Role of Iron and Iron Overload in the Pathogenesis of Invasive Fungal Infections in Patients with Hematological Malignancies
Abstract
:1. Invasive Fungal Infections in Hematology
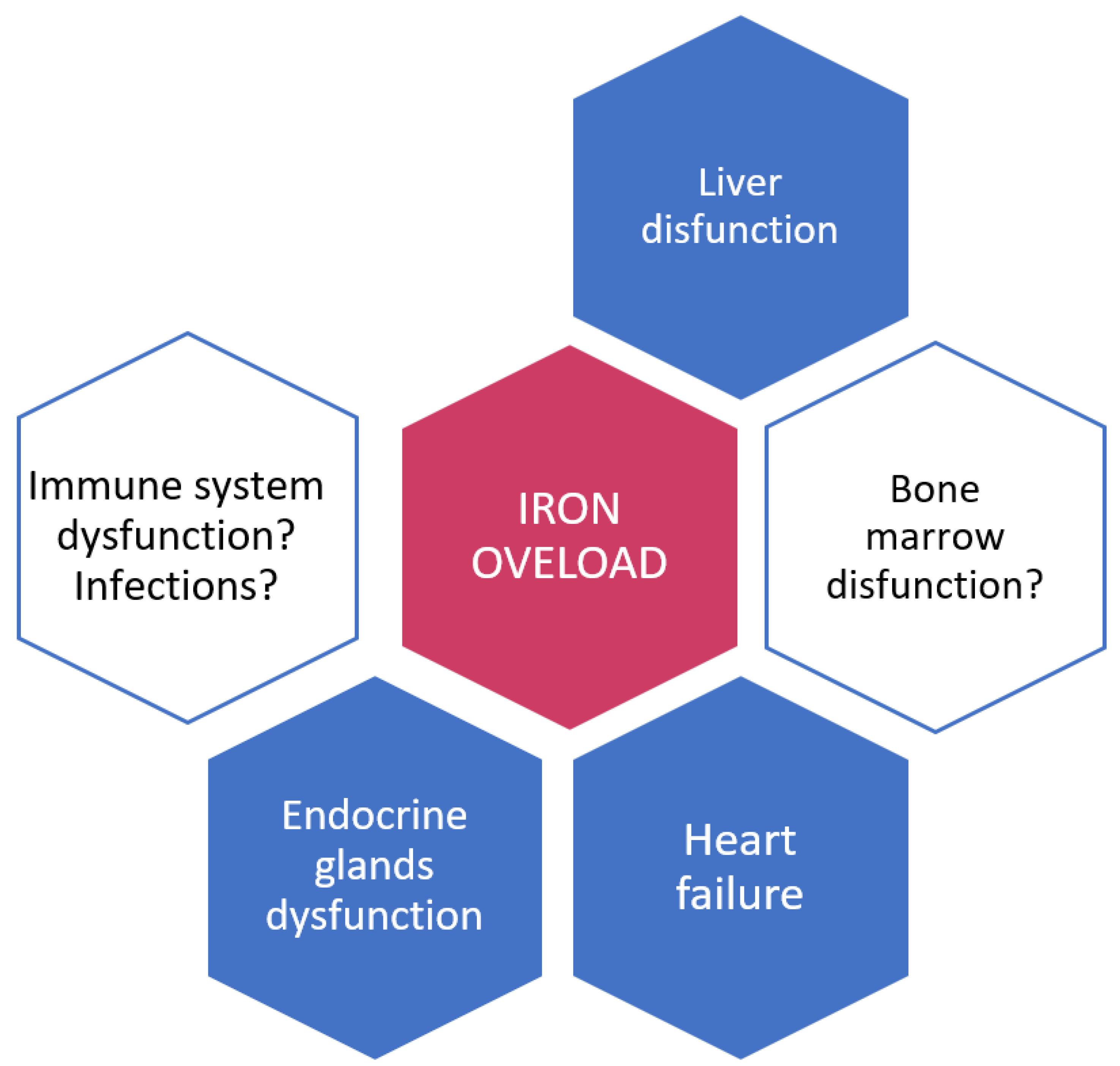
2. Iron and Iron Overload: Their Role in Infections
3. Mechanisms of Iron Acquisition by Fungal Pathogens
3.1. Reduction of Ferric to Ferrous Iron with Subsequent Transport
3.2. Siderophore Production and Transport
3.3. Iron Acquisition from Host’s Iron-Containing Proteins Such as Hemoglobin and Other Proteins
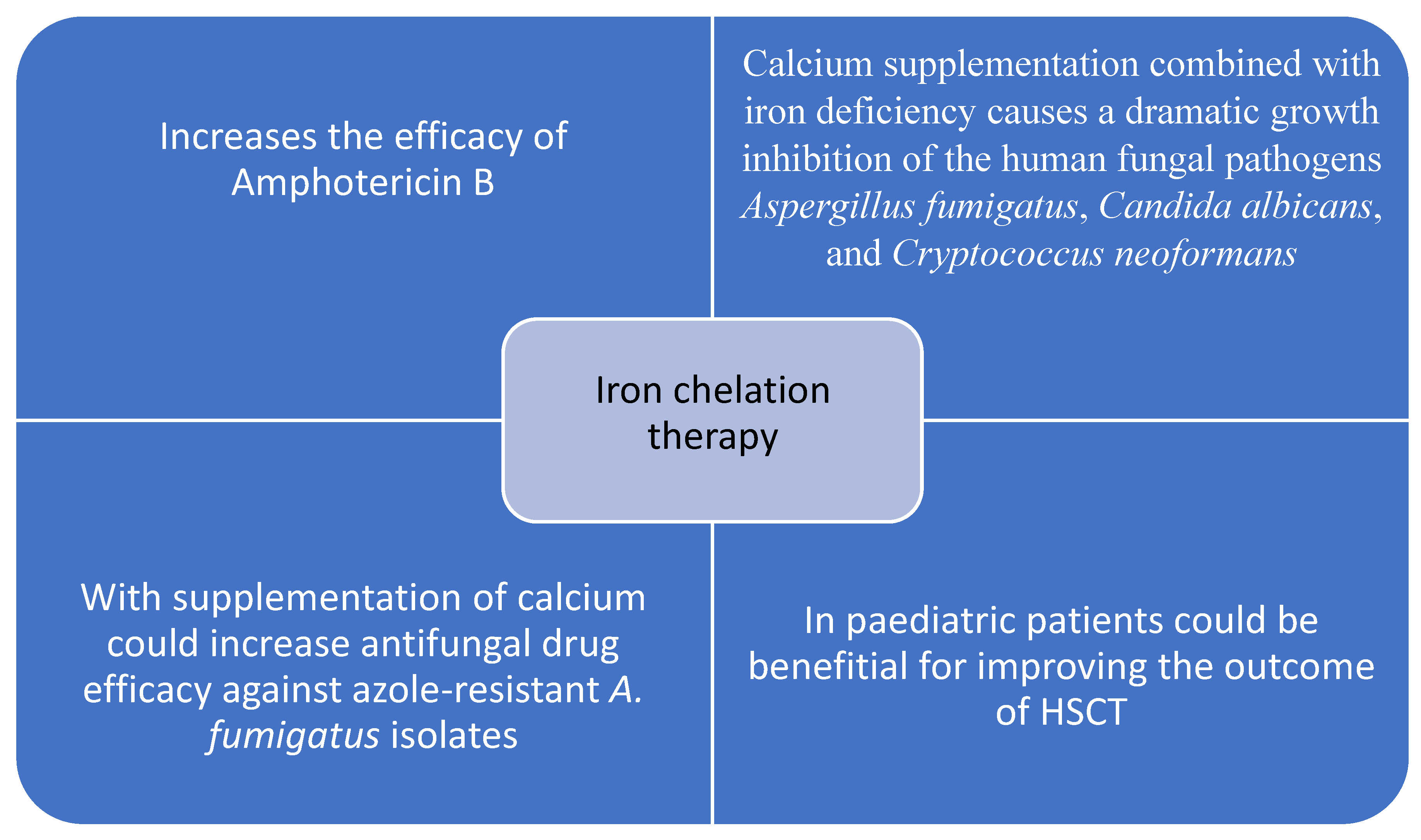
4. Iron Overload, Iron Chelation Therapy and Invasive Fungal Infections in Hematology
5. Future Perspectives and Possible Therapeutic Application
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ninin, E.; Milpied, N.; Moreau, P.; André-Richet, B.; Morineau, N.; Mahé, B.; Vigier, M.; Imbert, B.; Morin, O.; Harousseau, J.; et al. Longitudinal study of bacterial, viral, and fungal infections in adult recipients of bone marrow transplants. Clin. Infect. Dis. 2001, 33, 41–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pagano, L.; Caira, M.; Nosari, A.; Van Lint, M.T.; Candoni, A.; Offidani, M.; Aloisi, T.; Irrera, G.; Bonini, A.; Picardi, M.; et al. Fungal infections in recipients of hematopoietic stem cell transplants: Results of the SEIFEM B-2004 study-Sorveglianza Epidemiologica Infezioni Fungine Nelle Emopatie Maligne. Clin. Infect. Dis. 2007, 45, 1161–1170. [Google Scholar] [CrossRef] [PubMed]
- Cornely, O.A.; Maertens, J.; Winston, D.J.; Perfect, J.; Ullmann, A.J.; Walsh, T.J.; Helfgott, D.; Holowiecki, J.; Stockelberg, D.; Goh, Y.T.; et al. Posaconazole vs fluconazole or intraconazole prophylaxis in patients with neutropenia. N. Engl. J. Med. 2007, 356, 348–359. [Google Scholar] [CrossRef] [Green Version]
- Egerer, G.; Geist, M.J. Posaconazole prophylaxis in patients with acute myelogenous leukemia—Results from an observational study. Mycoses 2011, 54 (Suppl. 1), 7–11. [Google Scholar] [CrossRef]
- Orasch, C.; Weisser, M.; Mertz, D.; Conen, A.; Heim, D.; Christen, S.; Gratwohl, A.; Battegay, M.; Widmer, A.F.; Fluckiger, U. Comparison of infectious complications during induction/consolidation chemotherapy versus allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant. 2010, 45, 521–526. [Google Scholar] [CrossRef]
- Jenks, J.D.; Cornely, O.A.; Chen, S.C.; Thompson, G.R., 3rd; Hoenigl, M. Breakthrough invasive fungal infections: Who is at risk? Mycoses 2020, 63, 1021–1032. [Google Scholar] [CrossRef] [PubMed]
- Aldoss, I.; Dadwal, S.; Zhang, J.; Tegtmeier, B.; Mei, M.; Arslan, S.; Al Malki, M.M.; Salhotra, A.; Ali, H.; Aribi, A.; et al. Invasive fungal infections in acute myeloid leukemia treated with venetoclax and hypomethylating agents. Blood Adv. 2019, 3, 4043–4049. [Google Scholar] [CrossRef] [Green Version]
- Infante, M.S.; Fernández-Cruz, A.; Núñez, L.; Carpio, C.; Jiménez-Ubieto, A.; López-Jiménez, J.; Vásquez, L.; Del Campo, R.; Romero, S.; Alonso, C.; et al. Grupo Español de Linfomas y Trasplante Autólogo de Medula Ósea (GELTAMO). Severe infections in patients with lymphoproliferative diseases treated with new targeted drugs: A multicentric real-world study. Cancer Med. 2021, 10, 7629–7640. [Google Scholar] [CrossRef]
