History of Technological Advancements towards MR-Linac: The Future of Image-Guided Radiotherapy
Abstract
:1. Introduction
2. History of Technologic Advancements in IGRT
2.1. The Origins of Radiotherapy—Dose and Fractionation
2.2. The Rise of Image Guidance in Radiotherapy
2.3. Technical Evolution of Treatment Conformality
2.4. Adaptive Treatment Planning
2.5. A Brief History of Magnetic Resonance Imaging
3. Current MRgRT Systems and Applications
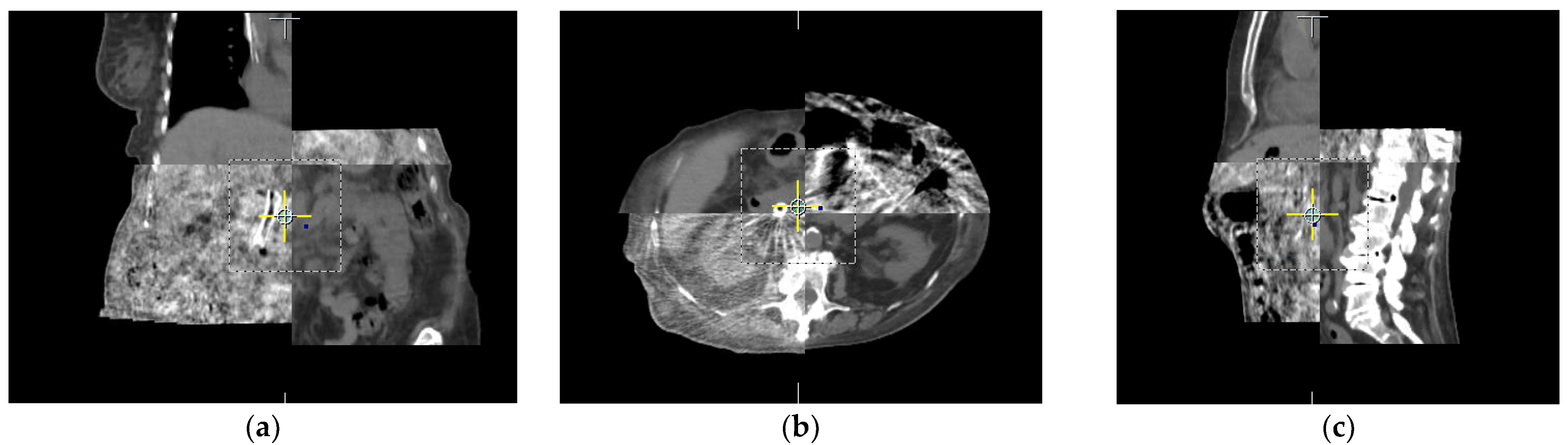
3.1. Advancing from CT to MRI-Guided Radiotherapy
3.2. Current MR-Guided Systems
3.2.1. The ViewRay MRIdian
3.2.2. The Elekta Unity
3.2.3. Comparison between ViewRay MRIdian and Elekta Unity
3.3. Other MRI-Linacs in Development
3.4. Advantages of MR-Guided Radiotherapy
3.5. Limitations of MR-Guided Radiotherapy
4. Future Applications and Expected Advancements in MRL Technology
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Abbreviation | Definition |
| 2D | Two-dimensional |
| 3D | Three-dimensional |
| ATP | Adapt-to-Position |
| ATS | Adapt-to-Shape |
| CBCT | Cone-beam computed tomography |
| cGy | Centigray |
| CT | Computed Tomography |
| dB | Decibel |
| DNA | Deoxyribonucleic acid |
| ERE | Electron Return Effect |
| Gy | Gray |
| IGRT | Image-guided Radiotherapy |
| IMRT | Intensity-modulated radiation therapy |
| Linac | Linear Accelerator |
| MLC | Multileaf Collimator |
| MR | Magnetic Resonance |
| MRgRT | Magnetic Resonance-Guided Radiotherapy |
| MRI | Magnetic Resonance Imaging |
| MRL | Magnetic Resonance Linear Accelerator |
| MU | Monitor Unit |
| MV | Megavolt |
| MVCT | Megavoltage Computed Tomography |
| NMR | Nuclear Magnetic Resonance |
| OAR | Organ at Risk |
| PET | Positron Emission Tomography |
| PTV | Planning Target Volume |
| RF | Radiofrequency |
| RT | Radiotherapy |
| S&S | Step-and-Shoot |
| SNR | Signal-to-Noise Ratio |
| SPECT | single-photon emission computed tomography |
| SW | Sliding Window |
| T | Tesla |
| T1 | Longitudinal relaxation time |
| T2 | Transverse relaxation time |
| TPS | Treatment planning system |
| VMAT | Volumetric Modulated Arc Therapy |
References
- Hall, W.A.; Paulson, E.S.; van der Heide, U.A.; Fuller, C.D.; Raaymakers, B.W.; Lagendijk, J.J.W.; Li, X.A.; Jaffray, D.A.; Dawson, L.A.; Erickson, B.; et al. The transformation of radiation oncology using real-time magnetic resonance guidance: A review. Eur. J. Cancer 2019, 122, 42–52. [Google Scholar] [CrossRef] [PubMed]
- Jaffray, D.A. Image-guided radiotherapy: From current concept to future perspectives. Nat. Rev. Clin. Oncol. 2012, 9, 688–699. [Google Scholar] [CrossRef] [PubMed]
- Almansour, H.; Afat, S.; Fritz, V.; Schick, F.; Nachbar, M.; Thorwarth, D.; Zips, D.; Muller, A.C.; Nikolaou, K.; Othman, A.E.; et al. Prospective Image Quality and Lesion Assessment in the Setting of MR-Guided Radiation Therapy of Prostate Cancer on an MR-Linac at 1.5 T: A Comparison to a Standard 3 T MRI. Cancers 2021, 13, 1533. [Google Scholar] [CrossRef] [PubMed]
- De Muinck Keizer, D.M.; van der Voort van Zyp, J.R.N.; de Groot-van Breugel, E.N.; Raaymakers, B.W.; Lagendijk, J.J.W.; de Boer, H.C.J. On-line daily plan optimization combined with a virtual couch shift procedure to address intrafraction motion in prostate magnetic resonance guided radiotherapy. Phys. Imaging Radiat. Oncol. 2021, 19, 90–95. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Cazoulat, G.; Wu, C.; Peterson, C.; McCulloch, M.; Anderson, B.; Pollard-Larkin, J.; Balter, P.; Liao, Z.; Mohan, R.; et al. Geometric and dosimetric accuracy of deformable image registration between average-intensity images for 4DCT-based adaptive radiotherapy for non-small cell lung cancer. J. Appl. Clin. Med Phys. 2021, 22, 156–167. [Google Scholar] [CrossRef] [PubMed]
