Investigating the Prediction Accuracy of Recently Updated Intraocular Lens Power Formulas with Artificial Intelligence for High Myopia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Institutions and Institutional Review Board Approval
2.2. Participants
2.3. IOL Power Calculation
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Haigis, W. Intraocular lens calculation in extreme myopia. J. Cataract Refract. Surg. 2009, 35, 906–911. [Google Scholar] [CrossRef] [PubMed]
- Melles, R.B.; Holladay, J.T.; Chang, W.J. Accuracy of Intraocular Lens Calculation Formulas. Ophthalmology 2018, 125, 169–178. [Google Scholar] [CrossRef] [PubMed]
- Dolgin, E. The myopia boom. Nature 2015, 519, 276–278. [Google Scholar] [CrossRef] [PubMed]
- Morgan, I.G.; French, A.N.; Ashby, R.S.; Guo, X.; Ding, X.; He, M.; Rose, K.A. The epidemics of myopia: Aetiology and prevention. Prog. Retin. Eye Res. 2018, 62, 134–149. [Google Scholar] [CrossRef]
- Morgan, I.G.; Ohno-Matsui, K.; Saw, S.-M. Myopia. Lancet 2012, 379, 1739–1748. [Google Scholar] [CrossRef]
- Ji, J.; Liu, Y.; Zhang, J. Comparison of six methods for the intraocular lens power calculation in high myopic eyes. Eur. J. Ophthalmol. 2021, 31, 96–102. [Google Scholar] [CrossRef]
- Liu, J.; Wang, L.; Chai, F.; Han, Y.; Qian, S.; Koch, D.D.; Weikert, M.P. Comparison of intraocular lens power calculation formulas in Chinese eyes with axial myopia. J. Cataract Refract. Surg. 2019, 45, 725–731. [Google Scholar] [CrossRef]
- Omoto, M.K.; Torii, H.; Hayashi, K.; Ayaki, M.; Tsubota, K.; Negishi, K. Ratio of Axial Length to Corneal Radius in Japanese Patients and Accuracy of Intraocular Lens Power Calculation Based on Biometric Data. Am. J. Ophthalmol. 2020, 218, 320–329. [Google Scholar] [CrossRef]
- Omoto, M.K.; Torii, H.; Masui, S.; Ayaki, M.; Tsubota, K.; Negishi, K. Ocular biometry and refractive outcomes using two swept-source optical coherence tomography-based biometers with segmental or equivalent refractive indices. Sci. Rep. 2019, 9, 6557. [Google Scholar] [CrossRef]
- Wang, L.; Holladay, J.T.; Koch, D.D. Wang-Koch axial length adjustment for the Holladay 2 formula in long eyes. J. Cataract Refract. Surg. 2018, 44, 1291–1292. [Google Scholar] [CrossRef]
- Wang, L.; Shirayama, M.; Ma, X.J.; Kohnen, T.; Koch, D.D. Optimizing intraocular lens power calculations in eyes with axial lengths above 25.0 mm. J. Cataract Refract. Surg. 2011, 37, 2018–2027. [Google Scholar] [CrossRef] [PubMed]
- Warren, E.H. Hill-RBF Calculator Version 3.0. Available online: http://rbfcalculator.com/online/index.html (accessed on 1 May 2022).
