The Relationship between Bone Conduction Hearing Threshold Shifts after Surgery for Chronic Otitis Media with Cholesteatoma According to STAM, EAONO/JOS, and SAMEO-ATO Classifications
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Audiometry
2.3. STAM, Stage of Cholesteatoma, EAONO/JOS and SAMEO-ATO Classifications
- S1 primary surgery, S2p planned 2nd surgery, S2r revision surgery.
- A1 endoscopic, A2 transcanal, A3 endaural, A4 retrouaricular approach.
- Mx no mastoidectomy, M1a canal wall preserved, M1b canal wall preserved and posterior tympanotomy, M2a only scutum removed, M2b scutum removed and posterosuperior canal wall removed, M2c whole canal removed, M3a subtotal petrosectomy with preservation of the otic capsule, M3b subtotal petrosectomy with removal of the otic capsula, including labyrinthectomy.
- E1 no reconstruction, E2 soft material reconstruction, E2 hard material reconstruction of external ear canal.
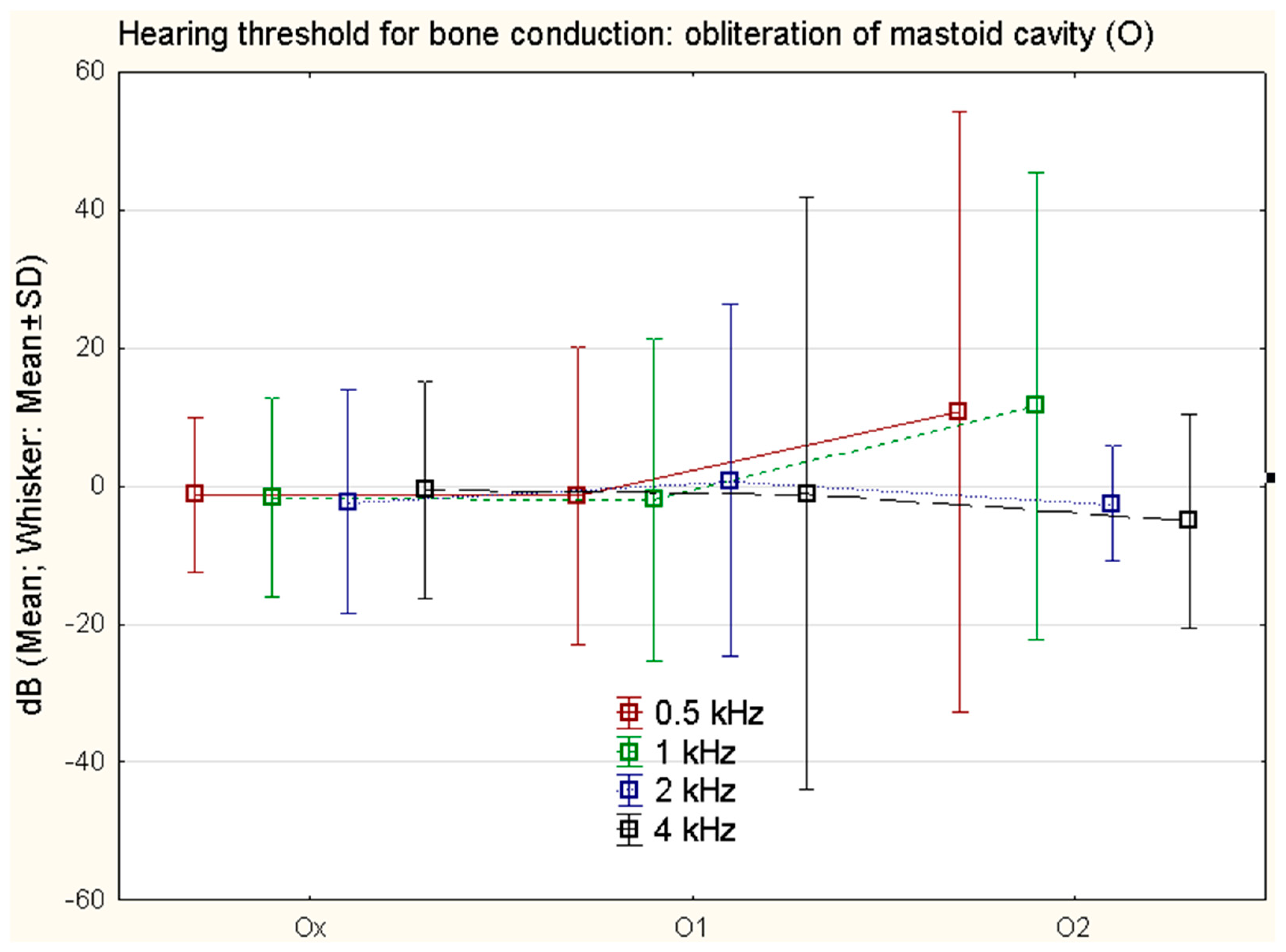
- Ox no reconstruction, O1 partial obliteration, O2 total obliteration of mastoid cavity.
