The Interdisciplinary Management of Lung Cancer in the European Community
Abstract
:1. Introduction
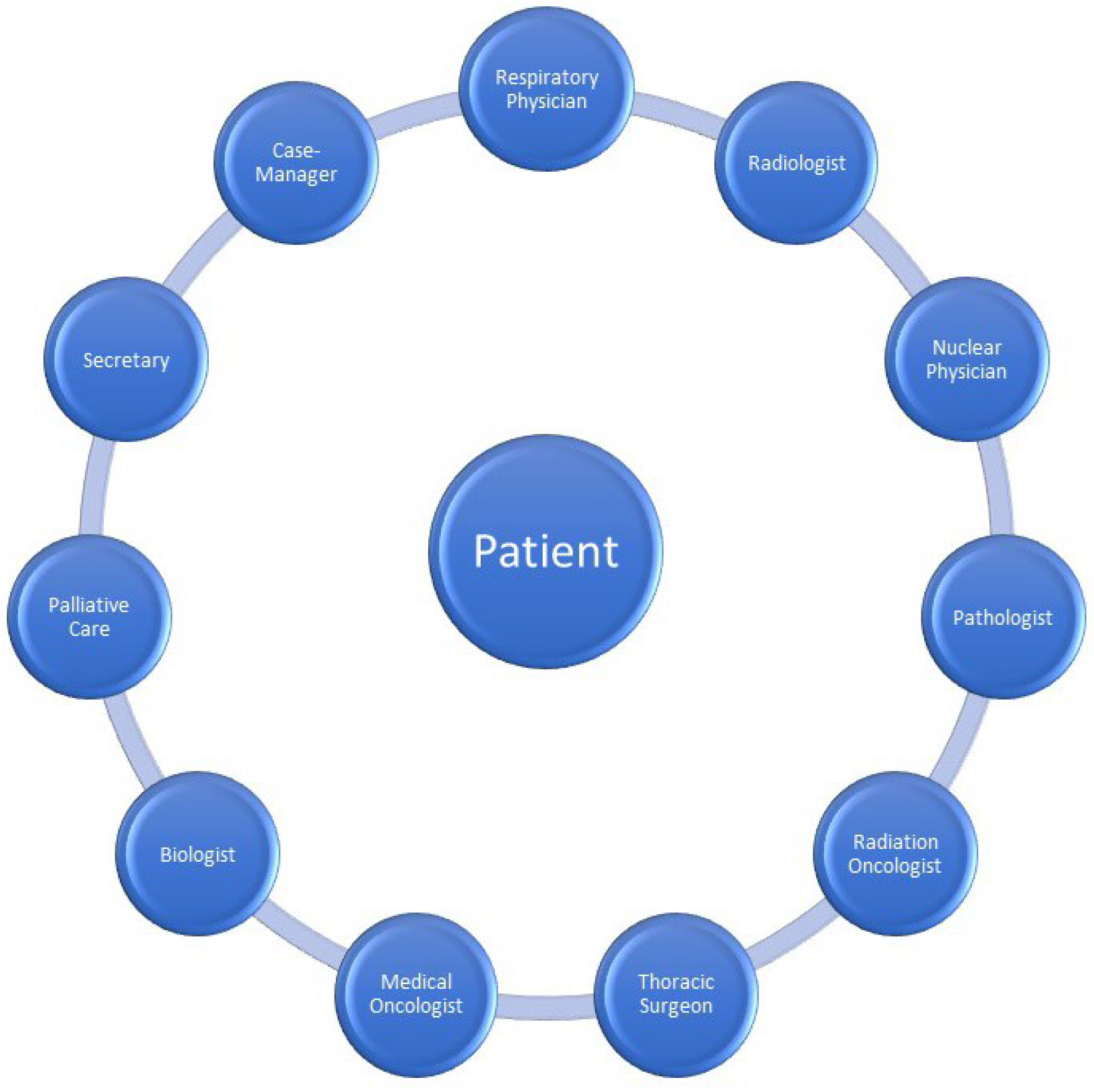
2. Interdisciplinary Service
3. Multidisciplinary Meeting Roles and Responsibilities
3.1. Respiratory Physician
3.2. Medical Oncologists
3.3. Radiation Oncologist
3.4. Thoracic Surgeon
3.5. Palliative Care
3.6. Radiologists and Nuclear Medicine Physicians
3.7. Pathologist
3.8. Biologist
3.9. Clinical Nurse Specialist
3.10. Psychologist
4. Impact on Survival
5. Treatment Utilisation
5.1. Surgery
5.2. Radiation Therapy
5.3. Targeted Therapies or Immunotherapy
5.4. Guideline Treatment
5.5. Timeliness of Care
5.6. Palliative Care, Quality of Life, Patient Satisfaction
6. Discussion
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- American Society of Clinical Oncology; European Society for Medical Oncology. ASCO-ESMO consensus statement on quality cancer care. Ann. Oncol. 2006, 17, 1063–1064. [Google Scholar] [CrossRef] [PubMed]
- Gouveia, J.; Coleman, M.; Haward, R.; Zanetti, R.; Hakama, M.; Borras, J.M.; Primic-Žakelj, M.; de Koning, H.J.; Travado, L. Improving cancer control in the European Union: Conclusions from the Lisbon roundtable under the Portuguese EU presidency, 2007. Eur. J. Cancer 2008, 44, 1457–1462. [Google Scholar] [CrossRef] [PubMed]