- Chamilos, G.; Lionakis, M.S.; Kontoyiannis, D.P. Call for action: Invasive fungal infections associated with ibrutinib and other small molecule kinase inhibitors targeting immune signaling pathways. Clin. Infect. Dis. 2018, 66, 140–148. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Little, J.S.; Weiss, Z.F.; Hammond, S.P. Invasive Fungal Infections and Targeted Therapies in Hematological Malignancies. J. Fungi 2021, 7, 1058. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.R.; Byrd, J.C.; Coutre, S.E.; Benson, D.M.; Flinn, I.; Wagner-Johnston, N.D.; Spurgeon, S.E.; Kahl, B.S.; Bello, C.; Webb, H.K.; et al. Idelalisib, an inhibitor of phosphatidylinositol 3-kinase p110δ, for relapsed/refractory chronic lymphocytic leukemia. Blood 2014, 123, 3390–3397. [Google Scholar] [CrossRef] [PubMed]
- Maertens, J.A.; Girmenia, C.; Brüggemann, R.J.; Duarte, R.F.; Kibbler, C.C.; Ljungman, P.; Racil, Z.; Ribaud, P.; Slavin, M.; Cornely, O.A.; et al. European Conference on Infections in Leukaemia (ECIL), a joint venture of the European Group for Blood and Marrow Transplantation (EBMT), the European Organization for Research and Treatment of Cancer (EORTC), the Immunocompromised Host Society (ICHS) and the European LeukemiaNet (ELN). European guidelines for primary antifungal prophylaxis in adult haematology patients: Summary of the updated recommendations from the European Conference on Infections in Leukaemia. J. Antimicrob. Chemother. 2018, 73, 3221–3230. [Google Scholar] [CrossRef] [PubMed]
- Chamilos, G.; Lewis, R.E.; Kontoyiannis, D.P. Delaying amphotericin B-based frontline therapy significantly increases mortality among patients with hematologic malignancy who have zygomycosis. Clin. Infect. Dis. 2008, 47, 503–509. [Google Scholar] [CrossRef] [PubMed]
- Torti, F.M.; Torti, S.V. Regulation of ferritin genes and protein. Blood 2002, 99, 3505–3516. [Google Scholar] [CrossRef] [Green Version]
- Senjo, H.; Higuchi, T.; Okada, S.; Takahashi, O. Hyperferritinemia: Causes and significance in a general hospital. Hematology 2018, 23, 817–822. [Google Scholar] [CrossRef] [Green Version]
- Ganz, T. Iron and infection. Int. J. Hematol. 2018, 107, 7–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gattermann, N. Iron overload in myelodysplastic syndromes (MDS). Int. J. Hematol. 2018, 107, 55–63. [Google Scholar] [CrossRef] [Green Version]
- Shah, F.T.; Porter, J.B.; Sadasivam, N.; Kaya, B.; Moon, J.C.; Velangi, M.; Ako, E.; Pancham, S. Guidelines for the monitoring and management of iron overload in patients with haemoglobinopathies and rare anaemias. Br. J. Haematol. 2022, 196, 336–350. [Google Scholar] [CrossRef]
- Oliva, E.N.; Huey, K.; Deshpande, S.; Turner, M.; Chitnis, M.; Schiller, E.; Tang, D.; Yucel, A.; Hughes, C.; Shah, F. A Systematic Literature Review of the Relationship between Serum Ferritin and Outcomes in Myelodysplastic Syndromes. J. Clin. Med. 2022, 11, 895. [Google Scholar] [CrossRef] [PubMed]
- Malcovati, L.; Della Porta, M.G.; Cazzola, M. Predicting survival and leukemic evolution in patients with myelodysplastic syndrome. Haematologica 2006, 91, 1588–1590. [Google Scholar]