- Schreuder, N. Principles and Practice of Proton Beam Therapy; AAPM Monograph No. 37, 2015 Summer School; Das, I.J., Paganett, H., Eds.; Medical Physics Publishing: Madison, WI, USA, 2019; Volume 46, p. 3324. ISBN 9781936366439. [Google Scholar] [CrossRef]
- Glasser, O. Wilhelm Conrad Röntgen and the Early History of the Roentgen Rays; Norman Pub.: San Francisco, CA, USA, 1993; pp. 233–282. [Google Scholar]
- Röntgen, W.C. Ueber eine neue Art von Strahlen. Ann. Phys. 1898, 300, 12–17. [Google Scholar] [CrossRef]
- Clark, A. The Effect of the Roentgen Rays in a Case of Chronic Carcinoma of the Breast. Br. Med. J. 1901, 1, 1398–1399. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, G.B. Recurrent Carcinoma Treated by the Roentgen Rays. Br. Med. J. 1902, 1, 265–266. [Google Scholar] [CrossRef] [PubMed]
- Colvett, K. The history of radiation oncology. South. Med. J. 2006, 99, 1155–1156. [Google Scholar] [CrossRef] [PubMed]
- McCarty, P.J.; Million, R.R. History of radiation oncology. J. Fla. Med. Assoc. 1995, 82, 745–748. [Google Scholar]
- Eric, J.; Hall, A.J.G. Radiobiology for the Radiologist, 8th ed.; Wolters Kluwer: Alphen aan den Rijn, The Netherlands, 2018. [Google Scholar]
- Giaccia, A.J. Molecular radiobiology: The state of the art. J. Clin. Oncol. 2014, 32, 2871–2878. [Google Scholar] [CrossRef]
- Hall, E.J.; Astor, M.; Bedford, J.; Borek, C.; Curtis, S.B.; Fry, M.; Geard, C.; Hei, T.; Mitchell, J.; Oleinick, N.; et al. Basic radiobiology. Am. J. Clin. Oncol. 1988, 11, 220–252. [Google Scholar] [CrossRef] [PubMed]
- Thames, H.D. On the Origin of Dose Fractionation Regimens in Radiotherapy. Semin. Radiat. Oncol. 1992, 2, 3–9. [Google Scholar] [CrossRef]
- Laprie, A.; LaMarre, A.K.; Haas-Kogan, D.A. Hyperfractionation: Fractious or not? Int. J. Radiat. Oncol. Biol. Phys. 2014, 88, 269–271. [Google Scholar] [CrossRef]
- Gilbo, P.; Potters, L.; Lee, L. Implementation and utilization of hypofractionation for breast cancer. Adv. Radiat. Oncol. 2018, 3, 265–270. [Google Scholar] [CrossRef] [PubMed]
- Hickey, B.E.; James, M.L.; Daly, T.; Soh, F.Y.; Jeffery, M. Hypofractionation for clinically localized prostate cancer. Cochrane Database Syst. Rev. 2019, 9, CD011462. [Google Scholar] [CrossRef] [PubMed]
- Vischioni, B.; Petrucci, R.; Valvo, F. Hypofractionation in prostate cancer radiotherapy: A step forward towards clinical routine. Transl. Androl. Urol. 2019, 8, S528–S532. [Google Scholar] [CrossRef] [PubMed]
- Group, S.T.; Bentzen, S.M.; Agrawal, R.K.; Aird, E.G.; Barrett, J.M.; Barrett-Lee, P.J.; Bliss, J.M.; Brown, J.; Dewar, J.A.; Dobbs, H.J.; et al. The UK Standardisation of Breast Radiotherapy (START) Trial A of radiotherapy hypofractionation for treatment of early breast cancer: A randomised trial. Lancet Oncol. 2008, 9, 331–341. [Google Scholar] [CrossRef]
- Group, S.T.; Bentzen, S.M.; Agrawal, R.K.; Aird, E.G.; Barrett, J.M.; Barrett-Lee, P.J.; Bentzen, S.M.; Bliss, J.M.; Brown, J.; Dewar, J.A.; et al. The UK Standardisation of Breast Radiotherapy (START) Trial B of radiotherapy hypofractionation for treatment of early breast cancer: A randomised trial. Lancet 2008, 371, 1098–1107. [Google Scholar] [CrossRef]
- Loblaw, A. Ultrahypofractionation Should be a Standard of Care Option for Intermediate-Risk Prostate Cancer. Clin. Oncol. (R. Coll. Radiol.) 2020, 32, 170–174. [Google Scholar] [CrossRef]
- Verellen, D.; De Ridder, M.; Storme, G. A (short) history of image-guided radiotherapy. Radiother. Oncol. 2008, 86, 4–13. [Google Scholar] [CrossRef]
- Hounsfield, G.N. Computerized transverse axial scanning (tomography). 1. Description of system. Br. J. Radiol. 1973, 46, 1016–1022. [Google Scholar] [CrossRef] [PubMed]
- Bull, J. The History of Computed Tomography. In Computerized Tomography; Caillé, J.M., Salamon, G., Eds.; Springer: Berlin/Heidelberg, Germany, 1980; pp. 3–6. [Google Scholar]