- Gaga, M.; Powell, C.A.; Schraufnagel, D.E.; Schönfeld, N.; Rabe, K.; Hill, N.S.; Sculier, J.-P. An official American Thoracic Society/European Respiratory Society statement: The role of the pulmonologist in diagnosing and managing lung cancer. Am. J. Respir. Crit. Care Med. 2013, 188, 503–507. [Google Scholar] [CrossRef] [Green Version]
- Hardavella, G.; Frille, A.; Theochari, C.; Keramida, E.; Bellou, E.; Fotineas, A.; Bracka, I.; Pappa, L.; Zagana, V.; Palamiotou, M.; et al. Multidisciplinary care models for patients with lung cancer. Breathe 2020, 16, 200076. [Google Scholar] [CrossRef]
- Haas, M.; Mortensen, M. The secrets of great teamwork. Harv. Bus. Rev. 2016, 94, 70–76. [Google Scholar] [PubMed]
- World Health Organization. Framework for Action on Interprofessional Education and Collaborative Practice; World Health Organization: Geneva, Switzerland, 2010. Available online: www.who.int/hrh/resources/framework_action/en/index.html (accessed on 26 April 2020).
- Royal College of Physicians. Respiratory Medicine: Workforce and Job Planning. Available online: www.rcpmedicalcare.org.uk/developingphysicians/specialties/respiratory-medicine/workforce (accessed on 20 April 2020).