- Weber, S.; Parmon, A.; Kurrle, N.; Schnütgen, F.; Serve, H. The Clinical Significance of Iron Overload and Iron Metabolism in Myelodysplastic Syndrome and Acute Myeloid Leukemia. Front. Immunol. 2021, 11, 627662. [Google Scholar] [CrossRef] [PubMed]
- Cadet, J.; Wagner, J.R. DNA base damage by reactive oxygen species, oxidizing agents, and UV radiation. Cold Spring Harbor Perspect. Biol. 2013, 5, a012559. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Sapena, R.; Kelaidi, C.; Vassilieff, D.; Bordessoule, D.; Stamatoullas, A.; Cheze, S.; Beyne-Rauzy, O.; Vey, N.; Rose, C.; et al. Ferritin level at diagnosis is not correlated with poorer survival in non RBC transfusion dependent lower risk de novo MDS. Leuk. Res. 2011, 35, 1530–1533. [Google Scholar] [CrossRef] [PubMed]
- Waszczuk-Gajda, A.; Madry, K.; Machowicz, R.; Drozd-Sokołowska, J.; Stella-Hołowiecka, B.; Mital, A.; Obara, A.; Szmigielska-Kapłon, A.; Sikorska, A.; Subocz, E.; et al. Red blood cell transfusion dependency and hyperferritinemia are associated with impaired survival in patients diagnosed with myelodysplastic syndromes: Results from the first Polish MDS-PALG Registry. Adv. Clin. Exp. Med. 2016, 25, 633–641. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuo, C.H.; Dai, Z.K.; Wu, J.R.; Hsieh, T.-J.; Hung, C.-H.; Hsu, J.-H. Septic arthritis as the initial manifestation of fatal Vibrio vulnificus septicemia in a patient with thalassemia and iron overload. Pediatric Blood Cancer 2009, 53, 1156–1158. [Google Scholar] [CrossRef] [PubMed]
- Barton, J.C.; Acton, R.T. Hemochromatosis and Vibrio vulnificus wound infections. J. Clin. Gastroenterol. 2009, 43, 890–893. [Google Scholar] [CrossRef]
- Bergmann, T.K.; Vinding, K.; Hey, H. Multiple hepatic abscesses due to Yersinia enterocolitica infection secondary to primary haemochromatosis. Scand. J. Gastroenterol. 2001, 36, 891–895. [Google Scholar] [CrossRef]
- Portugal, S.; Carret, C.; Recker, M.; Armitage, A.; Gonçalves, L.A.; Epiphanio, S.; Sullivan, D.; Roy, C.; Newbold, C.; Drakesmith, A.; et al. Host-mediated regulation of superinfection in malaria. Nat. Med. 2011, 17, 732–737. [Google Scholar] [CrossRef]
- Soofi, S.; Cousens, S.; Iqbal, S.P.; Akhund, T.; Khan, J.; Ahmed, I.; Zaidi, A.K.; Bhutta, Z.A. Effect of provision of daily zinc and iron with several micronutrients on growth and morbidity among young children in Pakistan: A cluster-randomised trial. Lancet 2013, 82, 29–40. [Google Scholar] [CrossRef]
- Sazawal, S.; Black, R.E.; Ramsan, M.; Chwaya, H.M.; Stoltzfus, R.J.; Dutta, A.; Dhingra, U.; Kabole, I.; Deb, S.; Othman, M.K.; et al. Effects of routine prophylactic supplementation with iron and folic acid on admission to hospital and mortality in preschool children in a high malaria transmission setting: Community-based, randomised, placebo-controlled trial. Lancet 2006, 67, 133–143. [Google Scholar] [CrossRef]
