Assistive Technology in Multiple Sclerosis Patients—Two Points of View
Abstract
:1. Introduction
2. Materials and Methods
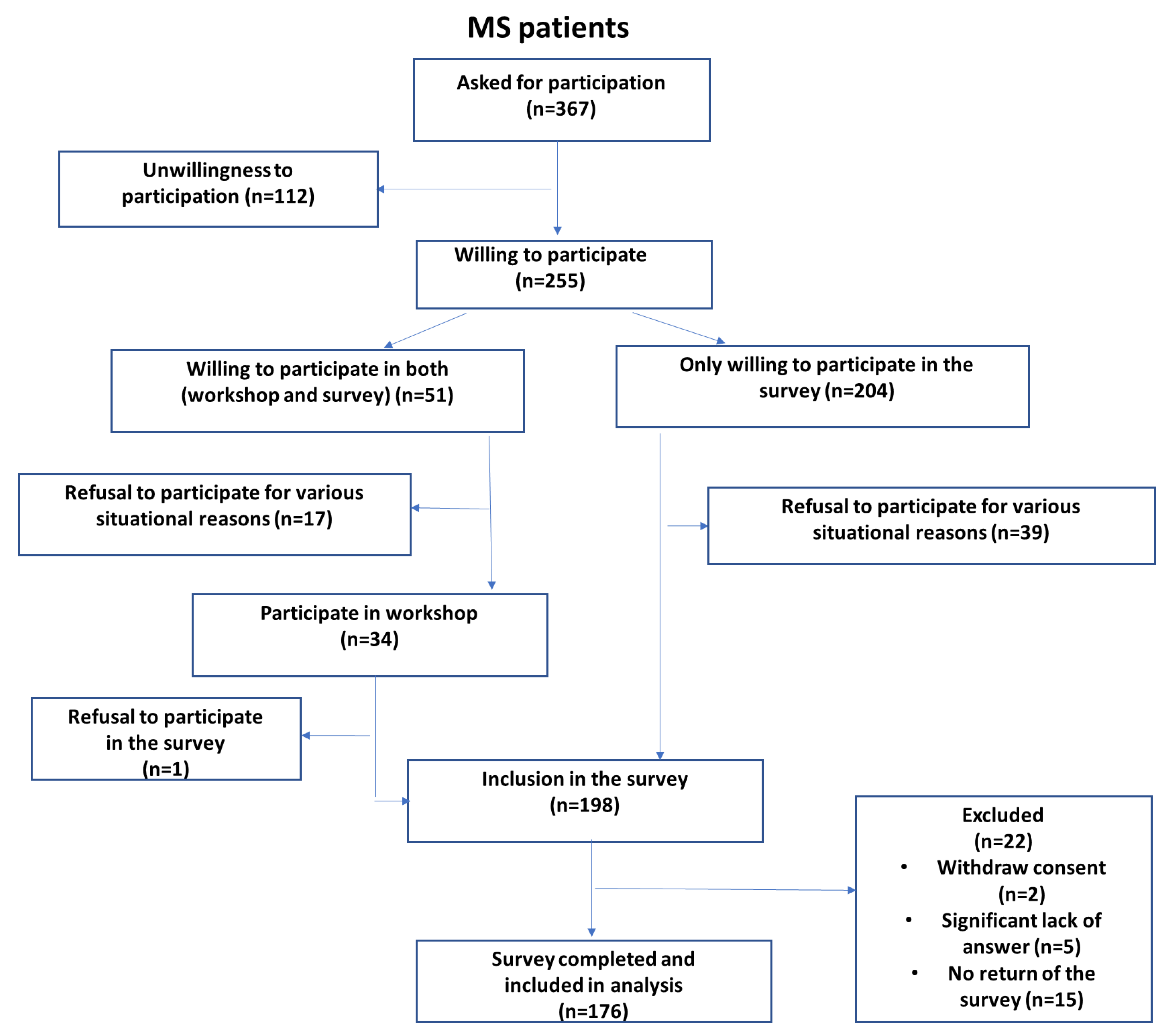
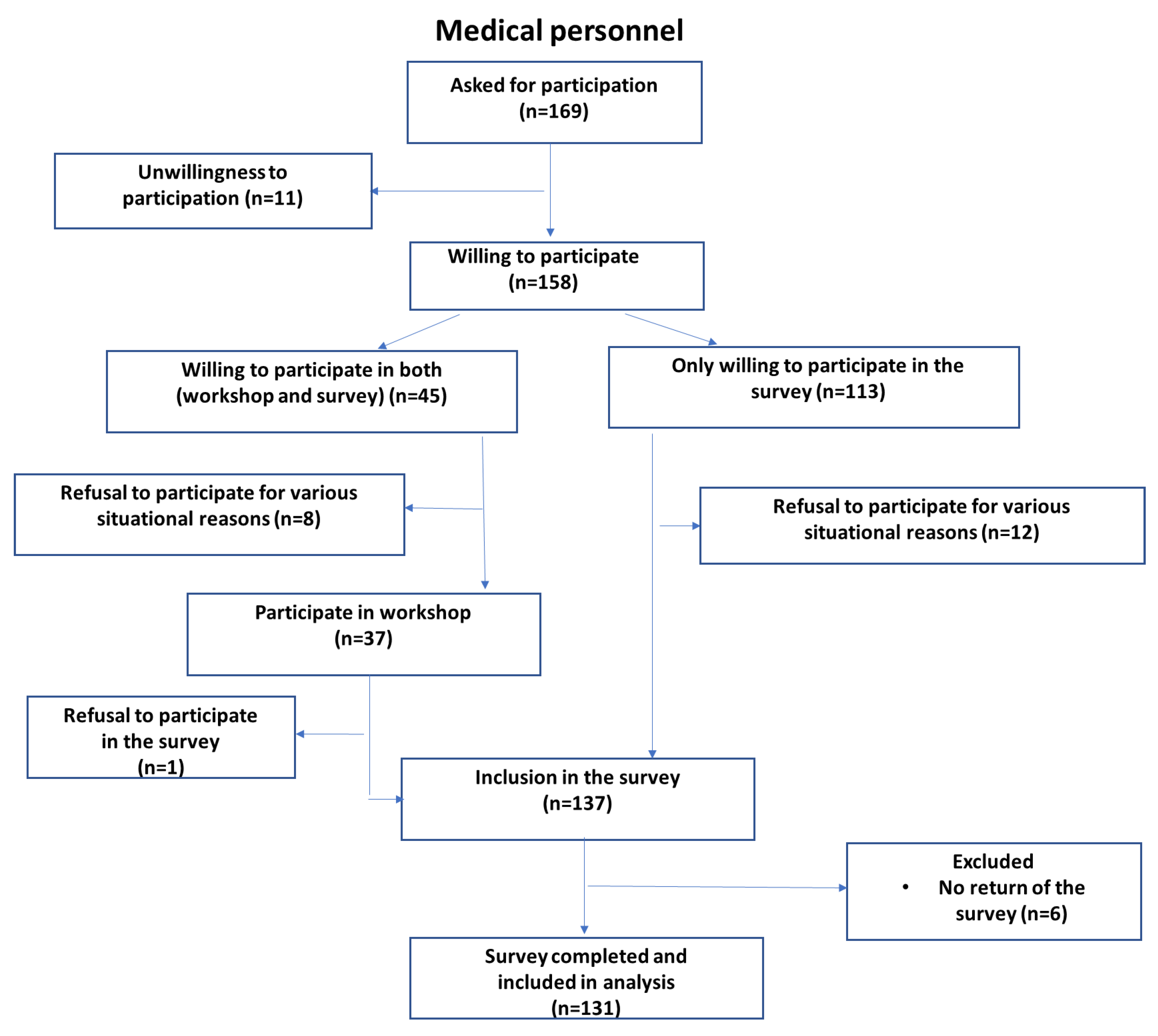
2.1. Participants
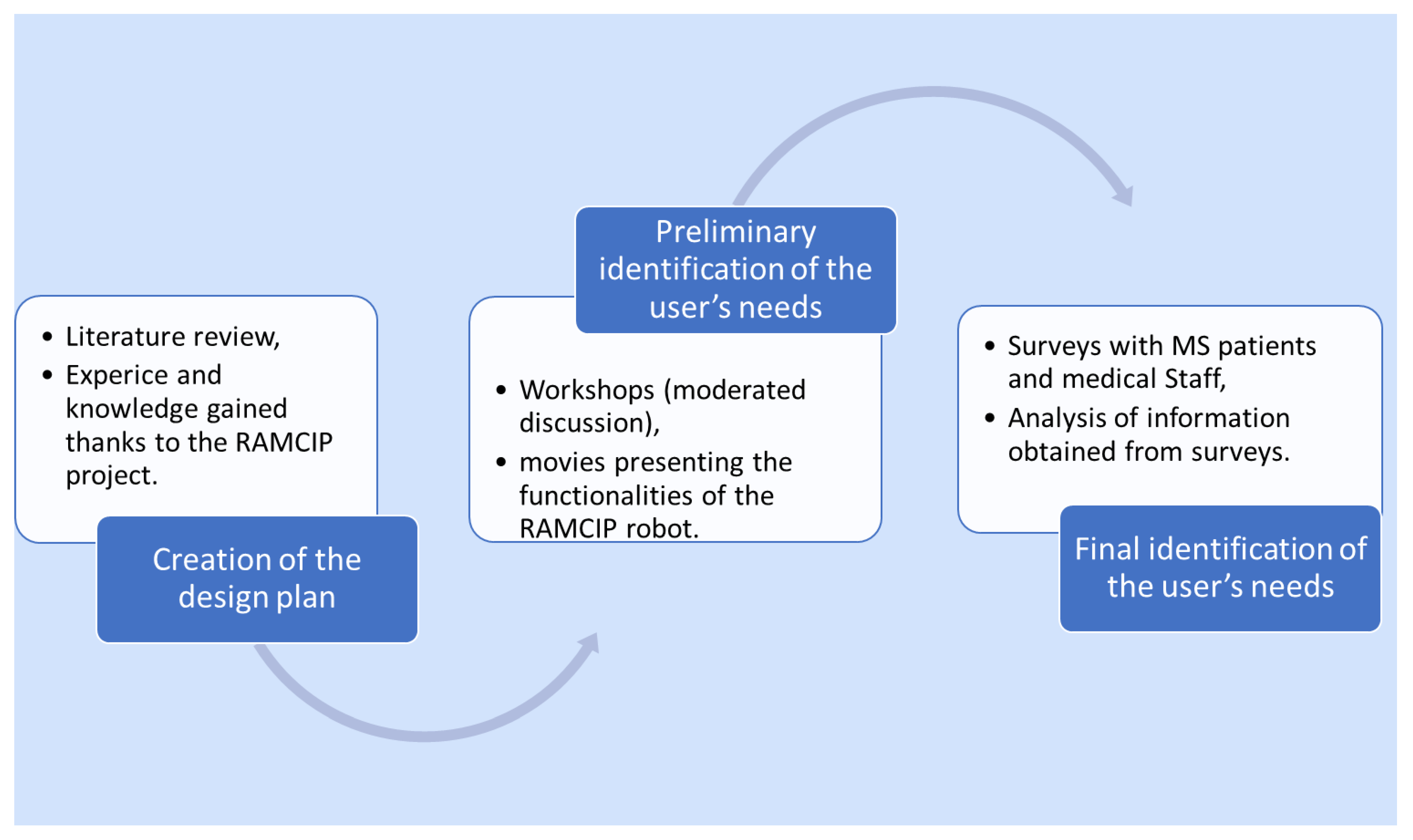
2.2. Study Design
2.3. Statistical Analysis
3. Results
3.1. Profile of Participants
3.2. Prioritizing Target Use Cases for the Robot Assistant
3.3. Prioritizing Human–Robot Interaction
3.4. Evaluation of the RAMCIP Appearance
3.5. Assistive Technology Acceptance and Readiness
3.6. Correlates of Demographics, Disease-Specific Variables, and Priority Level of the Functionalities
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Compston, A.; Coles, A. Multiple sclerosis. Lancet 2008, 372, 1502–1517. [Google Scholar] [CrossRef]
- Blake, D.J.; Bodine, C. An overview of assistive technology for persons with multiple sclerosis. J. Rehabil. Res. Dev. 2002, 39, 299–312. [Google Scholar]
- Jacobs, L.D.; Wende, K.E.; Brownscheidle, C.M.; Apatoff, B.; Coyle, P.K.; Goodman, A.; Gottesman, M.H.; Granger, C.V.; Greenberg, S.J.; Herbert, J.; et al. A profile of multiple sclerosis: The New York State Multiple Sclerosis Consortium. Mult. Scler. 1999, 5, 369–376. [Google Scholar] [CrossRef] [PubMed]
- Deshande, R.; Kremenchutzky, M.; Rice, G.P. The natural history of multiplensclerosis. Adv. Neurol. 2006, 98, 183–272. [Google Scholar]
- Johnson, K.L.; Bamer, A.M.; Yorkston, K.M.; Amtmann, D. Use of cognitive aids and other assistive technology by individuals with multiple sclerosis. Disabil. Rehabil. Assist. Technol. 2009, 4, 1–8. [Google Scholar] [CrossRef] [PubMed]
- De Angelis, M.; Lavorgna, L.; Carotenuto, A.; Petruzzo, M.; Lanzillo, R.; Brescia Morra, V.; Moccia, M.J. Digital Technology in Clinical Trials for Multiple Sclerosis: Systematic Review. Clin. Med. 2021, 10, 2328. [Google Scholar] [CrossRef]
- Lavorgna, L.; Brigo, F.; Moccia, M.; Leocani, L.; Lanzillo, R.; Clerico, M.; Abbadessa, G.; Schmierer, K.; Solaro, C.; Prosperini, L.; et al. e-Health and multiple sclerosis: An update. Mult. Scler. J. 2018, 24, 1657–1664. [Google Scholar] [CrossRef] [Green Version]