- Ax no bone canal removal, A1 tympanic sulcus widening, A2 external canal widening, A3 total canalplasty.
- Tx no ear drum grafting, Tn original ear drum preserved, T1 intact membrane reinforcement, T2 partial grafting, T3 total ear drum grafting.
- Ost tympanic membrane to stapes head, On intact chain preservation, Ox no reconstruction performed, Osd ear drum directly repositioned to stapes head, Oft reconstruction between ear drum and foot plate of the stapes, Ofd ear drum directly repositioned onto stapes footplate [12].
2.4. Statistics
2.5. Theory/Calculation
3. Results
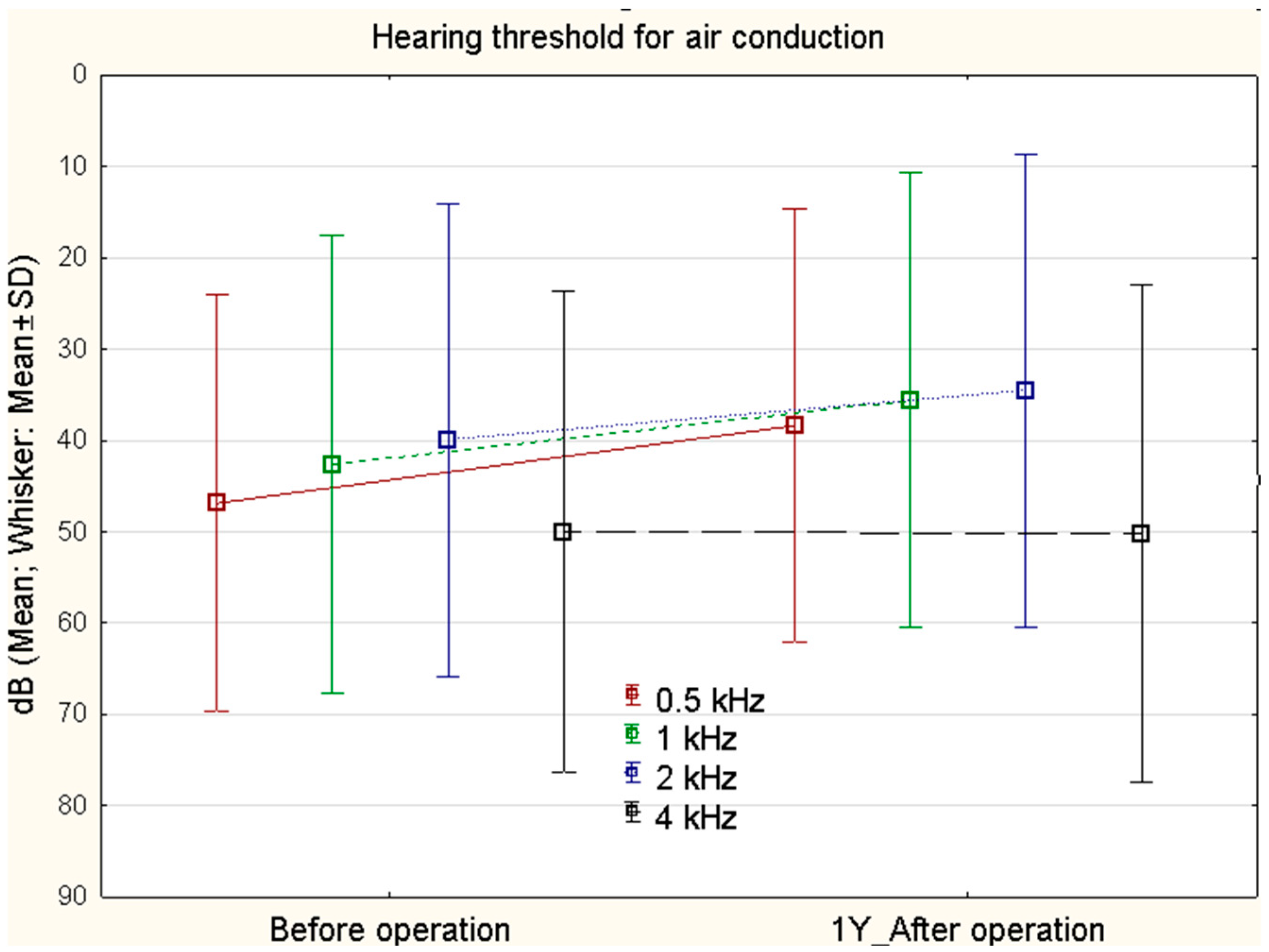
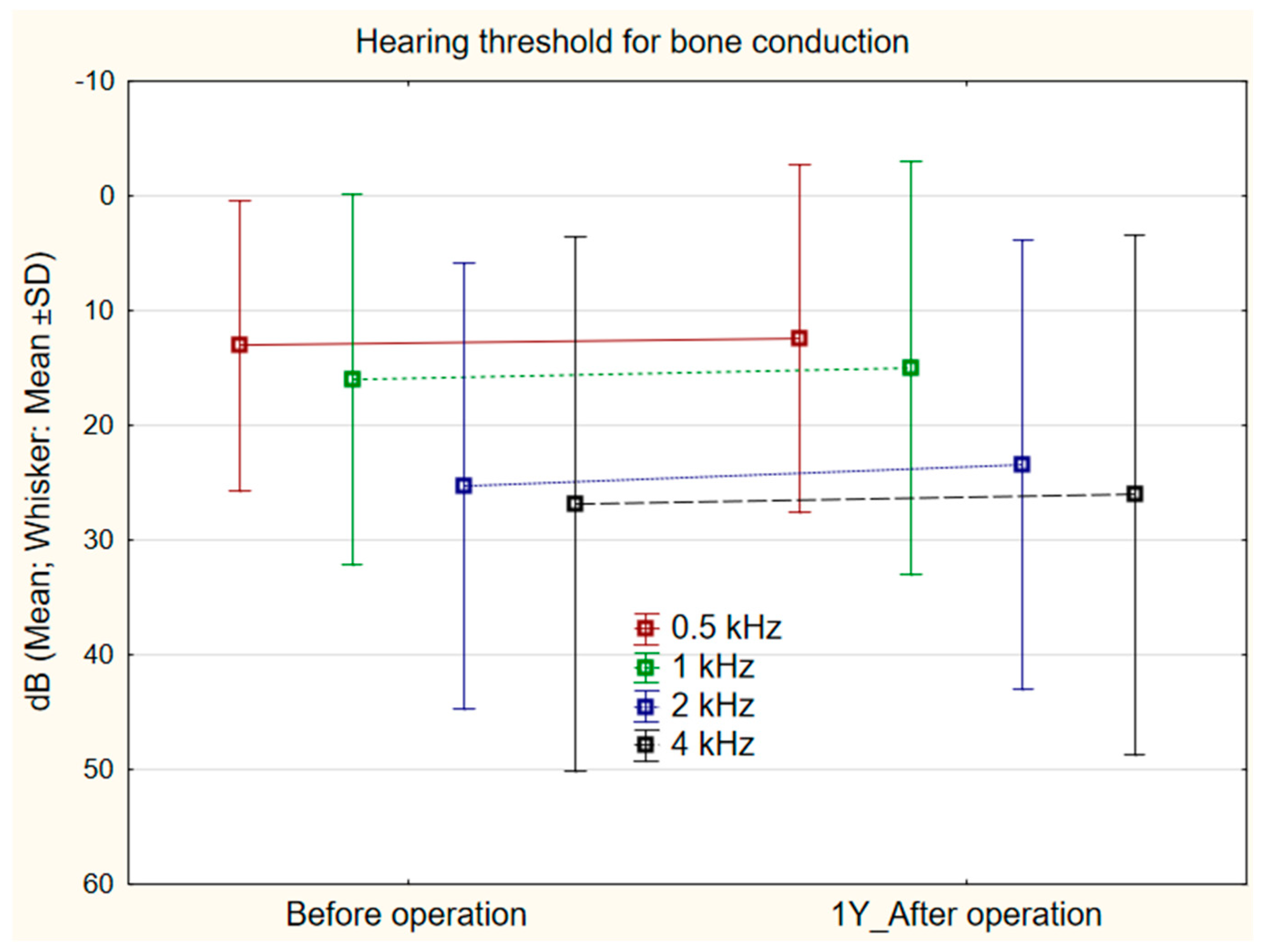
3.1. Changes in Bone Conduction
3.2. STAM
3.3. Stage of Cholesteatoma
3.4. SAMEO-ATO
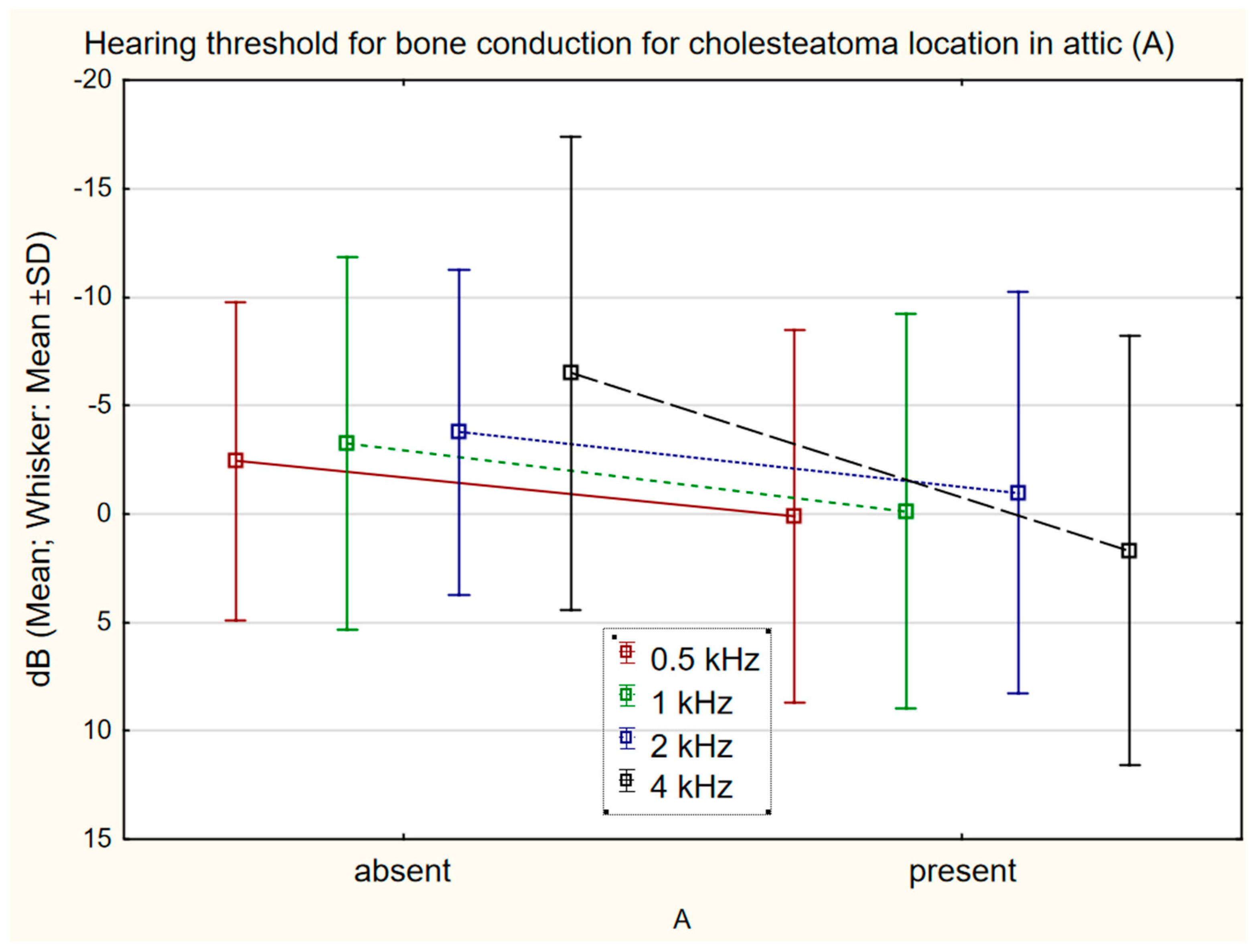
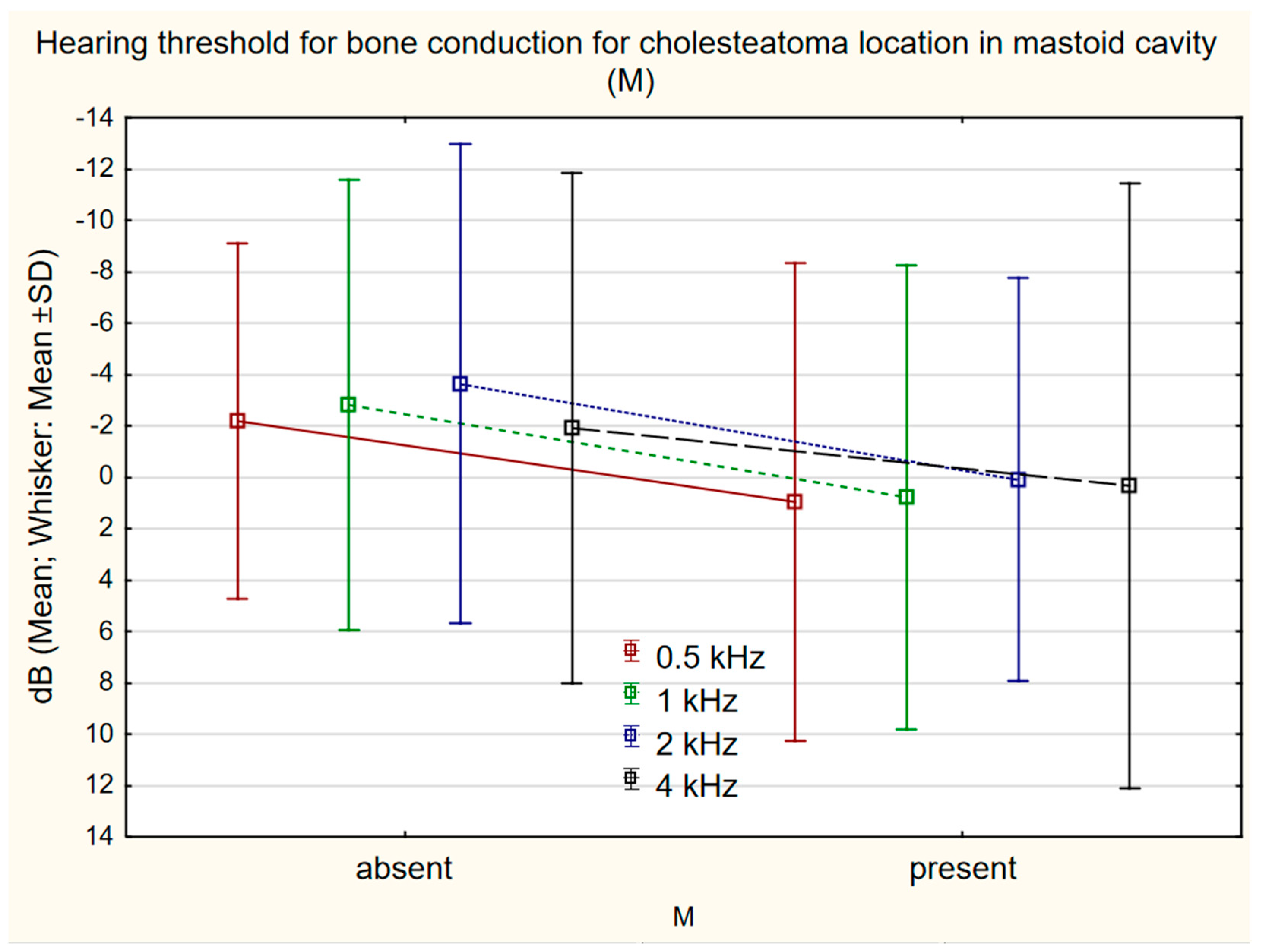
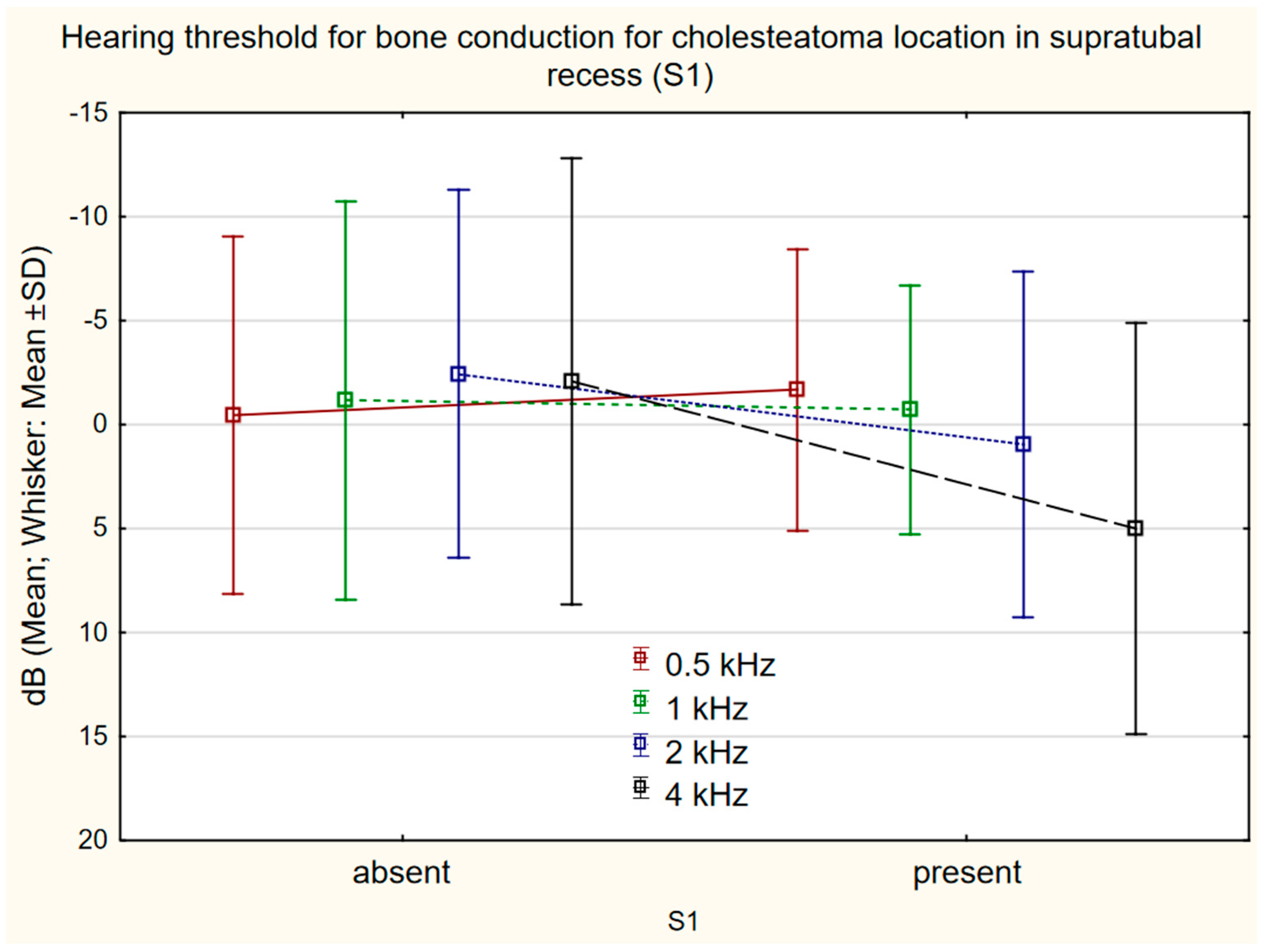
3.5. Relationship between Cholesteatoma Location and Bone Conduction Frequency
4. Discussion
- Physically, by blocking the movement of the middle-ear bones and oval window membrane, which decreases the motility of liquid and firm structures of the inner ear under sound stimulation. Cholesteatoma impairs the movement of the oval window membrane by direct contact; and contact with middle-ear bones increases impedance and reactance, and hinders movement of the footplate in the oval window. These mechanisms also block the movements of perilymph and thus, indirectly, the movement of hair cells.