- Macdougall, I.C.; Bircher, A.J.; Eckardt, K.U.; Obrador, G.T.; Pollock, C.A.; Stenvinkel, P.; Swinkels, D.W.; Wanner, C.; Weiss, G.; Chertow, G.M.; et al. Iron management in chronic kidney disease: Conclusions from a Kidney Disease: Improving Global Outcomes’ (KDIGO) controversies conference. Kidney Int. 2016, 89, 28–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fernández-Ruiz, M.; Parra, P.; Ruiz-Merlo, T.; López-Medrano, F.; Juan, R.S.; Polanco, N.; González, E.; Andrés, A.; Aguado, J.M. Association between baseline serum hepcidin levels and infection in kidney transplant recipients: Potential role for iron overload. Transpl. Infect. Dis. 2018, 20, e12807. [Google Scholar] [CrossRef] [PubMed]
- Chow, J.K.L.; Ganz, T.; Ruthazer, R.; Simpson, M.A.; Pomfret, E.A.; Gordon, F.D.; Westerman, M.E.; Snydman, D. Iron-related markers are associated with infection after liver transplantation. Liver Transpl. 2017, 23, 1541–1552. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tachibana, T.; Tanaka, M.; Takasaki, H.; Numata, A.; Ito, S.; Watanabe, R.; Hyo, R.; Ohshima, R.; Hagihara, M.; Sakai, R.; et al. Pretransplant serum ferritin levels are associated with bloodstream infections within 100 days of allogeneic stem cell transplantation for myeloid malignancies. Int. J. Hematol. 2011, 93, 368–374. [Google Scholar] [CrossRef] [PubMed]
- Kanda, J.; Mizumoto, C.; Ichinohe, T.; Kawabata, H.; Saito, T.; Yamashita, K.; Kondo, T.; Takakura, S.; Ichiyama, S.; Uchiyama, T.; et al. Pretransplant serum ferritin and C-reactive protein as predictive factors for early bacterial infection after allogeneic hematopoietic cell transplantation. Bone Marrow Transplant. 2011, 46, 208–216. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miceli, M.H.; Dong, L.; Grazziutti, M.L.; Fassas, A.; Thertulien, R.; Van Rhee, F.; Barlogie, B.; Anaissie, E.J. Iron overload is a major risk factor for severe infection after autologous stem cell transplantation: A study of 367 myeloma patients. Bone Marrow Transplant. 2006, 37, 857–864. [Google Scholar] [CrossRef]
- Valkovic, T.; Gacic, V.; Nacinovic-Duletic, A. Multiple Myeloma Index for Risk of Infections. J. Cancer 2018, 9, 2211–2214. [Google Scholar]
- Caza, M.; Kronstad, J.W. Shared and distinct mechanisms of iron acquisition by bacterial and fungal pathogens of humans. Front. Cell Infect. Microbiol. 2013, 3, 80. [Google Scholar] [CrossRef]
- Bairwa, G.; Hee Jung, W.; Kronstad, J.W. Iron acquisition in fungal pathogens of humans. Metallomics 2017, 9, 215–227. [Google Scholar] [CrossRef] [Green Version]
- Kosman, D.J. Molecular mechanisms of iron uptake in fungi. Mol. Microbiol. 2003, 47, 1185–1197. [Google Scholar] [CrossRef]
- Morrissey, J.A.; Williams, P.H.; Cashmore, A.M. Candida albicans has a cell-associated ferric-reductase activity which is regulated in response to levels of iron and copper. Microbiology 1996, 142 Pt 3, 485–492. [Google Scholar] [CrossRef] [Green Version]
- Knight, S.A.; Lesuisse, E.; Stearman, R.; Klausner, R.D.; Dancis, A. Reductive iron uptake by Candida albicans: Role of copper, iron and the TUP1 regulator. Microbiology 2002, 148, 29–40. [Google Scholar] [CrossRef] [Green Version]