- Thompson, A.J.; Banwell, B.L.; Barkhof, F.; Carroll, W.M.; Coetzee, T.; Comi, G.; Correale, J.; Fazekas, F.; Filippi, M.; Freesman, M.S.; et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 2018, 17, 162–173. [Google Scholar] [CrossRef]
- Likert, R. A technique for the measurement of attitudes. Arch. Psychol. 1932, 22, 140–155. [Google Scholar]
- Kim, D.J.; Hazlett-Knudsen, R.; Culver-Godfrey, H.; Rucks, G.; Cunningham, T.; Portee, D.; Bricout, J.; Wang, Z.; Behal, A. How Autonomy Impacts Performance and Satisfaction: Results From a Study with Spinal Cord Injured Subjects Using an Assistive Robot. IEEE Trans. Syst. Man Cybern.-Part A Syst. Hum. 2011, 42, 2–14. [Google Scholar] [CrossRef]
- Korchut, A.; Szklener, S.; Abnelnour, C.; Tantinya, N.; Hermandez-Farigola, J.; Ribes, J.; Skrobas, U.; Grabowska-Aleksandrowicz, K.; Szczęśniak-Stańczyk, D.; Rejdak, K. Challenges for Service Robots-requirements of Elderly Adults with Cognitive Impairments. Front. Neurol. 2017, 8, 228. [Google Scholar] [CrossRef] [Green Version]
- Peterson, E.W.; Cho, C.C.; Finlayson, M.L. Fear of falling and associated activity curtailment among middle aged and older adults with multiple sclerosis. Mult. Scler. 2007, 13, 1168–1175. [Google Scholar] [CrossRef]
- Noseworthy, J.H.; Lucchinetti, C.; Rodriguez, M.; Weinshenker, B.G. Multiple sclerosis. N. Engl. J. Med. 2000, 343, 938–952. [Google Scholar] [CrossRef]
- Finlayson, M.L.; Peterson, E.W.; Cho, C.C. Risk factors for falling among people aged 45 to 90 years with multiple sclerosis. Arch. Phys. Med. Rehabil. 2006, 87, 1274–1279. [Google Scholar] [CrossRef]
- Osterberg, L.; Blaschke, T. Adherence to medication. N. Engl. J. Med. 2005, 353, 487–497. [Google Scholar] [CrossRef] [Green Version]
- Van Biesen, W.; Decruyenaere, J.; Sideri, K.; Cockbain, J.; Sterckx, S. Remote digital monitoring of medication intake: Methodological, medical, ethical and legal reflections. Acta Clin. Belg. 2021, 76, 209–216. [Google Scholar] [CrossRef] [Green Version]
- Johansson, K.; Schalling, E.; Hartelius, L. Self-Reported Changes in Cognition, Communication and Swallowing in Multiple Sclerosis: Data from the Swedish Multiple Sclerosis Registry and from a National Survey. Folia Phoniatr. Logop. 2021, 73, 50–56. [Google Scholar] [CrossRef]
