Associations between Abdominal Trunk Muscle Weakness and Future Osteoporotic Vertebral Fracture in Middle-Aged and Older Adult Women: A Three-Year Prospective Longitudinal Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics Statement
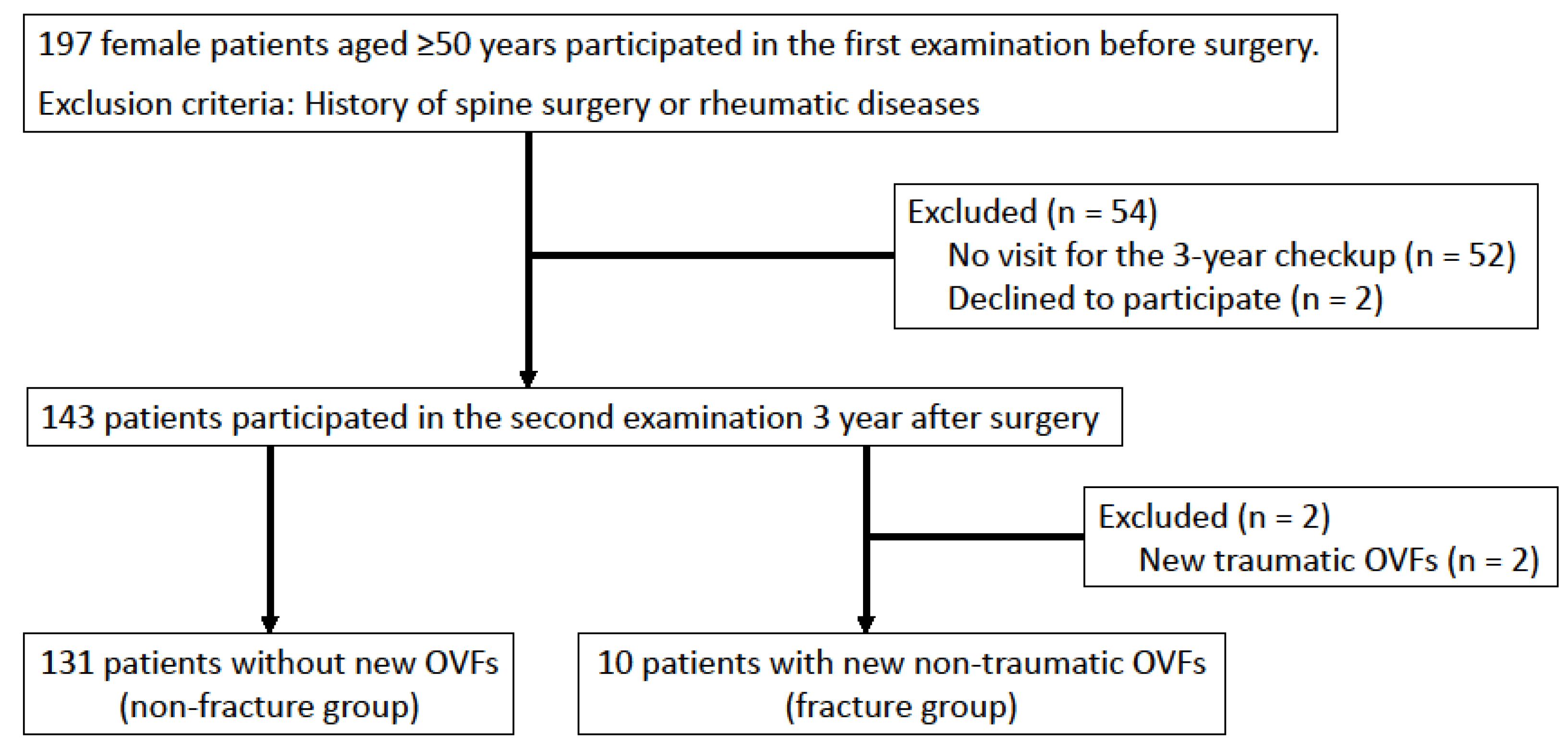
2.2. Study Participants
2.3. Evaluation
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Burge, R.; Dawson-Hughes, B.; Solomon, D.H.; Wong, J.B.; King, A.; Tosteson, A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J. Bone Miner. Res. 2007, 22, 465–475. [Google Scholar] [CrossRef] [PubMed]
- Christiansen, B.A.; Bouxsein, M.L. Biomechanics of vertebral fractures and the vertebral fracture cascade. Curr. Osteoporos. Rep. 2010, 8, 198–204. [Google Scholar] [CrossRef] [PubMed]
- Lindsay, R.; Silverman, S.L.; Cooper, C.; Hanley, D.A.; Barton, I.; Broy, S.B.; Licata, A.; Benhamou, L.; Geusens, P.; Flowers, K.; et al. Risk of new vertebral fracture in the year following a fracture. JAMA 2001, 285, 320–323. [Google Scholar] [CrossRef] [PubMed]
- Horii, C.; Asai, Y.; Iidaka, T.; Muraki, S.; Oka, H.; Tsutsui, S.; Hashizume, H.; Yamada, H.; Yoshida, M.; Kawaguchi, H.; et al. Differences in prevalence and associated factors between mild and severe vertebral fractures in Japanese men and women: The third survey of the ROAD study. J. Bone Miner. Metab. 2019, 37, 844–853. [Google Scholar] [CrossRef]
- Kado, D.M.; Duong, T.; Stone, K.L.; Ensrud, K.E.; Nevitt, M.C.; Greendale, G.A.; Cummings, S.R. Incident vertebral fractures and mortality in older women: A prospective study. Osteoporos. Int. 2003, 14, 589–594. [Google Scholar] [CrossRef]
- Jalava, T.; Sarna, S.; Pylkkänen, L.; Mawer, B.; Kanis, J.A.; Selby, P.; Davies, M.; Adams, J.; Francis, R.M.; Robinson, J.; et al. Association between vertebral fracture and increased mortality in osteoporotic patients. J. Bone Miner. Res. 2003, 18, 1254–1260. [Google Scholar] [CrossRef]
- Schousboe, J.T. Epidemiology of Vertebral Fractures. J. Clin. Densitom. 2016, 19, 8–22. [Google Scholar] [CrossRef]
- Cooper, C.; O’Neill, T.; Silman, A. The epidemiology of vertebral fractures. European Vertebral Osteoporosis Study Group. Bone 1993, 14 (Suppl. S1), S89–S97. [Google Scholar] [CrossRef]
- Balasubramanian, A.; Zhang, J.; Chen, L.; Wenkert, D.; Daigle, S.G.; Grauer, A.; Curtis, J.R. Risk of subsequent fracture after prior fracture among older women. Osteoporos. Int. 2019, 30, 79–92. [Google Scholar] [CrossRef]
- Banefelt, J.; Åkesson, K.E.; Spångéus, A.; Ljunggren, O.; Karlsson, L.; Ström, O.; Ortsäter, G.; Libanati, C.; Toth, E. Risk of imminent fracture following a previous fracture in a Swedish database study. Osteoporos. Int. 2019, 30, 601–609. [Google Scholar] [CrossRef]