- Denton, E.; Conron, M. Improving outcomes in lung cancer: The value of the multidisciplinary health care team. J. Multidiscip. Healthc. 2016, 9, 137–144. [Google Scholar]
- Ruhstaller, T.; Roe, H.; Thürlimann, B.; Nicoll, J.J. The multidisciplinary meeting: An indispensable aid to communication between different specialties. Eur. J. Cancer 2006, 42, 2459–2462. [Google Scholar] [CrossRef]
- Mathioudakis, A.; Rousalova, I.; Gagnat, A.A.; Saad, N.; Hardavella, G. How to keep good clinical records. Breathe 2016, 12, 369–373. [Google Scholar] [CrossRef] [Green Version]
- Jalil, R.; Lamb, B.; Russ, S.; Sevdalis, N.; Green, J.S.A. The cancer multidisciplinary team from the coordinators’ perspective: Results from a national survey in the UK. BMC Health Serv. Res. 2012, 12, 457. [Google Scholar] [CrossRef] [Green Version]
- Nancarrow, S.; Booth, A.; Ariss, S.; Smith, T.; Enderby, P.; Roots, A. Ten principles of good interdisciplinary teamwork. Hum. Resour. Health 2013, 11, 19. [Google Scholar] [CrossRef] [Green Version]
- Gamarra, F.; Noël, J.L.; Brunelli, A.; Dingemans, A.-M.C.; Felip, E.; Gaga, M.; Grigoriu, B.D.; Hardavella, G.; Huber, R.M.; Janes, S.; et al. Thoracic oncology HERMES: European curriculum recommendations for training in thoracic oncology. Breathe 2016, 12, 249–255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hardavella, G.; Gaga, M. Harmonising Education in Thoracic Oncology in Europe; European Recommendations for integrated training. Pneumon 2016, 29, 203–205. [Google Scholar]
- Shaw, D.J.; Davidson, J.E.; Smilde, R.I.; Sondoozi, T.; Agan, D. Multidisciplinary team training to enhance family communication in the ICU. Crit. Care Med. 2014, 42, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Cancer Australia. All about Multidisciplinary Care. Available online: www.canceraustralia.gov.au/clinical-best-practice/multidisciplinary-care/all-about-multidisciplinary-care (accessed on 20 April 2020).
- European Society for Medical Oncology. ESMO Management and Treatment Adapted Recommendations in the COVID-19 Era: Lung Cancer. Available online: www.esmo.org/guidelines/cancer-patientmanagement-during-the-covid-19-pandemic/lung-cancerin-the-covid-19-era (accessed on 28 August 2020).
- Osarogiagbon, R.U.; Freeman, R.K.; Krasna, M.J. Implementing effective and sustainable multidisciplinary clinical thoracic oncology programs. Transl. Lung Cancer Res. 2015, 4, 448–455. [Google Scholar] [PubMed]
- National Lung Cancer Working Group. Lung Cancer Multidisciplinary Meeting Toolkit; Ministry of Health: Wellington, New Zealand, 2014.
- Patkar, V.; Acosta, D.; Davidson, T.; Jones, A.; Fox, J.; Keshtgar, M. Cancer multidisciplinary team meetings: Evidence, challenges, and the role of clinical decision support technology. Int. J. Breast Cancer 2011, 2011, 831605. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jemal, A.; Ward, E.; Thun, M. Declining death rates reflect progress against cancer. PLoS ONE 2010, 5, e9584. [Google Scholar] [CrossRef] [Green Version]
- Hardavella, G.; George, J. Interventional bronchoscopy in the management of thoracic malignancy. Breathe 2015, 11, 202–212. [Google Scholar] [CrossRef] [Green Version]
- Popescu, R.A.; Schaefer, R.; Califano, R.; Eckert, R.; Coleman, R.; Douillard, J.-Y.; Cervantes, A.; Casali, P.G.; Sessa, C.; van Cutsem, E.; et al. The current and future role of the medical oncologist in the professional care for cancer patients: A position paper by the European Society for Medical Oncology (ESMO). Ann. Oncol. 2014, 25, 9–15. [Google Scholar] [CrossRef]