- Gutierrez, G.M.; Chow, J.W.; Tillman, M.D.; McCoy, S.C.; Castellano, V.; White, L.J. Resistance training improves gait kinematics in persons with multiple sclerosis. Arch. Phys. Med. Rehabil. 2005, 86, 1824–1829. [Google Scholar] [CrossRef]
- Forlizzi, J.; DiSalvo, C.; Gemperle, F. Assistive robotics and an ecology of elders living independently in their homes. Hum. Comput. Inter. 2004, 19, 25–59. [Google Scholar]
- Benedict, R.H.B.; Amato, M.P.; DeLuca, J.; Geurts, J.J.G. Cognitive impairment in multiple sclerosis: Clinical management, MRI, and therapeutic avenues. Lancet Neurol. 2020, 19, 860–871. [Google Scholar] [CrossRef]
- Strober, L.; Chiaravalloti, N.; Moore, N.; DeLuca, J. Unemployment in multiple sclerosis (MS): Utility of the MS Functional Composite and cognitive testing. Mult. Scler. 2014, 20, 112–115. [Google Scholar] [CrossRef]
- Frennert, S.; Eftring, H.; Östlund, B. What older people expect of robots: A mixed methods approach. International Conference in Social Robots. Lect. Notes Comput. Sci. 2013, 8239, 19–29. [Google Scholar]
- Halabchi, F.; Alizadeh, Z.; Sahraian, M.A.; Abolhasani, M. Exercise prescription for patients with multiple sclerosis; potential benefits and practical recommendations. BMC Neurol. 2017, 17, 185. [Google Scholar] [CrossRef]
- Sandoval, A.E. Exercise in multiple sclerosis. Phys. Med. Rehabil. Clin. N. Am. 2013, 24, 605–618. [Google Scholar] [CrossRef]
- Pilutti, L.A.; Greenlee, T.A.; Motl, R.W.; Nickrent, M.S.; Petruzzello, S.J. Effects of exercise training on fatigue in multiple sclerosis: A meta-analysis. Psychosom. Med. 2013, 75, 575–580. [Google Scholar] [CrossRef]
- Solaro, C.; Gamberini, G.; Masuccio, F.G. Depression in Multiple Sclerosis: Epidemiology, Aetiology, Diagnosis and Treatment. CNS Drugs 2018, 32, 117–133. [Google Scholar] [CrossRef]
- Begum, M.; Wang, R.; Huq, R.; Mihailidis, A. Performance of daily activities by older adults with dementia: The role of an assistive robot. In Proceedings of the 2013 IEEE 13th International Conference on Rehabilitation Robotics (ICORR), Seattle, WA, USA, 24–26 June 2013. [Google Scholar]