- Chemically, by releasing toxins into inner ear perilymph, which impairs the movement and metabolism of hair cells.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Valenta, T.; Homoláč, M.; Školoudík, L.; Mejzlík, J.; Chrobok, V. Current classification and staging of middle ear cholesteatoma. Otolaryngol. A Foniat. Prague 2020, 69, 172–176. [Google Scholar]
- Albrecht, W. Classification of the cholesteatoma of the middle ear as neoplasm? Z. Laryngol. Rhinol. Otol. 1952, 31, 417–424. [Google Scholar] [PubMed]
- Saleh, H.A.; Mills, R.P. Classification and staging of cholesteatoma. Clin. Otolaryngol. Allied Sci. 1999, 24, 355–359. [Google Scholar] [CrossRef] [PubMed]
- Bachinger, D.; Rrahmani, A.; Weiss, N.M.; Mlynski, R.; Huber, A.; Roosli, C. Evaluating hearing outcome, recidivism and complications in cholesteatoma surgery using the ChOLE classification system. Eur. Arch. Otorhinolaryngol. 2020, 278, 1365–1371. [Google Scholar] [CrossRef] [PubMed]
- Tos, M.; Lau, T.; Plate, S. Sensorineural hearing loss following chronic ear surgery. Ann. Otol. Rhinol. Laryngol. 1984, 93, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Sunwoo, W.; Lee, S.Y.; Seong, J.; Han, Y.E.; Park, M.H. Clinical Characteristics of Patients with Cochlear Fistulas Caused by Chronic Otitis Media with Cholesteatoma. J. Int. Adv. Otol. 2020, 16, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.; Kim, Y.; Kim, D.K. Sensorineural Hearing Loss after Surgery to Treat Chronic Otitis Media. Ear Nose Throat J. 2020, 100, 220S–224S. [Google Scholar] [CrossRef]