- Knight, S.A.; Vilaire, G.; Lesuisse, E.; Dancis, A. Iron acquisition from transferrin by Candida albicans depends on the reductive pathway. Infect. Immun. 2005, 73, 5482–5492. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramanan, N.; Wang, Y. A high-affinity iron permease essential for Candida albicans virulence. Science 2000, 288, 1062–1064. [Google Scholar] [CrossRef]
- Jeeves, R.E.; Mason, R.P.; Woodacre, A.; Cashmore, A.M. Ferric reductase genes involved in high-affinity iron uptake are differentially regulated in yeast and hyphae of Candida albicans. Yeast 2011, 28, 629–644. [Google Scholar] [CrossRef]
- Blatzer, M.; Binder, U.; Haas, H. The metalloreductase FreB is involved in adaptation of Aspergillus fumigatus to iron starvation. Fungal Genet. Biol. 2011, 48, 1027–1033. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andrews, S.C.; Robinson, A.K.; Rodríguez-Quiñones, F. Bacterial iron homeostasis. FEMS Microbiol. Rev. 2003, 27, 215–237. [Google Scholar] [CrossRef]
- Miethke, M.; Marahiel, M.A. Siderophore-based iron acquisition and pathogen control. Microbiol. Mol. Biol. Rev. 2007, 71, 413–451. [Google Scholar] [CrossRef] [Green Version]
- Winkelmann, G. Ecology of siderophores with special reference to the fungi. Biometals 2007, 20, 379–392. [Google Scholar] [CrossRef] [PubMed]
- Haas, H.; Eisendle, M.; Turgeon, B.G. Siderophores in fungal physiology and virulence. Annu. Rev. Phytopathol. 2008, 46, 149–187. [Google Scholar] [CrossRef]
- Schrettl, M.; Bignell, E.; Kragl, C.; Joechl, C.; Rogers, T.; Arst, H.N., Jr.; Haynes, K.; Haas, H. Siderophore biosynthesis but not reductive iron assimilation is essential for Aspergillus fumigatus virulence. J. Exp. Med. 2004, 200, 1213–1219. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hissen, A.H.; Wan, A.N.; Warwas, M.L.; Pinto, L.J.; Moore, M.M. The Aspergillus fumigatus siderophore bio-synthetic gene sidA, encoding L-ornithine N5-oxygenase, is required for virulence. Infect. Immun. 2005, 73, 5493–5503. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Howard, D.H.; Rafie, R.; Tiwari, A.; Faull, K.F. Hydroxamate siderophores of Histoplasma capsulatum. Infect. Immun. 2000, 68, 2338–2343. [Google Scholar] [CrossRef] [Green Version]
- Schrettl, M.; Haas, H. Iron homeostasis–Achilles’ heel of Aspergillus fumigatus? Curr. Opin. Microbiol. 2011, 14, 400–405. [Google Scholar] [CrossRef] [Green Version]
- Haas, H. Molecular genetics of fungal siderophore biosynthesis and uptake: The role of siderophores in iron uptake and storage. Appl. Microbiol. Biotechnol. 2003, 62, 316–330. [Google Scholar] [CrossRef] [PubMed]
- Philpott, C.C. Iron uptake in fungi: A system for every source. Biochim. Biophys. Acta 2006, 1763, 636–645. [Google Scholar] [CrossRef] [Green Version]
- Lesuisse, E.; Blaiseau, P.L.; Dancis, A.; Camadro, J.M. Siderophore uptake and use by the yeast Saccharomyces Cerevisiae. Microbiology 2001, 147, 289–298. [Google Scholar] [CrossRef] [Green Version]
- Pao, S.S.; Paulsen, I.T.; Saier, M.H. Major, Facilitator Superfamily. Microbiol. Mol. Biol. Rev. 1998, 62, 1–34. [Google Scholar] [CrossRef] [Green Version]
- Philpott, C.C.; Protchenko, O. Response to iron deprivation in Saccharomyces cerevisiae. Eukaryot. Cell 2008, 7, 20–27. [Google Scholar] [CrossRef] [Green Version]