- Gulick, E.E. Emotional distress and activities of daily living functioning in persons with multiple sclerosis. Nurs. Res. 2001, 50, 147–154. [Google Scholar] [CrossRef]
- Chita-Tegmark, M.; Scheutz, M. Assistive Robots for the Social Management of Health: A Framework for Robot Design and Human-Robot Interaction Research. Int. J. Soc. Robot. 2020, 2, 197–217. [Google Scholar] [CrossRef] [Green Version]
- Kodate, N.; Donnelly, S.; Suwa, S.; Tsujimura, M.; Kitinoja, H.; Hallila, J.; Toivonen, M.; Ide, H.; Yu, W. Home-care robots-Attitudes and perceptions among older people, carers and care professionals in Ireland: A questionnaire study. Health Soc. Care Community 2021, 10, 1086–1096. [Google Scholar] [CrossRef]
- Broadbent, E.; Stafford, R.; MacDonald, B. Acceptance of healthcare robots for the older population: Review and future directions. Int. J. Soc. Robot. 2009, 1, 319. [Google Scholar] [CrossRef]
- Rudigkeit, N.; Gebhard, M. AMiCUS 2.0—System Presentation and Demonstration of Adaptability to Personal Needs by the Example of an Individual with Progressed Multiple Sclerosis. Sensors 2020, 20, 1194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hughes, A.; Burridge, J.; Freeman, C.T.; Donnovan-Hall, M.; Chappell, P.H.; Lewin, P.L.; Rogers, E.; Dibb, B. Stroke participants’ perceptions of robotic and electrical stimulation therapy: A new approach Disabil. Rehabil. Assist. Technol. 2011, 6, 130–138. [Google Scholar] [CrossRef] [PubMed]
- Roger, K.; Guse, L.; Mordoch, E.; Osterreicher, A. Social commitment robots and dementia. Can. J. Aging 2012, 31, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Sadasivam, R.S.; Luger, T.M.; Coley, H.L.; Taylor, B.B.; Padir, T.; Ritchie, C.S.; Houston, T.K. Robot-assisted home hazard assessment for fall prevention: A feasibility study. J. Telemed. Telecare 2014, 20, 3–10. [Google Scholar] [CrossRef]
- Pfadenhauer, M.; Dukat, C. Robot caregiver or robot-supported caregiving? Int. J. Soc. Robot. 2015, 7, 393–406. [Google Scholar] [CrossRef]
- Salichs, M.A.; Encinar, I.P.; Salichs, E.; Castro-González, Á.; Malfaz, M. Study of scenarios and technical requirements of a social assistive robot for Alzheimer’s disease patients and their caregivers. Int. J. Soc. Robot. 2015, 8, 85–102. [Google Scholar] [CrossRef]