- Gulustan, F.; Yazici, Z.M.; Sayin, I.; Abakay, M.A.; Gunes, S.; Akidil, A.O. Evaluation of the Presence of Sensorineural Hearing Loss and the Relationship With Intraoperative Findings in Cholesteatoma. Ear Nose Throat J. 2021, 100, 249S–252S. [Google Scholar] [CrossRef]
- Wiatr, M.; Skladzien, J.; Wiatr, A.; Tomik, J.; Strek, P.; Medon, D. Postoperative bone conduction threshold changes in patients operated on for chronic otitis media-analysis. Otolaryngol. Pol. 2015, 69, 1–6. [Google Scholar] [CrossRef][Green Version]
- Kazikdas, K.C.; Onal, K.; Yildirim, N. Sensorineural hearing loss after ossicular manipulation and drill-generated acoustic trauma in type I tympanoplasty with and without mastoidectomy: A series of 51 cases. Ear Nose Throat J. 2015, 94, 378–398. [Google Scholar]
- Yung, M.; James, A.; Merkus, P.; Philips, J.; Black, B.; Tono, T.; Linder, T.; Dornhoffer, J.; Incesulu, A. International Otology Outcome Group and the International Consensus on the Categorization of Tympanomastoid Surgery. J. Int. Adv. Otol. 2018, 14, 216–226. [Google Scholar] [CrossRef]
- Yung, M.; Tono, T.; Olszewska, E.; Yamamoto, Y.; Sudhoff, H.; Sakagami, M.; Mulder, J.; Kojima, H.; İncesulu, A.; Trabalzini, F.; et al. EAONO/JOS Joint Consensus Statements on the Definitions, Classification and Staging of Middle Ear Cholesteatoma. J. Int. Adv. Otol. 2017, 13, 1–8. [Google Scholar] [CrossRef]
