The Value of Cardiopulmonary Exercise Testing in Predicting the Severity of Coronary Artery Disease
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Patients
2.2. Data Collection
2.3. CPET
2.4. Coronary Angiography
2.5. QFR
2.6. Gensini Score
2.7. Assignment and Grouping
- (1)
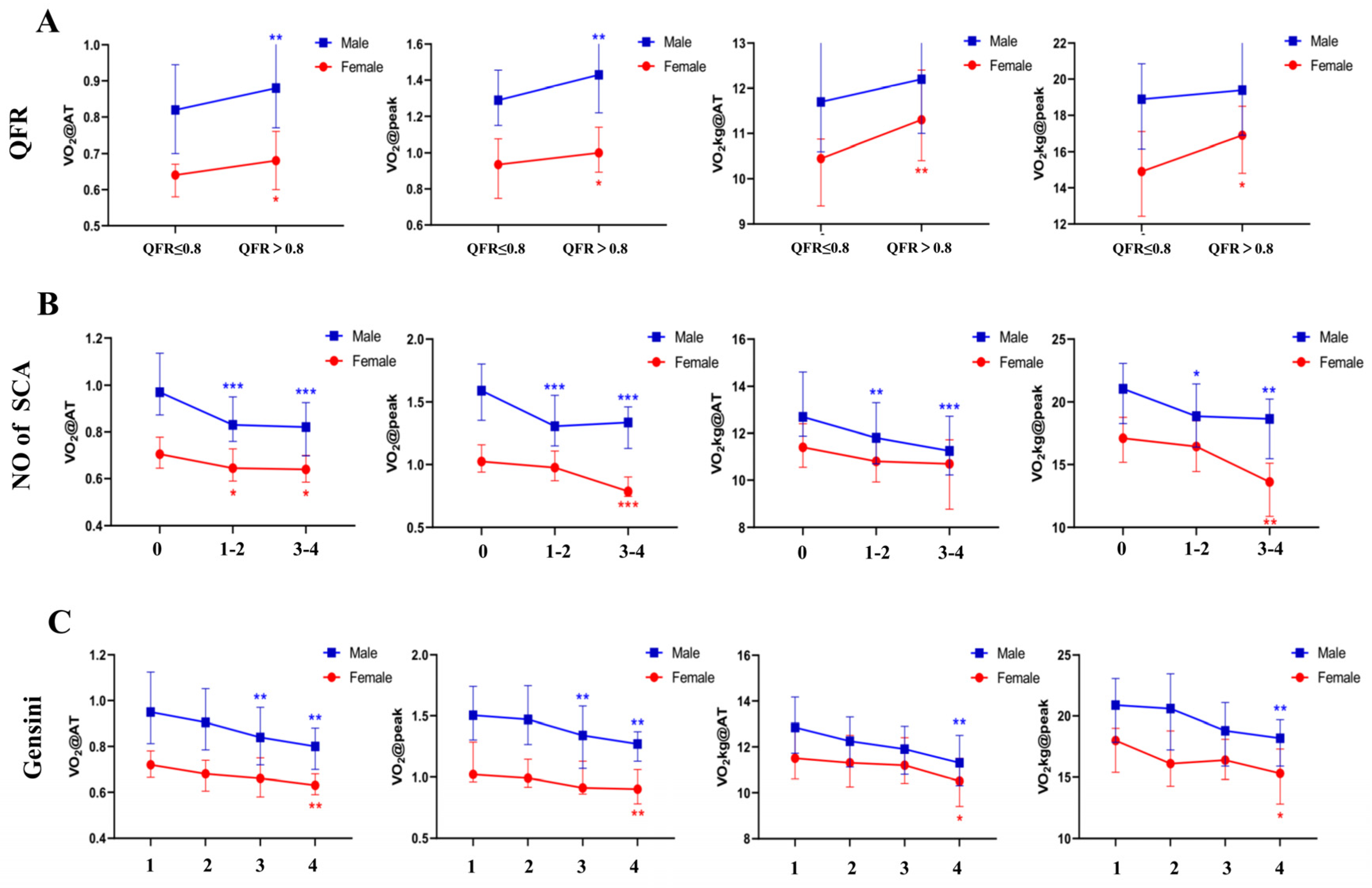
- QFR assignment and grouping. The enrolled patients were divided into two groups according to QFR (QFR > 0.8 and QFR ≤ 0.8). Those with one or more than one coronary arteries with QFR ≤ 0.8 were assigned 0, while the patients with no coronary artery with QFR ≤ 0.8 were assigned 1.