- Wilson, G.; Pereyda, C.; Raghunath, N.; de la Cruz, G.; Goel, S.; Nesaei, S.; Minor, B.; Schmitter-Edgecombe, M.; Taylor, M.E.; Cook, D.J. Robot-enabled support of daily activities in smart home environments. Cogn. Syst. Res. 2019, 54, 258–272. [Google Scholar] [CrossRef]
- Pino, M.; Boulay, M.; Jouen, F.; Rigaud, A.S. ‘Are we ready for robots that care for us?’ Attitudes and opinions of older adults toward socially assistive robots. Front. Aging Neurosci. 2015, 7, 141. [Google Scholar] [CrossRef] [Green Version]
- Dijkers, M.I.; deBear, P.C.; Erlandson, R.F.; Kristy, K.; Geer, D.M.; Nichols, A. Patient and staff acceptance of robotic technology in occupational therapy: A pilot study. J. Rehabil. Res. Dev. 1991, 28, 33–44. [Google Scholar] [CrossRef]
| Variables | |
|---|---|
| Age [n (%)] | |
| 21–30 | 30 (17.05%) |
| 31–40 | 44 (25.00%) |
| 41–50 | 45 (25.57%) |
| 51–60 | 36 (20.45%) |
| 60+ | 21 (11.93%) |
| Female/Male [n (%)] | 132 (75%)/44 (25%) |
| Education level [n (%)] | |
| Elementary | 10 (5.68%) |
| Vocational | 27 (15.34%) |
| Secondary | 62 (35.23%) |
| Higher | 77 (43.75%) |
| Employment status [n (%)] | |
| Self-employment | 13 (7.39%) |
| Full-time employee | 47 (26.70%) |
| Student | 6 (3.41%) |
| Retired | 95 (53.98%) |
| Unemployed | 13 (8.52%) |
| Course of disease [n (%)] | |
| Relapsing remitting | 114 (64.77%) |
| Secondry progressive | 30 (17.05%) |
| Primary progressive | 25 (14.20%) |
| Progressive relapsing | 7 (3.98%) |
| Duration of the disease [n (%)] | |
| <1 year | 6 (3.41%) |
| 1–2 years | 9 (5.11%) |
| 2–5 years | 25 (14.20%) |
| 5–10 years | 43 (24.43%) |
| >10 years | 93 (52.84%) |
| Level of disability (EDSS) [n (%)] | |
| 0–4.0 | 47.73% |
| 4.5–6.5 | 37.50% |
| 7.0–10.0 | 14.77% |
| Depression [n (%)] | |
| never | 28 (15.91%) |
| hardly ever | 34 (19.32%) |
| sometimes | 73 (41.48%) |
| often | 38 (21.59%) |
| almost always | 3 (1.70%) |
| Intensity level of depression [n (%)] | |
| 1–5 | 104 (59.09%) |
| 6–10 | 72 (40.91%) |
| Cognitive problems [n (%)] | |
| never | 31 (17.61%) |
