Colostomy Reversal following Hartmann’s Procedure: The Importance of Timing in Short- and Long-Term Complications: A Retrospective Multicentric Study
Abstract
:1. Introduction
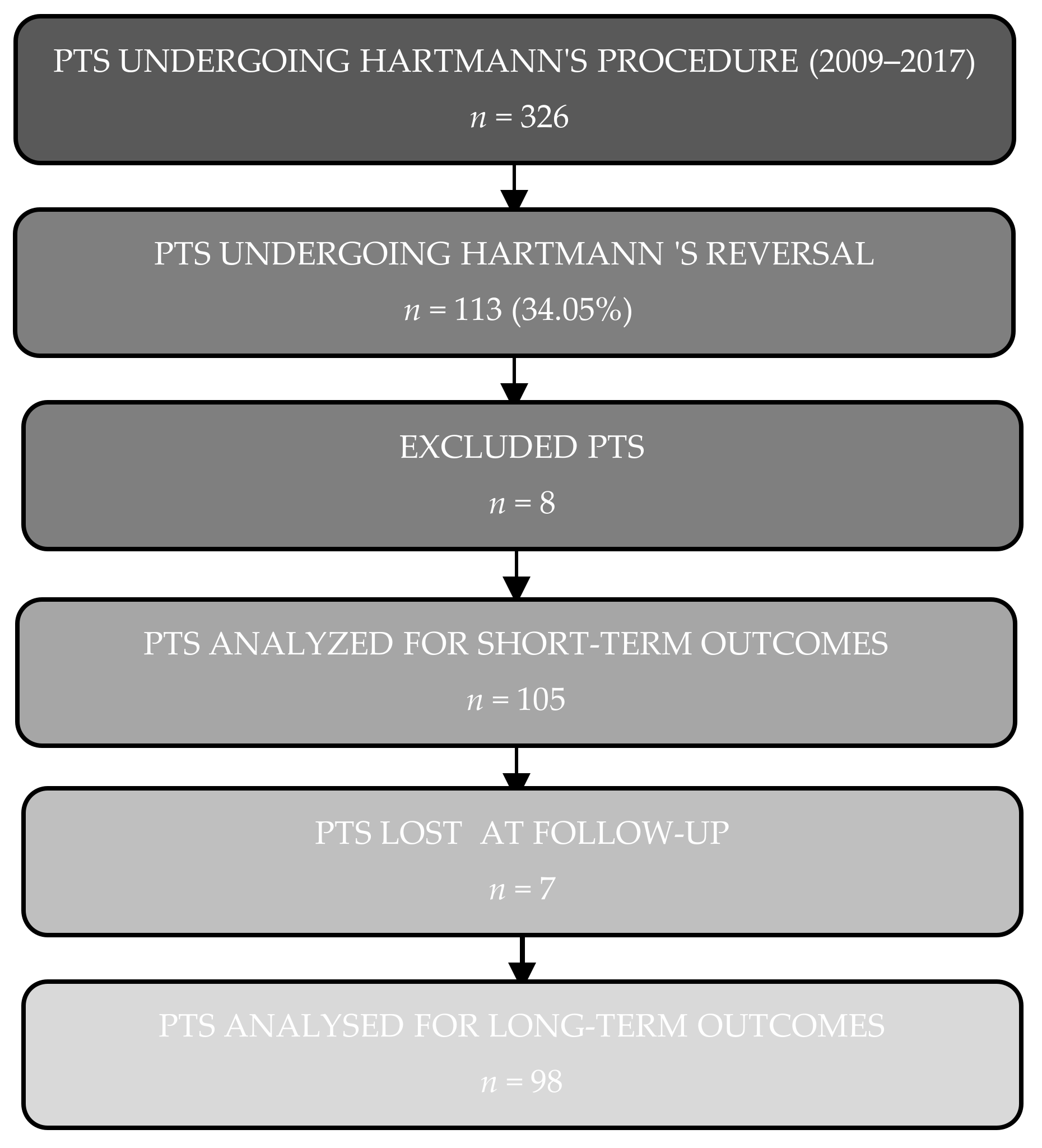
2. Patients and Methods
2.1. Study Design
2.2. Surgical Procedure
2.3. Statistical Analysis
3. Results
3.1. Patients’ Characteristics
3.2. Short-Term Outcomes
3.3. Long-Term Outcomes
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hartmann, H. Note sur un procede nouveau d’extirpation des cancers de la partie terminale du colon. Bull. Mém. Soc. Chir. Paris 1923, 49, 1474–1477. [Google Scholar]
- David, G.G.; Al-Sarira, A.A.; Willmott, S.; Cade, D.; Corless, D.J.; Slavin, J.P. Use of Hartmann’s procedure in England. Colorectal Dis. 2009, 11, 308–312. [Google Scholar] [CrossRef] [PubMed]
- Khosraviani, K.; Campbell, W.J.; Parks, T.G.; Irwin, S.T. Hartmann’s procedure revisited. Eur. J. Surg. 2000, 166, 878–881. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, S.; Leather, A.; Rennie, J.A.; Samano, N.; Gonzalez, J.G.; Papagrigoriadis, S. Feasibility and morbidity of reversal of Hartmann’s. Colorectal Dis. 2005, 7, 454–459. [Google Scholar] [CrossRef]
- Maggard, M.A.; Zingmond, D.; O’Connell, J.B.; Ko, C.Y. What proportion of patients with an ostomy (for diverticulitis) get reversed? Am. Surg. 2004, 70, 928–931. [Google Scholar]
- Roque-Castellano, C.; Marchena-Gomez, J.; Hemmersbach-Miller, M.; Acosta-Merida, A.; Rodriguez-Mendez, A.; Fariña-Castro, R.; Hernandez-Romero, J. Analysis of the factors related to the decision of restoring intestinal continuity after Hartmann’s procedure. Int. J. Colorectal Dis. 2007, 22, 1091–1096. [Google Scholar] [CrossRef]
- Horesh, N.; Rudnicki, Y.; Dreznik, Y.; Zbar, A.P.; Gutman, M.; Zmora, O.; Rosin, D. Reversal of Hartmann’s procedure: Still a complicated operation. Tech. Coloproctol. 2018, 22, 81–87. [Google Scholar] [CrossRef]
- Mealy, K.; O’Broin, E.; Donohue, J.; Tanner, A.; Keane, F.B.V. Reversible colostomy—What is the outcome? Dis. Colon Rectum 1996, 39, 1227–1231. [Google Scholar] [CrossRef]
- Desai, D.C.; Brennan, E.J.; Reilly, J.F.; Smink, R.D. The utility of the Hartmann procedure. Am. J. Surg. 1998, 175, 152–154. [Google Scholar] [CrossRef]
- Roe, A.M.; Prabhu, S.; Ali, A.; Brown, C.; Brodribb, A.J.M. Reversal of Hartmann’s procedure: Timing and operative technique. Br. J. Surg. 1991, 78, 1167–1170. [Google Scholar] [CrossRef]
