Sleep Quality and Insomnia Severity among Italian University Students: A Latent Profile Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measures
2.2.1. Insomnia Severity Index
2.2.2. Pittsburgh Sleep Quality Index
2.2.3. Depression Anxiety Stress Scale-21
2.2.4. Short Form-12
2.3. Statistical Analyses
3. Results
3.1. Sample Characteristics
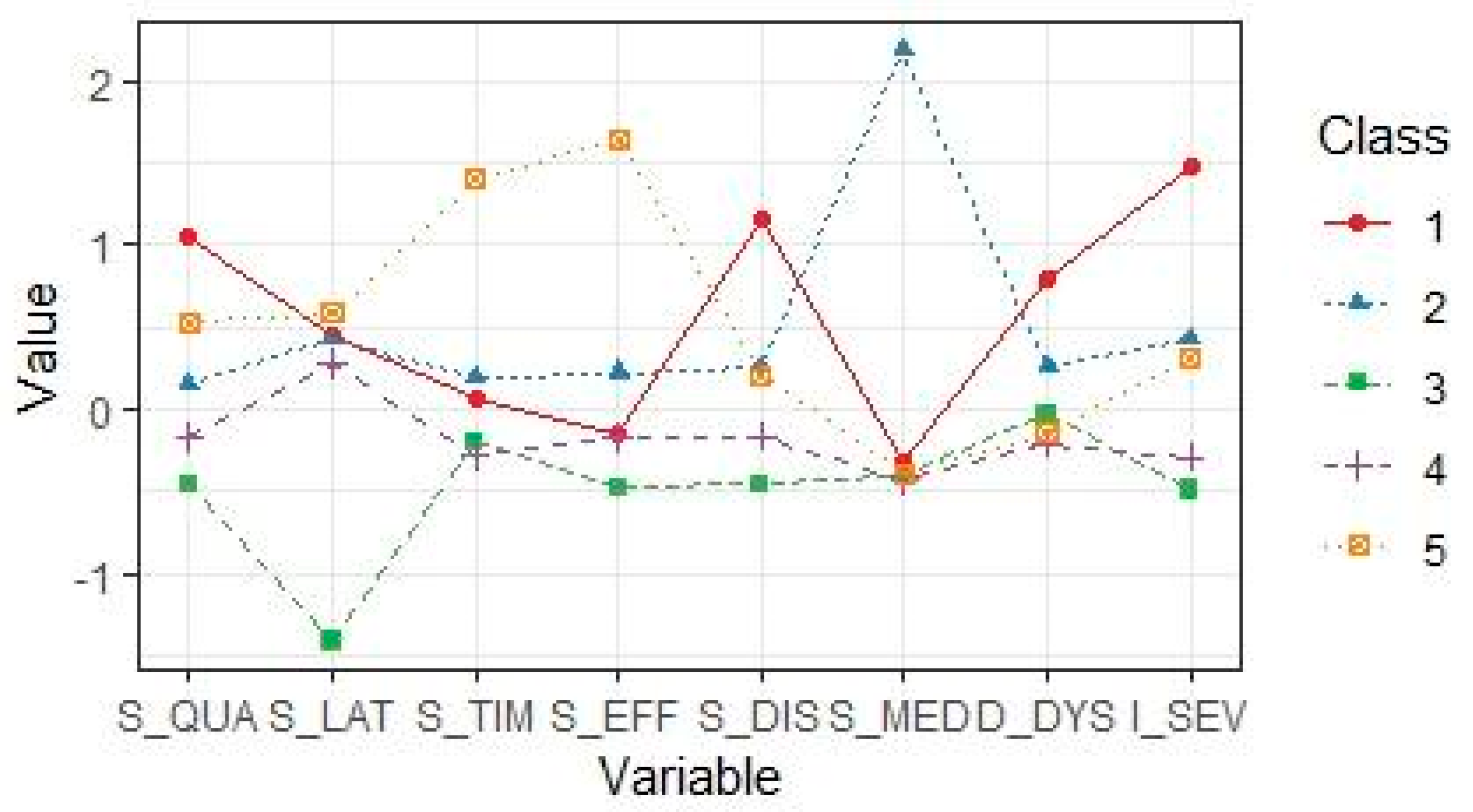
3.2. Insomnia Profiles Characterization
3.3. Differences between Insomnia Profiles in Health Habits, Psychological Complaints, and Health-Related Quality of Life
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| SI (n = 43) (1) | MI-MU (n = 78) (2) | SubI (n = 100) (3) | SubI-SL (n = 228) (4) | MI-SD (n = 41) (5) | |
|---|---|---|---|---|---|
| Variable | |||||
| Sex (N (%)) | |||||
| Female | 38 (88.4) | 75 (96.2) | 87 (87.0) | 192 (84.2) | 40 (88.2) |
| Male | 5 (11.6) | 3 (3.8) | 13 (13.0) | 36 (15.8) | 58 (11.8) |
| Age (M (SD)) | 23.3 (2.0) | 23.6 (2.3) | 23.5 (2.8) | 23.2 (2.3) | 23.8 (2.8) |
| Tobacco use (N (%)) | |||||
| Yes | 27 (62.8) | 47 (60.3) | 49 (49.0) | 105 (46.1) | 24 (58.5) |
| No | 16 (37.2) | 31 (39.7) | 51 (51.0) | 123 (53.9) | 17 (41.5) |
| Excessive alcohol consumption (N (%)) | |||||
| ≥2 per week | 8 (18.6) | 16 (20.5) | 10 (10.0) | 24 (10.5) | 6 (14.6) |
| <2 per week | 35 (81.4) | 62 (79.5) | 90 (90.0) | 204 (89.5) | 35 (85.4) |
| Physical exercise (N (%)) | |||||
| ≥2 per week | 14 (32.6) | 30 (38.5) | 31 (31.0) | 88 (38.6) | 17 (41.5) |
| <2 per week | 29 (67.4) | 48 (61.5) | 69 (69.0) | 140 (61.4) | 24 (58.5) |
| BMI (kg/m2) (M (SD)) | 23.1 (4.3) | 22.6 (5.1) | 22.6 (3.7) | 22.4 (3.8) | 22.2 (3.8) |
References
- Ohayon, M.M. Epidemiological Overview of Sleep Disorders in the General Population. Sleep Med. Res. 2011, 2, 1–9. [Google Scholar] [CrossRef]
- Morin, C.M.; Drake, C.L.; Harvey, A.G.; Krystal, A.D.; Manber, R.; Riemann, D.; Spiegelhalder, K. Insomnia Disorder. Nat. Rev. Dis. Primer. 2015, 1, 15026. [Google Scholar] [CrossRef] [PubMed]
- Chung, K.-F.; Yeung, W.-F.; Ho, F.Y.-Y.; Yung, K.-P.; Yu, Y.-M.; Kwok, C.-W. Cross-Cultural and Comparative Epidemiology of Insomnia: The Diagnostic and Statistical Manual (DSM), International Classification of Diseases (ICD) and International Classification of Sleep Disorders (ICSD). Sleep Med. 2015, 16, 477–482. [Google Scholar] [CrossRef]
- Morin, C.M.; Bjorvatn, B.; Chung, F.; Holzinger, B.; Partinen, M.; Penzel, T.; Ivers, H.; Wing, Y.K.; Chan, N.Y.; Merikanto, I.; et al. Insomnia, Anxiety, and Depression during the COVID-19 Pandemic: An International Collaborative Study. Sleep Med. 2021, 87, 38–45. [Google Scholar] [CrossRef]
- Alvaro, P.K.; Roberts, R.M.; Harris, J.K. A Systematic Review Assessing Bidirectionality between Sleep Disturbances, Anxiety, and Depression. Sleep 2013, 36, 1059–1068. [Google Scholar] [CrossRef] [PubMed]