- (2)
- The patients were divided into three groups, according to the number of stenotic coronary artery (0, 1–2 and 3–4, respectively). Assignment of CPET indices (VO2@peak, VO2@AT, VO2kg@peak and VO2@AT). VO2@peak, VO2@AT, VO2kg@peak and VO2@AT of the male and female patients were arranged in descending order, respectively, and divided into four equal groups, with values of 1, 2, 3 and 4.
- (3)
- Gensini scores were grouped by quartile. The four groups of males were group 1 (Gensini score ≤ 6.0), group 2 (6.0 < Gensini score ≤ 12.5), group 3 (12.5 < Gensini score ≤ 27.5) and group 4 (Gensini score > 27.5), respectively. The four groups of females were group 1 (Gensini score ≤ 3.0), group 2 (3.0 < Gensini score ≤ 7.5), group 3 (7.5 < Gensini score ≤ 14.5) and group 4 (Gensini score > 14.5), respectively. Then the enrolled subjects were divided into the four groups according to their Gensini score.
2.8. Statistical Analysis
3. Results
3.1. Study Participants
3.2. CRF Was Correlated with QFR
3.3. CRF Showed Negative Correlation with the Number of Stenotic Coronary Arteries (SCA)
3.4. CRF Was Correlated with Gensini Score
3.5. The Diagnostic Value and Predictors of the Severity of the Coronary Lesions
4. Discussion
5. Conclusions
6. Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Guazzi, M.; Bandera, F.; Ozemek, C.; Systrom, D.; Arena, R. Cardiopulmonary Exercise Testing: What Is its Value? J. Am. Coll. Cardiol. 2017, 70, 1618–1636. [Google Scholar] [CrossRef] [PubMed]
- Albouaini, K.; Egred, M.; Alahmar, A.; Wright, D.J. Cardiopulmonary exercise testing and its application. Heart 2007, 93, 1285–1292. [Google Scholar] [CrossRef] [PubMed]
- Guazzi, M.; Arena, R.; Halle, M.; Piepoli, M.F.; Myers, J.; Lavie, C.J. 2016 Focused Update: Clinical Recommendations for Cardiopulmonary Exercise Testing Data Assessment in Specific Patient Populations. Circulation 2016, 133, e694–e711. [Google Scholar] [CrossRef] [Green Version]
- Malhotra, R.; Bakken, K.; D’Elia, E.; Lewis, G.D. Cardiopulmonary Exercise Testing in Heart Failure. JACC Heart Fail. 2016, 4, 607–616. [Google Scholar] [CrossRef] [PubMed]
- Pelliccia, A.; Sharma, S.; Gati, S.; Back, M.; Borjesson, M.; Caselli, S.; Collet, J.P.; Corrado, D.; Drezner, J.A.; Halle, M.; et al. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur. Heart J. 2021, 42, 17–96. [Google Scholar] [CrossRef]
- Mazaheri, R.; Shakerian, F.; Vasheghani-Farahani, A.; Halabchi, F.; Mirshahi, M.; Mansournia, M.A. The usefulness of cardiopulmonary exercise testing in assessment of patients with suspected coronary artery disease. Postgrad. Med. J. 2016, 92, 328–332. [Google Scholar] [CrossRef]
- Akinci Ozyurek, B.; Savas Bozbas, S.; Aydinalp, A.; Bozbas, H.; Ulubay, G. Value of cardiopulmonary exercise testing in the diagnosis of coronary artery disease. Tuberk Toraks 2019, 67, 102–107. [Google Scholar] [CrossRef]
- Belardinelli, R.; Lacalaprice, F.; Tiano, L.; Mucai, A.; Perna, G.P. Cardiopulmonary exercise testing is more accurate than ECG-stress testing in diagnosing myocardial ischemia in subjects with chest pain. Int. J. Cardiol. 2014, 174, 337–342. [Google Scholar] [CrossRef]
- Boden, W.E.; O’Rourke, R.A.; Teo, K.K.; Hartigan, P.M.; Maron, D.J.; Kostuk, W.J.; Knudtson, M.; Dada, M.; Casperson, P.; Harris, C.L.; et al. Optimal medical therapy with or without PCI for stable coronary disease. N. Engl. J. Med. 2007, 356, 1503–1516. [Google Scholar] [CrossRef] [Green Version]