- Riansuwan, W.; Hull, T.L.; Millan, M.M.; Hammel, J.P. Nonreversal of Hartmann’s procedure for diverticulitis: Derivation of a scoring system to predict nonreversal. Dis. Colon Rectum 2009, 52, 1400–1408. [Google Scholar] [CrossRef]
- Vaid, S.; Wallet, J.; Litt, J.; Bell, T.; Grim, R.; Ahuja, V. Application of a tertiary referral scoring system to predict nonreversal of Hartmann’s procedure for diverticulitis in a community hospital. Am. Surg. 2011, 77, 814–819. [Google Scholar] [CrossRef]
- Aydin, H.N.; Tekkis, P.P.; Remzi, F.H.; Constantinides, V.; Fazio, V.W. Evaluation of the risk of a nonrestorative resection for the treatment of diverticular disease: The Cleveland Clinic diverticular disease propensity score. Dis. Colon Rectum 2006, 49, 629–639. [Google Scholar] [CrossRef]
- Aquina, C.T.; Probst, C.P.; Becerra, A.Z.; Hensley, B.J.; Iannuzzi, J.C.; Noyes, K.; Monson, J.R.; Fleming, F.J. The impact of surgeon volume on colostomy reversal outcomes after Hartmann’s procedure for diverticulitis. Surgery 2016, 160, 1309–1317. [Google Scholar] [CrossRef]
- Tokode, O.M.; Akingboye, A.; Coker, O. Factors affecting reversal following Hartmann’s procedure: Experience from two district general hospitals in the UK. Surg. Today 2011, 41, 79–83. [Google Scholar] [CrossRef]
- Kang, J.H.; Kang, B.M.; Yoon, S.N.; Kim, J.Y.; Park, J.H.; Oh, B.Y.; Kim, J.W. Analysis of factors affecting reversal of Hartmann’s procedure and postreversal complications. Sci. Rep. 2020, 10, 16820. [Google Scholar] [CrossRef]
- Whitney, S.; Gross, B.D.; Mui, A.; Hahn, S.; Read, B.; Bauer, J. Hartmann’s reversal: Factors affecting complications and outcomes. Int. J. Colorectal Dis. 2020, 35, 1875–1880. [Google Scholar] [CrossRef]
- Baiocchi, G.L.; Guercioni, G.; Vettoretto, N.; Scabini, S.; Millo, P.; Muratore, A.; Clementi, M.; Sica, G.; Delrio, P.; Longo, G.; et al. ICG fluorescence imaging in colorectal surgery: A snapshot from the ICRAL study group. BMC Surg. 2021, 21, 190. [Google Scholar] [CrossRef]
- Schietroma, M.; Pessia, B.; Colozzi, S.; Carlei, F.; Clementi, M.; Amicucci, G.; Guadagni, S. Septic Complications after Resection for Middle or Low Rectal Cancer: Role of Gut Barrier Function and Inflammatory Serum Markers. Dig. Surg. 2017, 34, 507–517. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Dindo, D.; Demartines, N.; Clavien, P.A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef]