- Mitchell, W.K.; Williams, J.; Atherton, P.; Larvin, M.; Lund, J.; Narici, M. Sarcopenia, dynapenia, and the impact of advancing age on human skeletal muscle size and strength; a quantitative review. Front. Physiol. 2012, 3, 260. [Google Scholar] [CrossRef] [PubMed]
- Delmonico, M.J.; Harris, T.B.; Visser, M.; Park, S.W.; Conroy, M.B.; Velasquez-Mieyer, P.; Boudreau, R.; Manini, T.M.; Nevitt, M.; Newman, A.B.; et al. Longitudinal study of muscle strength, quality, and adipose tissue infiltration. Am. J. Clin. Nutr. 2009, 90, 1579–1585. [Google Scholar]
- Singh, D.K.; Bailey, M.; Lee, R.Y. Ageing modifies the fibre angle and biomechanical function of the lumbar extensor muscles. Clin Biomech (Bristol, Avon) 2011, 26, 543–547. [Google Scholar] [CrossRef] [PubMed]
- Anderson, D.E.; D’Agostino, J.M.; Bruno, A.G.; Demissie, S.; Kiel, D.P.; Bouxsein, M.L. Variations of CT-based trunk muscle attenuation by age, sex, and specific muscle. J. Gerontol. A Biol. Sci. Med. Sci. 2013, 68, 317–323. [Google Scholar] [CrossRef] [PubMed]
- Dai, J.; Yu, X.; Huang, S.; Fan, L.; Zhu, G.; Sun, H.; Tang, X. Relationship between sagittal spinal alignment and the incidence of vertebral fracture in menopausal women with osteoporosis: A multicenter longitudinal follow-up study. Eur. Spine J. 2015, 24, 737–743. [Google Scholar] [CrossRef] [PubMed]
- Asahi, R.; Nakamura, Y.; Kanai, M.; Watanabe, K.; Yuguchi, S.; Kamo, T.; Azami, M.; Ogihara, H.; Asano, S. Stand-up test predicts occurrence of non-traumatic vertebral fracture in outpatient women with osteoporosis. J. Bone Miner. Metab. 2021, 39, 883–892. [Google Scholar] [CrossRef]
- Lin, T.; Lu, J.; Zhang, Y.; Wang, Z.; Chen, G.; Gu, Y.; Zhou, L.; Liu, W. Does spinal sagittal imbalance lead to future vertebral compression fractures in osteoporosis patients. Spine J. 2021, 21, 1362–1375. [Google Scholar] [CrossRef]
- Dreischarf, M.; Shirazi-Adl, A.; Arjmand, N.; Rohlmann, A.; Schmidt, H. Estimation of loads on human lumbar spine: A review of in vivo and computational model studies. J. Biomech. 2016, 49, 833–845. [Google Scholar] [CrossRef]
- Kato, S.; Demura, S.; Kurokawa, Y.; Shinmura, K.; Yokogawa, N.; Yonezawa, N.; Shimizu, T.; Oku, N.; Kitagawa, R.; Matsubara, H.; et al. Correlation between osteoporotic vertebral fracture and abdominal trunk muscle strength in middle-aged and older women. Arch. Osteoporos. 2019, 14, 106. [Google Scholar] [CrossRef]
- Suzuki, T. Reliability of measurements of knee extensor muscle strength using a pull-type hand-held dynamometer. J. Phys. Ther. Sci. 2015, 27, 967–971. [Google Scholar] [CrossRef]
