Peri-Implant Bone Loss and Overload: A Systematic Review Focusing on Occlusal Analysis through Digital and Analogic Methods
Abstract
1. Introduction
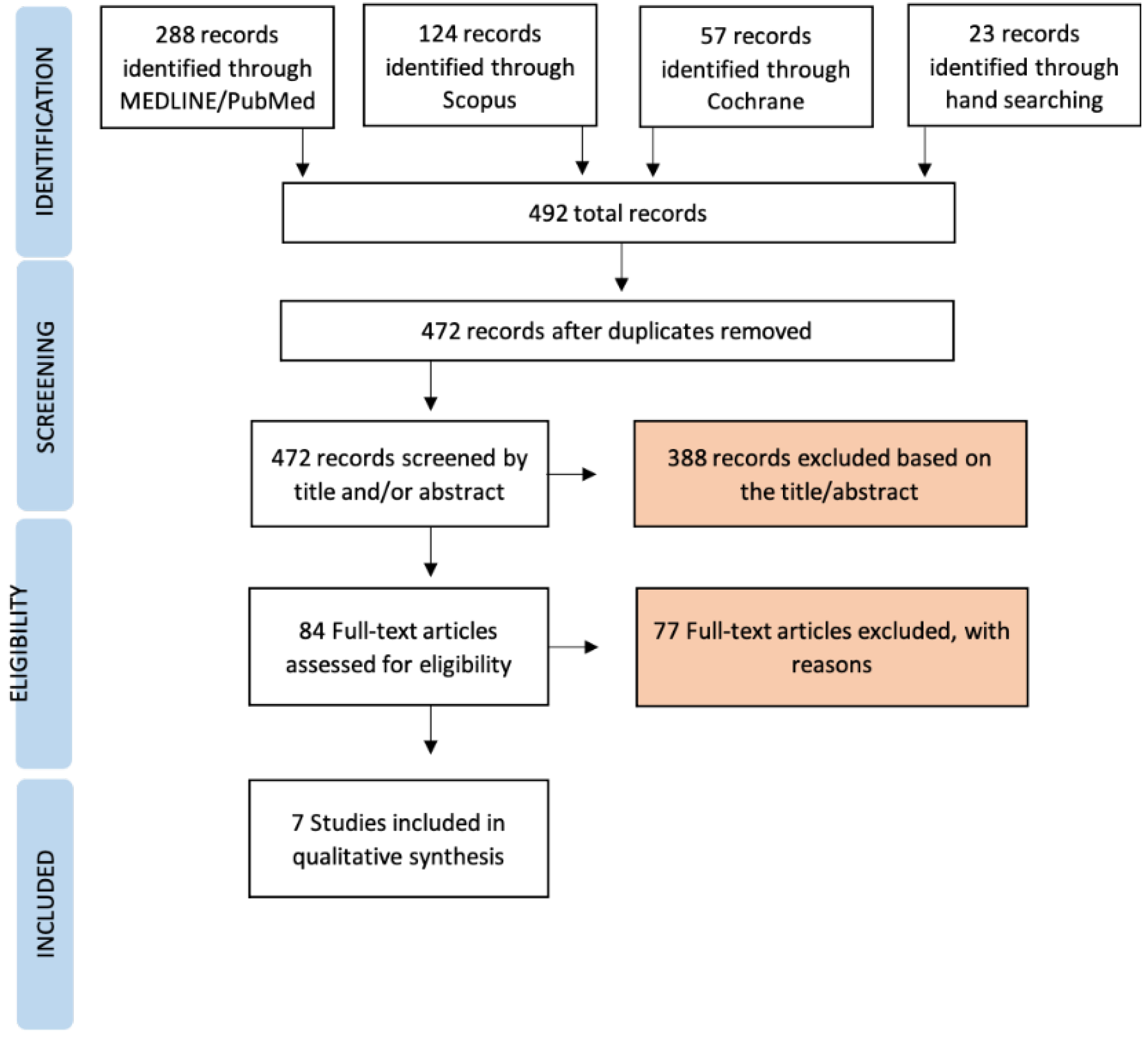
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Study Selection and Data Extraction
2.4. Quality Assessment
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Elani, H.W.; Starr, J.R.; Da Silva, J.D.; Gallucci, G.O. Trends in Dental Implant Use in the U.S., 1999–2016, and Projections to 2026. J. Dent. Res. 2018, 97, 1424–1430. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Bäumer, D.; Ozga, A.K.; Körner, G.; Bäumer, A. Patient satisfaction and oral health-related quality of life 10 years after implant placement. BMC Oral Health 2021, 21, 30. [Google Scholar] [CrossRef]
- Perea, C.; Del Río, J.; Preciado, A.; Lynch, C.D.; Celemín, A.; Castillo-Oyagüe, R. Validation of the ‘Quality of Life with Implant Prostheses (QoLIP-10)’ questionnaire for wearers of cement-retained implant-supported restorations. J. Dent. 2015, 43, 1021–1031. [Google Scholar] [CrossRef] [PubMed]
- Moraschini, V.; Poubel, L.A.D.C.; Ferreira, V.F.; Barboza, E.D.S.P. Evaluation of survival and success rates of dental implants reported in longitudinal studies with a follow-up period of at least 10 years: A systematic review. Int. J. Oral Maxillofac. Surg. 2015, 44, 377–388. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Z.; Ao, X.; Xie, P.; Jiang, F.; Chen, W. The biological width around implant. J. Prosthodont. Res. 2021, 65, 11–18. [Google Scholar] [CrossRef]
- Oh, T.-J.; Yoon, J.; Misch, C.E.; Wang, H.-L. The Causes of Early Implant Bone Loss: Myth or Science? J. Periodontol. 2002, 73, 322–333. [Google Scholar] [CrossRef]
- Bertolini, M.M.; Del Bel Cury, A.A.; Pizzoloto, L.; Acapa, I.R.H.; Shibli, J.A.; Bordin, D. Does traumatic occlusal forces lead to peri-implant bone loss? A systematic review. Braz. Oral Res. 2019, 33, e069. [Google Scholar] [CrossRef]
- Uribe, R.; Peñarrocha, M.; Sanchis, J.M.; García, O. Marginal peri-implantitis due to occlusal overload. A case report. Med. Oral 2004, 9, 160–162. [Google Scholar]
- Graves, C.V.; Harrel, S.K.; Rossmann, J.A.; Kerns, D.; Gonzalez, J.A.; Kontogiorgos, E.D.; Al-Hashimi, I.; Abraham, C. The Role of Occlusion in the Dental Implant and Peri-implant Condition: A Review. Open Dent. J. 2016, 10, 594–601. [Google Scholar] [CrossRef]
- Merin, R.L. Repair of peri-implant bone loss after occlusal adjustment: A case report. J. Am. Dent. Assoc. 2014, 145, 1058–1062. [Google Scholar] [CrossRef]
- Rangert, B.; Jemt, T.; Jörneus, L. Forces and moments on Branemark implants. Int. J. Oral Maxillofac. Implant. 1989, 4, 241–247. [Google Scholar]
- Misch, C.E.; Suzuki, J.B.; Misch-Dietsh, F.M.; Bidez, M.W. A positive correlation between occlusal trauma and peri-implant bone loss: Literature support. Implant Dent. 2005, 14, 108–116. [Google Scholar] [CrossRef] [PubMed]
- Adell, R.; Lekholm, U.; Rockler, B.; Brånemark, P.-I. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int. J. Oral Surg. 1981, 10, 387–416. [Google Scholar] [CrossRef]
- Van Steenberghe, D.; Naert, I.; Jacobs, R.; Quirynen, M. Influence of inflammatory reactions vs. occlusal loading on peri-implant marginal bone level. Adv. Dent. Res. 1999, 13, 130–135. [Google Scholar] [CrossRef] [PubMed]
- Quirynen, M.; Naert, I.; Van Steenberghe, D. Fixture design and overload influence marginal bone loss and future success in the Brånemark® system. Clin. Oral. Implants Res. 1992, 3, 104–111. [Google Scholar] [CrossRef] [PubMed]