- De Bruyne, B.; Pijls, N.H.; Kalesan, B.; Barbato, E.; Tonino, P.A.; Piroth, Z.; Jagic, N.; Mobius-Winkler, S.; Rioufol, G.; Witt, N.; et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N. Engl. J. Med. 2012, 367, 991–1001. [Google Scholar] [CrossRef] [Green Version]
- Banerjee, A.; Newman, D.R.; Van den Bruel, A.; Heneghan, C. Diagnostic accuracy of exercise stress testing for coronary artery disease: A systematic review and meta-analysis of prospective studies. Int. J. Clin. Pract. 2012, 66, 477–492. [Google Scholar] [CrossRef] [PubMed]
- Chaudhry, S.; Arena, R.; Bhatt, D.L.; Verma, S.; Kumar, N. A practical clinical approach to utilize cardiopulmonary exercise testing in the evaluation and management of coronary artery disease: A primer for cardiologists. Curr. Opin. Cardiol. 2018, 33, 168–177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Douglas, P.S.; Hoffmann, U.; Patel, M.R.; Mark, D.B.; Al-Khalidi, H.R.; Cavanaugh, B.; Cole, J.; Dolor, R.J.; Fordyce, C.B.; Huang, M.; et al. Outcomes of anatomical versus functional testing for coronary artery disease. N. Engl. J. Med. 2015, 372, 1291–1300. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Letnes, J.M.; Dalen, H.; Vesterbekkmo, E.K.; Wisloff, U.; Nes, B.M. Peak oxygen uptake and incident coronary heart disease in a healthy population: The HUNT Fitness Study. Eur. Heart J. 2019, 40, 1633–1639. [Google Scholar] [CrossRef] [PubMed]
- Tousoulis, D.; Siasos, G.; Maniatis, K.; Oikonomou, E.; Kioufis, S.; Zaromitidou, M.; Paraskevopoulos, T.; Michalea, S.; Kollia, C.; Miliou, A.; et al. Serum osteoprotegerin and osteopontin levels are associated with arterial stiffness and the presence and severity of coronary artery disease. Int. J. Cardiol. 2013, 167, 1924–1928. [Google Scholar] [CrossRef]
- Tveit, S.H.; Cwikiel, J.; Myhre, P.L.; Omland, T.; Berge, E.; Seljeflot, I.; Flaa, A. Differential associations of cardiac troponin T and cardiac troponin I with coronary artery pathology and dynamics in response to short-duration exercise. Clin. Biochem. 2021, 88, 23–29. [Google Scholar] [CrossRef]
- Pencina, M.J.; D’Agostino, R.B., Sr.; Steyerberg, E.W. Extensions of net reclassification improvement calculations to measure usefulness of new biomarkers. Stat. Med. 2011, 30, 11–21. [Google Scholar] [CrossRef]
- Popovic, D.; Guazzi, M.; Jakovljevic, D.G.; Lasica, R.; Banovic, M.; Ostojic, M.; Arena, R. Quantification of coronary artery disease using different modalities of cardiopulmonary exercise testing. Int. J. Cardiol. 2019, 285, 11–13. [Google Scholar] [CrossRef]
- Engstrom, T.; Kelbaek, H.; Helqvist, S.; Hofsten, D.E.; Klovgaard, L.; Holmvang, L.; Jorgensen, E.; Pedersen, F.; Saunamaki, K.; Clemmensen, P.; et al. Complete revascularisation versus treatment of the culprit lesion only in patients with ST-segment elevation myocardial infarction and multivessel disease (DANAMI-3-PRIMULTI): An open-label, randomised controlled trial. Lancet 2015, 386, 665–671. [Google Scholar] [CrossRef]
- Zhang, R.; Song, C.; Guan, C.; Liu, Q.; Wang, C.; Xie, L.; Sun, Z.; Cai, M.; Zhang, M.; Wang, H.; et al. Prognostic Value of Quantitative Flow Ratio Based Functional SYNTAX Score in Patients With Left Main or Multivessel Coronary Artery Disease. Circ. Cardiovasc. Interv. 2020, 13, e009155. [Google Scholar] [CrossRef]