- Kato, S.; Murakami, H.; Inaki, A.; Mochizuki, T.; Demura, S.; Nakase, J.; Yoshioka, K.; Yokogawa, N.; Igarashi, T.; Takahashi, N.; et al. Innovative exercise device for the abdominal trunk muscles: An early validation study. PLoS ONE 2017, 12, e0172934. [Google Scholar] [CrossRef] [PubMed]
- Kato, S.; Inaki, A.; Murakami, H.; Kurokawa, Y.; Mochizuki, T.; Demura, S.; Yoshioka, K.; Yokogawa, N.; Yonezawa, N.; Shimizu, T.; et al. Reliability of the muscle strength measurement and effects of the strengthening by an innovative exercise device for the abdominal trunk muscles. J. Back Musculoskelet. Rehabil. 2020, 33, 677–684. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, K.; Ogata, T. Locomotive Syndrome: Definition and Management. Clin. Rev. Bone Miner. Metab. 2016, 14, 56–67. [Google Scholar] [CrossRef] [PubMed]
- Genant, H.K.; Wu, C.Y.; van Kuijk, C.; Nevitt, M.C. Vertebral fracture assessment using a semiquantitative technique. J. Bone Miner. Res. 1993, 8, 1137–1148. [Google Scholar] [CrossRef] [PubMed]
- Schwab, F.; Ungar, B.; Blondel, B.; Buchowski, J.; Coe, J.; Deinlein, D.; DeWald, C.; Mehdian, H.; Shaffrey, C.; Tribus, C.; et al. Scoliosis Research Society-Schwab adult spinal deformity classification: A validation study. Spine (Phila Pa 1976) 2012, 37, 1077–1082. [Google Scholar] [CrossRef]
- Wu, J.; Wei, F.; Ma, L.; Li, J.; Zhang, N.; Tian, W.; Sun, Y. Accuracy and Reliability of Standing Lateral Lumbar Radiographs for Measurements of Spinopelvic Parameters. Spine (Phila Pa 1976) 2021, 46, 1033–1038. [Google Scholar] [CrossRef]
- Inose, H.; Kato, T.; Ichimura, S.; Nakamura, H.; Hoshino, M.; Togawa, D.; Hirano, T.; Tokuhashi, Y.; Ohba, T.; Haro, H.; et al. Risk factors for subsequent vertebral fracture after acute osteoporotic vertebral fractures. Eur. Spine J. 2021, 30, 2698–2707. [Google Scholar] [CrossRef]
- Kurokawa, Y.; Kato, S.; Demura, S.; Shinmura, K.; Yokogawa, N.; Yonezawa, N.; Shimizu, T.; Kitagawa, R.; Miaki, H.; Tsuchiya, H. Validation and comparison of trunk muscle activities in male participants during exercise using an innovative device and abdominal bracing maneuvers. J. Back Musculoskelet. Rehabil. 2022, 35, 589–596. [Google Scholar] [CrossRef]
- Akuthota, V.; Ferreiro, A.; Moore, T.; Fredericson, M. Core stability exercise principles. Curr. Sports Med. Rep. 2008, 7, 39–44. [Google Scholar] [CrossRef]
- Akuthota, V.; Nadler, S.F. Core strengthening. Arch. Phys. Med. Rehabil. 2004, 85, S86–S92. [Google Scholar] [CrossRef]
- Kato, S.; Demura, S.; Kurokawa, Y.; Takahashi, N.; Shinmura, K.; Yokogawa, N.; Yonezawa, N.; Shimizu, T.; Kitagawa, R.; Tsuchiya, H. Efficacy and Safety of Abdominal Trunk Muscle Strengthening Using an Innovative Device in Elderly Patients with Chronic Low Back Pain: A Pilot Study. Ann. Rehabil. Med. 2020, 44, 246–255. [Google Scholar] [CrossRef] [PubMed]