- Manor, Y.; Oubaid, S.; Mardinger, O.; Chaushu, G.; Nissan, J. Characteristics of Early Versus Late Implant Failure: A Retrospective Study. J. Oral Maxillofac. Surg. 2009, 67, 2649–2652. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Zhao, B.; Deng, C.; Shang, D.; Zhang, C. Assessment of Implant Cumulative Survival Rates in Sites with Different Bone Density and Related Prognostic Factors: An 8-Year Retrospective Study of 2,684 Implants. Int. J. Oral Maxillofac. Implants 2015, 30, 360–371. [Google Scholar] [CrossRef]
- Vidyasagar, L.; Apse, P. Biological response to dental implant loading/overloading. Implant overloading: Empiricism or science. Stomatologija 2003, 5, 83–89. [Google Scholar]
- Kim, Y.; Oh, T.J.; Misch, C.E.; Wang, H.L. Occlusal considerations in implant therapy: Clinical guidelines with biomechanical rationale. Clin. Oral Implants Res. 2005, 16, 26–35. [Google Scholar] [CrossRef]
- Duyck, J.; Vandamme, K. The effect of loading on peri-implant bone: A critical review of the literature. J. Oral Rehabil. 2014, 41, 783–794. [Google Scholar] [CrossRef]
- Koyano, K.; Esaki, D. Occlusion on oral implants: Current clinical guidelines. J. Oral Rehabil. 2015, 42, 153–161. [Google Scholar] [CrossRef] [PubMed]
- Ayuso-Montero, R.; Mariano-Hernandez, Y.; Khoury-Ribas, L.; Rovira-Lastra, B.; Willaert, E.; Martinez- Gomis, J. Reliability and Validity of T-scan and 3D Intraoral Scanning for Measuring the Occlusal Contact Area. J. Prosthodont. 2020, 29, 19–25. [Google Scholar] [CrossRef]
- Shopova, D.; Bozhkova, T.; Yordanova, S.; Yordanova, M. Case Report: Digital analysis of occlusion with T-Scan Novus in occlusal splint treatment for a patient with bruxism. F1000Research 2021, 10, 915. [Google Scholar] [CrossRef] [PubMed]
- Gümüş, H.Ö.; Kılınç, H.İ.; Tuna, S.H.; Ozcan, N. Computerized analysis of occlusal contacts in bruxism patients treated with occlusal splint therapy. J. Adv. Prosthodont. 2013, 5, 256–261. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Miyata, T.; Kobayashi, Y.; Araki, H.; Ohto, T.; Shin, K. The influence of controlled occlusal overload on peri-implant tissue. Part 3: A histologic study in monkeys. Int. J. Oral Maxillofac. Implant. 2000, 15, 425–431. [Google Scholar]
- Isidor, F. Loss of osseointegration caused by occlusal load of oral implants: A clinical and radiographic study in monkeys. Clin. Oral Implants Res. 1996, 7, 143–152. [Google Scholar] [CrossRef] [PubMed]
- Duyck, J.; Naert, I.; Rønold, H.J.; Ellingsen, J.E.; Van Oosterwyck, H.; Vander Sloten, J. The influence of static and dynamic loading on marginal bone reactions around osseointegrated implants: An animal experimental study. Clin. Oral Implants Res. 2001, 12, 207–218. [Google Scholar] [CrossRef]
- Hürzeler, M.B.; Quiñones, C.R.; Kohal, R.J.; Rohde, M.; Strub, J.R.; Teuscher, U.; Caffesse, R.G. Changes in Peri-Implant Tissues Subjected to Orthodontic Forces and Ligature Breakdown in Monkeys. J. Periodontol. 1998, 69, 396–404. [Google Scholar] [CrossRef]
- Heitz-Mayfield, L.J.; Schmid, B.; Weigel, C.; Gerber, S.; Bosshardt, D.D.; Jönsson, J.; Lang, N.P.; Jönsson, J. Does excessive occlusal load affect osseointegration? An experimental study in the dog. Clin. Oral Implants Res. 2004, 15, 259–268. [Google Scholar] [CrossRef]
- Gotfredsen, K.; Berglundh, T.; Lindhe, J. Bone reactions adjacent to titanium implants subjected to static load: A study in the dog (I). Clin. Oral Implants Res. 2001, 12, 1–8. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 89. [Google Scholar]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savovic, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, 4–10. [Google Scholar] [CrossRef]