- Mahmoudian-Sani, M.R.; Mehri-Ghahfarrokhi, A.; Ahmadinejad, F.; Hashemzadeh-Chaleshtori, M.; Saidijam, M.; Jami, M.S. MicroRNAs: Effective elements in ear-related diseases and hearing loss. Eur. Arch. Otorhinolaryngol. 2017, 274, 2373–2380. [Google Scholar] [CrossRef] [PubMed]
- Wiatr, M.; Skladzien, J.; Strek, P.; Przeklasa-Muszynska, A.; Wiatr, A. Chronic Otitis Media with Granulation Is a Poor Prognostic Factor for Hearing Improvement and Development of Intracranial Complications. J. Int. Adv. Otol. 2019, 15, 12–17. [Google Scholar] [CrossRef]
- Chrobok, V.; Pellant, A.; Meloun, M.; Pokorný, K.; Šimáková, E. Prognostic factors of chronic otitis. Part 1-Preoperative factors. Otolaryngol. A Foniat. Prague 2007, 56, 195–207. [Google Scholar]
- Baradaranfar, M.H.; Shahbazian, H.; Behniafard, N.; Atighechi, S.; Dadgarnia, M.H.; Mirvakili, A.; Mollasadeghi, A.; Baradaranfar, A. The effect of drill-generated noise in the contralateral healthy ear following mastoid surgery: The emphasis on hearing threshold recovery time. Noise Health 2015, 17, 209–215. [Google Scholar] [CrossRef]
- Vartiainen, E.; Seppa, J. Results of bone conduction following surgery for chronic ear disease. Eur. Arch. Otorhinolaryngol. 1997, 254, 384–386. [Google Scholar] [CrossRef]