- Yun, C.W.; Tiedeman, J.S.; Moore, R.E.; Philpott, C.C. Siderophore-iron uptake in Saccharomyces cerevisiae. Identification of ferrichrome and fusarinine transporters. J. Biol. Chem. 2000, 275, 16354–16359. [Google Scholar] [CrossRef] [Green Version]
- Heymann, P.; Gerads, M.; Schaller, M.; Dromer, F.; Winkelmann, G.; Ernst, J.F. The siderophore iron transporter of Candida albicans (Sit1p/Arn1p) mediates uptake of ferrichrome-type siderophores and is required for epithelial invasion. Infect. Immun. 2002, 70, 5246–5255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nairz, M.; Schroll, A.; Sonnweber, T.; Weiss, G. The struggle for iron—A metal at the host-pathogen interface. Cell Microbiol. 2010, 12, 1691–1702. [Google Scholar] [CrossRef] [PubMed]
- Cassat, J.E.; Skaar, E.P. Iron in infection and immunity. Cell Host Microbe 2013, 13, 509–519. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weissman, Z.; Shemer, R.; Kornitzer, D. Deletion of the copper transporter CaCCC2 reveals two distinct pathways for iron acquisition in Candida albicans. Mol. Microbiol. 2002, 44, 1551–1560. [Google Scholar] [CrossRef]
- Santos, R.; Buisson, N.; Knight, S.; Dancis, A.; Camadro, J.M.; Lesuisse, E. Haemin uptake and use as an iron source by Candida albicans: Role of CaHMX1-encoded haem oxygenase. Microbiology 2003, 149, 579–588. [Google Scholar] [CrossRef]
- Weissman, Z.; Kornitzer, D. A family of Candida cell surface haem-binding proteins involved in haemin and haemoglobin-iron utilization. Mol. Microbiol. 2004, 53, 1209–1220. [Google Scholar] [CrossRef]
- Manns, J.M.; Mosser, D.M.; Buckley, H.R. Production of a hemolytic factor by Candida albicans. Infect. Immun. 1994, 62, 5154–5156. [Google Scholar] [CrossRef] [Green Version]
- Weissman, Z.; Shemer, R.; Conibear, E.; Kornitzer, D. An endocytic mechanism for haemoglobin-iron acquisition in Candida albicans. Mol. Microbiol. 2008, 69, 201–217. [Google Scholar] [CrossRef] [PubMed]
- Okamoto-Shibayama, K.; Kikuchi, Y.; Kokubu, E.; Sato, Y.; Ishihara, K. Csa2, a member of the Rbt5 protein family, is involved in the utilization of iron from human hemoglobin during Candida albicans hyphal growth. FEMS Yeast Res. 2014, 14, 674–677. [Google Scholar] [CrossRef] [Green Version]
- Braun, B.R.; Head, W.S.; Wang, M.X.; Johnson, A.D. Identification and characterization of TUP1-regulated genes in Candida albicans. Genetics 2000, 156, 31–44. [Google Scholar] [CrossRef]
- Perez, A.; Pedros, B.; Murgui, A.; Casanova, M.; Lopez-Ribot, J.L.; Martinez, J.P. Biofilm formation by Candida albicans mutants for genes coding fungal proteins exhibiting the eight-cysteine-containing CFEM domain. FEMS Yeast Res. 2006, 6, 1074–1084. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoo, J.; Lee, Y.S.; Song, C.Y.; Kim, B.S. Purification and characterization of a 43-kilodalton extracellular serine proteinase from Cryptococcus neoformans. J. Clin. Microbiol. 2004, 42, 722–726. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, G.; Caza, M.; Cadieux, B.; Chan, V.; Liu, V.; Kronstad, J. Cryptococcus neoformans requires the ESCRT protein Vps23 for iron acquisition from heme, for capsule formation, and for virulence. Infect. Immun. 2013, 81, 292–302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cadieux, B.; Lian, T.; Hu, G.; Wang, J.; Biondo, C.; Teti, G.; Liu, V.; Murphy, M.E.; Creagh, A.L.; Kronstad, J.W. The Mannoprotein Cig1 supports iron acquisition from heme and virulence in the pathogenic fungus Cryptococcus neoformans. J. Infect. Dis. 2013, 207, 1339–1347. [Google Scholar] [CrossRef] [Green Version]