- Podaropoulos, L.; Veis, A.A.; Trisi, P.; Papadimitriou, S.; Alexandridis, C.; Kalyvas, D. Bone reactions around dental implants subjected to progressive static load: An experimental study in dogs. Clin. Oral Implants Res. 2016, 27, 910–917. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, D.S.; Piattelli, A.; Iezzi, G.; Faveri, M.; Rodrigues, J.A.; Shibli, J.A. Effect of lateral static load on immediately restored implants: Histologic and radiographic evaluation in dogs. Clin. Oral Implants Res. 2015, 26, e51–e56. [Google Scholar] [CrossRef] [PubMed]
- Nagasawa, M.; Takano, R.; Maeda, T.; Uoshima, K. Observation of the Bone Surrounding an Overloaded Implant in a Novel Rat Model. Int. J. Oral Maxillofac. Implants 2013, 28, 109–116. [Google Scholar] [CrossRef]
- Miyamoto, Y.; Koretake, K.; Hirata, M.; Kubo, T.; Akagawa, Y. Influence of static overload on the bony interface around implants in dogs. Int. J. Prosthodont. 2008, 21, 437–444. [Google Scholar]
- Kozlovsky, A.; Tal, H.; Laufer, B.Z.; Leshem, R.; Rohrer, M.D.; Weinreb, M.; Artzi, Z. Impact of implant overloading on the peri-implant bone in inflamed and non-inflamed peri-implant mucosa. Clin. Oral Implants Res. 2007, 18, 601–610. [Google Scholar] [CrossRef]
- Miyata, T.; Kobayashi, Y.; Araki, H.; Ohto, T.; Shin, K. The influence of controlled occlusal overload on peri-implant tissue. part 4: A histologic study in monkeys. Int. J. Oral Maxillofac. Implants 2002, 17, 384–390. [Google Scholar]
- Asikainen, P.; Klemettil, E.; Vuilleminz, T.; Sutter, F.; Rainio, V.; Kotilainen, R. Titanium implants and lateral forces. Clin. Oral Implants Res. 1997, 8, 465–468. [Google Scholar] [CrossRef]
- Isidor, F. Histological evaluation of peri-implant bone at implants subjected to occlusal overload or plaque accumulation. Clin. Oral Implants Res. 1997, 8, 1–9. [Google Scholar] [CrossRef]
- Hoshaw, S.J.; Brunski, J.B.; Cochran, G.V.B. Mechanical loading of brånemark implants affects interfacial bone modeling and remodeling. Int. J. Oral Maxillofac. Implants 1994, 9, 1–33. [Google Scholar]
- Ogiso, M.; Tabata, T.; Kuo, P.T.; Borghese, D. A histologic an occluded Prosthetics and Dental Implants comparison of the functional loading capacity of dense apatite implant and the natural dentition. J. Prosthet. Dent. 1994, 71, 581–588. [Google Scholar] [CrossRef]
- Podaropoulos, L.; Trisi, P.; Papadimitriou, S.; Lazzara, R.; Kalyvas, D. The Influence of Progressive Study in Dogs. Int. J. Oral Maxillofac. Implants 2020, 35, 25–38. [Google Scholar] [CrossRef] [PubMed]
- Lima, L.A.; Bosshardt, D.D.; Chambrone, L.; Araújo, M.G.; Lang, N.P. Excessive occlusal load on chemically modified and moderately rough titanium implants restored with cantilever reconstructions. An experimental study in dogs. Clin. Oral Implant. Res. 2019, 30, 1142–1154. [Google Scholar] [CrossRef]
- Piccinini, M.; Cugnoni, J.; Botsis, J.; Ammann, P.; Wiskott, A. Peri-implant bone adaptations to overloading in rat tibiae: Experimental investigations and numerical predictions. Clin. Oral Implant. Res. 2016, 27, 1444–1453. [Google Scholar] [CrossRef]
- Yagihara, A.; Kawasaki, R.; Mita, A.; Takakuda, K. Impact of Dynamic and Static Load on Bone Around Implants: An Experimental Study in a Rat Model. Int. J. Oral Maxillofac. Implant. 2016, 31, e49–e56. [Google Scholar] [CrossRef][Green Version]
- Maminskas, J.; Puisys, A.; Kuoppala, R.; Raustia, A.; Juodzbalys, G. The Prosthetic Influence and Biomechanics on Peri-Implant Strain: A Systematic Literature Review of Finite Element Studies. J. Oral Maxillofac. Res. 2016, 7, e4. [Google Scholar] [CrossRef]