| hardly ever | 25 (14.20%) |
| sometimes | 67 (38.07%) |
| often | 47 (26.70%) |
| almost always | 6 (3.41%) |
| Intensity level of memory and concentration problems [n (%)] | |
| 1–5 | 110 (62.50%) |
| 6–10 | 66 (37.50%) |
| Fatigue [n (%)] | |
| never | 5 (2.84%) |
| hardly ever | 13 (7.39%) |
| sometimes | 58 (32.95%) |
| often | 70 (39.77%) |
| almost always | 30 (17.05%) |
| Fatigue level [n (%)] | |
| 1–5 | 63 (35.78%) |
| 6–10 | 113 (64.22%) |
| A. Safety | ||||
| Safety | Mean | Users Priority | Mean | Medical Staff Priority |
| Detection of falls | 1,668,966 | H | 1,456,311 | H |
| Asks the patient how they feel after falls | 2,055,172 | M | 1,968,452 | H |
| Informs family members about unwanted incident at home | 1,506,849 | H | 1,494,624 | H |
| Calls for help if something happens to the patient or dangerous situations at home are detected (detects smoke or gas) | 1,621,622 | H | 1,359,223 | H |
| Detection of obstacles on the floor to prevent falls | 1,932,432 | H | 1,902,174 | H |
| Turns the light on when it is too dark and the person starts moving around the house | 1,956,989 | H | 1,902,913 | H |
| Recognizes when it can or cannot open the house door | 2,652,778 | M | 2,516,129 | M |
| Turns working home appliances (electric, water, gas) off while user is busy and asks to do it | 1,768,707 | H | 188,172 | H |
| Monitors correctness of the patient’s medication intake | 1,978,521 | H | 1,556,732 | H |
| Controls proper daily amount of water | 1,841,096 | H | 1,734,750 | H |
| Keeps alert at night | 1,643,466 | H | 1,525,592 | H |
| B. Cognitive Aids | ||||
| Cognitive Aids | Mean | Users Priority | Mean | Medical Staff Priority |
| Provides cognitive exercise to the patient | 2,110345 | M | 1,932,432 | H |
| Reminds the patient that it is time for them to take their medication | 1,958621 | H | 161,165 | H |
| Reminds about regular water drinking and meal time | 1,956989 | H | 1,980,583 | H |
| Reminds about important dates (e.g., medical appointments, events, deadlines) | 2,041096 | M | 227,957 | M |
| C. Physical Aids | ||||
| Physical Aids | Mean | Users Priority | Mean | Medical Staff Priority |