- Tu, S.; Westra, J.; Yang, J.; von Birgelen, C.; Ferrara, A.; Pellicano, M.; Nef, H.; Tebaldi, M.; Murasato, Y.; Lansky, A.; et al. Diagnostic Accuracy of Fast Computational Approaches to Derive Fractional Flow Reserve From Diagnostic Coronary Angiography: The International Multicenter FAVOR Pilot Study. JACC Cardiovasc. Interv. 2016, 9, 2024–2035. [Google Scholar] [CrossRef] [PubMed]
- Swift, D.L.; Lavie, C.J.; Johannsen, N.M.; Arena, R.; Earnest, C.P.; O’Keefe, J.H.; Milani, R.V.; Blair, S.N.; Church, T.S. Physical activity, cardiorespiratory fitness, and exercise training in primary and secondary coronary prevention. Circ. J. 2013, 77, 281–292. [Google Scholar] [CrossRef] [Green Version]
- Myers, J.; McAuley, P.; Lavie, C.J.; Despres, J.P.; Arena, R.; Kokkinos, P. Physical activity and cardiorespiratory fitness as major markers of cardiovascular risk: Their independent and interwoven importance to health status. Prog. Cardiovasc. Dis. 2015, 57, 306–314. [Google Scholar] [CrossRef]
- Wu, N.N.; Tian, H.; Chen, P.; Wang, D.; Ren, J.; Zhang, Y. Physical Exercise and Selective Autophagy: Benefit and Risk on Cardiovascular Health. Cells 2019, 8, 1436. [Google Scholar] [CrossRef] [Green Version]
- Kaminsky, L.A.; Arena, R.; Ellingsen, O.; Harber, M.P.; Myers, J.; Ozemek, C.; Ross, R. Cardiorespiratory fitness and cardiovascular disease—The past, present, and future. Prog. Cardiovasc. Dis. 2019, 62, 86–93. [Google Scholar] [CrossRef]
- Kaminsky, L.A.; Imboden, M.T.; Arena, R.; Myers, J. Reference Standards for Cardiorespiratory Fitness Measured With Cardiopulmonary Exercise Testing Using Cycle Ergometry: Data From the Fitness Registry and the Importance of Exercise National Database (FRIEND) Registry. Mayo. Clin. Proc. 2017, 92, 228–233. [Google Scholar] [CrossRef]
- Lee, D.C.; Sui, X.; Artero, E.G.; Lee, I.M.; Church, T.S.; McAuley, P.A.; Stanford, F.C.; Kohl, H.W., 3rd; Blair, S.N. Long-term effects of changes in cardiorespiratory fitness and body mass index on all-cause and cardiovascular disease mortality in men: The Aerobics Center Longitudinal Study. Circulation 2011, 124, 2483–2490. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kodama, S.; Saito, K.; Tanaka, S.; Maki, M.; Yachi, Y.; Asumi, M.; Sugawara, A.; Totsuka, K.; Shimano, H.; Ohashi, Y.; et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: A meta-analysis. JAMA 2009, 301, 2024–2035. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khan, H.; Jaffar, N.; Rauramaa, R.; Kurl, S.; Savonen, K.; Laukkanen, J.A. Cardiorespiratory fitness and nonfatalcardiovascular events: A population-based follow-up study. Am. Heart J. 2017, 184, 55–61. [Google Scholar] [CrossRef]
- Ribeiro, P.A.B.; Boidin, M.; Juneau, M.; Nigam, A.; Gayda, M. High-intensity interval training in patients with coronary heart disease: Prescription models and perspectives. Ann. Phys. Rehabil. Med. 2017, 60, 50–57. [Google Scholar] [CrossRef] [Green Version]
- Cattadori, G.; Di Marco, S.; Farina, S.; Limongelli, G.; Monda, E.; Badagliacca, R.; Papa, S.; Tricarico, L.; Correale, M. Beta-blockers in heart failure prognosis: Lessons learned by MECKI Score Group papers. Eur. J. Prev. Cardiol. 2020, 27, 65–71. [Google Scholar] [CrossRef] [PubMed]