- Afrashtehfar, K.I.; Afrashtehfar, C.D. Lack of association between overload and peri-implant tissue loss in healthy conditions. Evid. Based Dent. 2016, 17, 92–93. [Google Scholar] [CrossRef]
- Pellegrini, G.; Canullo, L.; Dellavia, C. Histological features of peri-implant bone subjected to overload. Ann. Anat.-Anat. Anz. 2016, 206, 57–63. [Google Scholar] [CrossRef]
- Chang, M.; Chronopoulos, V.; Mattheos, N. Impact of excessive occlusal load on successfully-osseointegrated dental implants: A literature review. J. Investig. Clin. Dent. 2013, 4, 142–150. [Google Scholar] [CrossRef]
- Rungruanganunt, P.; Taylor, T.D.; Eckert, S.E.; Karl, M. The effect of static load on dental implant survival: A systematic review. Int. J. Oral Maxillofac. Implants 2013, 28, 1218–1225. [Google Scholar] [CrossRef] [PubMed]
- Naert, I.; Duyck, J.; Vandamme, K. Occlusal overload and bone/implant loss. Clin. Oral Implants Res. 2012, 23 (Suppl. S6), 95–107. [Google Scholar] [CrossRef] [PubMed]
- Sakka, S.; Baroudi, K.; Nassani, M.Z. Factors associated with early and late failure of dental implants. J. Investig. Clin. Dent. 2012, 3, 258–261. [Google Scholar] [CrossRef] [PubMed]
- Hsu, Y.-T.; Fu, J.-H.; Al-Hezaimi, K.; Wang, H.-L. Biomechanical implant treatment complications: A systematic review of clinical studies of implants with at least 1 year of functional loading. Int. J. Oral Maxillofac. Implants 2012, 27, 894–904. [Google Scholar]
- Chambrone, L.; Chambrone, L.A.; Lima, L.A. Effects of Occlusal Overload on Peri-Implant Tissue Health: A Systematic Review of Animal-Model Studies. J. Periodontol. 2010, 81, 1367–1378. [Google Scholar] [CrossRef]
- Dănilă, V.; Augustin, M. Occlusal overload--a risk factor in implant based prostheses. Rev. Med. Chir. Soc. Med. Nat. Iasi. 2010, 114, 214–217. [Google Scholar]
- Rilo, B.; da Silva, J.L.; Mora, M.J.; Santana, U. Guidelines for occlusion strategy in implant-borne prostheses. A review. Int. Dent. J. 2008, 58, 139–145. [Google Scholar] [CrossRef]
- Hui, F.J.; Yap, A.U.J. Occlusion and periodontal disease—Where is the link? Singapore Dent. J. 2007, 29, 22–23. [Google Scholar]
- Lobbezoo, F.; Brouwers, J.; Cune, M.; Naeije, M. Dental implants in patients with bruxing habits. J. Oral Rehabil. 2006, 33, 152–159. [Google Scholar] [CrossRef]
- Isidor, F. Influence of forces on peri-implant bone. Clin. Oral Implants Res. 2006, 17 (Suppl. S2), 8–18. [Google Scholar] [CrossRef]
- Saadoun, A.P.; Le Gall, M.; Kricheck, M. Microbial infections and occlusal overload: Causes of failure in osseointegrated implants. Pract. Periodontics Aesthet. Dent. 1993, 5, 11–20. [Google Scholar]
- Zandim-Barcelos, D.L.; Carvalho, G.G.; De Sapata, V.M.; Villar, C.C.; Hämmerle, C.; Romito, G.A. Implant-based factor as possible risk for peri-implantitis. Braz. Oral Res. 2019, 33 (Suppl. S1), e067. [Google Scholar] [CrossRef] [PubMed]
- Sadowsky, S.J. Occlusal overload with dental implants: A review. Int. J. Implant Dent. 2019, 5, 29. [Google Scholar] [CrossRef] [PubMed]
- Naveau, A.; Shinmyouzu, K.; Moore, C.; Avivi-Arber, L.; Jokerst, J.; Koka, S. Etiology and Measurement of Peri-Implant Crestal Bone Loss (CBL). J. Clin. Med. 2019, 8, 166. [Google Scholar] [CrossRef] [PubMed]
- Nuţu, E. Role of initial density distribution in simulations of bone remodeling around dental implants. Acta Bioeng. Biomech. 2018, 20, 23–31. [Google Scholar]