- Cherny, N.I.; Catane, R.; Kosmidis, P. ESMO takes a stand on supportive and palliative care. Ann. Oncol. 2003, 14, 1335–1337. [Google Scholar] [CrossRef] [PubMed]
- Basse, C.; Morel, C.; Alt, M.; Sablin, M.P.; Franck, C.; Pierron, G.; Callens, C.; Melaabi, S.; Masliah-Planchon, J.; Bataillon, G.; et al. Relevance of a molecular tumour board (MTB) for patients’ enrolment in clinical trials: Experience of the Institut Curie. ESMO Open 2018, 3, e000339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salomaa, E.R.; Sällinen, S.; Hiekkanen, H.; Kari, L. Delays in the diagnosis and treatment of lung cancer. Chest 2005, 128, 2282–2288. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Falcoz, P.E.; Puyraveau, M.; Rivera, C.M.; Bernard, A.; Massard, G.; Mauny, F.; Dahan, M.; Thomas, P.; Epithor Group. The impact of hospital and surgeon volume on the 30-day mortality of lung cancer surgery: A nation-based reappraisal. J. Thorac. Cardiovasc. Surg. 2014, 148, 841–848. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Massard, G.; Antonoff, M.B.; Noel, J.L.; Brunelli, A.; Farjah, F.; Lanuti, M.; van Raemdonck, D. Transatlantic editorial: Thoracic surgeons need recognition of competence in thoracic oncology. J. Thorac. Cardiovasc. Surg. 2017, 154, 1387–1392. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spronk, I.; Meijers, M.C.; Heins, M.J.; Francke, A.L.; Elwyn, G.; van Lindert, A.; van Dulmen, S.; van Vliet, L.M. Availability and effectiveness of decision aids for supporting shared decision making in patients with advanced colorectal and lung cancer: Results from a systematic review. Eur. J. Cancer Care 2019, 28, e13079. [Google Scholar] [CrossRef] [Green Version]
- Temel, J.S.; Greer, J.A.; Muzikansky, A.; Gallagher, E.R.; Admane, S.; Jackson, V.A.; Dahlin, C.M.; Blinderman, C.D.; Jacobsen, J.; Pirl, W.F.; et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N. Engl. J. Med. 2010, 363, 733–742. [Google Scholar] [CrossRef] [Green Version]
- Prabhakar, C.N.; Fong, K.M.; Peake, M.D.; Lam, D.C.; Barnes, D.J. The effectiveness of lung cancer MDT and the role of respiratory physicians. Respirology 2015, 20, 884–888. [Google Scholar] [CrossRef]
- Lim, E.; Baldwin, D.; Beckles, M.; Duffy, J.; Entwisle, J.; Faivre-Finn, C.; Kerr, K.; Macfie, A.; McGuigan, J.; Padley, S.; et al. Guidelines on the radical management of patients with lung cancer. Thorax 2010, 65, 1–27. [Google Scholar] [CrossRef] [Green Version]
- Davidson, M.R.; Gazdar, A.F.; Clarke, B.E. The pivotal role of pathology in the management of lung cancer. J. Thorac. Dis 2013, 5 (Suppl. S5), S463–S478. [Google Scholar]
- McPhillips, D.; Evans, R.; Ryan, D.; Daneshvar, C.; Sarkar, S.A.; Breen, D. The role of a nurse specialist in a modern lung-cancer service. Br. J. Nurs. 2015, 24, S21–S27. [Google Scholar] [CrossRef]
- Baider, L.; Surbone, A. Universality of aging: Family caregivers for elderly cancer patients. Front. Psychol. 2014, 5, 744. [Google Scholar] [CrossRef]
- Castelli, L.; Binaschi, L.; Caldera, P.; Mussa, A.; Torta, R. Fast screening of depression in cancer patients: The effectiveness of the HADS. Eur. J. Cancer Care 2011, 20, 528–533. [Google Scholar] [CrossRef] [PubMed]
- Forrest, L.M.; McMillan, D.C.; McArdle, C.S.; Dunlop, D.J. An evaluation of the impact of a multidisciplinary team, in a single centre, on treatment and survival in patients with inoperable non-small-cell lung cancer. Br. J. Cancer 2005, 93, 977–978. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tamburini, N.; Maniscalco, P.; Mazzara, S.; Maietti, E.; Santini, A.; Calia, N.; Stefanelli, A.; Frassoldati, A.; Santi, I.; Rinaldi, R.; et al. Multidisciplinary management improves survival at 1 year after surgical treatment for non-small-cell lung cancer: A propensity score-matched study. Eur. J. Cardiothorac. Surg. 2018, 53, 1199–1204. [Google Scholar] [CrossRef] [PubMed]