- Blakley, B.W.; Kim, S.; VanCamp, M. Preoperative hearing predicts postoperative hearing. Otolaryngol. Head Neck Surg. 1998, 119, 559–563. [Google Scholar] [CrossRef]
- Rosito, L.S.; Netto, L.S.; Teixeira, A.R.; da Costa, S.S. Sensorineural Hearing Loss in Cholesteatoma. Otol. Neurotol. 2016, 37, 214–217. [Google Scholar] [CrossRef][Green Version]
- Fukuda, A.; Morita, S.; Nakamaru, Y.; Hoshino, K.; Fujiwara, K.; Homma, A. Short-Term Hearing Prognosis of Ossiculoplasty in Pars Flaccida Cholesteatoma Using the EAONO/JOS Staging System. J. Int. Adv. Otol. 2019, 15, 2–7. [Google Scholar] [CrossRef]
- Wang, Y.; Pan, T.; Lu, Z.Y.; Ma, F.R. The hearing outcomes of modified canal wall down and canal wall up mastoidectomy and tympanoplasty. Chin. J. Otorhinolaryngol. Head Neck Surg. 2020, 55, 748–753. [Google Scholar] [CrossRef]
- Eeg-Olofsson, M.; Stenfelt, S.; Taghavi, H.; Reinfeldt, S.; Hakansson, B.; Tengstrand, T.; Finizia, C. Transmission of bone conducted sound-correlation between hearing perception and cochlear vibration. Hear. Res. 2013, 306, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Putzeys, T.; Borgers, C.; Fierens, G.; Walraevens, J.; Van Wieringen, A.; Verhaert, N. Intracochlear pressure as an objective measure for perceived loudness with bone conduction implants. Hear. Res. 2022, 422, 108550. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, H.; Miyamoto, I.; Takahashi, H. Relationship between CT findings and sensorineural hearing loss in chronic otitis media. Auris Nasus Larynx 2014, 41, 259–263. [Google Scholar] [CrossRef]