- Uldin, T. Virtual anthropology—A brief review of the literature and history of computed tomography. Forensic Sci. Res. 2017, 2, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Dawson, L.A.; Sharpe, M.B. Image-guided radiotherapy: Rationale, benefits, and limitations. Lancet Oncol. 2006, 7, 848–858. [Google Scholar] [CrossRef]
- Cho, P.S.; Johnson, R.H.; Griffin, T.W. Cone-beam CT for radiotherapy applications. Phys. Med. Biol. 1995, 40, 1863–1883. [Google Scholar] [CrossRef]
- Jaffray, D.A.; Siewerdsen, J.H. Cone-beam computed tomography with a flat-panel imager: Initial performance characterization. Med. Phys. 2000, 27, 1311–1323. [Google Scholar] [CrossRef] [PubMed]
- Pacelli, R.; Caroprese, M.; Palma, G.; Oliviero, C.; Clemente, S.; Cella, L.; Conson, M. Technological evolution of radiation treatment: Implications for clinical applications. Semin. Oncol. 2019, 46, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Bruch, P.M.; Zhen, W. Viewpoints to consider in the development of MLC and IMRT programs. Med. Dosim. 2001, 26, 91–94. [Google Scholar] [CrossRef]
- Wang, X.; Zhang, X.; Dong, L.; Liu, H.; Wu, Q.; Mohan, R. Development of methods for beam angle optimization for IMRT using an accelerated exhaustive search strategy. Int. J. Radiat. Oncol. Biol. Phys. 2004, 60, 1325–1337. [Google Scholar] [CrossRef]
- Das, I.J.; Sanfilippo, N.J.; Fogliata, A.; Cozzi, L. Intensity Modulated Radiation Therapy. In A Clinical Overview; IOP Publishing: Bristol, UK, 2020. [Google Scholar] [CrossRef]
- Herman Tde, L.; Schnell, E.; Young, J.; Hildebrand, K.; Algan, O.; Syzek, E.; Herman, T.; Ahmad, S. Dosimetric comparison between IMRT delivery modes: Step-and-shoot, sliding window, and volumetric modulated arc therapy—For whole pelvis radiation therapy of intermediate-to-high risk prostate adenocarcinoma. J. Med. Phys. 2013, 38, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Otto, K. Volumetric modulated arc therapy: IMRT in a single gantry arc. Med. Phys. 2008, 35, 310–317. [Google Scholar] [CrossRef]
- Zygmanski, P.; Hogele, W.; Cormack, R.; Chin, L.; Loschel, R. A volumetric-modulated arc therapy using sub-conformal dynamic arc with a monotonic dynamic multileaf collimator modulation. Phys. Med. Biol. 2008, 53, 6395–6417. [Google Scholar] [CrossRef]
- Brock, K.K.; Dawson, L.A. Adaptive management of liver cancer radiotherapy. Semin. Radiat. Oncol. 2010, 20, 107–115. [Google Scholar] [CrossRef]
- Brock, K.K. Adaptive Radiotherapy: Moving Into the Future. Semin. Radiat. Oncol. 2019, 29, 181–184. [Google Scholar] [CrossRef]
- Paulson, E.S.; Ahunbay, E.; Chen, X.; Mickevicius, N.J.; Chen, G.P.; Schultz, C.; Erickson, B.; Straza, M.; Hall, W.A.; Li, X.A. 4D-MRI driven MR-guided online adaptive radiotherapy for abdominal stereotactic body radiation therapy on a high field MR-Linac: Implementation and initial clinical experience. Clin. Transl. Radiat. Oncol. 2020, 23, 72–79. [Google Scholar] [CrossRef]
- Yan, D.; Chen, S.; Krauss, D.J.; Chen, P.Y.; Chinnaiyan, P.; Wilson, G.D. Tumor Voxel Dose-Response Matrix and Dose Prescription Function Derived Using (18)F-FDG PET/CT Images for Adaptive Dose Painting by Number. Int. J. Radiat. Oncol. Biol. Phys. 2019, 104, 207–218. [Google Scholar] [CrossRef] [PubMed]
- Urwin, R.; Barrington, S.F.; Mikhaeel, N.G. Role of PET imaging in adaptive radiotherapy for lymphoma. Q. J. Nucl. Med. Mol. Imaging 2018, 62, 411–419. [Google Scholar] [CrossRef] [PubMed]
- Otazo, R.; Lambin, P.; Pignol, J.P.; Ladd, M.E.; Schlemmer, H.P.; Baumann, M.; Hricak, H. MRI-guided Radiation Therapy: An Emerging Paradigm in Adaptive Radiation Oncology. Radiology 2021, 298, 248–260. [Google Scholar] [CrossRef] [PubMed]