- Hertenstein, E.; Feige, B.; Gmeiner, T.; Kienzler, C.; Spiegelhalder, K.; Johann, A.; Jansson-Fröjmark, M.; Palagini, L.; Rücker, G.; Riemann, D.; et al. Insomnia as a Predictor of Mental Disorders: A Systematic Review and Meta-Analysis. Sleep Med. Rev. 2019, 43, 96–105. [Google Scholar] [CrossRef]
- Vgontzas, A.N.; Fernandez-Mendoza, J.; Liao, D.; Bixler, E.O. Insomnia with Objective Short Sleep Duration: The Most Biologically Severe Phenotype of the Disorder. Sleep Med. Rev. 2013, 17, 241–254. [Google Scholar] [CrossRef] [Green Version]
- Sivertsen, B.; Hysing, M.; Harvey, A.G.; Petrie, K.J. The Epidemiology of Insomnia and Sleep Duration across Mental and Physical Health: The SHoT Study. Front. Psychol. 2021, 12, 662572. [Google Scholar] [CrossRef]
- Taylor, D.J.; Lichstein, K.L.; Durrence, H.H.; Reidel, B.W.; Bush, A.J. Epidemiology of Insomnia, Depression, and Anxiety. Sleep 2005, 28, 1457–1464. [Google Scholar] [CrossRef]
- Taylor, D.J.; Mallory, L.J.; Lichstein, K.L.; Durrence, H.H.; Riedel, B.W.; Bush, A.J. Comorbidity of Chronic Insomnia With Medical Problems. Sleep 2007, 30, 213–218. [Google Scholar] [CrossRef]
- Morin, C.M.; Jarrin, D.C. Epidemiology of Insomnia. Sleep Med. Clin. 2013, 8, 281–297. [Google Scholar] [CrossRef] [Green Version]
- McArdle, N.; Ward, S.V.; Bucks, R.S.; Maddison, K.; Smith, A.; Huang, R.-C.; Pennell, C.E.; Hillman, D.R.; Eastwood, P.R. The Prevalence of Common Sleep Disorders in Young Adults: A Descriptive Population-Based Study. Sleep 2020, 43, zsaa072. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.l.; Zheng, X.Y.; Yang, J.; Ye, C.P.; Chen, Y.Y.; Zhang, Z.G.; Xiao, Z.J. A Systematic Review of Studies on the Prevalence of Insomnia in University Students. Public Health 2015, 129, 1579–1584. [Google Scholar] [CrossRef]
- Marelli, S.; Castelnuovo, A.; Somma, A.; Castronovo, V.; Mombelli, S.; Bottoni, D.; Leitner, C.; Fossati, A.; Ferini-Strambi, L. Impact of COVID-19 Lockdown on Sleep Quality in University Students and Administration Staff. J. Neurol. 2021, 268, 8–15. [Google Scholar] [CrossRef]
- Fila-Witecka, K.; Malecka, M.; Senczyszyn, A.; Wieczorek, T.; Wieckiewicz, M.; Szczesniak, D.; Piotrowski, P.; Rymaszewska, J. Sleepless in Solitude—Insomnia Symptoms Severity and Psychopathological Symptoms among University Students during the COVID-19 Pandemic in Poland. Int. J. Environ. Res. Public Health 2022, 19, 2551. [Google Scholar] [CrossRef]
- American Academy of Sleep Medicine. International Classification of Sleep Disorders, 3rd ed.; American Academy of Sleep Medicine: Darien, IL, USA, 2014. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Pillai, V.; Roth, T.; Drake, C.L. The Nature of Stable Insomnia Phenotypes. Sleep 2015, 38, 127–138. [Google Scholar] [CrossRef]
- Fernandez-Mendoza, J. The Insomnia with Short Sleep Duration Phenotype: An Update on It’s Importance for Health and Prevention. Curr. Opin. Psychiatry 2017, 30, 56–63. [Google Scholar] [CrossRef]