- Almeida, R.S.; Brunke, S.; Albrecht, A.; Thewes, S.; Laue, M.; Edwards, J.E., Jr.; Filler, S.G.; Hube, B. The hyphal-associated adhesin and invasin Als3 of Candida albicans mediates iron acquisition from host ferritin. PLoS Pathog. 2008, 4, e1000217. [Google Scholar] [CrossRef]
- Karp, J.E.; Merz, W.G. Association of reduced total iron binding capacity and fungal infections in leukemic granulocytopenic patients. J. Clin. Oncol. 1986, 4, 216–220. [Google Scholar] [CrossRef]
- Altes, A.; Remacha, A.F.; Sarda, P.; Sancho, F.J.; Sureda, A.; Martino, R.; Briones, J.; Brunet, S.; Canals, C.; Sierra, J. Frequent severe liver iron overload after stem cell transplantation and its possible association with invasive aspergillosis. Bone Marrow Transplant. 2004, 34, 505–509. [Google Scholar] [CrossRef]
- Maertens, J.; Demuynck, H.; Verbeken, E.K.; Zachee, P.; Verhoef, G.; Vandenberghe, P.; Boogaerts, M.A. Mucormycosis in allogeneic bone marrow transplant recipients: Report of five cases and review of the role of iron overload in the pathogenesis. Bone Marrow Transplant. 1999, 24, 307–312. [Google Scholar] [CrossRef] [Green Version]
- Kontoyiannis, D.P.; Chamilos, G.; Lewis, R.E.; Giralt, S.; Cortes, J.; Raad, I.I.; Manning, J.T.; Han, X. Increasedbone marrow iron stores is an independent risk factor for invasive aspergillosis in patients with high risk hematologic malignancies patientsand recipients of allogeneic hematopoietic stem cell transplantation. Cancer 2007, 110, 1303–1306. [Google Scholar] [CrossRef]
- Alessandrino, E.P.; Della Porta, M.G.; Bacigalupo, A.; Malcovati, L.; Angelucci, E.; Van Lint, M.T.; Falda, M.; Onida, F.; Bernardi, M.; Guidi, S.; et al. Prognostic impact of pre-transplantation transfusion history and secondary iron overload in patients with myelodysplastic syndrome undergoing allogeneic stem cell transplantation: A GITMO study. Haematologica 2010, 95, 476–484. [Google Scholar] [CrossRef] [Green Version]
- Lai, Y.W.; Campbell, L.T.; Wilkins, M.R.; Pang, C.N.; Chen, S.; Carter, D.A. Synergy and antagonism between iron chelators and antifungal drugs in Cryptococcus. Int. J. Antimicrob. Agents 2016, 48, 388–394. [Google Scholar] [CrossRef] [PubMed]
- Chayakulkeeree, M.; Tangkoskul, T.; Waywa, D.; Tiengrim, S.; Pati, N.; Thamlikitkul, V. Impact of iron chelators on growth and expression of iron-related genes of Cryptococcus species. J. Mycol. Med. 2020, 30, 100905. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, A.S.; Gebermariam, T.; Fu, Y.; Lin, L.; Husseiny, M.I.; French, S.W.; Schwartz, J.; Skory, C.D.; Edwards, J.E.; Spellberg, B.J. The iron chelator deferasirox protects mice from mucormycosis through iron starvation. J. Clin. Investig. 2007, 117, 2649–2657. [Google Scholar] [CrossRef] [Green Version]