- Eazhil, R.; Swaminathan, S.V.; Gunaseelan, M.; Kannan, G.V.; Alagesan, C. Impact of implant diameter and length on stress distribution in osseointegrated implants: A 3D FEA study. J. Int. Soc. Prev. Community Dent. 2016, 6, 590–596. [Google Scholar] [CrossRef]
- Baggi, L.; Pastore, S.; Di Girolamo, M.; Vairo, G. Implant-bone load transfer mechanisms in complete-arch prostheses supported by four implants: A three-dimensional finite element approach. J. Prosthet. Dent. 2013, 109, 9–21. [Google Scholar] [CrossRef]
- Baggi, L.; Cappelloni, I.; Di Girolamo, M.; Maceri, F.; Vairo, G. The influence of implant diameter and length on stress distribution of osseointegrated implants related to crestal bone geometry: A three-dimensional finite element analysis. J. Prosthet. Dent. 2008, 100, 422–431. [Google Scholar] [CrossRef]
- Kitamura, E.; Stegaroiu, R.; Nomura, S.; Miyakawa, O. Influence of marginal bone resorption on stress around an implant—A three-dimensional finite element analysis. J. Oral Rehabil. 2005, 32, 279–286. [Google Scholar] [CrossRef]
- Crupi, V.; Guglielmino, E.; La Rosa, G.; Vander Sloten, J.; Van Oosterwyck, H. Numerical analysis of bone adaptation around an oral implant due to overload stress. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2004, 218, 407–415. [Google Scholar] [CrossRef]
- Watanabe, F.; Hata, Y.; Komatsu, S.; Ramos, T.C.; Fukuda, H. Finite element analysis of the influence of implant inclination, loading position, and load direction on stress distribution. Odontology 2003, 91, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Akça, K.; Iplikçioğlu, H. Finite element stress analysis of the influence of staggered versus straight placement of dental implants. Int. J. Oral Maxillofac. Implants 2001, 16, 722–730. [Google Scholar] [PubMed]
- O’Mahony, A.; Bowles, Q.; Woolsey, G.; Robinson, S.J.; Spencer, P. Stress distribution in the single-unit osseointegrated dental implant: Finite element analyses of axial and off-axial loading. Implant Dent. 2000, 9, 207–218. [Google Scholar] [CrossRef] [PubMed]
- Papavasiliou, G.; Kamposiora, P.; Bayne, S.C.; Felton, D.A. Three-dimensional finite elemente analysis of stress-distribution around single tooth implants as a function of bony support, prosthesis type, and loading durinf function. J. Prosthet. Dent. 1996, 76, 633–640. [Google Scholar] [CrossRef]
- Chang, C.-L.; Chen, C.-S.; Yeung, T.C.; Hsu, M.-L. Biomechanical effect of a zirconia dental implant-crown system: A three-dimensional finite element analysis. Int. J. Oral Maxillofac. Implant 2012, 27, e49–e57. [Google Scholar]
- Sridhar, S.; Wang, F.; Wilson, T.G.G.; Palmer, K.; Valderrama, P.; Rodrigues, D.C. The role of bacterial biofilm and mechanical forces in modulating dental implant failures. J. Mech. Behav. Biomed. Mater. 2019, 92, 118–127. [Google Scholar] [CrossRef]
- Kan, J.P.M.; Judge, R.B.; Palamara, J.E.A. In vitro bone strain analysis of implant following occlusal overload. Clin. Oral Implants Res. 2014, 25, e73–e82. [Google Scholar] [CrossRef]
- Nakashima, T.; Hayashi, M.; Fukunaga, T.; Kurata, K.; Oh-Hora, M.; Feng, J.Q.; Bonewald, L.F.; Kodama, T.; Wutz, A.; Wagner, E.F.; et al. Evidence for osteocyte regulation of bone homeostasis through RANKL expression. Nat. Med. 2011, 17, 1231–1234. [Google Scholar] [CrossRef]
- Sheridan, R.A.; Decker, A.M.; Plonka, A.B.; Wang, H.-L. The Role of Occlusion in Implant Therapy: A Comprehensive Updated Review. Implant Dent. 2016, 25, 829–838. [Google Scholar] [CrossRef]
- Hosokawa, R. Significance of occlusion for dental implant treatment. Clinical evidence of occlusion as a risk factor. Nihon Hotetsu Shika Gakkai Zasshi 2008, 52, 25–30. [Google Scholar] [CrossRef][Green Version]