- Benjamins, J.S.; Migliorati, F.; Dekker, K.; Wassing, R.; Moens, S.; Blanken, T.F.; te Lindert, B.H.W.; Sjauw Mook, J.; Van Someren, E.J.W. Insomnia Heterogeneity: Characteristics to Consider for Data-Driven Multivariate Subtyping. Sleep Med. Rev. 2017, 36, 71–81. [Google Scholar] [CrossRef]
- Ruivo Marques, D.; Clemente, V.; Allen Gomes, A.; de Azevedo, M.H.P. Profiling Insomnia Using Subjective Measures: Where Are We and Where Are We Going. Sleep Med. 2018, 42, 103–104. [Google Scholar] [CrossRef] [Green Version]
- Marques, D.R.; Gomes, A.A.; Clemente, V.; dos Santos, J.M.; Serra, J.; de Azevedo, M.H.P. Trends in Insomnia Research for the next Decade: A Narrative Review. Sleep Biol. Rhythms 2020, 18, 199–207. [Google Scholar] [CrossRef]
- Shahid, A.; Wilkinson, K.; Marcu, S.; Shapiro, C.M. STOP, THAT and One Hundred Other Sleep Scales; Springer: New York, NY, USA, 2012. [Google Scholar]
- Van Loo, H.M.; de Jonge, P.; Romeijn, J.-W.; Kessler, R.C.; Schoevers, R.A. Data-Driven Subtypes of Major Depressive Disorder: A Systematic Review. BMC Med. 2012, 10, 156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bathelt, J.; Holmes, J.; Astle, D.E.; Holmes, J.; Gathercole, S.; Astle, D.; Manly, T.; Kievit, R. Data-Driven Subtyping of Executive Function–Related Behavioral Problems in Children. J. Am. Acad. Child Adolesc. Psychiatry 2018, 57, 252–262.e4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miller, C.B.; Bartlett, D.J.; Mullins, A.E.; Dodds, K.L.; Gordon, C.J.; Kyle, S.D.; Kim, J.W.; D’Rozario, A.L.; Lee, R.S.C.; Comas, M.; et al. Clusters of Insomnia Disorder: An Exploratory Cluster Analysis of Objective Sleep Parameters Reveals Differences in Neurocognitive Functioning, Quantitative EEG, and Heart Rate Variability. Sleep 2016, 39, 1993–2004. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crawford, M.R.; Chirinos, D.A.; Iurcotta, T.; Edinger, J.D.; Wyatt, J.K.; Manber, R.; Ong, J.C. Characterization of Patients Who Present With Insomnia: Is There Room for a Symptom Cluster-Based Approach? J. Clin. Sleep Med. 2017, 13, 911–921. [Google Scholar] [CrossRef] [Green Version]
- Foley, K.A.; Sarsour, K.; Kalsekar, A.; Walsh, J.K. Subtypes of Sleep Disturbance: Associations among Symptoms, Comorbidities, Treatment, and Medical Costs. Behav. Sleep. Med. 2010, 8, 90–104. [Google Scholar] [CrossRef]
- Marques, D.R.; Gomes, A.A.; Clemente, V.; Drake, C.L.; Roth, T.; Morin, C.M.; de Azevedo, M.H.P. Typologies of Individuals Vulnerable to Insomnia: A Two-Step Cluster Analysis. Sleep Biol. Rhythms 2021, 19, 33–44. [Google Scholar] [CrossRef]