- Hall, W.A.; Paulson, E.; Li, X.A.; Erickson, B.; Schultz, C.; Tree, A.; Awan, M.; Low, D.A.; McDonald, B.A.; Salzillo, T.; et al. Magnetic resonance linear accelerator technology and adaptive radiation therapy: An overview for clinicians. CA Cancer J. Clin. 2022, 72, 34–56. [Google Scholar] [CrossRef] [PubMed]
- Damadian, R. Tumor detection by nuclear magnetic resonance. Science 1971, 171, 1151–1153. [Google Scholar] [CrossRef] [PubMed]
- Lauterbur, P.C. Image formation by induced local interactions. Examples employing nuclear magnetic resonance. Nature 1973, 242, 190–191. [Google Scholar] [CrossRef]
- Lauterbur, P.C. Paul Lauterbur and Sir Peter Mansfield for MRI. Eur. Heart J. 2019, 40, 1898–1899. [Google Scholar] [CrossRef]
- Caravan, P.; Ellison, J.J.; McMurry, T.J.; Lauffer, R.B. Gadolinium(III) Chelates as MRI Contrast Agents: Structure, Dynamics, and Applications. Chem. Rev. 1999, 99, 2293–2352. [Google Scholar] [CrossRef] [PubMed]
- Helm, L.; Merbach, A.E.; Tóth, É. The Chemistry of Contrast Agents in Medical Magnetic Resonance Imaging, 2nd ed.; John Wiley & Sons Inc.: Hoboken, NJ, USA, 2013; pp. 98e–497e. Available online: http://turing.library.northwestern.edu/login?url=http://site.ebrary.com/lib/northwestern/Doc?id=10667388 (accessed on 1 July 2016).
- Winter, P.M.; Caruthers, S.D.; Wickline, S.A.; Lanza, G.M. Molecular imaging by MRI. Curr. Cardiol. Rep. 2006, 8, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Villaraza, A.J.L.; Bumb, A.; Brechbiel, M.W. Macromolecules, Dendrimers, and Nanomaterials in Magnetic Resonance Imaging: The Interplay between Size, Function, and Pharmacokinetics. Chem. Rev. 2010, 110, 2921–2959. [Google Scholar] [CrossRef] [PubMed]
- Shellock, F.G.; Spinazzi, A. MRI Safety Update 2008: Part 1, MRI Contrast Agents and Nephrogenic Systemic Fibrosis. Am. J. Roentgenol. 2008, 191, 1129–1139. [Google Scholar] [CrossRef] [PubMed]
- Shellock, F.G.; Spinazzi, A. MRI Safety Update 2008: Part 2, Screening Patients for MRI. Am. J. Roentgenol. 2008, 191, 1140–1149. [Google Scholar] [CrossRef]
- Brown, R.W.; Cheng, Y.-C.N.; Haacke, E.M.; Thompson, M.R.; Venkatesan, R. Magnetic Properties of Tissues. In Magnetic Resonance Imaging; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2014; Volume 25, pp. 739–777. [Google Scholar] [CrossRef]
- Srivastava, A.K.; Kadayakkara, D.K.; Bar-Shir, A.; Gilad, A.A.; McMahon, M.T.; Bulte, J.W. Advances in using MRI probes and sensors for in vivo cell tracking as applied to regenerative medicine. Dis. Models Mech. 2015, 8, 323–336. [Google Scholar] [CrossRef]
- Raymond, K.N.; Pierre, V.C. Next Generation, High Relaxivity Gadolinium MRI Agents. Bioconj. Chem. 2005, 16, 3–8. [Google Scholar] [CrossRef]
- Eisbruch, A.; Harris, J.; Garden, A.S.; Chao, C.K.; Straube, W.; Harari, P.M.; Sanguineti, G.; Jones, C.U.; Bosch, W.R.; Ang, K.K. Multi-institutional trial of accelerated hypofractionated intensity-modulated radiation therapy for early-stage oropharyngeal cancer (RTOG 00-22). Int. J. Radiat. Oncol. Biol. Phys. 2010, 76, 1333–1338. [Google Scholar] [CrossRef]
- Kachnic, L.A.; Winter, K.; Myerson, R.J.; Goodyear, M.D.; Willins, J.; Esthappan, J.; Haddock, M.G.; Rotman, M.; Parikh, P.J.; Safran, H.; et al. RTOG 0529: A phase 2 evaluation of dose-painted intensity modulated radiation therapy in combination with 5-fluorouracil and mitomycin-C for the reduction of acute morbidity in carcinoma of the anal canal. Int. J. Radiat. Oncol. Biol. Phys. 2013, 86, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Klopp, A.H.; Yeung, A.R.; Deshmukh, S.; Gil, K.M.; Wenzel, L.; Westin, S.N.; Gifford, K.; Gaffney, D.K.; Small, W., Jr.; Thompson, S.; et al. Patient-Reported Toxicity During Pelvic Intensity-Modulated Radiation Therapy: NRG Oncology-RTOG 1203. J. Clin. Oncol. 2018, 36, 2538–2544. [Google Scholar] [CrossRef] [PubMed]