- Passanezi, E.; Sant’Ana, A.C.P.; Damante, C.A. Occlusal trauma and mucositis or peri-implantitis? J. Am. Dent. Assoc. 2017, 148, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Mattheos, N.; Janda, M.S.; Zampelis, A.; Chronopoulos, V. Reversible, Non-plaque-induced loss of osseointegration of successfully loaded dental implants. Clin. Oral Implants Res. 2013, 24, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Tawil, G. Peri-implant bone loss caused by occlusal overload: Repair of the peri-implant defect following correction of the traumatic occlusion. A case report. Int. J. Oral Maxillofac. Implant. 2008, 23, 153–157. [Google Scholar]
- Uribe, R.; Peñarrocha, M.; Sanchis, J.M.; García, O. Periimplantitis marginal por sobrecarga oclusal. A propósito de un caso Marginal peri-implantitis due to occlusal overload. A case. Med. Oral Organo Of. Soc. Esp. Med. Oral. Acad. Iberoam. Patol. Med. Bucal 2004, 9, 159–162. [Google Scholar]
- Leung, K.C.M.; Chow, T.W.; Wat, P.Y.P.; Comfort, M.B. Peri-implant Bone Loss: Management of a Patient. Int. J. Oral Maxillofac. Implant 2001, 16, 273–277. [Google Scholar]
- Rosenberg, E.S.; Torosian, J.P.; Slots, J. Microbial differences in 2 clinically distinct types of failures of osseointegrated implants. Clin. Oral Implants Res. 1991, 2, 135–144. [Google Scholar] [CrossRef]
- Jofré, J.; Hamada, T.; Nishimura, M.; Klattenhoff, C. The effect of maximum bite force on marginal bone loss of mini-implants supporting a mandibular overdenture: A randomized controlled trial. Clin. Oral Implants Res. 2010, 21, 243–249. [Google Scholar] [CrossRef] [PubMed]
- Naert, I.; Quirynen, M.; van Steenberghe, D.; Darius, P. A study of 589 consecutive implants supporting complete fixed prostheses. Part II: Prosthetic aspects. J. Prosthet. Dent. 1992, 68, 949–956. [Google Scholar] [CrossRef]
- Chitumalla, R.; Kumari, K.H.; Mohapatra, A.; Parihar, A.S.; Anand, K.S.; Katragadda, P. Assessment of survival rate of dental implants in patients with bruxism: A 5-year retrospective study. Contemp. Clin. Dent. 2018, 9, S278–S282. [Google Scholar] [CrossRef]
- Han, H.-J.; Kim, S.; Han, D.-H. Multifactorial Evaluation of Implant Failure: A 19-year Retrospective Study. Int. J. Oral Maxillofac. Implants 2014, 29, 303–310. [Google Scholar] [CrossRef]
- Becker, C.M. Cantilever fixed prostheses utilizing dental implants: A 10-year retrospective analysis. Quintessence Int. 2004, 35, 437–441. [Google Scholar] [PubMed]
- Lindquist, L.W.; Rockler, B.; Carlsson, G.E. Bone resorption around fixtures in edentulous patients treated with mandibular fixed tissue-integrated prostheses. J. Prosthet. Dent. 1988, 59, 59–63. [Google Scholar] [CrossRef]
- Lindquist, L.W.; Carlsson, G.E.; Jemt, T. A prospective 15-year follow-up study of mandibular fixed prostheses supported by osseointegrated implants: Clinical results and marginal bone loss. Clin. Oral Implants Res. 1996, 7, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Carlsson, G.E.; Lindquist, L.W.; Jemt, T. Long-term marginal periimplant bone loss in edentulous patients. Int. J. Prosthodont. 2000, 13, 295–302. [Google Scholar] [PubMed]
- Engel, E.; Gomez-Roman, G.; Axmann-Krcmar, D. Effect of occlusal wear on bone loss and Periotest value of dental implants. Int. J. Prosthodont. 2001, 14, 444–450. [Google Scholar]
- Dalago, H.R.; Schuldt Filho, G.; Rodrigues, M.A.P.; Renvert, S.; Bianchini, M.A. Risk indicators for Peri-implantitis. A cross-sectional study with 916 implants. Clin. Oral Implant. Res. 2017, 28, 144–150. [Google Scholar] [CrossRef]