| Variable | Total (n = 280) |
|---|---|
| Age (y) | 56.74 ± 8.27 |
| BMI (kg/m2) | 25.11 ± 3.07 |
| Height (cm) | 166.35 ± 7.86 |
| Body weight (kg) | 69.59 ± 10.54 |
| Comorbidities (n, %) | |
| Myocardial infarction | 39 (13.9) |
| Arrhythmia | 41 (14.6) |
| Hypertension | 165 (59.0) |
| Hyperlipemia | 80 (28.6) |
| Cardiac insufficiency | 21 (7.5) |
| Diabetic mellitus | 83 (29.6) |
| Thyroid dysfunction | 16 (5.7) |
| Noncardiogenic chest pain | 77 (27.5) |
| Cerebrovascular disease | 24 (8.6) |
| Medications (n, %) | |
| Aspirin | 241 (86.1) |
| Antiplatelet agents (Ticagrelor or Clopidogrel) | 210 (75) |
| Statins | 212 (75.7) |
| ACEI or ARB | 96 (34.3) |
| CCB | 84 (30.0) |
| β-blocker | 171 (61.1) |
| Nitrates | 31 (11.1) |
| Anti-arrhythmia agent | 17 (6.1) |
| Hypoglycemic drugs or insulin | 23 (8.2) |
| CPET | |
| VO2@AT (L/min) | 0.79 (0.69, 0.93) |
| VO2@peak (L/min) | 1.24 (1.01, 1.47) |
| VO2kg@AT (mL/min/kg) | 11.60 (10.70, 13.10) |
| VO2kg@peak (mL/min/kg) | 18.20 (15.80, 20.90) |
| RER@peak | 1.18 (1.09, 1.24) |
| VO2@AT/VO2prediction (%) | 43.3 (38.2, 50.9) |
| VO2@peak/VO2prediction (%) | 67.5 (59.6, 77.2) |
| CPET Parameters | Male | Female | ||
|---|---|---|---|---|
| r | p Value | r | p Value | |
| VO2@peak (L/min) | 0.176 | 0.016 | 0.231 | 0.027 |
| VO2@AT (L/min) | 0.161 | 0.027 | 0.212 | 0.043 |
| VO2kg@peak (mL/min/kg) | 0.094 | 0.200 | 0.212 | 0.044 |
| VO2kg@AT (mL/min/kg) | 0.067 | 0.361 | 0.277 | 0.008 |
| CPET Parameters | Male | Female | ||
|---|---|---|---|---|
| τ | p Value | τ | p Value | |
| VO2@peak (L/min) | −0.307 | 0.000 | −0.230 | 0.01 |
| VO2@AT (L/min) | −0.312 | 0.000 | −0.261 | 0.004 |
| VO2kg@peak (mL/min/kg) | −0.235 | 0.000 | −0.158 | 0.08 |
| VO2kg@AT (mL/min/kg) | −0.245 | 0.000 | −0.172 | 0.056 |
| CPET Parameters | Male (n = 188) | Female (n = 92) | ||
|---|---|---|---|---|
| R (Spearman Coefficient) | p-Value | R (Spearman Coefficient) | p-Value | |
| VO2@AT (L/min) | −0.406 | 0.000 | −0.368 | 0.000 |
| VO2/kg@AT (L/min) | −0.308 | 0.000 | −0.259 | 0.013 |
| VO2@peak (mL/min/kg) | −0.425 | 0.000 | −0.338 | 0.001 |
| VO2/kg@peak (mL/min/kg) | −0.326 | 0.000 | −0.241 | 0.022 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, W.; Liu, X.; Liu, T.; Xie, Y.; He, X.; Zuo, H.; Zeng, H. The Value of Cardiopulmonary Exercise Testing in Predicting the Severity of Coronary Artery Disease. J. Clin. Med. 2022, 11, 4170. https://doi.org/10.3390/jcm11144170
Liu W, Liu X, Liu T, Xie Y, He X, Zuo H, Zeng H. The Value of Cardiopulmonary Exercise Testing in Predicting the Severity of Coronary Artery Disease. Journal of Clinical Medicine. 2022; 11(14):4170. https://doi.org/10.3390/jcm11144170
Chicago/Turabian StyleLiu, Wanjun, Xiaolei Liu, Tao Liu, Yang Xie, Xingwei He, Houjuan Zuo, and Hesong Zeng. 2022. "The Value of Cardiopulmonary Exercise Testing in Predicting the Severity of Coronary Artery Disease" Journal of Clinical Medicine 11, no. 14: 4170. https://doi.org/10.3390/jcm11144170
APA StyleLiu, W., Liu, X., Liu, T., Xie, Y., He, X., Zuo, H., & Zeng, H. (2022). The Value of Cardiopulmonary Exercise Testing in Predicting the Severity of Coronary Artery Disease. Journal of Clinical Medicine, 11(14), 4170. https://doi.org/10.3390/jcm11144170