- Kasivisvanathan, V.; Rannikko, A.S.; Borghi, M.; Panebianco, V.; Mynderse, L.A.; Vaarala, M.H.; Briganti, A.; Budäus, L.; Hellawell, G.; Hindley, R.G.; et al. MRI-Targeted or Standard Biopsy for Prostate-Cancer Diagnosis. N. Engl. J. Med. 2018, 378, 1767–1777. [Google Scholar] [CrossRef] [PubMed]
- Kerkmeijer, L.G.W.; Groen, V.H.; Pos, F.J.; Haustermans, K.; Monninkhof, E.M.; Smeenk, R.J.; Kunze-Busch, M.; de Boer, J.C.J.; van der Voort van Zijp, J.; van Vulpen, M.; et al. Focal Boost to the Intraprostatic Tumor in External Beam Radiotherapy for Patients With Localized Prostate Cancer: Results From the FLAME Randomized Phase III Trial. J. Clin. Oncol. 2021, 39, 787–796. [Google Scholar] [CrossRef]
- Noel, C.E.; Parikh, P.J.; Spencer, C.R.; Green, O.L.; Hu, Y.; Mutic, S.; Olsen, J.R. Comparison of onboard low-field magnetic resonance imaging versus onboard computed tomography for anatomy visualization in radiotherapy. Acta Oncol. 2015, 54, 1474–1482. [Google Scholar] [CrossRef]
- Chin, S.; Eccles, C.L.; McWilliam, A.; Chuter, R.; Walker, E.; Whitehurst, P.; Berresford, J.; Van Herk, M.; Hoskin, P.J.; Choudhury, A. Magnetic resonance-guided radiation therapy: A review. J. Med. Imaging Radiat. Oncol. 2020, 64, 163–177. [Google Scholar] [CrossRef]
- Liney, G.P.; Whelan, B.; Oborn, B.; Barton, M.; Keall, P. MRI-Linear Accelerator Radiotherapy Systems. Clin. Oncol. (R. Coll. Radiol.) 2018, 30, 686–691. [Google Scholar] [CrossRef]
- Mutic, S.; Dempsey, J.F. The ViewRay system: Magnetic resonance-guided and controlled radiotherapy. Semin. Radiat. Oncol. 2014, 24, 196–199. [Google Scholar] [CrossRef]
- Raaymakers, B.W.; Lagendijk, J.J.; Overweg, J.; Kok, J.G.; Raaijmakers, A.J.; Kerkhof, E.M.; van der Put, R.W.; Meijsing, I.; Crijns, S.P.; Benedosso, F.; et al. Integrating a 1.5 T MRI scanner with a 6 MV accelerator: Proof of concept. Phys. Med. Biol. 2009, 54, N229–N237. [Google Scholar] [CrossRef]
- Winkel, D.; Bol, G.H.; Kroon, P.S.; van Asselen, B.; Hackett, S.S.; Werensteijn-Honingh, A.M.; Intven, M.P.W.; Eppinga, W.S.C.; Tijssen, R.H.N.; Kerkmeijer, L.G.W.; et al. Adaptive radiotherapy: The Elekta Unity MR-linac concept. Clin. Transl. Radiat. Oncol. 2019, 18, 54–59. [Google Scholar] [CrossRef]
- Wang, D.; Strugnell, W.; Cowin, G.; Doddrell, D.M.; Slaughter, R. Geometric distortion in clinical MRI systems Part II: Correction using a 3D phantom. Magn. Reson. Imaging 2004, 22, 1223–1232. [Google Scholar] [CrossRef] [PubMed]
- Raaijmakers, A.J.; Raaymakers, B.W.; Lagendijk, J.J. Magnetic-field-induced dose effects in MR-guided radiotherapy systems: Dependence on the magnetic field strength. Phys. Med. Biol. 2008, 53, 909–923. [Google Scholar] [CrossRef]
- Kontaxis, C.; Woodhead, P.L.; Bol, G.H.; Lagendijk, J.J.W.; Raaymakers, B.W. Proof-of-concept delivery of intensity modulated arc therapy on the Elekta Unity 1.5 T MR-linac. Phys. Med. Biol. 2021, 66, 04LT01. [Google Scholar] [CrossRef]
- Fallone, B.G.; Murray, B.; Rathee, S.; Stanescu, T.; Steciw, S.; Vidakovic, S.; Blosser, E.; Tymofichuk, D. First MR images obtained during megavoltage photon irradiation from a prototype integrated linac-MR system. Med. Phys. 2009, 36, 2084–2088. [Google Scholar] [CrossRef] [PubMed]
- Keall, P.J.; Barton, M.; Crozier, S. Linac Program, including contributors from Ingham Institute, Illawarra Cancer Care Centre, Liverpool Hospital. The Australian magnetic resonance imaging-linac program. Semin. Radiat. Oncol. 2014, 24, 203–206. [Google Scholar] [CrossRef] [PubMed]
- Mayinger, M.; Ludwig, R.; Christ, S.M.; Dal Bello, R.; Ryu, A.; Weitkamp, N.; Pavic, M.; Garcia Schüler, H.; Wilke, L.; Guckenberger, M.; et al. Benefit of replanning in MR-guided online adaptive radiation therapy in the treatment of liver metastasis. Radiat. Oncol. 2021, 16, 84. [Google Scholar] [CrossRef]
- Feldman, A.M.; Modh, A.; Glide-Hurst, C.; Chetty, I.J.; Movsas, B. Real-time Magnetic Resonance-guided Liver Stereotactic Body Radiation Therapy: An Institutional Report Using a Magnetic Resonance-Linac System. Cureus 2019, 11, e5774. [Google Scholar] [CrossRef]