- Kissa, J.; El Kholti, W.; Chemlali, S.; Kawtari, H.; Laalou, Y.; Albandar, J.M. Prevalence and risk indicators of peri-implant diseases in a group of Moroccan patients. J. Periodontol. 2021, 92, 1096–1106. [Google Scholar] [CrossRef]
- Canullo, L.; Tallarico, M.; Radovanovic, S.; Delibasic, B.; Covani, U.; Rakic, M. Distinguishing predictive profiles for patient-based risk assessment and diagnostics of plaque induced, surgically and prosthetically triggered peri-implantitis. Clin. Oral Implants Res. 2016, 27, 1243–1250. [Google Scholar] [CrossRef]
- Sadowsky, S.J. Mandibular implant-retained overdentures: A literature review. J. Prosthet. Dent. 2001, 86, 468–473. [Google Scholar] [CrossRef]
- Sadowsky, S.J. Treatment considerations for maxillary implant overdentures: A systematic review. J. Prosthet. Dent. 2007, 97, 340–348. [Google Scholar] [CrossRef]
- Klemetti, E. Is there a certain number of implants needed to retain an overdenture? J. Oral Rehabil. 2008, 35, 80–84. [Google Scholar] [CrossRef] [PubMed]
- Nicolae, V.; Chiscop, I.; Cioranu, V.S.I.; Martu, M.A.; Luchian, A.I.; Martu, S.; Solomon, S.M. The use of photoactivated blue-o toluidine for periimplantitis treatment in patients with periodontal disease. Rev. Chim. (Buchar.) 2015, 66, 2121–2123. [Google Scholar]
- Kerstein, R.B.; Radke, J. Clinician accuracy when subjectively interpreting articulating paper markings. Cranio 2014, 32, 13–23. [Google Scholar] [CrossRef] [PubMed]
- Cenkoglu, B.G.; Balcioglu, N.B.; Ozdemir, T.; Mijiritsky, E. The Effect of the Length and Distribution of Implants for Fixed Prosthetic Reconstructions in the Atrophic Posterior Maxilla: A Finite Element Analysis. Materials 2019, 12, 2556. [Google Scholar] [CrossRef]
- Farronato, D.; Manfredini, M.; Stevanello, A.; Campana, V.; Azzi, L.; Farronato, M. A Comparative 3D Finite Element Computational Study of Three Connections. Materials 2019, 12, 3135. [Google Scholar] [CrossRef]
- Brune, A.; Stiesch, M.; Eisenburger, M.; Greuling, A. The effect of different occlusal contact situations on peri-implant bone stress—A contact finite element analysis of indirect axial loading. Mater. Sci. Eng. 2019, 99, 367–373. [Google Scholar] [CrossRef]
| Author(s), Year | Study Design | Total No. of Patients | Total No. of Implants | No. of Compromized Implants | Implant Diameter and Length [mm] § | Other Implant Features * | Type of Prosthesis | Follow-up (Range or ±SD) [Years] ° | Occlusal Analysis | Correlation Overload–Cretal Bone Loss (Y/N) |
|---|---|---|---|---|---|---|---|---|---|---|
| Canullo et al., 2016 [98] | Retrospective case-control study | 56 | 332 | 125 | D < 4: 26 D = 4: 279 D > 4: 27 L not reported | Peri-implantitis group: Rough (n = 85) Smooth (n = 40) | Healthy implant group: Screwed (n = 127) Cemented (n = 80) Peri-implantitis group: Screwed (n = 64) Cemented (n = 61) | Healthy implant group: 6.48 ± 3.57 Peri-implantitis group: 5.94 ± 3.16 | Fracture or chipping of the veneering; loss of retention; dynamic occlusal measurement by T-Scan III; occlusal photographs | Y ** |
| Carlsson et al., 2000 [94] | Prospective cohort study | 47 (of which 13 received treatment in both jaws) | 343 (273 mandible; 75 maxilla) | 8 (7 before loading) | D not reported L = 10 mm | Standard Brånemark implants (Nobel Biocare) | Full-arch implant-supported FDP (resin teeth) | 15 (mandibular implants) 10.5 (8 to 13; maxillary implants) | Occlusal wear; bite force | N |