- Wiatr, M.; Wiatr, A.; Kocon, S.; Skladzien, J. Factors that have an influence on bone conduction thresholds changes after otosurgery in the patients operated on due to the perforation of the tympanic membrane with the preserved ossicular chain. Otolaryngol. Pol. 2017, 71, 26–33. [Google Scholar] [CrossRef]
| S | A | M | E | O | |||||
|---|---|---|---|---|---|---|---|---|---|
| S1 | 120 | A3 | 28 | Mx | 21 | Ex | 48 | Ox | 96 |
| A4 | 92 | M1a | 4 | E1 | 19 | O1 | 18 | ||
| M1a + 2a | 46 | E2 | 53 | O2 | 6 | ||||
| M2a | 18 | ||||||||
| M2b | 6 | ||||||||
| M2c | 20 | ||||||||
| M3a | 4 | ||||||||
| M3b | 1 |
| A | T | O | |||
|---|---|---|---|---|---|
| Ax | 115 | Tx | 12 | Ost | 14 |
| A1 | 4 | T1 | 4 | On | 13 |
| A2 | 1 | T2 | 102 | Ox | 15 |
| T3 | 2 | Osd | 52 | ||
| Oft | 18 | ||||
| Ofd | 8 | ||||
| Location/ p-Value | 0.5 kHz | 1 kHz | 2 kHz | 4 kHz |
|---|---|---|---|---|
| A | 0.087 | 0.053 | 0.189 | 0.0001 |
| T | 0.497 | 0.681 | 0.745 | 0.742 |
| M | 0.024 | 0.032 | 0.039 | 0.476 |
| S1 | 0.683 | 0.712 | 0.103 | 0.003 |
| S2 | 0.684 | 0.841 | 0.473 | 0.555 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mejzlik, J.; Chrobok, V.; Homolac, M.; Valenta, T.; Svejdova, A.; Cerny, M.; Striteska, M.; Krtickova, J.; Skoloudik, L. The Relationship between Bone Conduction Hearing Threshold Shifts after Surgery for Chronic Otitis Media with Cholesteatoma According to STAM, EAONO/JOS, and SAMEO-ATO Classifications. J. Clin. Med. 2022, 11, 4481. https://doi.org/10.3390/jcm11154481