- Luterstein, E.; Cao, M.; Lamb, J.M.; Raldow, A.; Low, D.; Steinberg, M.L.; Lee, P. Clinical Outcomes Using Magnetic Resonance-Guided Stereotactic Body Radiation Therapy in Patients With Locally Advanced Cholangiocarcinoma. Adv. Radiat. Oncol. 2020, 5, 189–195. [Google Scholar] [CrossRef]
- Henke, L.; Kashani, R.; Robinson, C.; Curcuru, A.; DeWees, T.; Bradley, J.; Green, O.; Michalski, J.; Mutic, S.; Parikh, P.; et al. Phase I trial of stereotactic MR-guided online adaptive radiation therapy (SMART) for the treatment of oligometastatic or unresectable primary malignancies of the abdomen. Radiother. Oncol. 2018, 126, 519–526. [Google Scholar] [CrossRef]
- Finazzi, T.; van Sörnsen de Koste, J.R.; Palacios, M.A.; Spoelstra, F.O.B.; Slotman, B.J.; Haasbeek, C.J.A.; Senan, S. Delivery of magnetic resonance-guided single-fraction stereotactic lung radiotherapy. Phys. Imaging Radiat. Oncol. 2020, 14, 17–23. [Google Scholar] [CrossRef]
- Wojcieszynski, A.P.; Hill, P.M.; Rosenberg, S.A.; Hullett, C.R.; Labby, Z.E.; Paliwal, B.; Geurts, M.W.; Bayliss, R.A.; Bayouth, J.E.; Harari, P.M.; et al. Dosimetric Comparison of Real-Time MRI-Guided Tri-Cobalt-60 Versus Linear Accelerator-Based Stereotactic Body Radiation Therapy Lung Cancer Plans. Technol. Cancer Res. Treat. 2017, 16, 366–372. [Google Scholar] [CrossRef]
- Ehrbar, S.; Braga Kaser, S.; Chamberlain, M.; Krayenbuhl, J.; Wilke, L.; Mayinger, M.; Garcia Schuler, H.; Guckenberger, M.; Andratschke, N.; Tanadini-Lang, S. MR-guided beam gating: Residual motion, gating efficiency and dose reconstruction for stereotactic treatments of the liver and lung. Radiother. Oncol. 2022, 174, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Cao, M.; Gao, Y.; Yoon, S.M.; Yang, Y.; Sheng, K.; Ballas, L.K.; Basehart, V.; Sachdeva, A.; Felix, C.; Low, D.A.; et al. Interfractional Geometric Variations and Dosimetric Benefits of Stereotactic MRI Guided Online Adaptive Radiotherapy (SMART) of Prostate Bed after Radical Prostatectomy: Post-Hoc Analysis of a Phase II Trial. Cancers 2021, 13, 2802. [Google Scholar] [CrossRef] [PubMed]
- Nicosia, L.; Sicignano, G.; Rigo, M.; Figlia, V.; Cuccia, F.; De Simone, A.; Giaj-Levra, N.; Mazzola, R.; Naccarato, S.; Ricchetti, F.; et al. Daily dosimetric variation between image-guided volumetric modulated arc radiotherapy and MR-guided daily adaptive radiotherapy for prostate cancer stereotactic body radiotherapy. Acta Oncol. 2021, 60, 215–221. [Google Scholar] [CrossRef]
- Placidi, L.; Romano, A.; Chiloiro, G.; Cusumano, D.; Boldrini, L.; Cellini, F.; Mattiucci, G.C.; Valentini, V. On-line adaptive MR guided radiotherapy for locally advanced pancreatic cancer: Clinical and dosimetric considerations. Tech. Innov. Patient Support Radiat. Oncol. 2020, 15, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Van Houdt, P.J.; Yang, Y.; van der Heide, U.A. Quantitative Magnetic Resonance Imaging for Biological Image-Guided Adaptive Radiotherapy. Front. Oncol. 2020, 10, 615643. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Cao, M.; Sheng, K.; Gao, Y.; Chen, A.; Kamrava, M.; Lee, P.; Agazaryan, N.; Lamb, J.; Thomas, D.; et al. Longitudinal diffusion MRI for treatment response assessment: Preliminary experience using an MRI-guided tri-cobalt 60 radiotherapy system. Med. Phys. 2016, 43, 1369–1373. [Google Scholar] [CrossRef]
- Park, J.M.; Shin, K.H.; Kim, J.I.; Park, S.Y.; Jeon, S.H.; Choi, N.; Kim, J.H.; Wu, H.G. Air-electron stream interactions during magnetic resonance IGRT: Skin irradiation outside the treatment field during accelerated partial breast irradiation. Strahlenther. Onkol. 2018, 194, 50–59. [Google Scholar] [CrossRef] [PubMed]