- Tsessler, M.; Cohen, S.; Wang, L.; Koch, D.D.; Zadok, D.; Abulafia, A. Evaluating the prediction accuracy of the Hill-RBF 3.0 formula using a heteroscedastic statistical method. J. Cataract Refract. Surg. 2021, 48, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Melles, R.B.; Kane, J.X.; Olsen, T.; Chang, W.J. Update on Intraocular Lens Calculation Formulas. Ophthalmology 2019, 126, 1334–1335. [Google Scholar] [CrossRef] [PubMed]
- Bernardes, J.; Raimundo, M.; Lobo, C.; Murta, J.N. A Comparison of Intraocular Lens Power Calculation Formulas in High Myopia. J. Refract Surg. 2021, 37, 207–211. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.; Wang, L.; Kane, J.X.; Li, J.; Liu, L.; Wu, M. Accuracy of Artificial Intelligence Formulas and Axial Length Adjustments for Highly Myopic Eyes. Am. J. Ophthalmol. 2021, 223, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Mo, E.; Lin, L.; Wang, J.; Huo, Q.; Yang, Q.; Liu, E.; Zhang, L.; Yu, Y.; Ye, L.; Pan, A.; et al. Clinical Accuracy of 6 Intraocular Lens Power Calculation Formulas in Elongated Eyes, According to Anterior Chamber Depth. Am. J. Ophthalmol. 2021, 233, 153–162. [Google Scholar] [CrossRef]
- Popovic, M.; Schlenker, M.B.; Campos-Moller, X.; Pereira, A.; Ahmed, I.I.K. Wang-Koch formula for optimization of intraocular lens power calculation: Evaluation at a Canadian center. J. Cataract Refract. Surg. 2018, 44, 17–22. [Google Scholar] [CrossRef]
- Wang, L.; Koch, D.D. Modified axial length adjustment formulas in long eyes. J. Cataract Refract. Surg. 2018, 44, 1396–1397. [Google Scholar] [CrossRef]
- Kane, J.X.; Chang, D.F. Intraocular Lens Power Formulas, Biometry, and Intraoperative Aberrometry: A Review. Ophthalmology 2021, 128, e94–e114. [Google Scholar] [CrossRef]
- Kane, J.X.; Van Heerden, A.; Atik, A.; Petsoglou, C. Accuracy of 3 new methods for intraocular lens power selection. J. Cataract Refract. Surg. 2017, 43, 333–339. [Google Scholar] [CrossRef]
- Shajari, M.; Kolb, C.M.; Petermann, K.; Böhm, M.; Herzog, M.; de’Lorenzo, N.; Schönbrunn, S.; Kohnen, T. Comparison of 9 modern intraocular lens power calculation formulas for a quadrifocal intraocular lens. J. Cataract Refract. Surg. 2018, 44, 942–948. [Google Scholar] [CrossRef] [PubMed]