| Stimulates/provides instructions to the patient to perform physical exercises | 2,204,082 | M | 1,979,452 | H |
| Can reach medication which is difficult to reach for the patient | 2,158,621 | M | 2,086,022 | M |
| Reaches for fallen utensils and hands them over to the patient to prevent the patient from bending over. Grasps things from the floor/shelves | 2,296,552 | M | 2,106,796 | M |
| Brings food | 2,555,556 | M | 2,451,613 | M |
| Helps the patient take on/off her/his shoes | 2,643,357 | M | 2,361,702 | M |
| Finds the things the patient is looking for | 2,482,759 | M | 2,445,652 | M |
| Brings the things the patient asks for | 2,423,611 | M | 2,326,087 | M |
| Helps the patient properly button her/his clothes | 2,671,329 | M | 2,322,581 | M |
| D. Household Management and Socio-Emotional Wellness | ||||
| Household Management | Mean | Users Priority | Mean | Medical Staff Priority |
| Helps the patient clean the house | 2,421,769 | M | 2,698,925 | M |
| Helps the patient with a shopping list | 3,048,611 | L | 2,923,913 | M |
| Helps the patient prepare food | 2,643,836 | M | 2,673,913 | M |
| Detects an open fridge door and closes it | 2,503,448 | M | 2,300,971 | M |
| Stimulates the patient to keep in touch with family and friends | 2,393,103 | M | 2,408,602 | M |
| Communication and Interaction | Mean | Users Priority | Mean | Medical Staff Priority |
|---|---|---|---|---|
| The robotic assistant can reply to simple questions (e.g., what time is it?) | 2,372,414 | M | 2,225,806 | M |
| The robotic assistant can listen and respond to simple commands you give | 1,979,452 | H | 1,882,796 | H |
| The robotic assistant can comprehend and respond to simple gestures you make | 2,263,889 | M | 2,107,527 | M |
| The robotic assistant can take part in dialogue interactions with the user to complete required tasks | 2,472,603 | M | 2,397,849 | M |
| The robotic assistant can talk to you regarding its current task/state | 2,331,034 | M | 2,301,075 | M |
| The robotic assistant can be easily controlled by the touch screen which is mounted on it | 1,896,552 | H | 1,956,989 | H |
| The controls shown on the touch screen of the robotic assistant change to reflect the needs of the user and the current task | 2,082,192 | M | 2,043,011 | M |