- Blanken, T.F.; Benjamins, J.S.; Borsboom, D.; Vermunt, J.K.; Paquola, C.; Ramautar, J.; Dekker, K.; Stoffers, D.; Wassing, R.; Wei, Y.; et al. Insomnia Disorder Subtypes Derived from Life History and Traits of Affect and Personality. Lancet Psychiatry 2019, 6, 151–163. [Google Scholar] [CrossRef] [Green Version]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A New Instrument for Psychiatric Practice and Research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Krystal, A.D.; Edinger, J.D. Measuring Sleep Quality. Sleep Med. 2008, 9, S10–S17. [Google Scholar] [CrossRef]
- Ohayon, M.; Wickwire, E.M.; Hirshkowitz, M.; Albert, S.M.; Avidan, A.; Daly, F.J.; Dauvilliers, Y.; Ferri, R.; Fung, C.; Gozal, D.; et al. National Sleep Foundation’s Sleep Quality Recommendations: First Report. Sleep Health 2017, 3, 6–19. [Google Scholar] [CrossRef] [Green Version]
- Chen, H.-C.; Hsu, N.-W.; Chou, P. Subgrouping Poor Sleep Quality in Community-Dwelling Older Adults with Latent Class Analysis—The Yilan Study, Taiwan. Sci. Rep. 2020, 10, 5432. [Google Scholar] [CrossRef] [PubMed]
- Seow, L.S.E.; Abdin, E.; Chang, S.; Chong, S.A.; Subramaniam, M. Identifying the Best Sleep Measure to Screen Clinical Insomnia in a Psychiatric Population. Sleep Med. 2018, 41, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Bastien, C. Validation of the Insomnia Severity Index as an Outcome Measure for Insomnia Research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef]
- Morin, C.M.; Belleville, G.; Bélanger, L.; Ivers, H. The Insomnia Severity Index: Psychometric Indicators to Detect Insomnia Cases and Evaluate Treatment Response. Sleep 2011, 34, 601–608. [Google Scholar] [CrossRef] [Green Version]
- Carpi, M.; Cianfarani, C.; Vestri, A. Sleep Quality and Its Associations with Physical and Mental Health-Related Quality of Life among University Students: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 2874. [Google Scholar] [CrossRef]
- Gosling, S.D.; Mason, W. Internet Research in Psychology. Annu. Rev. Psychol. 2015, 66, 877–902. [Google Scholar] [CrossRef] [Green Version]
- Lovibond, P.F.; Lovibond, S.H. The Structure of Negative Emotional States: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Ware, J.E.; Kosinski, M.; Keller, S.D. A 12-Item Short-Form Health Survey: Construction of Scales and Preliminary Tests of Reliability and Validity. Med. Care 1996, 34, 220–233. [Google Scholar] [CrossRef] [Green Version]
- Nunnally, J.C.; Bernstein, I.H. Psychometric Theory, 3rd ed.; McGraw-Hill: New York, NY, USA, 1994. [Google Scholar]
- Cronbach, L.J. Coefficient Alpha and the Internal Structure of Tests. Psychometrika 1951, 16, 297–334. [Google Scholar] [CrossRef] [Green Version]
- McDonald, R.P. Test Theory: A Unified Treatment; Erlbaum: Hillsdale, NJ, USA, 1999. [Google Scholar]
- Curcio, G.; Tempesta, D.; Scarlata, S.; Marzano, C.; Moroni, F.; Rossini, P.M.; Ferrara, M.; De Gennaro, L. Validity of the Italian Version of the Pittsburgh Sleep Quality Index (PSQI). Neurol. Sci. 2013, 34, 511–519. [Google Scholar] [CrossRef]