- Ibrahim, A.S.; Gebremariam, T.; French, S.W.; Edwards, J.E., Jr.; Spellberg, B. The iron chelator deferasirox enhances liposomal amphotericin B efficacy in treating murine invasive pulmonary aspergillosis. J. Antimicrob. Chemother. 2010, 65, 289–292. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ye, J.; Wang, Y.; Li, X.; Wan, Q.; Zhang, Y.; Lu, L. Synergistic Antifungal Effect of a Combination of Iron Deficiency and Calcium Supplementation. Microbiol. Spectr. 2022, 8, e0112122. [Google Scholar] [CrossRef]
- Lee, J.W.; Kang, H.J.; Kim, E.K.; Kim, H.; Shin, H.Y.; Ahn, H.S. Effect of iron overload and iron-chelating therapy on allogeneic hematopoietic SCT in children. Bone Marrow Transplant. 2009, 44, 793–797. [Google Scholar] [CrossRef]
- Carroll, C.S.; Amankwa, L.N.; Pinto, L.J.; Fuller, J.D.; Moore, M.M. Detection of a Serum Siderophore by LC-MS/ MS as a Potential Biomarker of Invasive Aspergillosis. PLoS ONE 2016, 11, e0151260. [Google Scholar] [CrossRef]
- Balhara, M.; Chaudhary, R.; Ruhil, S.; Singh, B.; Dahiya, N.; Parmar, V.S.; Jaiwal, P.K.; Chhillar, A.K. Siderophores; iron scavengers: The novel & promising targets for pathogen specific antifungal therapy. Expert Opin. Ther. Targets 2016, 20, 1477–1489. [Google Scholar]
- Wilson, B.R.; Bogdan, A.R.; Miyazawa, M.; Hashimoto, K.; Tsuji, Y. Siderophores in Iron Metabolism: From Mechanism to Therapy Potential. Trends Mol. Med. 2016, 22, 1077–1090. [Google Scholar] [CrossRef] [Green Version]
- Lamb, A.L. Breaking a pathogen’s iron will: Inhibiting siderophore production as an antimicrobial strategy. Biochim. Biophys. Acta 2015, 1854, 1054–1070. [Google Scholar] [CrossRef] [Green Version]
- Pinto, L.J.; Moore, M.M. Screening method to identify inhibitors of siderophore biosynthesis in the opportunistic fungal pathogen, Aspergillus fumigatus. Lett. Appl. Microbiol. 2009, 49, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Bernier, G.; Girijavallabhan, V.; Murray, A.; Niyaz, N.; Ding, P.; Miller, M.J.; Malouin, F. Desketoneoenactin-siderophore conjugates for Candida: Evidence of iron transport-dependent species selectivity. Antimicrob. Agents Chemother. 2005, 49, 241–248. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Cryptococcus neoformans | |
| Saccharomyces cerevisiae | |
| Candida albicans | |
| Aspergillus fumigatus |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Valković, T.; Damić, M.S. Role of Iron and Iron Overload in the Pathogenesis of Invasive Fungal Infections in Patients with Hematological Malignancies. J. Clin. Med. 2022, 11, 4457. https://doi.org/10.3390/jcm11154457
Valković T, Damić MS. Role of Iron and Iron Overload in the Pathogenesis of Invasive Fungal Infections in Patients with Hematological Malignancies. Journal of Clinical Medicine. 2022; 11(15):4457. https://doi.org/10.3390/jcm11154457
Chicago/Turabian StyleValković, Toni, and Marija Stanić Damić. 2022. "Role of Iron and Iron Overload in the Pathogenesis of Invasive Fungal Infections in Patients with Hematological Malignancies" Journal of Clinical Medicine 11, no. 15: 4457. https://doi.org/10.3390/jcm11154457






