R.S.; Hintz, S.R.; Rhine, W.D. Improved outcomes with a standardized feeding protocol for very low birth weight infants. J. Perinatol. 2011, 31 (Suppl. S1), S61–S67. [Google Scholar] [CrossRef] [PubMed]
- Furlong-Dillard, J.; Neary, A.; Marietta, J.; Jones, C.; Jeffers, G.; Gakenheimer, L.; Puchalski, M.; Eckauser, A.; Delgado-Corcoran, C. Evaluating the Impact of a Feeding Protocol in Neonates before and after Biventricular Cardiac Surgery. Pediatr. Qual. Saf. 2018, 3, e080. [Google Scholar] [CrossRef]
- Patole, S.K.; de Klerk, N. Impact of standardised feeding regimens on incidence of neonatal necrotising enterocolitis: A systematic review and meta-analysis of observational studies. Arch. Dis. Child. Fetal Neonatal Ed. 2005, 90, F147–F151. [Google Scholar] [CrossRef]
- Martini, S.; Beghetti, I.; Annunziata, M.; Aceti, A.; Galletti, S.; Ragni, L.; Donti, A.; Corvaglia, L. Enteral Nutrition in Term Infants with Congenital Heart Disease: Knowledge Gaps and Future Directions to Improve Clinical Practice. Nutrients 2021, 13, 932. [Google Scholar] [CrossRef]
- Tume, L.N.; Valla, F.V.; Joosten, K.; Jotterand Chaparro, C.; Latten, L.; Marino, L.V.; Macleod, I.; Moullet, C.; Pathan, N.; Rooze, S.; et al. Nutritional support for children during critical illness: European Society of Pediatric and Neonatal Intensive Care (ESPNIC) metabolism, endocrine and nutrition section position statement and clinical recommendations. Intensive Care Med. 2020, 46, 411–425. [Google Scholar] [CrossRef] [Green Version]
- Strobel, A.M.; Lu le, N. The Critically Ill Infant with Congenital Heart Disease. Emerg. Med. Clin. N. Am. 2015, 33, 501–518. [Google Scholar] [CrossRef]
- Slicker, J.; Hehir, D.A.; Horsley, M.; Monczka, J.; Stern, K.W.; Roman, B.; Ocampo, E.C.; Flanagan, L.; Keenan, E.; Lambert, L.M.; et al. Nutrition algorithms for infants with hypoplastic left heart syndrome; birth through the first interstage period. Congenit. Heart Dis. 2013, 8, 89–102. [Google Scholar] [CrossRef] [PubMed]
- Kataria-Hale, J.; Roddy, D.J.; Cognata, A.; Hochevar, P.; Zender, J.; Sheaks, P.; Osborne, S.; Tucker, K.; Hurst, N.; Hagan, J.; et al. A preoperative standardized feeding protocol improves human milk use in infants with complex congenital heart disease. J. Perinatol. 2021, 41, 590–597. [Google Scholar] [CrossRef] [PubMed]
- Alten, J.A.; Rhodes, L.A.; Tabbutt, S.; Cooper, D.S.; Graham, E.M.; Ghanayem, N.; Marino, B.S.; Figueroa, M.I.; Chanani, N.K.; Jacobs, J.P.; et al. Perioperative feeding management of neonates with CHD: Analysis of the Pediatric Cardiac Critical Care Consortium (PC4) registry. Cardiol. Young 2015, 25, 1593–1601. [Google Scholar] [CrossRef]
- Larsen, B.M.; Goonewardene, L.A.; Field, C.J.; Joffe, A.R.; Van Aerde, J.E.; Olstad, D.L.; Clandinin, M.T. Low energy intakes are associated with adverse outcomes in infants after open heart surgery. JPEN J. Parenter. Enteral. Nutr. 2013, 37, 254–260. [Google Scholar] [CrossRef] [PubMed]
- Curzon, C.L.; Milford-Beland, S.; Li, J.S.; O’Brien, S.M.; Jacobs, J.P.; Jacobs, M.L.; Welke, K.F.; Lodge, A.J.; Peterson, E.D.; Jaggers, J. Cardiac surgery in infants with low birth weight is associated with increased mortality: Analysis of the Society of Thoracic Surgeons Congenital Heart Database. J. Thorac. Cardiovasc. Surg. 2008, 135, 546–551. [Google Scholar] [CrossRef] [Green Version]
- Schwalbe-Terilli, C.R.; Hartman, D.H.; Nagle, M.L.; Gallagher, P.R.; Ittenbach, R.F.; Burnham, N.B.; Gaynor, J.W.; Ravishankar, C. Enteral feeding and caloric intake in neonates after cardiac surgery. Am. J. Crit. Care 2009, 18, 52–57. [Google Scholar] [CrossRef] [Green Version]
- Sahu, M.K.; Singal, A.; Menon, R.; Singh, S.P.; Mohan, A.; Manral, M.; Singh, D.; Devagouru, V.; Talwar, S.; Choudhary, S.K. Early enteral nutrition therapy in congenital cardiac repair postoperatively: A randomized, controlled pilot study. Ann. Card. Anaesth. 2016, 19, 653–661. [Google Scholar] [CrossRef]