- Lagendijk, J.J.; Raaymakers, B.W.; van Vulpen, M. The magnetic resonance imaging-linac system. Semin. Radiat. Oncol. 2014, 24, 207–209. [Google Scholar] [CrossRef]
- Snyder, J.E.; St-Aubin, J.; Yaddanapudi, S.; Boczkowski, A.; Dunkerley, D.A.P.; Graves, S.A.; Hyer, D.E. Commissioning of a 1.5T Elekta Unity MR-linac: A single institution experience. J. Appl. Clin. Med. Phys. 2020, 21, 160–172. [Google Scholar] [CrossRef] [PubMed]
- Xia, W.; Zhang, K.; Li, M.; Tian, Y.; Men, K.; Wang, J.; Yi, J.; Li, Y.; Dai, J. Impact of Magnetic Field on Dose Distribution in MR-Guided Radiotherapy of Head and Neck Cancer. Front. Oncol. 2020, 10, 1739. [Google Scholar] [CrossRef] [PubMed]
- Henke, L.E.; Olsen, J.R.; Contreras, J.A.; Curcuru, A.; DeWees, T.A.; Green, O.L.; Michalski, J.; Mutic, S.; Roach, M.C.; Bradley, J.D.; et al. Stereotactic MR-Guided Online Adaptive Radiation Therapy (SMART) for Ultracentral Thorax Malignancies: Results of a Phase 1 Trial. Adv. Radiat. Oncol. 2019, 4, 201–209. [Google Scholar] [CrossRef]
- Corradini, S.; Alongi, F.; Andratschke, N.; Belka, C.; Boldrini, L.; Cellini, F.; Debus, J.; Guckenberger, M.; Horner-Rieber, J.; Lagerwaard, F.J.; et al. MR-guidance in clinical reality: Current treatment challenges and future perspectives. Radiat. Oncol. 2019, 14, 92. [Google Scholar] [CrossRef] [PubMed]
- Bohoudi, O.; Bruynzeel, A.M.E.; Senan, S.; Cuijpers, J.P.; Slotman, B.J.; Lagerwaard, F.J.; Palacios, M.A. Fast and robust online adaptive planning in stereotactic MR-guided adaptive radiation therapy (SMART) for pancreatic cancer. Radiother. Oncol. 2017, 125, 439–444. [Google Scholar] [CrossRef] [PubMed]
- Kerkmeijer, L.G.; Fuller, C.D.; Verkooijen, H.M.; Verheij, M.; Choudhury, A.; Harrington, K.J.; Schultz, C.; Sahgal, A.; Frank, S.J.; Goldwein, J.; et al. The MRI-Linear Accelerator Consortium: Evidence-Based Clinical Introduction of an Innovation in Radiation Oncology Connecting Researchers, Methodology, Data Collection, Quality Assurance, and Technical Development. Front. Oncol. 2016, 6, 215. [Google Scholar] [CrossRef] [PubMed]
- Bainbridge, H.; Salem, A.; Tijssen, R.H.N.; Dubec, M.; Wetscherek, A.; Van Es, C.; Belderbos, J.; Faivre-Finn, C.; McDonald, F.; Lung tumour site group of the international Atlantic; et al. Magnetic resonance imaging in precision radiation therapy for lung cancer. Transl. Lung Cancer Res. 2017, 6, 689–707. [Google Scholar] [CrossRef] [PubMed]
- Lim-Reinders, S.; Keller, B.M.; Al-Ward, S.; Sahgal, A.; Kim, A. Online Adaptive Radiation Therapy. Int. J. Radiat. Oncol. Biol. Phys. 2017, 99, 994–1003. [Google Scholar] [CrossRef] [PubMed]
- Eccles, C.L.; Campbell, M. Keeping Up with the Hybrid Magnetic Resonance Linear Accelerators: How Do Radiation Therapists Stay Current in the Era of Hybrid Technologies? J. Med. Imaging Radiat. Sci. 2019, 50, 195–198. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.M.; Cao, M.; Hsu, S.; Lamb, J.; Mikaeilian, A.; Yang, Y.; Agazaryan, N.; Low, D.A.; Steinberg, M.L. Magnetic resonance imaging guided reirradiation of recurrent and second primary head and neck cancer. Adv. Radiat. Oncol. 2017, 2, 167–175. [Google Scholar] [CrossRef] [PubMed]
- Kishan, A.U.; Lamb, J.; Casado, M.; Wang, X.; Ma, T.M.; Low, D.; Sheng, K.; Yang, Y.; Gao, Y.; Basehart, V.; et al. Magnetic resonance imaging-guided versus computed tomography-guided stereotactic body radiotherapy for prostate cancer (MIRAGE): Interim analysis of a phase III randomized trial. J. Clin. Oncol. 2022, 40, 255. [Google Scholar] [CrossRef]
- Lamb, J.; Cao, M.; Kishan, A.; Agazaryan, N.; Thomas, D.H.; Shaverdian, N.; Yang, Y.; Ray, S.; Low, D.A.; Raldow, A.; et al. Online Adaptive Radiation Therapy: Implementation of a New Process of Care. Cureus 2017, 9, e1618. [Google Scholar] [CrossRef] [PubMed]