- Ohnishi, T.; Iwata, A.; Kanayama, M.; Oha, F.; Hashimoto, T.; Iwasaki, N. Impact of spino-pelvic and global spinal alignment on the risk of osteoporotic vertebral collapse. Spine Surg. Relat. Res. 2018, 2, 72–76. [Google Scholar] [CrossRef]
- Hongo, M.; Itoi, E.; Sinaki, M.; Miyakoshi, N.; Shimada, Y.; Maekawa, S.; Okada, K.; Mizutani, Y. Effect of low-intensity back exercise on quality of life and back extensor strength in patients with osteoporosis: A randomized controlled trial. Osteoporos. Int. 2007, 18, 1389–1395. [Google Scholar] [CrossRef] [PubMed]
- Hongo, M.; Miyakoshi, N.; Shimada, Y.; Sinaki, M. Association of spinal curve deformity and back extensor strength in elderly women with osteoporosis in Japan and the United States. Osteoporos. Int. 2012, 23, 1029–1034. [Google Scholar] [CrossRef] [PubMed]
- Miyakoshi, N.; Kudo, D.; Hongo, M.; Kasukawa, Y.; Ishikawa, Y.; Shimada, Y. Comparison of spinal alignment, muscular strength, and quality of life between women with postmenopausal osteoporosis and healthy volunteers. Osteoporos. Int. 2017, 28, 3153–3160. [Google Scholar] [CrossRef]
- Sinaki, M.; Itoi, E.; Wahner, H.W.; Wollan, P.; Gelzcer, R.; Mullan, B.P.; Collins, D.A.; Hodgson, S.F. Stronger back muscles reduce the incidence of vertebral fractures: A prospective 10 year follow-up of postmenopausal women. Bone 2002, 30, 836–841. [Google Scholar] [CrossRef]
- Sinaki, M.; Mikkelsen, B.A. Postmenopausal spinal osteoporosis: Flexion versus extension exercises. Arch. Phys. Med. Rehabil. 1984, 65, 593–596. [Google Scholar]
- Sinaki, M. Exercise for patients with osteoporosis: Management of vertebral compression fractures and trunk strengthening for fall prevention. PM R 2012, 4, 882–888. [Google Scholar] [CrossRef]


| Patients with the 2nd Examination | Patients without the 2nd Examination | p-Value | |
|---|---|---|---|
| No. of participants | 143 | 54 | |
| Age (years), mean ± SD [range] | 65.8 ± 8.3 (50–84) | 69.1 ± 7.8 (53–84) | 0.013 |
| BMI (kg/m2), mean ± SD [range] | 23.8 ± 3.9 (14.7–36.7) | 24.4 ± 4.8 (14.1–34.4) | 0.411 |
| L-BMD (g/cm2), mean ± SD [range] | 1.07 ± 0.22 (0.63–1.80) | 1.01 ± 0.18 (0.65–1.37) | 0.057 |
| Presence of old OVF, no. (%) | 17 (11.9) | 7 (13.0) | 0.837 |
| Disease pathology (n) | Hip joint disease (100) Knee joint disease (20) Foot & ankle disease (23) | Hip joint disease (35) Knee joint disease (8) Foot & ankle disease (11) |
| Fracture Group | Non-Fracture Group | p-Value | |
|---|---|---|---|
| No. of subjects | 10 | 131 | |
| Age (years), mean ± SD | 67.5 ± 9.3 | 65.6 ± 8.3 | 0.491 |