Mejzlik J, Chrobok V, Homolac M, Valenta T, Svejdova A, Cerny M, Striteska M, Krtickova J, Skoloudik L. The Relationship between Bone Conduction Hearing Threshold Shifts after Surgery for Chronic Otitis Media with Cholesteatoma According to STAM, EAONO/JOS, and SAMEO-ATO Classifications. Journal of Clinical Medicine. 2022; 11(15):4481. https://doi.org/10.3390/jcm11154481
Chicago/Turabian StyleMejzlik, Jan, Viktor Chrobok, Michal Homolac, Tomas Valenta, Anna Svejdova, Michal Cerny, Maja Striteska, Jana Krtickova, and Lukas Skoloudik. 2022. "The Relationship between Bone Conduction Hearing Threshold Shifts after Surgery for Chronic Otitis Media with Cholesteatoma According to STAM, EAONO/JOS, and SAMEO-ATO Classifications" Journal of Clinical Medicine 11, no. 15: 4481. https://doi.org/10.3390/jcm11154481
APA StyleMejzlik, J., Chrobok, V., Homolac, M., Valenta, T., Svejdova, A., Cerny, M., Striteska, M., Krtickova, J., & Skoloudik, L. (2022). The Relationship between Bone Conduction Hearing Threshold Shifts after Surgery for Chronic Otitis Media with Cholesteatoma According to STAM, EAONO/JOS, and SAMEO-ATO Classifications. Journal of Clinical Medicine, 11(15), 4481. https://doi.org/10.3390/jcm11154481