- De la Plaza Llamas, R.; Ramia Ángel, J.M.; Bellón, J.M.; Arteaga Peralta, V.; García Amador, C.; López Marcano, A.J.; Medina Velasco, A.A.; González Sierra, B.; Manuel Vázquez, A. Clinical Validation of the Comprehensive Complication Index as a Measure of Postoperative Morbidity at a Surgical Department: A Prospective Study. Ann. Surg. 2018, 268, 838–844. [Google Scholar] [CrossRef]
- Benedetti, M.; Ciano, P.; Pergolini, I.; Ciotti, S.; Guercioni, G.; Ruffo, G.; Borghi, F.; Patriti, A.; Del Rio, P.; Scatizzi, M.; et al. Early diagnosis of anastomotic leakage after colorectal surgery by the Dutch leakage score, serum procalcitonin and serum C-reactive protein: Study protocol of a prospective multicentre observational study by the Italian ColoRectal Anastomotic Leakage (iCral). G. Chir. 2019, 40, 20–25. [Google Scholar]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [Green Version]
- Richards, C.H.; Roxburgh, C.S. Surgical outcome in patients undergoing reversal of Hartmann’s procedures: A multicentre study. Colorectal Dis. 2015, 17, 242–249. [Google Scholar] [CrossRef]
- Roig, J.V.; Cantos, M.; Balciscueta, Z.; Uribe, N.; Espinosa, J.; Roselló, V.; García-Calvo, R.; Hernandis, J.; Landete, F.; Representing the Sociedad Valenciana de Cirugía Cooperative Group (SVCCG). Hartmann’s operation: How often is it reversed and at what cost? A multicentre study. Colorectal Dis. 2011, 13, e396–e402. [Google Scholar] [CrossRef]
- Kim, T.H.; Suh, Y.S.; Huh, Y.J.; Son, Y.G.; Park, J.H.; Yang, J.Y.; Kong, S.H.; Ahn, H.S.; Lee, H.J.; Slankamenac, K.; et al. The comprehensive complication index (CCI) is a more sensitive complication index than the conventional Clavien-Dindo classification in radical gastric cancer surgery. Gastric Cancer 2018, 21, 171–181. [Google Scholar] [CrossRef]
- Yamashita, S.; Sheth, R.A.; Niekamp, A.S.; Aloia, T.A.; Chun, Y.S.; Lee, J.E.; Vauthey, J.N.; Conrad, C. Comprehensive Complication Index Predicts Cancer-Specific Survival after Resection of Colorectal Metastases Independent of RAS Mutational Status. Ann. Surg. 2017, 266, 1045–1054. [Google Scholar] [CrossRef]
- Rajcoomar, M.S.; Kinoo, S.M.; Naidoo, R.; Sewkurren, N.; Singh, B. The Challenges of the Hartmann’s Rectal Stump Reversal: A Clinical Audit and Review of the Literature. Int. Surg. 2017, 102, 404–411. [Google Scholar] [CrossRef]
- Okabayashi, K.; Ashrafian, H.; Zacharakis, E.; Hasegawa, H.; Kitagawa, Y.; Athanasiou, T.; Darzi, A. Adhesions after abdominal surgery: A systematic review of the incidence, distribution and severity. Surg. Today 2014, 44, 405–420. [Google Scholar] [CrossRef]