- Hoffer, K.J.; Savini, G. Update on Intraocular Lens Power Calculation Study Protocols: The Better Way to Design and Report Clinical Trials. Ophthalmology 2021, 128, e115–e120. [Google Scholar] [CrossRef] [PubMed]

| Variables | Values |
|---|---|
| Number of eyes | 70 eyes of 70 patients |
| Right/left | 33/37 |
| Male/female | 38/32 |
| Age at the surgery (years) | 64.0 ± 9.0 |
| Best corrected visual acuity (logMAR) | 0.14 ± 0.26 |
| Spherical equivalent (D) | −9.73 ± 4.40 |
| Target refraction (D) | −1.79 ± 1.15 |
| Axial length (mm) | 27.84 ± 1.34 |
| Keratometry (D) | 54.3 ± 24.9 |
| Anterior chamber depth (mm) | 3.45 ± 0.35 |
| Lens thickness (mm) | 4.45 ± 0.37 |
| Central corneal thickness (μm) | 556 ± 38 |
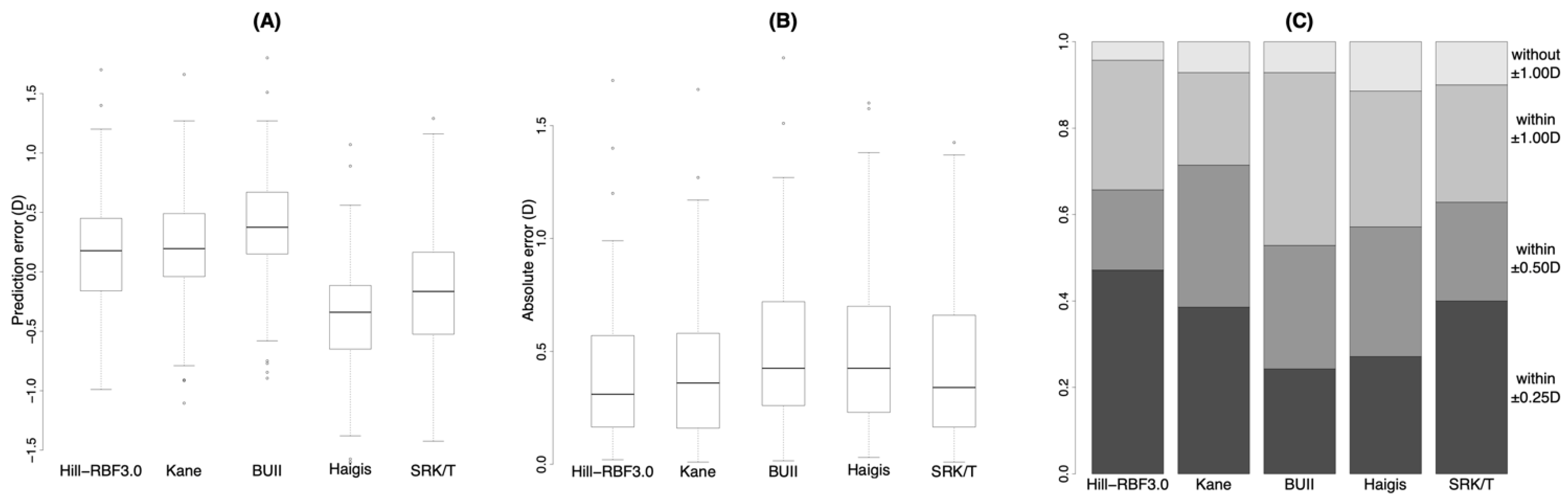
| Hill-RBF3.0 | Kane | BUII | Haigis | SRK/T | p-Value | ||
|---|---|---|---|---|---|---|---|
| Prediction error (D) | Mean ± SD | 0.17 ± 0.52 | 0.19 ± 0.51 | 0.36 ± 0.51 | −0.38 ± 0.52 | −0.18 ± 0.58 | <0.001 * |
| Median | 0.18 | 0.2 | 0.38 †,‡ | −0.34 †,‡,§ | −0.16 †,‡,§,‖ | ||
| Absolute error (D) | Mean ± SD | 0.42 ± 0.34 | 0.42 ± 0.34 | 0.51 ± 0.35 | 0.52 ± 0.38 | 0.46 ± 0.38 | <0.001 * |
| Median | 0.31 | 0.36 | 0.42 †‡ | 0.42 | 0.34 | ||
| Percentage (%) | Within ±0.25 D | 47.1 | 38.6 | 24.3 † | 27.1 | 40.0 | 0.015 * |
| Within ±0.50 D | 65.7 | 71.4 | 52.9 | 57.1 | 62.9 | 0.068 | |
| Within ±1.00 D | 95.7 | 92.9 | 92.9 | 88.6 | 90.0 | 0.28 |
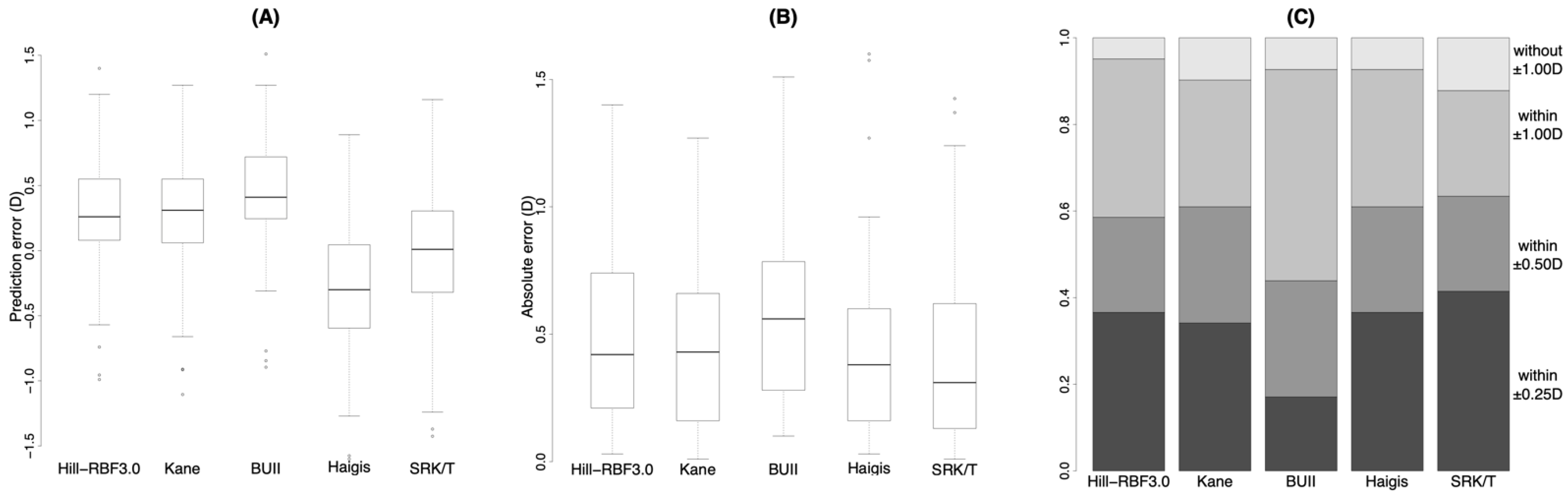
| Hill-RBF3.0 | Kane | BUII | Haigis | SRK/T | p-Value | ||
|---|---|---|---|---|---|---|---|
| Prediction error (D) | Mean ± SD | 0.02 ± 0.48 | 0.10 ± 0.49 | 0.26 ± 0.50 | −0.50 ± 0.50 | −0.34 ± 0.49 | <0.001 * |
| Median | −0.04 | 0.14 † | 0.32 †,‡ | −0.43 †,‡,§ | −0.34 †,‡,§,‖ | ||
| Absolute error (D) | Mean ± SD | 0.33 ± 0.34 | 0.36 ± 0.34 | 0.43 ± 0.36 | 0.6 ± 0.36 | 0.48 ± 0.35 | 0.0015 * |
| Median | 0.20 | 0.30 | 0.42 | 0.50 † | 0.37 ‖ | ||
| Percentage (%) | Within ± 0.25 D | 62.1 | 44.8 | 34.5 | 13.8 † | 37.9 | 0.0029 * |