- Bottesi, G.; Ghisi, M.; Altoè, G.; Conforti, E.; Melli, G.; Sica, C. The Italian Version of the Depression Anxiety Stress Scales-21: Factor Structure and Psychometric Properties on Community and Clinical Samples. Compr. Psychiatry 2015, 60, 170–181. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.E.; Kosinski, M.; Keller, S.D. SF-12: How to Score the SF-12 Physical and Mental Health Summary Scales; The Health Institute, New England Medical Center: Boston, MA, USA, 1995. [Google Scholar]
- Apolone, G.; Mosconi, P.; Quattrociocchi, L.; Gianicolo, E.A.L.; Groth, N.; Ware, J.E. Questionario Sullo Stato Di Salute SF-12. Versione Italiana; Guerini e Associati: Milan, Italy, 2005. [Google Scholar]
- Spurk, D.; Hirschi, A.; Wang, M.; Valero, D.; Kauffeld, S. Latent Profile Analysis: A Review and “How to” Guide of Its Application within Vocational Behavior Research. J. Vocat. Behav. 2020, 120, 103445. [Google Scholar] [CrossRef]
- Slavish, D.C.; Contractor, A.A.; Dietch, J.R.; Messman, B.; Lucke, H.R.; Briggs, M.; Thornton, J.; Ruggero, C.; Kelly, K.; Kohut, M.; et al. Characterizing Patterns of Nurses’ Daily Sleep Health: A Latent Profile Analysis. Int. J. Behav. Med. 2022. online ahead of print. [Google Scholar] [CrossRef]
- Wallace, D.M.; Wohlgemuth, W.K. Predictors of Insomnia Severity Index Profiles in United States Veterans with Obstructive Sleep Apnea. J. Clin. Sleep Med. 2019, 15, 1827–1837. [Google Scholar] [CrossRef] [PubMed]
- Celeux, G.; Soromenho, G. An Entropy Criterion for Assessing the Number of Clusters in a Mixture Model. J. Classif. 1996, 13, 195–212. [Google Scholar] [CrossRef] [Green Version]
- Nylund, K.L.; Asparouhov, T.; Muthén, B.O. Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling: A Monte Carlo Simulation Study. Struct. Equ. Model. Multidiscip. J. 2007, 14, 535–569. [Google Scholar] [CrossRef]
- Mooi, E.; Sarstedt, M. A Concise Guide to Market Research; Springer: Berlin/Heidelberg, Germany, 2011. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021. [Google Scholar]
- Rosenberg, J.; Beymer, P.; Anderson, D.; Van Lissa, C.; Schmidt, J. TidyLPA: An R Package to Easily Carry Out Latent Profile Analysis (LPA) Using Open-Source or Commercial Software. J. Open Source Softw. 2018, 3, 978. [Google Scholar] [CrossRef] [Green Version]
- Miley Akerstedt, A.; Hetta, J.; Akerstedt, T. Criteria for Self-Reported Quantitative Sleep Characteristics of Individuals Who Sought Medical Help for Disturbed Sleep—A Survey of a Representative Sample of the Swedish Population. Nat. Sci. Sleep 2018, 10, 295–301. [Google Scholar] [CrossRef] [Green Version]
- Steptoe, A. Sleep Duration and Health in Young Adults. Arch. Intern. Med. 2006, 166, 1689. [Google Scholar] [CrossRef] [Green Version]
- Buscemi, N.; Vandermeer, B.; Friesen, C.; Bialy, L.; Tubman, M.; Ospina, M.; Klassen, T.P.; Witmans, M. The Efficacy and Safety of Drug Treatments for Chronic Insomnia in Adults: A Meta-Analysis of RCTs. J. Gen. Intern. Med. 2007, 22, 1335–1350. [Google Scholar] [CrossRef] [Green Version]