| The robotic assistant can display information on a touch screen that is mounted on it | 1,968,966 | H | 1,902,174 | H |
| The robotic assistant can be controlled directly through the touch screen it carries without the need to engage in a dialogue with the user | 2,294,521 | M | 2,150,538 | M |
| The robotic assistant has a face that can express its feelings throughout interactions with the user | 3,027,397 | L | 2,602,151 | M |
| The robotic assistant should continuously listen to the user for commands | 2,184,932 | M | 2,139,785 | M |
| The robotic assistant can understand the psychological state of the user and provide positive affective impact (actions) | 2,458,333 | M | 2,391,304 | M |
| Provision Cognitive Excersises | ||||
| Mean | SD | 95% CI | p-Value | |
| Age | 45 | 15 | ±2.07 | <0.001 |
| EDSS: | ||||
| 0–4.0 | 2.56 | 1.02 | ±0.214 | NS |
| 4.5–6.5 | 5.61 | 0.83 | ±0.00 | <0.001 |
| 7–10 | 8.46 | 0.97 | - | NS |
| Cognitive problems | 4.35 | 2.52 | ±0.295 | <0.001 |
| Performance of Physical Excersises | ||||
| Mean | SD | 95% CI | p-Value | |
| Fatigue | 6.14 | 2.48 | ±0.293 | <0.001 |
| Depression | 4.60 | 2.70 | ±0.295 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Korchut, A.; Petit, V.; Szwedo-Brzozowska, E.; Rejdak, K. Assistive Technology in Multiple Sclerosis Patients—Two Points of View. J. Clin. Med. 2022, 11, 4068. https://doi.org/10.3390/jcm11144068
Korchut A, Petit V, Szwedo-Brzozowska E, Rejdak K. Assistive Technology in Multiple Sclerosis Patients—Two Points of View. Journal of Clinical Medicine. 2022; 11(14):4068. https://doi.org/10.3390/jcm11144068
Chicago/Turabian StyleKorchut, Agnieszka, Veronique Petit, Ewelina Szwedo-Brzozowska, and Konrad Rejdak. 2022. "Assistive Technology in Multiple Sclerosis Patients—Two Points of View" Journal of Clinical Medicine 11, no. 14: 4068. https://doi.org/10.3390/jcm11144068
APA StyleKorchut, A., Petit, V., Szwedo-Brzozowska, E., & Rejdak, K. (2022). Assistive Technology in Multiple Sclerosis Patients—Two Points of View. Journal of Clinical Medicine, 11(14), 4068. https://doi.org/10.3390/jcm11144068