| Within ± 0.50 D | 75.9 | 86.2 | 65.5 | 51.7 | 62.1 | 0.012 * | |
| Within ± 1.00 D | 96.6 | 96.6 | 93.1 | 82.8 | 93.1 | 0.044 * |
| Hill-RBF3.0 | Kane | BUII | Haigis | SRK/T | p-Value | ||
|---|---|---|---|---|---|---|---|
| Prediction error (D) | Mean ± SD | 0.27 ± 0.53 | 0.25 ± 0.52 | 0.42 ± 0.50 | −0.3 ± 0.52 | −0.06 ± 0.61 | <0.001 * |
| Median | 0.26 | 0.31 | 0.41 †,‡ | −0.3 †,‡,§ | 0.01 †,‡,§,‖ | ||
| Absolute error (D) | Mean ± SD | 0.49 ± 0.33 | 0.46 ± 0.34 | 0.57 ± 0.33 | 0.46 ± 0.38 | 0.45 ± 0.40 | 0.0017 * |
| Median | 0.42 | 0.43 | 0.56 †,‡ | 0.38 | 0.31 | ||
| Percentage (%) | Within ±0.25 D | 36.6 | 34.1 | 17.1 | 36.6 | 41.5 | 0.12 |
| Within ±0.50 D | 58.5 | 61.0 | 43.9 | 61.0 | 63.4 | 0.22 | |
| Within ±1.00 D | 95.1 | 90.2 | 92.7 | 92.7 | 87.8 | 0.60 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Omoto, M.; Sugawara, K.; Torii, H.; Yotsukura, E.; Masui, S.; Shigeno, Y.; Nishi, Y.; Negishi, K. Investigating the Prediction Accuracy of Recently Updated Intraocular Lens Power Formulas with Artificial Intelligence for High Myopia. J. Clin. Med. 2022, 11, 4848. https://doi.org/10.3390/jcm11164848
Omoto M, Sugawara K, Torii H, Yotsukura E, Masui S, Shigeno Y, Nishi Y, Negishi K. Investigating the Prediction Accuracy of Recently Updated Intraocular Lens Power Formulas with Artificial Intelligence for High Myopia. Journal of Clinical Medicine. 2022; 11(16):4848. https://doi.org/10.3390/jcm11164848
Chicago/Turabian StyleOmoto, Miki, Kaoruko Sugawara, Hidemasa Torii, Erisa Yotsukura, Sachiko Masui, Yuta Shigeno, Yasuyo Nishi, and Kazuno Negishi. 2022. "Investigating the Prediction Accuracy of Recently Updated Intraocular Lens Power Formulas with Artificial Intelligence for High Myopia" Journal of Clinical Medicine 11, no. 16: 4848. https://doi.org/10.3390/jcm11164848
APA StyleOmoto, M., Sugawara, K., Torii, H., Yotsukura, E., Masui, S., Shigeno, Y., Nishi, Y., & Negishi, K. (2022). Investigating the Prediction Accuracy of Recently Updated Intraocular Lens Power Formulas with Artificial Intelligence for High Myopia. Journal of Clinical Medicine, 11(16), 4848. https://doi.org/10.3390/jcm11164848