- Floh, A.A.; Nakada, M.; La Rotta, G.; Mah, K.; Herridge, J.E.; Van Arsdell, G.; Schwartz, S.M. Systemic inflammation increases energy expenditure following pediatric cardiopulmonary bypass. Pediatr. Crit. Care Med. 2015, 16, 343–351. [Google Scholar] [CrossRef]
- Gebara, B.M.; Gelmini, M.; Sarnaik, A. Oxygen consumption, energy expenditure, and substrate utilization after cardiac surgery in children. Crit. Care Med. 1992, 20, 1550–1554. [Google Scholar] [CrossRef]
- Alfares, F.A.; Hynes, C.F.; Ansari, G.; Chounoune, R.; Ramadan, M.; Shaughnessy, C.; Reilly, B.K.; Zurakowski, D.; Jonas, R.A.; Nath, D.S. Outcomes of recurrent laryngeal nerve injury following congenital heart surgery: A contemporary experience. J. Saudi Heart Assoc. 2016, 28, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Garcia, X.; Jaquiss, R.D.; Imamura, M.; Swearingen, C.J.; Dassinger, M.S., 3rd; Sachdeva, R. Preemptive gastrostomy tube placement after Norwood operation. J. Pediatr. 2011, 159, 602–607.e601. [Google Scholar] [CrossRef] [PubMed]
- Thuijls, G.; Derikx, J.P.; van Wijck, K.; Zimmermann, L.J.; Degraeuwe, P.L.; Mulder, T.L.; Van der Zee, D.C.; Brouwers, H.A.; Verhoeven, B.H.; van Heurn, L.W.; et al. Non-invasive markers for early diagnosis and determination of the severity of necrotizing enterocolitis. Ann. Surg. 2010, 251, 1174–1180. [Google Scholar] [CrossRef] [PubMed]
- Heida, F.H.; Hulscher, J.B.; Schurink, M.; Timmer, A.; Kooi, E.M.; Bos, A.F.; Bruggink, J.L.; Kasper, D.C.; Pones, M.; Benkoe, T. Intestinal fatty acid-binding protein levels in Necrotizing Enterocolitis correlate with extent of necrotic bowel: Results from a multicenter study. J. Pediatr. Surg. 2015, 50, 1115–1118. [Google Scholar] [CrossRef] [PubMed]
- Watson, J.D.; Urban, T.T.; Tong, S.S.; Zenge, J.; Khailova, L.; Wischmeyer, P.E.; Davidson, J.A. Immediate Post-operative Enterocyte Injury, as Determined by Increased Circulating Intestinal Fatty Acid Binding Protein, Is Associated with Subsequent Development of Necrotizing Enterocolitis after Infant Cardiothoracic Surgery. Front. Pediatr. 2020, 8, 267. [Google Scholar] [CrossRef] [PubMed]
- Pergialiotis, V.; Konstantopoulos, P.; Karampetsou, N.; Koutaki, D.; Gkioka, E.; Perrea, D.N.; Papantoniou, N. Calprotectin levels in necrotizing enterocolitis: A systematic review of the literature. Inflamm. Res. 2016, 65, 847–852. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, G.; Brown, K.L.; Taylor, A.M. Faecal calprotectin concentrations in neonates with CHD: Pilot study. Cardiol. Young 2020, 30, 624–628. [Google Scholar] [CrossRef] [PubMed]
| Cardiac NEC Risk Factors |
|---|
| Premature birth (<37 wk gestation) |
| Low birth weight (<2500 g) |
| High preoperative risk assessment scores (e.g., RACHS-1) |
| Red blood cell transfusions |
| Trisomy 21 diagnosis |
| Specific CHD pathologies (HLHS, AVSD, TA, APW) |
| Potential Cardiac NEC Biomarkers |
|---|
| Intestinal fatty acid binding protein (IFABP) |
| Fecal calprotectin |
| Endotoxin activity |
| Serum lactate |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Burge, K.Y.; Gunasekaran, A.; Makoni, M.M.; Mir, A.M.; Burkhart, H.M.; Chaaban, H. Clinical Characteristics and Potential Pathogenesis of Cardiac Necrotizing Enterocolitis in Neonates with Congenital Heart Disease: A Narrative Review. J. Clin. Med. 2022, 11, 3987. https://doi.org/10.3390/jcm11143987
Burge KY, Gunasekaran A, Makoni MM, Mir AM, Burkhart HM, Chaaban H. Clinical Characteristics and Potential Pathogenesis of Cardiac Necrotizing Enterocolitis in Neonates with Congenital Heart Disease: A Narrative Review. Journal of Clinical Medicine. 2022; 11(14):3987. https://doi.org/10.3390/jcm11143987
Chicago/Turabian StyleBurge, Kathryn Y., Aarthi Gunasekaran, Marjorie M. Makoni, Arshid M. Mir, Harold M. Burkhart, and Hala Chaaban. 2022. "Clinical Characteristics and Potential Pathogenesis of Cardiac Necrotizing Enterocolitis in Neonates with Congenital Heart Disease: A Narrative Review" Journal of Clinical Medicine 11, no. 14: 3987. https://doi.org/10.3390/jcm11143987