| Dalago et al., 2017 [96] | Retrospective cross-sectional study | 183 | 938 | 89 (16 lost; 6 inactivated; 67 peri-implantitis) | D < 3.5 (n = 148) D = 3.5 (n = 575) D > 3.5 (n = 193) L < 9 (n = 796) L ≥ 9 (n = 120) | Connection: External Hexagon (n = 400) Internal Hexagon (n = 516) | Fixed restoration: Screwed (n = 436) Cemented (n = 480) Type of prosthesis: Single (n = 167) Partial (n = 522) Total (n = 227) | Mean: 5.64 (range 1 to 14) | Coronal fracture; wear facets | Y ** |
| Engel et al., 2001 [95] | Prospective cohort study | 379 | 379 | 21 | D = 3.5 (n = 44) D = 3.5–4 (n = 153) D = 4.5–7 (n = 182) L not reported | Frialit-2 (n = 227) Bonefit (n = 51) IMZ (n = 47) Tübingen (n = 47) Brånemark (n = 6) TPS (n = 1) | Type of prostheses: Single (n = 188) Partial (n = 84) Overdenture (n = 107) Occlusal material: Ceramic (n = 182) Non-ceramic (n = 197) | Mean: 6 (range 1 to 10) | Wear facets | N |
| Lindquist et al., 1988 [92] | Prospective cohort study | 46 25 (group 1) 21 (group 2) | 276 | N/A | Not reported | Brånemark implants | Mandibular full-arch implant-supported FDP | Group 1: 5½ to 6 Group 2: 3 to 4 | Bite force; attrition and occlusal wear | Y |
| Lindquist et al., 1996 [93] | Prospective cohort study | 47 26 (group 1) 21 (group 2) | 273 | 3 | Not reported | Brånemark implants | Mandibular full-arch implant-supported FDP Mean cantilever length left = 14.7 mm (7 to 20) Mean cantilever length right= 15 mm (7 to 20) | Group 1: 15 Group 2: 10 | Bite force; attrition and occlusal wear | N |
| Kissa et al., 2020 [97] | Retrospective cross-sectional study | 145 | 642 | 146 | Not reported | SA (n = 221) SLA (n = 161) HA (n = 260) | Fixed restoration: Screwed (n = 436) Cemented (n = 480) | Mean: 6.4 (1 to 16) (1 to 3: 242) (4 to 8: 226) (>8: 174) | Occlusal wear | Y |
| Study | Pre-Intervention | At Intervention | Post-Intervention | Overall Risk of Bias | ||||
|---|---|---|---|---|---|---|---|---|
| Confounding | Selection | Classification of Intervention | Deviation from Intended Intervention | Missing Data | Measurement of Outcome | Reporting Result | ||
| Canullo et al., 2016 [98] | L | M | L | N/A | L | L | L | M |
| Carlsson et al., 2000 [94] | L | L | M | N/A | L | M | S | S |
| Dalago et al., 2017 [96] | L | M | M | N/A | L | L | L | M |
| Engel et al., 2001 [95] | L | L | M | N/A | S | M | M | S |
| Lindquist et al., 1988 [92] | L | L | M | N/A | L | M | S | S |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Fiore, A.; Montagner, M.; Sivolella, S.; Stellini, E.; Yilmaz, B.; Brunello, G. Peri-Implant Bone Loss and Overload: A Systematic Review Focusing on Occlusal Analysis through Digital and Analogic Methods. J. Clin. Med. 2022, 11, 4812. https://doi.org/10.3390/jcm11164812
Di Fiore A, Montagner M, Sivolella S, Stellini E, Yilmaz B, Brunello G. Peri-Implant Bone Loss and Overload: A Systematic Review Focusing on Occlusal Analysis through Digital and Analogic Methods. Journal of Clinical Medicine. 2022; 11(16):4812. https://doi.org/10.3390/jcm11164812
Chicago/Turabian StyleDi Fiore, Adolfo, Mattia Montagner, Stefano Sivolella, Edoardo Stellini, Burak Yilmaz, and Giulia Brunello. 2022. "Peri-Implant Bone Loss and Overload: A Systematic Review Focusing on Occlusal Analysis through Digital and Analogic Methods" Journal of Clinical Medicine 11, no. 16: 4812. https://doi.org/10.3390/jcm11164812
APA StyleDi Fiore, A., Montagner, M., Sivolella, S., Stellini, E., Yilmaz, B., & Brunello, G. (2022). Peri-Implant Bone Loss and Overload: A Systematic Review Focusing on Occlusal Analysis through Digital and Analogic Methods. Journal of Clinical Medicine, 11(16), 4812. https://doi.org/10.3390/jcm11164812