- Winkler, A.; Auer, C.; Doering, B.K.; Rief, W. Drug Treatment of Primary Insomnia: A Meta-Analysis of Polysomnographic Randomized Controlled Trials. CNS Drugs 2014, 28, 799–816. [Google Scholar] [CrossRef] [PubMed]
- Sasai, T.; Inoue, Y.; Komada, Y.; Nomura, T.; Matsuura, M.; Matsushima, E. Effects of Insomnia and Sleep Medication on Health-Related Quality of Life. Sleep Med. 2010, 11, 452–457. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Wing, Y.-K. Sex Differences in Insomnia: A Meta-Analysis. Sleep 2006, 29, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Van Straten, A.; van der Zweerde, T.; Kleiboer, A.; Cuijpers, P.; Morin, C.M.; Lancee, J. Cognitive and Behavioral Therapies in the Treatment of Insomnia: A Meta-Analysis. Sleep Med. Rev. 2018, 38, 3–16. [Google Scholar] [CrossRef]
- Van der Zweerde, T.; Bisdounis, L.; Kyle, S.D.; Lancee, J.; van Straten, A. Cognitive Behavioral Therapy for Insomnia: A Meta-Analysis of Long-Term Effects in Controlled Studies. Sleep Med. Rev. 2019, 48, 101208. [Google Scholar] [CrossRef]
- Muench, A.; Vargas, I.; Grandner, M.A.; Ellis, J.G.; Posner, D.; Bastien, C.H.; Drummond, S.P.; Perlis, M.L. We Know CBT-I Works, Now What? Fac. Rev. 2022, 11, 4. [Google Scholar] [CrossRef]
- Edinger, J.D.; Arnedt, J.T.; Bertisch, S.M.; Carney, C.E.; Harrington, J.J.; Lichstein, K.L.; Sateia, M.J.; Troxel, W.M.; Zhou, E.S.; Kazmi, U.; et al. Behavioral and Psychological Treatments for Chronic Insomnia Disorder in Adults: An American Academy of Sleep Medicine Clinical Practice Guideline. J. Clin. Sleep Med. 2021, 17, 255–262. [Google Scholar] [CrossRef]
- Morin, C.M. Cognitive-Behavioral Therapy of Insomnia. Sleep Med. Clin. 2006, 1, 375–386. [Google Scholar] [CrossRef]
- Rybarczyk, B.; Mack, L. Behavioral Treatment of Insomnia: A Proposal for a Stepped-Care Approach to Promote Public Health. Nat. Sci. Sleep 2011, 3, 87–99. [Google Scholar] [CrossRef] [Green Version]
- Kloss, J.D.; Nash, C.O.; Walsh, C.M.; Culnan, E.; Horsey, S.; Sexton-Radek, K. A “Sleep 101” Program for College Students Improves Sleep Hygiene Knowledge and Reduces Maladaptive Beliefs about Sleep. Behav. Med. 2016, 42, 48–56. [Google Scholar] [CrossRef]
- Morin, C.M.; Bastien, C.; Guay, B.; Radouco-Thomas, M.; Leblanc, J.; Vallières, A. Randomized Clinical Trial of Supervised Tapering and Cognitive Behavior Therapy to Facilitate Benzodiazepine Discontinuation in Older Adults With Chronic Insomnia. Am. J. Psychiatry 2004, 161, 332–342. [Google Scholar] [CrossRef]
- Collins, L.M.; Lanza, S.T. Latent Class and Latent Transition Analysis: With Applications in the Social, Behavioral, and Health Sciences; John Wiley: New York, NY, USA, 2009. [Google Scholar]