- Keck, J.O.; Collopy, B.T.; Ryan, P.J.; Fink, R.; Mackay, J.R.; Woods, R.J. Reversal of Hartmann’s procedure: Effect of timing and technique on ease and safety. Dis. Colon Rectum 1994, 37, 243–248. [Google Scholar] [CrossRef] [PubMed]
- Fleming, F.J.; Gillen, P. Reversal of Hartmann’s procedure following acute diverticulitis: Is timing everything? Int. J. Colorectal Dis. 2009, 24, 1219–1225. [Google Scholar] [CrossRef] [PubMed]
- Resio, B.J.; Jean, R.; Chiu, A.S.; Pei, K.Y. Association of Timing of Colostomy Reversal with Outcomes following Hartmann Procedure for Diverticulitis. JAMA Surg. 2019, 154, 218–224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Montroni, I.; Rostoft, S.; Spinelli, A.; Van Leeuwen, B.L.; Ercolani, G.; Saur, N.M.; Jaklitsch, M.T.; Somasundar, P.S.; de Liguori Carino, N.; Ghignone, F.; et al. GOSAFE—Geriatric Oncology Surgical Assessment and Functional rEcovery after Surgery: Early analysis on 977 patients. J. Geriatr. Oncol. 2020, 11, 244–255. [Google Scholar] [CrossRef] [Green Version]
- Bosanquet, D.C.; Ansell, J.; Abdelrahman, T.; Cornish, J.; Harries, R.; Stimpson, A.; Davies, L.; Glasbey, J.C.; Frewer, K.A.; Frewer, N.C.; et al. Systematic Review and Meta-Regression of Factors Affecting Midline Incisional Hernia Rates: Analysis of 14,618 Patients. PLoS ONE 2015, 10, e0138745. [Google Scholar] [CrossRef] [Green Version]
- Akinci, M.; Ergul, Z.; Kantarcioglu, M.; Tapan, S.; Ozler, M.; Gunal, A.; Kulacoglu, H.; Ide, T.; Sayal, A.; Eryilmaz, M.; et al. The effect of relaparotomy timing on wound healing in an animal model. Int. J. Surg. 2014, 12, 1434–1438. [Google Scholar] [CrossRef] [Green Version]
- Maatouk, M.; Ben Safta, Y.; Mabrouk, A.; Kbir, G.H.; Dhaou, A.B.; Daldoul, S.; Sayari, S.; Haouet, K.; Dziri, C.; Ben Moussa, M. Surgical site infection in mesh repair for ventral hernia in contaminated field: A systematic review and meta-analysis: Mesh repair for Ventral Hernia in contaminated field. Ann. Med. Surg. 2021, 63, 102173. [Google Scholar] [CrossRef]
- Birolini, C.; de Miranda, J.S.; Tanaka, E.Y.; Utiyama, E.M.; Rasslan, S.; Birolini, D. The use of synthetic mesh in contaminated and infected abdominal wall repairs: Challenging the dogma—A long-term prospective clinical trial. Hernia 2020, 24, 307–323. [Google Scholar] [CrossRef]