| BMI (kg/m2), mean ± SD | 25.4 ± 5.7 | 23.7 ± 3.7 | 0.177 |
| Hand grip strength (kg), mean ± SD | 18.3 ± 6.1 | 21.1 ± 5.0 | 0.089 |
| KEMS (N/kg), mean ± SD | 3.5 ± 1.6 | 3.8 ± 1.2 | 0.552 |
| ATMS (kPa), mean ± SD | 2.7 ± 1.8 | 5.3 ± 2.8 | 0.006 |
| GLFS-25 score (point), mean ± SD | 48.0 ± 27.2 | 40.0 ± 19.3 | 0.221 |
| NRS (0–4) of back pain (point), median [IQR] | 1 [1–1] | 1 [0–2] | 0.431 |
| L-BMD (g/cm2), mean ± SD | 0.93 ± 0.16 | 1.08 ± 0.22 | 0.027 |
| Presence of old OVF, No. (%) | 6 (60) | 11 (8.4) | <0.001 |
| Sagittal vertical axis (mm), mean ± SD | 51.1 ± 39.9 | 38.8 ± 42.6 | 0.378 |
| Lumbar lordosis (degree), mean ± SD | 43.7 ± 19.6 | 46.1 ± 16.7 | 0.671 |
| Pelvic incidence (degree), mean ± SD | 52.8 ± 9.0 | 55.4 ± 10.6 | 0.451 |
| Sacral slope (degree), mean ± SD | 27.8 ± 13.9 | 38.4 ± 12.3 | 0.010 |
| Pelvic tilt (degree), mean ± SD | 24.7 ± 10.7 | 17.0 ± 11.1 | 0.036 |
| Pelvic incidence minus Lumbar lordosis (degree), mean ± SD | 9.1 ± 15.1 | 9.4 ± 15.8 | 0.962 |
| Reference | aOR | p-Value | 95% CI | |
|---|---|---|---|---|
| ATMS (kPa) | +1 kPa | 0.557 | 0.037 | 0.322–0.964 |
| L-BMD (g/cm2) | +1 SD | 0.226 | 0.011 | 0.072–0.707 |
| Presence of old OVF | No old OVF | 6.956 | 0.023 | 1.304–37.105 |
| Sacral slope (degree) | +1 kPa | 0.924 | 0.087 | 0.843–1.012 |
| Pelvic tilt (degree) | +1 kPa | 0.973 | 0.588 | 0.882–1.073 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kato, S.; Demura, S.; Shinmura, K.; Yokogawa, N.; Kurokawa, Y.; Annen, R.; Kobayashi, M.; Yamada, Y.; Nagatani, S.; Matsubara, H.; et al. Associations between Abdominal Trunk Muscle Weakness and Future Osteoporotic Vertebral Fracture in Middle-Aged and Older Adult Women: A Three-Year Prospective Longitudinal Cohort Study. J. Clin. Med. 2022, 11, 4868. https://doi.org/10.3390/jcm11164868
Kato S, Demura S, Shinmura K, Yokogawa N, Kurokawa Y, Annen R, Kobayashi M, Yamada Y, Nagatani S, Matsubara H, et al. Associations between Abdominal Trunk Muscle Weakness and Future Osteoporotic Vertebral Fracture in Middle-Aged and Older Adult Women: A Three-Year Prospective Longitudinal Cohort Study. Journal of Clinical Medicine. 2022; 11(16):4868. https://doi.org/10.3390/jcm11164868
Chicago/Turabian StyleKato, Satoshi, Satoru Demura, Kazuya Shinmura, Noriaki Yokogawa, Yuki Kurokawa, Ryohei Annen, Motoya Kobayashi, Yohei Yamada, Satoshi Nagatani, Hidenori Matsubara, and et al. 2022. "Associations between Abdominal Trunk Muscle Weakness and Future Osteoporotic Vertebral Fracture in Middle-Aged and Older Adult Women: A Three-Year Prospective Longitudinal Cohort Study" Journal of Clinical Medicine 11, no. 16: 4868. https://doi.org/10.3390/jcm11164868