- Price, A.; Kerr, G.; Gregor, A. 237 Oral The impact of multidisciplinary teams and site specialisation on the use of radiotherapy in elderly people with non-small cell lung cancer (NSCLC). Radiother. Oncol. 2002, 64, S80. [Google Scholar]
- Murray, P.V.; O’Brien, M.E.; Sayer, R.; Cooke, N.; Knowles, G.; Miller, A.C.; Varney, V.; Rowell, N.P.; Padhani, A.R.; MacVicar, D.; et al. The pathway study: Results of a pilot feasibility study in patients suspected of having lung carcinoma investigated in a conventional chest clinic setting compared to a centralised two-stop pathway. Lung Cancer 2003, 42, 283–290. [Google Scholar] [CrossRef]
- Passiglia, F.; Bertolaccini, L.; Del Re, M.; Facchinetti, F.; Ferrara, R.; Franchina, T.; Malapelle, U.; Menis, J.; Passaro, A.; Pilotto, S.; et al. Diagnosis and treatment of early and locally advanced non-small-cell lung cancer: The 2019 AIOM (Italian Association of Medical Oncology) clinical practice guidelines. Crit. Rev. Oncol. Hematol. 2020, 148, 102862. [Google Scholar] [CrossRef]
- Davison, A.G.; Eraut, C.D.; Haque, A.S. Telemedicine for multidisciplinary lung cancer meetings. J. Telemed. Telecare 2004, 10, 140–143. [Google Scholar] [CrossRef]
- Lin, P.; Koh, E.S.; Lin, M.; Vinod, S.K.; Ho-Shon, I.; Yap, J.; Som, S. Diagnostic and staging impact of radiotherapy planning FDG-PET-CT in non-small-cell lung cancer. Radiother. Oncol. 2011, 101, 284–290. [Google Scholar] [CrossRef]
- Mohammed, N.; Kestin, L.L.; Grills, I.S.; Battu, M.; Fitch, D.L.; Wong, C.-Y.O.; Margolis, J.H.; Chmielewski, G.W.; Welsh, R.J. Rapid disease progression with delay in treatment of non-small-cell lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 2011, 79, 466–472. [Google Scholar] [CrossRef]
- Osarogiagbon, R.U. Making the evidentiary case for universal multidisciplinary thoracic oncologic care. Clin. Lung Cancer 2018, 19, 294–300. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.; Williamson, I.; Ionescu, A.; Brewster, A.E.; Howison, H.; Williams, S.; Smith, C.; Noble, S.I.R. 97 Improving outcomes for palliative lung cancer patients: Experience of a multiprofessional parallel clinic model in a district general hospital. Lung Cancer 2012, 75, S32. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bertolaccini, L.; Mohamed, S.; Bardoni, C.; Lo Iacono, G.; Mazzella, A.; Guarize, J.; Spaggiari, L. The Interdisciplinary Management of Lung Cancer in the European Community. J. Clin. Med. 2022, 11, 4326. https://doi.org/10.3390/jcm11154326
Bertolaccini L, Mohamed S, Bardoni C, Lo Iacono G, Mazzella A, Guarize J, Spaggiari L. The Interdisciplinary Management of Lung Cancer in the European Community. Journal of Clinical Medicine. 2022; 11(15):4326. https://doi.org/10.3390/jcm11154326
Chicago/Turabian StyleBertolaccini, Luca, Shehab Mohamed, Claudia Bardoni, Giorgio Lo Iacono, Antonio Mazzella, Juliana Guarize, and Lorenzo Spaggiari. 2022. "The Interdisciplinary Management of Lung Cancer in the European Community" Journal of Clinical Medicine 11, no. 15: 4326. https://doi.org/10.3390/jcm11154326
APA StyleBertolaccini, L., Mohamed, S., Bardoni, C., Lo Iacono, G., Mazzella, A., Guarize, J., & Spaggiari, L. (2022). The Interdisciplinary Management of Lung Cancer in the European Community. Journal of Clinical Medicine, 11(15), 4326. https://doi.org/10.3390/jcm11154326