- Dietch, J.R.; Taylor, D.J. Evaluation of the Consensus Sleep Diary in a Community Sample: Comparison with Single-Channel Electroencephalography, Actigraphy, and Retrospective Questionnaire. J. Clin. Sleep Med. 2021, 17, 1389–1399. [Google Scholar] [CrossRef]
- Aili, K.; Åström-Paulsson, S.; Stoetzer, U.; Svartengren, M.; Hillert, L. Reliability of Actigraphy and Subjective Sleep Measurements in Adults: The Design of Sleep Assessments. J. Clin. Sleep Med. 2017, 13, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Carrión-Pantoja, S.; Prados, G.; Chouchou, F.; Holguín, M.; Mendoza-Vinces, Á.; Expósito-Ruiz, M.; Fernández-Puerta, L. Insomnia Symptoms, Sleep Hygiene, Mental Health, and Academic Performance in Spanish University Students: A Cross-Sectional Study. J. Clin. Med. 2022, 11, 1989. [Google Scholar] [CrossRef]
- Park, J.H.; An, H.; sook Jang, E.; Chung, S. The Influence of Personality and Dysfunctional Sleep-Related Cognitions on the Severity of Insomnia. Psychiatry Res. 2012, 197, 275–279. [Google Scholar] [CrossRef] [PubMed]
- Baglioni, C.; Spiegelhalder, K.; Lombardo, C.; Riemann, D. Sleep and Emotions: A Focus on Insomnia. Sleep Med. Rev. 2010, 14, 227–238. [Google Scholar] [CrossRef] [PubMed]
| Variable | N (%) | Mean (SD) |
|---|---|---|
| Sex | ||
| Women | 432 (88.2) | |
| Men | 58 (11.8) | |
| Age | 23.4 (2.4) | |
| Study course | ||
| Undergraduate | 411 (83.9) | |
| Postgraduate | 79 (16.1) | |
| Occupational situation | ||
| Full-time student | 363 (74.1) | |
| Part-time job | 92 (18.8) | |
| Full-time job | 35 (7.1) | |
| Living situation | ||
| With parents | 354 (72.2) | |
| With roommates/partner | 117 (23.9) | |
| Alone | 19 (3.9) | |
| Tobacco use | ||
| Yes | 252 (51.4) | |
| No | 238 (48.6) | |
| Excessive alcohol consumption | ||
| ≥2 per week | 64 (13.1) | |
| <2 per week | 426 (86.9) | |
| Physical exercise | ||
| ≥2 per week | 180 (36.7) | |
| <2 per week | 310 (63.3) | |
| BMI (kg/m2) | 22.5 (4.0) | |
| <18.5 (underweight) | 60 (12.2) | |
| 18.5 to 24.99 (normal weight) | 335 (68.4) | |
| ≥25 (overweight) | 95 (19.4) | |
| Total sleep time (hours) | 6.5 (1.1) | |
| Sleep-onset latency (minutes) | 48.5 (37.5) | |
| Sleep efficiency index (%) | 80.5 (11.9) | |
| Total Sample (n = 490) | SI (n = 43) (1) | MI-MU (n = 78) (2) | SubI (n = 100) (3) | SubI-SL (n = 228) (4) | MI-SD (n = 41) (5) | ||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | F | η2 | Significant Post Hoc |
| ISI | 13.8 (3.3) | 18.8 (3.1) | 15.2 (3.8) | 12.2 (2.2) | 12.8 (2.3) | 14.9 (3.3) | 58.4 *** | 0.33 | 1:2;1:3;1:4;1:5;2:3;2:4;3:5;4:5 |
| PSQI total | 9.5 (2.8) | 11.6 (1.6) | 12.7 (2.3) | 6.6 (1.5) | 8.6 (1.6) | 12.7 (1.2) | 216.5 *** | 0.64 | 1:2;1:3;1:4;1:5;2:3;2:4;3:4;3:5;4:5 |
| PSQI perceived sleep quality | 1.9 (0.6) | 2.6 (0.5) | 2.0 (0.6) | 1.7 (0.6) | 1.8 (0.5) | 2.2 (0.6) | 30.2 *** | 0.2 | 1:2;1:3;1:4;1:5;2:3;2:4;3:5;4:5 |
| PSQI sleep latency | 2.1 (0.9) | 2.6 (0.7) | 2.5 (0.7) | 0.7 (0.5) | 2.4 (0.5) | 2.7 (0.6) | 210.5 *** | 0.64 | 1:3;2:3;3:4;3:5;4:5 |