- Borab, Z.M.; Shakir, S.; Lanni, M.A.; Tecce, M.G.; MacDonald, J.; Hope, W.W.; Fischer, J.P. Does prophylactic mesh placement in elective, midline laparotomy reduce the incidence of incisional hernia? A systematic review and meta-analysis. Surgery 2017, 161, 1149–1163. [Google Scholar] [CrossRef] [Green Version]
- Payne, R.; Aldwinckle, J.; Ward, S. Meta-analysis of randomised trials comparing the use of prophylactic mesh to standard midline closure in the reduction of incisional herniae. Hernia 2017, 21, 843–853. [Google Scholar] [CrossRef]
- El-Khadrawy, O.H.; Moussa, G.; Mansour, O.; Hashish, M.S. Prophylactic prosthetic reinforcement of midline abdominal incisions in high-risk patients. Hernia 2009, 13, 267–274. [Google Scholar] [CrossRef]
- Kurmann, A.; Barnetta, C.; Candinas, D.; Beldi, G. Implantation of prophylactic non-absorbable intraperitoneal mesh in patients with peritonitis is safe and feasible. World J. Surg. 2013, 37, 1656–1660. [Google Scholar] [CrossRef] [Green Version]
- García-Ureña, M.Á.; López-Monclús, J.; Hernando, L.A.; Montes, D.M.; Valle de Lersundi, A.R.; Pavón, C.C.; Ceinos, C.J.; Quindós, P.L. Randomized controlled trial of the use of a large-pore polypropylene mesh to prevent incisional hernia in colorectal surgery. Ann. Surg. 2015, 261, 876–881. [Google Scholar] [CrossRef] [Green Version]
- Guerra, F.; Coletta, D.; Del Basso, C.; Giuliani, G.; Patriti, A. Conventional Versus Minimally Invasive Hartmann Takedown: A Meta-Analysis of the Literature. World J. Surg. 2019, 43, 1820–1828. [Google Scholar] [CrossRef]
- Van de Wall, B.J.; Draaisma, W.A.; Schouten, E.S.; Broeders, I.A.; Consten, E.C. Conventional and laparoscopic reversal of the Hartmann procedure: A review of the literature. J. Gastrointest. Surg. 2010, 14, 743–752. [Google Scholar] [CrossRef] [Green Version]
- Siddiqui, M.R.; Sajid, M.S.; Baig, M.K. Open vs. laparoscopic approach for reversal of Hartmann’s procedure: A systematic review. Colorectal Dis. 2010, 12, 733–741. [Google Scholar] [CrossRef]

| Diagnosis | Patients, n (%) |
|---|---|
| Benign disease | 77 (78.1) |
| Complicated diverticulitis | 55 (52.4) |
| Ischemic colitis | 9 (8.57) |
| Volvulus | 5 (4.76) |
| Adhesion | 5 (4.76) |
| Iatrogenic perforation | 5 (4.76) |
| Road traffic accident | 3 (2.86) |
| Cancer | 23 (21.9) |
| Obstruction | 18 (17.14) |
| Perforation | 5 (4.76) |
| Clavien–Dindo Grade | n | n | |
|---|---|---|---|
| I | 48 | Fever | 36 |
| Ileus | 24 | ||
| Surgical site infection | 10 | ||
| Diarrhea syndrome | 4 | ||
| II | 33 | Pneumonia | 10 |
| Prolonged parenteral nutrition | 10 | ||