- Oktay, O.; Nanavati, J.; Schwaighofer, A.; Carter, D.; Bristow, M.; Tanno, R.; Jena, R.; Barnett, G.; Noble, D.; Rimmer, Y.; et al. Evaluation of Deep Learning to Augment Image-Guided Radiotherapy for Head and Neck and Prostate Cancers. JAMA Netw. Open 2020, 3, e2027426. [Google Scholar] [CrossRef]
- Zhang, Y.; Paulson, E.; Lim, S.; Hall, W.A.; Ahunbay, E.; Mickevicius, N.J.; Straza, M.W.; Erickson, B.; Li, X.A. A Patient-Specific Autosegmentation Strategy Using Multi-Input Deformable Image Registration for Magnetic Resonance Imaging-Guided Online Adaptive Radiation Therapy: A Feasibility Study. Adv. Radiat. Oncol. 2020, 5, 1350–1358. [Google Scholar] [CrossRef]
- Olanrewaju, A.; Court, L.E.; Zhang, L.; Naidoo, K.; Burger, H.; Dalvie, S.; Wetter, J.; Parkes, J.; Trauernicht, C.J.; McCarroll, R.E.; et al. Clinical Acceptability of Automated Radiation Treatment Planning for Head and Neck Cancer Using the Radiation Planning Assistant. Pract. Radiat. Oncol. 2021, 11, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Johnstone, E.; Wyatt, J.J.; Henry, A.M.; Short, S.C.; Sebag-Montefiore, D.; Murray, L.; Kelly, C.G.; McCallum, H.M.; Speight, R. Systematic Review of Synthetic Computed Tomography Generation Methodologies for Use in Magnetic Resonance Imaging–Only Radiation Therapy. Int. J. Radiat. Oncol. Biol. Phys. 2018, 100, 199–217. [Google Scholar] [CrossRef] [PubMed]
- Chin, A.L.; Lin, A.; Anamalayil, S.; Teo, B.K. Feasibility and limitations of bulk density assignment in MRI for head and neck IMRT treatment planning. J. Appl. Clin. Med. Phys. 2014, 15, 100–111. [Google Scholar] [CrossRef]
- Doemer, A.; Chetty, I.J.; Glide-Hurst, C.; Nurushev, T.; Hearshen, D.; Pantelic, M.; Traughber, M.; Kim, J.; Levin, K.; Elshaikh, M.A.; et al. Evaluating organ delineation, dose calculation and daily localization in an open-MRI simulation workflow for prostate cancer patients. Radiat. Oncol. 2015, 10, 37. [Google Scholar] [CrossRef] [PubMed]
- Dowling, J.A.; Sun, J.; Pichler, P.; Rivest-Hénault, D.; Ghose, S.; Richardson, H.; Wratten, C.; Martin, J.; Arm, J.; Best, L.; et al. Automatic Substitute Computed Tomography Generation and Contouring for Magnetic Resonance Imaging (MRI)-Alone External Beam Radiation Therapy From Standard MRI Sequences. Int. J. Radiat. Oncol. Biol. Phys. 2015, 93, 1144–1153. [Google Scholar] [CrossRef]
- Siversson, C.; Nordström, F.; Nilsson, T.; Nyholm, T.; Jonsson, J.; Gunnlaugsson, A.; Olsson, L.E. Technical Note: MRI only prostate radiotherapy planning using the statistical decomposition algorithm. Med. Phys. 2015, 42, 6090–6097. [Google Scholar] [CrossRef]
- Demol, B.; Boydev, C.; Korhonen, J.; Reynaert, N. Dosimetric characterization of MRI-only treatment planning for brain tumors in atlas-based pseudo-CT images generated from standard T1-weighted MR images. Med. Phys. 2016, 43, 6557–6568. [Google Scholar] [CrossRef] [PubMed]
- Gudur, M.S.; Hara, W.; Le, Q.T.; Wang, L.; Xing, L.; Li, R. A unifying probabilistic Bayesian approach to derive electron density from MRI for radiation therapy treatment planning. Phys. Med. Biol. 2014, 59, 6595–6606. [Google Scholar] [CrossRef] [PubMed]





Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rammohan, N.; Randall, J.W.; Yadav, P. History of Technological Advancements towards MR-Linac: The Future of Image-Guided Radiotherapy. J. Clin. Med. 2022, 11, 4730. https://doi.org/10.3390/jcm11164730
Rammohan N, Randall JW, Yadav P. History of Technological Advancements towards MR-Linac: The Future of Image-Guided Radiotherapy. Journal of Clinical Medicine. 2022; 11(16):4730. https://doi.org/10.3390/jcm11164730
Chicago/Turabian StyleRammohan, Nikhil, James W. Randall, and Poonam Yadav. 2022. "History of Technological Advancements towards MR-Linac: The Future of Image-Guided Radiotherapy" Journal of Clinical Medicine 11, no. 16: 4730. https://doi.org/10.3390/jcm11164730