| PSQI sleep duration | 1.0 (0.6) | 1.1 (0.5) | 1.1 (0.8) | 0.9 (0.6) | 0.8 (0.5) | 2.1 (0.6) | 44.2 *** | 0.27 | 1:5;2:3;2:4;2:5;3:5;4:5 |
| PSQI habitual sleep efficiency | 1.0 (1.0) | 0.9 (0.8) | 1.2 (1.1) | 0.5 (0.8) | 0.8 (0.8) | 2.7 (0.6) | 57.3 *** | 0.32 | 1:5;2:3;2:4;2:5;3:5;4:5 |
| PSQI sleep disturbances | 1.6 (0.6) | 2.3 (0.5) | 1.7 (0.6) | 1.3 (0.5) | 1.5 (0.5) | 1.7 (0.5) | 30.0 *** | 0.2 | 1:2;1:3;1:4;1:5;2:3;2:4;3:5 |
| PSQI sleep medication use | 0.5 (1.0) | 0.1 (0.4) | 2.6 (0.5) | 0.1 (0.2) | 0.0 (0.2) | 0.1 (0.3) | 931.2 *** a | 0.89 a | 1:2;2:3;2:4;2:5 |
| PSQI daytime dysfunction | 1.5 (0.7) | 2.1 (0.7) | 1.6 (0.7) | 1.4 (0.6) | 1.3 (0.6) | 1.3 (0.6) | 13.3 *** | 0.10 | 1:2;1:3;1:4;1:5;2:4 |
| DASS-21 anxiety | 9.7 (5.1) | 13.8 (4.9) | 11.2 (5.1) | 8.1 (4.6) | 9.0 (4.8) | 10.3 (4.9) | 13.9 *** | 0.10 | 1:2;1:3;1:4;1:5;2:3;2:4 |
| DASS-21 depression | 12.3 (5.3) | 16.1 (4.6) | 13.2 (5.3) | 11.4 (5.1) | 11.6 (5.2) | 13.0 (5.2) | 8.5 *** | 0.07 | 1:2;1:3;1:4 |
| DASS-21 stress | 14.9 (4.0) | 18.0 (2.9) | 15.9 (3.7) | 14.1 (4.1) | 14.2 (3.9) | 15.2 (3.6) | 11.2 *** | 0.08 | 1:3;1:4;1:5;2:3;2:4 |
| SF-12 PCS | 50.3 (7.9) | 45.7 (8.0) | 48.6 (9.1) | 51.6 (7.9) | 51.3 (7.1) | 49.4 (7.8) | 6.6 *** | 0.05 | 1:3;1:4 |
| SF-12 MCS | 30.2 (8.4) | 26.5 (8.3) | 29.4 (8.4) | 31.1 (8.8) | 30.6 (8.2) | 30.5 (8.3) | 2.8 * | 0.02 | 1:3;1:4 |
| Model | AIC | BIC | SABIC | Entropy | BLRT | BLRT p-Value |
|---|---|---|---|---|---|---|
| 2 classes | 10,820.77 | 10,925.63 | 10,846.28 | 0.83 | 345.7 | 0.01 |
| 3 classes | 10,738.86 | 10,881.47 | 10,773.56 | 0.77 | 99.9 | 0.01 |
| 4 classes | 10,121.82 | 10,302.18 | 10,165.7 | 0.81 | 635.04 | 0.01 |
| 5 classes | 10,045.95 | 10,264.06 | 10,099.01 | 0.83 | 93.88 | 0.01 |
| 6 classes | 10,048.15 | 10,304.01 | 10,110.4 | 0.80 | 15.8 | 0.17 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carpi, M.; Marques, D.R.; Milanese, A.; Vestri, A. Sleep Quality and Insomnia Severity among Italian University Students: A Latent Profile Analysis. J. Clin. Med. 2022, 11, 4069. https://doi.org/10.3390/jcm11144069
Carpi M, Marques DR, Milanese A, Vestri A. Sleep Quality and Insomnia Severity among Italian University Students: A Latent Profile Analysis. Journal of Clinical Medicine. 2022; 11(14):4069. https://doi.org/10.3390/jcm11144069
Chicago/Turabian StyleCarpi, Matteo, Daniel Ruivo Marques, Alberto Milanese, and Annarita Vestri. 2022. "Sleep Quality and Insomnia Severity among Italian University Students: A Latent Profile Analysis" Journal of Clinical Medicine 11, no. 14: 4069. https://doi.org/10.3390/jcm11144069
APA StyleCarpi, M., Marques, D. R., Milanese, A., & Vestri, A. (2022). Sleep Quality and Insomnia Severity among Italian University Students: A Latent Profile Analysis. Journal of Clinical Medicine, 11(14), 4069. https://doi.org/10.3390/jcm11144069