| Post-operative anemia treated with transfusion | 5 | ||
| Prolonged post-operative pain | 4 | ||
| Heart failure | 3 | ||
| Coagulopathy treated with plasma transfusion | 3 | ||
| Urinary infection | 1 | ||
| Atrial fibrillation | 1 | ||
| Adverse drug reaction | 1 | ||
| Deep surgical site infection | 1 | ||
| III | 7 | Anastomotic leakage | 7 |
| IV | 3 | Heart failure requiring intensive care unit | 3 |
| Comprehensive Complication Index (CCI) | |||||
|---|---|---|---|---|---|
| Total n = 105 | CCI ≤ 12.2 n = 68 (64.76%) | CCI > 12.2 n = 37 (35.24%) | p-Value | ||
| Age, median (IQR) | 69 (58–78) | 73 (58–78) | 67 (53–76) | 0.354 * | |
| Sex, n (%) | 0.002 ** | ||||
| Male | 61 (58.10) | 47 (69.12) | 14 (37.84) | ||
| Female | 44 (41.90) | 21 (30.88) | 23 (62.16) | ||
| BMI, median (IQR) | 24.47 (22.20–26.65) | 24.51 (22.33–26.72) | 24.14 (21.81–26.31) | 0.620 * | |
| ASA Score, n (%) | 0.817 ** | ||||
| I/II | 64 (60.95) | 42 (61.76) | 22 (59.46) | ||
| III | 41 (39.05) | 26 (38.24) | 15 (40.54) | ||
| CI, n (%) | 0.473 *** | ||||
| 0 | 68 (64.76) | 47 (69.12) | 21 (56.76) | ||
| 1 | 28 (26.67) | 16 (23.53) | 12 (32.43) | ||
| ≥2 | 9 (8.57) | 5 (7.35) | 4 (10.81) | ||
| Previous cancer history, n (%) | 0.349 ** | ||||
| No | 82 (78.10) | 55 (80.88) | 27 (72.97) | ||
| Yes | 23 (21.90) | 13 (19.12) | 10 (27.03) | ||
| Days between HP and HR, median (IQR) | 152 (62–250) | 119 (60–201) | 196 (92–282) | 0.005 * | |
| Operating time (min), median (IQR) | 185 (135–235) | 165 (125–223) | 200 (170–250) | 0.005 * | |
| Hospital stay (days), median (IQR) | 8 (8–10) | 8 (7–10) | 10 (8–13) | 0.002 * | |
| OR ° | 95% CI | p-Value | |
|---|---|---|---|
| Sex | |||
| Male a | 1 | ||
| Female | 4.65 | 1.80–12.03 | 0.001 |
| Days between HP and HR | 1.01 | 1.00–1.01 | 0.042 |
| Operating time | 1.01 | 1.00–1.02 | 0.034 |
| Hospital stay | 1.17 | 0.99–1.38 | 0.053 |
| Incisional Ventral Hernia | ||||
|---|---|---|---|---|
| Total n = 98 | No n = 63 (64.29%) | Yes n = 35 (35.71%) | p-Value | |
| Age, median (IQR) | 69 (58–78) | 69 (58–78) | 69 (56–76) | 0.789 * |
| Sex, n (%) | 1.000 ** | |||
| Male | 56 (57.14) | 36 (57.14) | 20 (57.14) | |
| Female | 42 (42.86) | 27 (42.86) | 15 (42.86) | |
| BMI, median (IQR) | 24.51 (22.20–26.65) | 22.94 (21.53–26.08) | 25.65 (24.14–26.79) | 0.004 * |
| ASA, n (%) | 0.689 ** | |||
| I/II | 59 (60.20) | 37 (58.73) | 22 (62.86) | |
| III | 39 (39.80) | 26 (41.27) | 13 (37.14) | |
| CI, n (%) | 0.850 *** | |||
| 0 | 63 (64.29) | 39 (61.90) | 24 (68.57) | |
| 1 | 26 (26.53) | 18 (28.57) | 8 (22.86) | |
| ≥2 | 9 (9.18) | 6 (9.52) | 3 (8.57) | |
| Previous cancer history, n (%) | 0.942 ** | |||
| No | 76 (77.55) | 49 (77.78) | 27 (77.14) | |
| Yes | 22 (22.45) | 14 (22.22) | 8 (22.86) | |
| Days between HP and HR, median (IQR) | 152 (62–252) | 174 (65–270) | 92 (59–176) | 0.009 * |
| Complications, n (%) | 0.164 ** | |||
| CCI ≤ 12.2 | 64 (65.31) | 38 (60.32) | 26 (74.29) | |
| CCI > 12.2 | 34 (34.69) | 25 (39.68) | 9 (25.71) | |
| Operating time, median (IQR) | 180 (135–230) | 190 (150–240) | 160 (125–210) | 0.033 * |
| Hospital stay, median (IQR) | 8 (7–10) | 8 (8–10) | 8 (7–10) | 0.952 * |
| OR ° | 95% CI | p-Value | |
|---|---|---|---|
| BMI | 1.27 | 1.10–1.47 | 0.001 |
| Days between HP and HR | 0.99 | 0.99–0.99 | 0.006 |
| Operating time | 0.99 | 0.99–1.00 | 0.131 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Clementi, M.; Pietroletti, R.; Carletti, F.; Sista, F.; Grasso, A.; Fiasca, F.; Cappelli, S.; Balla, A.; Rizza, V.; Ciarrocchi, A.; et al. Colostomy Reversal following Hartmann’s Procedure: The Importance of Timing in Short- and Long-Term Complications: A Retrospective Multicentric Study. J. Clin. Med. 2022, 11, 4388. https://doi.org/10.3390/jcm11154388
Clementi M, Pietroletti R, Carletti F, Sista F, Grasso A, Fiasca F, Cappelli S, Balla A, Rizza V, Ciarrocchi A, et al. Colostomy Reversal following Hartmann’s Procedure: The Importance of Timing in Short- and Long-Term Complications: A Retrospective Multicentric Study. Journal of Clinical Medicine. 2022; 11(15):4388. https://doi.org/10.3390/jcm11154388
Chicago/Turabian StyleClementi, Marco, Renato Pietroletti, Filippo Carletti, Federico Sista, Antonella Grasso, Fabiana Fiasca, Sonia Cappelli, Andrea Balla, Vinicio Rizza, Andrea Ciarrocchi, and et al. 2022. "Colostomy Reversal following Hartmann’s Procedure: The Importance of Timing in Short- and Long-Term Complications: A Retrospective Multicentric Study" Journal of Clinical Medicine 11, no. 15: 4388. https://doi.org/10.3390/jcm11154388
APA StyleClementi, M., Pietroletti, R., Carletti, F., Sista, F., Grasso, A., Fiasca, F., Cappelli, S., Balla, A., Rizza, V., Ciarrocchi, A., & Guadagni, S. (2022). Colostomy Reversal following Hartmann’s Procedure: The Importance of Timing in Short- and Long-Term Complications: A Retrospective Multicentric Study. Journal of Clinical Medicine, 11(15), 4388. https://doi.org/10.3390/jcm11154388







